Abstract
Objectives. We examined whether racial discrimination is associated with increased body mass index (BMI) and obesity among Asian Americans. Further, we explored whether this association strengthens with increasing time in the United States.
Methods. We analyzed data from the 2002 to 2003 National Latino and Asian American Study (n=1956). Regression models tested whether reports of racial discrimination were associated with BMI and obesity, after accounting for weight discrimination, age, gender, marital status, ethnicity, generation, employment, health status, and social desirability bias (the tendency to seek approval by providing the most socially desirable response to a question).
Results. We found that (1) racial discrimination was associated with increased BMI and obesity after we controlled for weight discrimination, social desirability bias, and other factors and (2) the association between racial discrimination and BMI strengthened with increasing time in the United States.
Conclusions. Racial discrimination may be an important factor related to weight gain among ethnic minorities.
Stress caused by disadvantaged social status may be related to obesity. Two elements provide the foundation for this observation. First, stress may have adverse physiological consequences, including increased risk for obesity and allostatic load, the “wear and tear” on organ systems that contributes to health problems.1 Stressors activate the hypothalamic–pituitary–adrenal axis system, releasing cortisol and other glucocorticoids. Glucocorticoids may stimulate appetite and blunt the satiety system.2 Cortisol increases fat retention, particularly in the abdominal region.3 Moreover, stressors may selectively increase the intake of “comfort foods” over other foods among humans and other animals.4,5
Stress may also be related to abdominal and general obesity. Daily stress,6 anxiety,7 and depressed mood8,9 are related to visceral obesity. Among monozygotic twins, stress-induced hormonal changes result in greater intra-abdominal fat deposits in the twin with higher stress.10 Further, obesity, indicated by a high body mass index (BMI), has been associated with work stress11,12 and early childhood trauma.13 In a prospective study of British civil servants, job stress was associated with metabolic syndrome (a group of risk factors that includes abdominal obesity, elevated blood pressure, and atherogenic dyslipidemia)8 and general and visceral obesity.12
Second, social disadvantage, such as experiences with racial discrimination, may produce stress.14 Self-reported discrimination appears to be related to several stress-related and obesity-related outcomes, including high blood pressure,15 depression and anxiety,16 sleep problems,17 and coronary calcification.18 Individuals may also use alcohol to cope with discrimination,19–21 and alcohol can contribute to obesity.22 Hence, discrimination may directly produce weight gain by activating the stress system and by influencing behavior change. Discrimination also may act indirectly by hindering socioeconomic advancement23,24 and by segregating individuals into communities with fewer healthy food options25,26 and fewer safe places for physical activity.27,28
Consistent with these observations, several studies have suggested that discrimination is associated with weight gain and metabolic problems. Tull et al. found that reports of internalized racism were associated with greater obesity among women in Barbados.29 Similarly, Chambers et al. found associations between internalized racism and insulin resistance among girls in Barbados.30 Butler et al. found associations between internalized racism and greater waist circumference and higher fasting glucose among Dominica women.31
We tested the first hypothesis that reports of discrimination are associated with higher BMI and the risk of obesity and build on previous research in 3 primary ways. First, overweight people may encounter weight discrimination,32 and associations between racial discrimination and weight might therefore be confounded by weight discrimination. To reduce the chance of spurious findings, we controlled for weight discrimination and other factors.
Second, we examined whether findings from Black populations generalize to Asian Americans. Among Asian Americans, discrimination is associated with outcomes related to obesity, including cardiovascular conditions,33,34 depression,35–37 and substance use,19 but no study has directly examined whether discrimination is associated with BMI and obesity in this population.
Third, we tested the main effects of discrimination and investigated whether discrimination is moderated by time spent in the United States. US-born Asians appear to have higher rates of obesity than their foreign-born counterparts, but the rates of obesity among the foreign born increase with years in the United States.38–40 Additionally, immigrants often report less racial discrimination than do nonimmigrants, but reports of discrimination increase with years spent in the United States, perhaps because immigrants are more likely to encounter and recognize discrimination over time.41–43 A recent study found that among African and Latino immigrants, the association between racial discrimination and mental health strengthened with increasing time in the United States.44 These observations motivate the second hypothesis that time spent in the United States will interact with the association between racial discrimination, such that the association between racial discrimination and BMI among immigrant Asians will strengthen with increasing time spent in the United States.
