Abstract
Objectives
To determine the percentage of residents accepting faculty positions following completion of a community pharmacy residency program (CPRP) and identify influences to pursue/not pursue an academic career.
Methods
CPRP directors and preceptors across the United States were contacted and 53 community pharmacy residents were identified. The residents were invited to participate in surveys at the beginning and end of the 2005-2006 residency year.
Results
Forty-five residents (85%) completed the preliminary survey instrument and 40 (75%) completed the follow-up survey instrument. Of these, 36 completed both survey instruments. Initially, 28 (62%) respondents indicated a faculty position as one of their potential job preferences. After completing their residency program, 3 (8%) residents accepted faculty positions; and 3 (8%) others were awaiting offers at follow-up. Reasons for accepting a faculty position were positive teaching experiences and the influence of a mentor or preceptor. Reasons for not pursuing a faculty position included lack of interest, geographic location, disliked teaching experiences, lack of preparedness, and non-competitive salary.
Conclusion
Many community pharmacy residents consider faculty positions early in their residency but few pursue faculty positions. CPRPs and colleges of pharmacy should work together to enhance residents' experiences to foster interest in academia.
Keywords: academia, community pharmacy residents, residency training, faculty
INTRODUCTION
The shortage of pharmacy faculty members has been an ongoing concern of many colleges of pharmacy across the country. The American Association of Colleges of Pharmacy (AACP) has reported a significant number of vacant and lost positions over recent years and has identified faculty recruitment and retention as a top priority. There were nearly 400 vacant faculty positions in the 2004-2005 academic year with almost 50% within the divisions of clinical science/pharmacy practice.1 Colleges of pharmacy indicated the top 3 reasons that these positions remained vacant were not enough qualified candidates (defined as applicants unable to meet requirements/expectations, lack of qualified candidates in the field, and lack of response to the position), budget limitations, and geographic location. The AACP Council of Deans - Councils of Faculties (COD-COF) Faculty Recruitment and Retention Committee suggested in their 2004 Final Report that pharmacy residents and fellows are key candidates to train and fill these faculty positions.2 The committee specifically recommended that the AACP be involved in efforts to create opportunities for residents to be involved in teaching pharmacy students and that the feasibility of adding a teaching component to all residency and fellowship programs be evaluated. Furthermore, the 2002 AACP Task Force on the Role of Colleges and Schools in Residency Training recommended that postgraduate training be a requirement for entering a faculty position and that colleges of pharmacy work together with residency programs to provide teaching opportunities to all residents.3 The taskforce suggested that formal training in teaching be incorporated into these residency programs. Many residency programs, especially those affiliated with colleges of pharmacy, have already included teaching as a component to the residents' experience and some have even begun to offer teaching certificate programs.4-6
Approximately 60% of practicing pharmacists have positions in community pharmacy; therefore, this may be an area of growth for colleges of pharmacy in recruiting new faculty.7 Furthermore, with the passage of the Medicare Modernization Act of 2003, which recognizes pharmacists as providers for medication therapy management, and the adoption of the Accreditation Council for Pharmaceutical Education (ACPE) 2007 standards which encourage the development of patient care-centered advanced pharmacy practice experiences, opportunities will continue to expand for clinically focused advanced practice experiences in the community setting.8,9 Colleges and universities need to respond to this opportunity by growing the number of community pharmacy faculty positions and recognizing that a prime resource for community pharmacy faculty candidates are graduates of existing community pharmacy residency programs (CPRPs).
CPRPs have grown significantly over the past several years. According to the American Pharmacists Association (APhA), the number of programs has more than doubled from 23 in 1999 to 58 in 2006; the number of individual sites/positions has also grown, from 35 to 99 (written communication, American Pharmacists Association, January 14, 2007).10 Although the primary purpose of CPRPs is not to develop and train future faculty members, approximately 85% of these programs are currently affiliated with a college of pharmacy, thus making them a potential training ground for community pharmacy faculty members. In addition, colleges of pharmacy should invest resources in community pharmacy faculty members to expand CPRPs in order to meet the proposed requirement by ACCP of at least a post-graduate year one (PGY-1) residency to practice in direct patient care and/or obtain an adjunct faculty position (ie, preceptorship).11
Considering the continuing growth of CPRPs and the shortage of pharmacy faculty members, especially within divisions of pharmacy practice, community pharmacy residents may be ideal candidates for faculty recruitment.1,10 A recent survey indicated that 22% of CPRP residents in the 1999-2000 residency class accepted faculty positions post residency; among residents dating back to 1986, 35% were currently in faculty positions.12 To date, assessment of factors that influence community pharmacy residents to choose or not choose academic careers has not been documented in the literature. Thus, a study was planned to identify residents' interest in pursuing faculty positions, and to identify perceived and actual barriers to the pursuit of academic career paths. This information could provide insight into ways CPRPs can be structured in order to help address the pharmacy faculty shortage and meet the interests of community pharmacy residents, specifically those considering a career in academia. Additionally, colleges of pharmacy may find that this information will assist in their efforts to recruit CPRP residents for faculty positions.
The primary objectives of this study were to (1) evaluate CPRP residents' interest in faculty positions at the beginning of the residency and determine the percentage of CPRP residents accepting faculty positions post-residency, (2) identify factors that influence residents' decision to pursue or not to pursue a career in academia, and (3) compare demographics, program characteristics, and residents' experiences and preparedness in teaching, research, and clinical practice in those that pursued faculty positions versus those who did not. A secondary objective was to identify the characteristics that were most important to CPRP residents when selecting a position post-residency.
METHODS
The study was submitted to The Ohio State University Institutional Review Board and approved as exempt research. A list of CPRP directors and preceptors was obtained from APhA. CPRP residency directors and preceptors were contacted via e-mail to obtain the e-mail addresses of 2005-2006 CPRP residents. E-mail addresses were obtained for 53 residents, which were believed to be the majority of CPRP residents in the US based on APhA data (written communication, American Pharmacists Association, April 6, 2006).
Two original survey instruments were developed to collect the data necessary to meet the stated objectives. Survey questions were predominantly multiple-choice, yes/no, and Likert scale format. Additionally, space was given