METHODS
Sample
Data were from the National Latino and Asian American Study (NLAAS). Inclusion criteria included Asian or Latino heritage, age 18 years or older, and residence in any of the 50 states or the District of Columbia. We focused on the Asian sample. The sampling design had 3 components: (1) selection of housing units based on primary sampling of metropolitan statistical areas or counties and secondary sampling units from census blocks; (2) sampling of housing units from block groups with greater than 5% density of Asian ethnic groups; (3) “secondary-respondent sampling,” in which a second person was interviewed from a household in which a primary respondent had already been interviewed. We oversampled Chinese (n = 600), Vietnamese (n = 508), and Filipinos (n = 502), but also included Asian Indians (n = 148), Japanese (n = 115), Koreans (n = 84), Pacific Islanders (n = 38), and other Asians (n = 82). We developed weights to account for the joint probabilities of selection for these 3 components and to allow the sample estimates to be nationally representative.45
Trained interviewers administered the survey in English, Cantonese, Mandarin, Spanish, Tagalog, or Vietnamese, either face-to-face or via telephone. Our sample included a total of 2095 Asian Americans (1611 primary and 484 secondary respondents). The response rates for primary and secondary respondents were 69.3% and 73.7%, respectively.45 Additional details of the study sample can be found elsewhere.45–47
Body Mass Index, Overweight, and Obesity
BMI was calculated by dividing self-reported weight in kilograms by height in meters squared.48 We classified BMI into the following categories: underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30.0 kg/m2).48 Because underweight was not prevalent (5.6% of the sample) and resulted in some analytic strata having few to no respondents (e.g., no one reporting weight discrimination was underweight), underweight was combined with normal, resulting in 3 categories: underweight or normal, overweight, and obese.
Self-Reported Experiences of Discrimination
Measures of discrimination were adapted from the Everyday Discrimination Scale.49,50 In this scale, respondents are first asked to respond to 9 items on unfair treatment and then asked to state the main reason for this unfair treatment. Because a primary goal of our study was to examine how racial discrimination—independent of weight discrimination or general experiences of unfair treatment—is associated with BMI, we examined only a respondent’s main reason for discrimination. These main reasons were coded into the following mutually exclusive categories: race (includes nationality, ethnicity, and skin color), weight, and other (includes height, gender, age, sexual orientation, income, and education); they were modeled as binary variables (yes or no). Height, gender, and income or education discrimination were considered as distinct variables but were not associated with BMI or obesity. Accordingly, these types of discrimination were included in the “other” category for parsimony.
Covariates
We included covariates for several factors that may confound the association between racial discrimination and BMI or obesity; these were sociodemographic characteristics, mental and physical illness, and social desirability bias.
A variety of sociodemographic characteristics have been correlated with both health and discrimination.51,52 We included the following in our analyses: marital status, gender, age, ethnicity (Chinese, Filipino, Vietnamese, other Asian/Pacific Islander), employment status, immigration generation (whether respondent or parents were US born or foreign born), and number of years spent in the United States.
Discrimination has been associated with depression and other mental disorders among Asian Americans.31,32 Additionally, obese people are at increased risk of experiencing mood disorders.53,54 To account for confounding caused by mental disorders, we used the World Health Organization Composite International Diagnostic Interview,55 an instrument that assesses the presence of psychiatric disorders using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV), criteria.56 Mental disorders, operationalized as a binary variable, indicated the presence of any of the following within the past 12 months: major depressive disorder, dysthymia, panic disorder, agoraphobia without panic, social phobia, generalized anxiety disorder, posttraumatic stress disorder, alcohol abuse, alcohol dependence, drug abuse, and drug dependence.
Although discrimination is purported to cause poor health, it is also possible that poor health causes one to report discrimination and contributes to obesity. We assessed self-rated physical health using 1 question: How would you rate your overall physical health?57 Responses ranged from 1 (poor) to 5 (excellent).
We also included a control for social desirability bias. Individuals are likely to under-report their weight to conform to socially desirable expectations of slimness. Moreover, people with high social desirability scores tend to underreport discrimination in order to “save face” and because of concerns that reports of discrimination will be met with skepticism.58,59 We used a 10-item social desirability scale developed by Crowne and Marlowe.60 Representative items include “I have never met a person I didn’t like” and “I always win at games.” Scores range from 0 (no social desirability bias) to 10 (highest social desirability bias). The internal consistency reliability coefficient (Kuder–Richardson Formula 20) was 0.71 for this sample.
Analyses
Ordinary least squares regression was used to test the hypothesis that discrimination is associated with higher BMI, with adjustment for age, gender, marital status, ethnicity, generation, employment, poverty, self-rated health, mental disorders, and social desirability bias. We used multinomial logistic regression to examine the association between discrimination and overweight and obesity (ordered logit was not used because the parallel regression assumption was violated).
To examine whether the association between racial discrimination and BMI varied by years living in the United States among immigrants, we included interaction terms in our ordinary least squares models. However, because years living in the United States was relevant only for immigrants and considered “missing” for nonimmigrants, we followed the approach of using conditionally relevant variables.61,62 This approach allowed the inclusion of the US born in our interaction model. We then calculated simple slopes and plotted the interactions to aid interpretation. In the interaction analyses, continuous covariates were centered at their mean to facilitate interpretation of the intercept. This interaction analysis was performed for BMI but not for obesity because of difficulties in testing and interpreting interactions with multinomial models.
One outlier and 138 cases with missing data were excluded, leaving 1956 respondents. Compared with the rest of the sample, excluded respondents were slightly older and less likely to be employed, but they did not differ in terms of BMI or reports of discrimination. All models were weighted to account for sample design. Stata version 9.2 software (StataCorp LP, College Station, Tex) was used.
RESULTS
Table 1 ▶ shows the characteristics of the sample. About 65% were underweight or normal, 27% overweight, and 9% obese. Although most respondents were in the normal-weight category, the average BMI was 24.2 kg/m2, just under the overweight threshold of 25 kg/m2. Most of the sample reported experiencing discrimination. Nearly 42% reported discrimination because of race/ethnicity, followed by income or education (6%), age (4%), gender (3%), weight (0.8%), height (0.8%), and other factors (17%). Approximately 10% had had a mental disorder within the past 12 months, and 15.8% reported fair or poor self-rated health. Participants reported a mean of 2.2 of the 10 items measuring social desirability bias. Most of the sample was employed (64%), foreign born (77%), married (75%), and lived in the West (67%).
TABLE 1—
Sample Weighted Characteristics of Asian Respondents (n = 1956): National Latino and Asian American Study, 2002–2003
| Characteristic | Value |
| BMI, kg/m2, mean (SD) | 24.2 (4.4) |
| Weight category,a % | |
| Underweight/normal | 64.9 |
| Overweight | 26.9 |
| Obese | 9.3 |
| Discrimination,b % | |
| None | 25.4 |
| Racial | 41.7 |
| Weight | 0.8 |
| Other | 32.1 |
| 12-mo DSM-IV mental disorder, % | 9.5 |
| Self-rated physical health, % | |
| Excellent | 17.2 |
| Very good | 32.5 |
| Good | 34.5 |
| Fair | 13.4 |
| Poor | 2.4 |
| Social desirability bias,c mean (SD) | 2.2 (2.1) |
| Age, mean (SD) | 41.1 (15.6) |
| Gender, % | |
| Women | 52.4 |
| Men | 47.6 |
| Ethnicity, % | |
| Vietnamese | 12.9 |
| Filipino | 21.6 |
| Chinese | 28.2 |
| Other Asian or Pacific Islander | 37.4 |
| Employed, % | 64.1 |
| Immigrant status, % | |
| Respondent foreign born | 76.6 |
| Respondent born in US, at least 1 parent foreign born | 14.1 |
| Respondent and both parents born in US | 9.4 |
| Years in the US, mean (SD) | 16.1 (15.5) |
| Marital status, % | |
| Married, living with partner | 65.1 |
| Never married, widowed, separated, divorced | 34.9 |
Note. BMI = body mass index; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.56
aWe classified BMI into the following categories: underweight (< 18.5 kg/m2), normal (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese (≥ 30.0 kg/m2).
bMeasures of discrimination were adapted from the Everyday Discrimination Scale. In this scale, respondents are first asked to respond to 9 items on unfair treatment and then asked to state the main reason for this unfair treatment.
cThe scale ranged from 0 (no social desirability bias) to 10 (highest social desirability bias).
BMI was positively associated with years in the United States, age, marital status, employment, male gender, ethnicity, birth in the United States, and depression. Racial discrimination was correlated with age, female gender, ethnicity, years in the United States, social desirability bias, self-rated health, and weight or other discrimination. A full correlation table is available upon request from G. C. G.
Table 2 ▶ shows the association between self-reported discrimination and BMI. The first column displays the raw means. BMI is highest among those reporting weight discrimination (mean = 31.2 kg/m2), followed by racial (mean = 24.5 kg/m2) and other (mean = 23.6 kg/m2) discrimination, and lowest among those not reporting any discrimination (mean = 23.5 kg/m2). The next column (model 2.1) shows the unadjusted regression analysis comparing BMI across the types of discrimination. BMI was significantly higher among those reporting weight (b = 0.97; P≤ .001) and racial (b = 0.97; P≤ .01) discrimination than among those not reporting discrimination. BMI was also higher among those reporting other discrimination, but the strength of association was lower (b = 0.09; P≤ .05) than for racial and weight discrimination. The third column (model 2.2) shows the associations adjusted for covariates. Weight discrimination (b = 0.86; P≤ .001) and racial discrimination (b = 0.68; P≤ .05) remained significantly associated with BMI, but other discrimination was no longer significant.
TABLE 2—
Association Between Self-Reported Discrimination and Body Mass Index (BMI) Among Asian Respondents (n=1956): National Latino and Asian American Study, 2002–2003
| Model 2.1 (Unadjusted)a,b | Model 2.2 (Adjusted)a,b,c | ||||
| Type of Discrimination | BMI,a kg/m2, Mean | b (SE) | P | b (SE) | P |
| None | 23.5 | Reference | Reference | ||
| Weight | 31.2 | 0.97 (0.22) | ≤ .001 | 0.86 (0.24) | ≤ .001 |
| Racial | 24.5 | 0.97 (0.30) | ≤ .01 | 0.68 (0.34) | ≤ .05 |
| Other | 23.6 | 0.09 (0.04) | ≤ .05 | 0.03 (0.91) | |
aWeighted to be nationally representative.
bOrdinary least squares regression.
cAnalyses controlled for age, gender, marital status, ethnicity, generation, employment, self-rated health status, 12-month mental disorders, and social desirability.
Table 3 ▶ shows how discrimination is associated with overweight and obesity. Among those considered overweight, 45.5% reported racial discrimination, 29.8% reported some other discrimination, 23.9% reported no discrimination, and 0.8% reported weight discrimination. A similar pattern was found among those classified as obese, although the reporting of weight discrimination was higher at 4% and the proportion of people reporting no discrimination dropped to 13.5%. In the second column (model 3.1), multinomial logistic regression was used to examine how discrimination is associated with overweight and obesity compared with normal weight. Reports of racial, weight, or other discrimination, compared with no discrimination, did not increase the odds of being overweight compared with being normal weight. Compared with no reports of discrimination, however, reports of any of these 3 types of discrimination increased the odds of being obese compared with being normal weight. For example, the reporting of racial discrimination (vs no discrimination) increased the odds of being obese (vs normal) by 2.42.
TABLE 3—
Association Between Self-Reported Discrimination and Overweight and Obesity Among Asian Respondents (n=1956): National Latino and Asian American Study, 2002–2003
| Model 3.1 (Unadjusted)a,b | Model 3.2 (Adjusted)a,b,c | ||||
| Distribution,a % | MOR (95% CI) | P | MOR (95% CI) | P | |
| Overweight | |||||
| No discrimination (Ref) | 23.9 | 1.00 | 1.00 | ||
| Weight discrimination | 0.8 | 1.16 (0.96, 1.39) | 1.11 (0.95, 1.30) | ||
| Racial discrimination | 45.5 | 1.34 (0.89, 2.01) | 1.16 (0.73, 1.83) | ||
| Other discrimination | 29.8 | 1.01 (0.96, 1.05) | 0.98 (0.94, 1.03) | ||
| Obesity | |||||
| No discrimination (Ref) | 13.5 | 1.00 | 1.00 | ||
| Weight discrimination | 4.0 | 1.51 (1.25, 1.83) | ≤ .001 | 1.52 (1.25, 1.85) | ≤ .001 |
| Racial discrimination | 46.5 | 2.42 (1.29, 4.54) | ≤ .01 | 2.12 (1.04, 4.33) | ≤ .05 |
| Other discrimination | 36.0 | 1.09 (1.01, 1.16) | ≤ .05 | 1.05 (0.98, 1.12) | |
Note. MOR = multinomial odds ratio; CI = confidence interval. Overweight was defined as a body mass index of 25.0 to 29.9 kg/m2 and obesity as 30.0 kg/m2 or greater.
aWeighted to be nationally representative.
bMultinomial logistic regression. The comparison group is “normal/underweight.”
cAnalyses controlled for age, gender, marital status, ethnicity, generation, employment, self-rated health status, 12-month mental disorders, and social desirability.
In the third column (model 3.2), covariates are included. A pattern similar to that of model 3.1 emerged, except that other discrimination were no longer significant. The odds for racial discrimination dropped slightly in model 3.2 (multinomial odds ratio = 2.12) compared with model 3.1, but it remained significant. Multinomial analyses are often difficult to interpret, and another way to think about these results is in probabilities. For a person with average values for the continuous covariates (e.g., age) and the modal values for the categorical covariates (e.g., marital status), the probability of being obese was 4.6% if the person did not report racial discrimination; however, the probability doubled to 9.3% if racial discrimination was reported.
We then tested the interaction between racial discrimination and years in the United States. After accounting for covariates, we found a significant interaction between years in the United States and racial discrimination. This interaction is plotted in 2 ways. Figure 1 ▶ shows that the association between discrimination and BMI strengthened with increasing time spent in the United States. Figure 2 ▶ shows that, among immigrants not reporting discrimination, BMI was constant across years spent in the United States. Among immigrants reporting discrimination, however, BMI increased with time spent in the United States.
FIGURE 1—
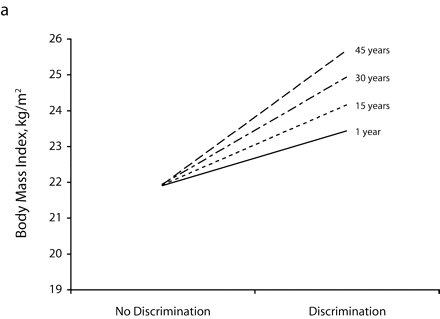
The relationship between racial discrimination and body mass index, among Asian respondents (n = 1956), by years spent in the United States: National Latino and Asian American Study, 2002–2003.
FIGURE 2—
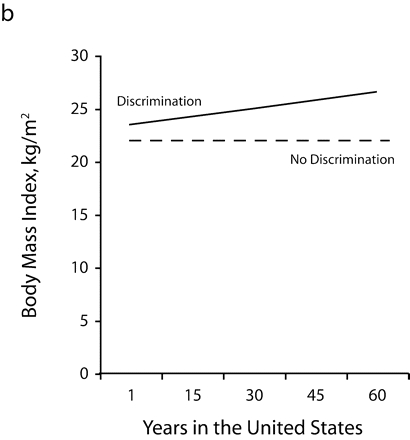
The relationship between racial discrimination and years spent in the United States among Asian respondents (n = 1956), by report of discrimination: National Latino and Asian American Study, 2002–2003.
We performed additional analyses to evaluate the robustness of our findings. First, we tested alternative indicators of socioeconomic position (per capita income, poverty, education), but the results of these analyses were consistent with those reported here. Second, we reran our multinomial logistic regression models, including underweight as a distinct outcome. Our findings were robust with that specification as well. Third, there has been some controversy regarding appropriate cut-points for overweight and obesity among persons of Asian descent. Some have argued that conventional BMI cutpoints underestimate the degree of risk for Asian populations and have suggested that the threshold for overweight and obesity should be lowered to 23 kg/m2 and 27.5 kg/m2, respectively.63 Results of analyses using these alternative thresholds were similar to those reported here. Fourth, we had considered region (West, Midwest, South, and Northeast) as a covariate, but region was omitted for parsimony because it was not significant in any models. Fifth, we tested moderation of discrimination with gender, nativity (US born vs immigrant), region, and ethnicity, but none of those interactions were significant.
DISCUSSION
We found that reports of racial and weight discrimination were associated with increased BMI and obesity among a nationally representative sample of Asian Americans. These findings persisted even after control for social desirability bias and a variety of other covariates.
Two important observations arise from these analyses. First, reports of weight discrimination were associated with increased BMI and obesity, suggesting that obese people experience discrimination because of their weight. Other studies have found that weight discrimination is associated with a variety of economic, social, and mental health outcomes, including decreased self-esteem, anxiety, and depression.32,64 Given the growing prevalence of obesity worldwide, it is important to continue to assess weight discrimination.65 Further, although it seems reasonable to assume that reports of weight discrimination arise because of one’s weight, future research might also examine whether weight discrimination is itself consequential. For example, one study found that being teased for being overweight was associated with disordered eating among obese and normal-weight boys.66
Second, reports of racial discrimination were associated with increased BMI and obesity among Asian Americans even after control for reports of weight discrimination and other factors. This finding is consistent with research suggesting that racial discrimination is a stressor. Our research joins other studies finding that racial discrimination, as measured by internalized racism, is associated with increased abdominal obesity and related problems among Blacks in Barbados and Dominica.29–31
The measurement of discrimination in future studies deserves further attention. Unlike the Barbados and Dominica studies, our study measured racial discrimination, not internalized racism. It is likely that reports of internalized racism (whereby one believes that the negative stereotypes associated with one’s racial group are true) differ from reports of how one experiences discriminatory treatment. Like our investigation, a study by Vines et al. asked about experiences with racism, but our findings are inconsistent with theirs.6 They found that Black women who reported no discrimination had higher levels of abdominal fat than those reporting discrimination. The authors suggested that their findings might be consistent with the internalized racism perspective if one assumed that reports of discrimination indicated “successful coping” and that no such reports indicated internalized racism. Another possibility is that the 2 studies had different findings because they used different sample populations; in the Vines et al. study, the respondents were premenopausal women of a prepaid health plan who volunteered for a uterine fibroids study. Future research should evaluate our contradictory findings by replicating our studies among a general population, using measures of both perceived discrimination and perceived internalized racism.
Perhaps the most interesting finding in our study is the interaction between years in the United States and racial discrimination. Among immigrants, the association between discrimination and BMI strengthened with increasing time in the United States, even after age and other factors were accounted for. Indeed, another study found that among African and Latino immigrants, the association between discrimination and poor mental health also increased with time in the United States.44 These patterns suggest that discrimination may be more “potent” among more acculturated immigrants, perhaps through the accumulation of stressors or because a given level of discrimination becomes more salient and important with increasing familiarity with US culture.
The interaction could be interpreted in another way. Studies of immigrants, Asian or otherwise, generally find a rise in BMI with years spent in the United States.38–40 These trends are often explained by dietary changes among immigrants. Our study did not examine diet, but diet could be an important mediator because stressors may cause one to seek sugary and fatty foods.4,5 Intriguingly, our data indicated that BMI was positively associated with time in the United States only among Asian immigrants reporting racial discrimination; however, among those not reporting discrimination, BMI was constant across years. Thus, these data suggest that general findings of rising BMI among immigrants67–69 might be qualified by racial discrimination.
Although we focused on the potential stress mechanism, it is likely that stress is just one pathway whereby racial discrimination may be associated with obesity.14,70 Structural discrimination, as evidenced by racial residential segregation, may decrease the availability of healthy foods and safe recreational areas.25–28,71,72 Fears of racial harassment may be a barrier to physical activity among Asians.73 An important question for future research is whether discrimination operates at multiple levels—for example, at the interpersonal level to induce stress and at the structural level to restrict dietary and physical activity options. Finally, although we focus on racial discrimination, many other biological and social factors are associated with obesity.52,74
Limitations
Several limitations should be acknowledged. Self-reported data are always subject to response factors. The prevalence of obesity in our study (9.3%) was slightly higher than that reported for Asian Americans in the 2005 National Health Interview Survey (8.5%), but our rates approach parity (8.8%) when we exclude Pacific Islanders from our estimates (who have a prevalence of 26.9%).75 Although we did not control for all response factors (e.g., recall bias), we did address the one factor that is very significant with regard to self-reported BMI and discrimination—social desirability bias. Individuals seeking approval by providing the most socially desirable response may misreport their weight and experiences with discrimination.59 Moreover, mental disorders might lead to inaccurate reporting. For example, depression might cause some people not only to lose or gain weight but also to misreport their weight and experiences of discrimination. It was thus important that the present study controlled for social desirability bias and mental disorders.
That said, future studies should use objective measures of BMI and alternative measures of risk (e.g., waist-to-hip ratio) as well as develop other ways to assess discrimination. Additionally, unlike prior studies that have often used the everyday discrimination scale without the attributions, we employed attributions of unfair treatment as the main analytic variable. Although doing so allowed us to distinguish weight from racial discrimination, these binary variables were limited in their ability to capture variation in the experience of discrimination. Future studies should use full scales of racial and weight discrimination. Further, our data are cross-sectional and we therefore cannot make causal statements. Our purported pathway—that racial discrimination causes obesity—seems more likely than the alternative of obesity causing racial discrimination. However, only prospective studies will provide a firmer test of this hypothesis.
Conclusions
Our study’s strengths include the use of a nationally representative sample of Asian Americans, adjustment for several important confounders, and theoretically derived hypotheses. To our knowledge, this is the first study that directly examines whether self-reports of racial discrimination are associated with increased BMI and obesity after accounting for weight discrimination. Our results raise several major areas for future research, including establishment of the causal direction, investigation of mediating pathways, and replication among other populations. Although preliminary, our findings also suggest that racial discrimination may account for some of the rise in obesity seen as immigrants spend more time in the United States.
Acknowledgments
The National Latino and Asian American Study is funded by the National Institute of Mental Health (grants U01 MH62209 and U01 MH62207), with additional support from the Office of Behavioral and Social Science Research and the Substance Abuse and Mental Health Services Administration.
Human Participant Protection Institutional review board approval was granted to G.C. Gee by the University of Michigan for data analysis purposes and to D. T. Takeuchi by the University of Washington for data collection and analysis.
Peer Reviewed
Contributors G. C. Gee led the writing and conceptualization of the study. A. Ro assisted with the writing and data analysis. A. Gavin assisted with the writing and editing. D. T. Takeuchi was the principal investigator of the National Latino and Asian American study and assisted with the writing.
References
- 1.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. [DOI] [PubMed] [Google Scholar]
- 2.Bjorntorp P. Do stress reactions cause abdominal obesity and comorbidities? Obes Rev. 2001;2:73–86. [DOI] [PubMed] [Google Scholar]
- 3.Rosmond R, Dallman M, Bjorntorp P. Stress-related cortisol secretion in men: relationships with abdominal obesity and endocrine, metabolic and hemodynamic abnormalities. J Clin Endocrinol Metab. 1998;83:1853–1859. [DOI] [PubMed] [Google Scholar]
- 4.Dallman MF, Pecoraro NC, la Fleur SE. Chronic stress and comfort foods: self-medication and abdominal obesity. Brain Behav Immun. 2005;19:275–280. [DOI] [PubMed] [Google Scholar]
- 5.Dallman MF, Pecoraro N, Akana SF, et al. Chronic stress and obesity: a new view of “comfort food.” Proc Natl Acad Sci U S A. 2003;100: 11696–11701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vines A, Baird D, Stevens J, Hertz-Picciotto I, Light K, McNeilly M. Associations of abdominal fat with perceived racism and passive emotional responses to racism in African American women. Am J Public Health. 2007;97:526–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosmond R, Lapidus L, Marin P, Bjorntorp P. Mental distress, obesity and body fat distribution in middle-aged men. Obes Res. 1996;4:245–252. [DOI] [PubMed] [Google Scholar]
- 8.Chandola T, Brunner E, Marmot M. Chronic stress at work and the metabolic syndrome: a prospective study. BMJ. 2006;332:521–525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee ES, Kim YH, Beck S, Lee S, Oh SW. Depressive mood and abdominal fat distribution in overweight premenopausal women. Obes Res. 2005;13:320–325. [DOI] [PubMed] [Google Scholar]
- 10.Marneimi J, Kronholm E, Aunola S, et al. Visceral fat and psychosocial stress in identical twins discordant for obesity. J Intern Med. 2002;251:35–43. [DOI] [PubMed] [Google Scholar]
- 11.Kouvonen A, Kivimaki M, Cox S, Cox T, Vahtera J. Relationship between work stress and body mass index among 45,810 female and male employees. Psychosom Med. 2005;67:577–583. [DOI] [PubMed] [Google Scholar]
- 12.Kivimaki J, Head J, Ferrie JE, et al. Work stress, weight gain and weight loss: evidence for bidirectional effects of job strain on body mass index in the Whitehall II study. Int J Obes. 2006;30:982–987. [DOI] [PubMed] [Google Scholar]
- 13.Gunstad J, Paul RH, Spitznagel MB, et al. Exposure to early life trauma is associated with adult obesity. Psychiatry Res. 2006;142:31–37. [DOI] [PubMed] [Google Scholar]
- 14.Williams DR, Neighbors H, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young Black and White adults. Am J Public Health. 1996;86(10):1370–1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Michelson KD, Williams DR. The prevalence, distribution and mental health correlates of perceived discrimination in the United States. J Health Soc Behav. 1999;40:208–230. [PubMed] [Google Scholar]
- 17.Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;16:16–21. [PubMed] [Google Scholar]
- 18.Lewis TT, Everson-Rose SA, Powell LH, et al. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: The SWAN Heart Study. Psychom Med. 2006;68:362–368. [DOI] [PubMed] [Google Scholar]
- 19.Gee GC, Delva J, Takeuchi DT. Perceived unfair treatment and the use of prescription medications, illicit drugs and alcohol dependence among Filipino Americans. Am J Public Health. 2007;97:933–940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yen IH, Ragland DR, Greiner BA, Fisher JM. Racial discrimination and alcohol-related behavior in urban transit operators: findings from the San Francisco Muni Health and Safety Study. Public Health Rep. 1999;114:448–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yen IH, Ragland DR, Greiner BA, Fisher JM. Workplace discrimination and alcohol consumption: findings from the San Francisco Muni Health and Safety Study. Ethn Dis. 1999;9:70–80. [PubMed] [Google Scholar]
- 22.Breslow RA, Smothers BA. Drinking patterns and body mass index in never smokers. Am J Epidemiol. 2005;161:368–376. [DOI] [PubMed] [Google Scholar]
- 23.Williams DR. Race, socioeconomic status, and health: the added effects of racism and discrimination. Ann N Y Acad Sci. 1999;896:173–188. [DOI] [PubMed] [Google Scholar]
- 24.Oliver ML, Shapiro TM. Black Wealth, White Wealth: A New Perspective on Inequality. New York, NY: Routledge; 1997.
- 25.Morland K, Wing S, Diez-Roux AV, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–29. [DOI] [PubMed] [Google Scholar]
- 26.LaVeist TA, Wallace JM. Health risk and inequitable distribution of liquor stores in African American neighborhood. Soc Sci Med. 2000;51:613–617. [DOI] [PubMed] [Google Scholar]
- 27.Williams DR, Collins CA. Racial residential segregation: a fundamental cause of racial disparities in health. Public Health Rep. 2001;116:404–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lopez R. Black–White residential segregation and physical activity. Ethn Dis. 2006;16:495–502. [PubMed] [Google Scholar]
- 29.Tull ES, Wickramasuriya T, Taylor J, et al. Relationship of internalized racism to abdominal obesity and blood pressure in Afro-Caribbean women. J Natl Med Assoc. 1999;91:447–452. [PMC free article] [PubMed] [Google Scholar]
- 30.Chambers EC, Tull ES, Fraser H, Mutunu NR, Sobers N, Niles E. The relationship of internalized racism to body fat distribution and insulin resistance among African adolescent youth. J Natl Med Assoc. 2004;96:1594–1598. [PMC free article] [PubMed] [Google Scholar]
- 31.Butler C, Tull ES, Chambers EC, Taylor J. Internalized racism, body fat distribution, and abnormal fasting glucose among African-Caribbean women in Dominica, West Indies. J Natl Med Assoc. 2002;94:143–148. [PMC free article] [PubMed] [Google Scholar]
- 32.Carr D, Friedman MA. Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J Health Soc Behav. 2005;46:244–259. [DOI] [PubMed] [Google Scholar]
- 33.Gee GC, Chen J, Spencer M, et al. Social support as a buffer for perceived unfair treatment among Filipino Americans: differences between San Francisco and Honolulu. Am J Public Health. 2006;96:677–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gee GC, Spencer M, Chen J, Takeuchi DT. A nationwide study of discrimination and chronic health conditions among Asian Americans. Am J Public Health. 2007;97:1275–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mossakowski KN. Coping with perceived discrimination: does ethnic identity protect mental health. J Health Soc Behav. 2003;44:318–331. [PubMed] [Google Scholar]
- 36.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation and ethnic support. Am J Public Health. 2003;93:232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee RM. Do ethnic identity and other-group orientation protect against discrimination for Asian Americans? J Couns Psychol. 2003;50:133–141. [Google Scholar]
- 38.Goel MS, McCarthy EP, Phillips RS, Wee CC. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292:2860–2867. [DOI] [PubMed] [Google Scholar]
- 39.Lauderdale DS, Rathouz PJ. Body mass index in a US national sample of Asian Americans: effects of nativity, years since immigration and socioeconomic status. Int J Obes. 2000;24:1188–1194. [DOI] [PubMed] [Google Scholar]
- 40.Popkin BM, Udry JR. Adolescent obesity increases significantly in second and third generation US immigrants: the National Longitudinal Study of Adolescent Health. J Nutr. 1998;128:701–706. [DOI] [PubMed] [Google Scholar]
- 41.Finch BA, Hummer RA, Kolody B, Vega WA. The role of discrimination and acculturative stress in Mexican-origin adults’ physical health. Hisp J Behav Sci. 2001;23:399–429. [Google Scholar]
- 42.Portes A, Parker RN, Cobas JA. Assimilation or consciousness: perceptions of US society among recent Latin American immigrants to the United States. Soc Forces. 1980;59:200–224. [Google Scholar]
- 43.Waters M. Black Identities. Boston, Mass: Harvard University Press; 1999.
- 44.Gee GC, Ryan AM, LaFlamme DJ, Holt J. Self-reported discrimination and mental health status among African Descendants, Mexican Americans, and other Latinos in the New Hampshire REACH 2010 Initiative: the added dimension of immigration. Am J Public Health. 2006;96:1821–1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Heerenga S, Warner J, Torres M, Duan N, Adams T, Berglund P. Sample designs and sampling methods for the Collaborative Psychiatric Epidemiology Studies (CPES). Int J Methods Psychiatr Res. 2004;13:221–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alegria M, Takeuchi DT, Canino G, Duan N, Shrout P, Meng X. Considering context, place, and culture: the National Latino and Asian American Study. Int J Methods Psychiatr Res. 2004;13:208–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Takeuchi DT, Zane N, Hong S, et al. Immigration-related factors and mental disorders among Asian Americans. Am J Public Health. 2007;97:84–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Heart, Lung and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. J Obes Res. 1998;6:51S–209S. [PubMed] [Google Scholar]
- 49.Jackson J, Williams DR. Detroit Area Study, 1995: social influences on health, stress, racism and health protective resources. Available at: http://www.icpsr.umich.edu/cocoon/ICPSR/STUDY/03272.xml. Accessed February 17, 2004.
- 50.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socioeconomic status, stress, and discrimination. J Health Psychol. 1997;2:335–351. [DOI] [PubMed] [Google Scholar]
- 51.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006;35:888–901. [DOI] [PubMed] [Google Scholar]
- 52.Canoy D, Buchan I. Challenges in obesity epidemiology. Obes Rev. 2007;8(suppl 1):1–11. [DOI] [PubMed] [Google Scholar]
- 53.Onyike CU, Crum RM, Hochang BL, Lyketsos CG, Eaton WW. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158: 1139–1147. [DOI] [PubMed] [Google Scholar]
- 54.Carpenter KM, Hasin DS, Allison DB, Faith MS. Relationships between obesity and DSM-IV major depressive disorder, suicide ideation, and suicide attempts: results from a general population study. Am J Public Health. 2000;90:251–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Disability Assessment Schedule II (WHO-DAS II). Geneva, Switzerland: World Health Organization; 1998.
- 56.Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- 57.Idler EL, Hudson SV, Leventhal H. The meanings of self-ratings of health. Res Aging. 1999;21:458–476. [Google Scholar]
- 58.Gee GC, Spencer M, Chen J, Yip T, Takeuchi DT. the association between self-reported discrimination and 12-month DSM-IV mental disorders among Asian Americans nationwide. Soc Sci Med. 2007;64:1984–1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Harrell SP. A multidimensional conceptualization of racism-related stress: implications for the well-being of people of color. Am J Orthopsychiatry. 2000;70:42–57. [DOI] [PubMed] [Google Scholar]
- 60.Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. J Consult Psychol. 1960;24:349–354. [DOI] [PubMed] [Google Scholar]
- 61.Noh S, Beiser M, Kaspar V, Hou F, Rummens J. Perceived racial discrimination, depression, and coping: a study of Southeast Asian refugees in Canada. J Health Soc Behav. 1999;40:193–207. [PubMed] [Google Scholar]
- 62.Ross CE, Mirowski J. Households, employment, and the sense of control. Soc Psychol Q. 1992;55:216–235. [Google Scholar]
- 63.World Health Organization. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004; 363:157–163. [DOI] [PubMed] [Google Scholar]
- 64.Puhl R, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. [DOI] [PubMed] [Google Scholar]
- 65.Puhl R, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. [DOI] [PubMed] [Google Scholar]
- 66.Neumark-Sztainer D, Falker N, Story M, et al. Weight-teasing among adolescents: correlations with weight status and disordered eating behaviors. Int J Obes. 2002;26:123–131. [DOI] [PubMed] [Google Scholar]
- 67.Frisbie WP, Cho Y, Hummer RA. Immigration and the health of Asian and Pacific Islander adults in the United States. Am J Epidemiol. 2001;153:372–380. [DOI] [PubMed] [Google Scholar]
- 68.Vega W, Kolody B, Aguilar-Gaxioloa S, Alderte E, Catalano R, Caraveo-Anduaga H. Lifetime prevalence of DSM-III-R psychiatric disorders among urban and rural Mexican Americans in California. Arch Gen Psychiatry. 1998;55:771–778. [DOI] [PubMed] [Google Scholar]
- 69.Hyman I, Forte T, Du Mont J, Romans S, Cohen MM. The association between length of stay in Canada and intimate partner violence among immigrant women. Am J Public Health. 2006;96:654–659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mays VM, Cochran S, Barnes NW. Race, race-based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92:615–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.LaVeist TA. Segregation, poverty, and empowerment: health consequences for African Americans. Milbank Q. 1993;71:41–64. [PubMed] [Google Scholar]
- 73.Johnson MRD. Perceptions of healthy physical activity among Asian communities. Sport Educ Soc. 2000;5:51–70. [Google Scholar]
- 74.Law C, Power C, Graham H, Merrick D. Obesity and health inequalities. Obes Rev. 2007;8(suppl 1):19–22. [DOI] [PubMed] [Google Scholar]
- 75.Pleis JR, Lethbridge-Cejku M. Summary health statistics for US adults: National Health Interview Survey, 2005. Vital Health Stat 10. 2006;No. 232:81. [PubMed]


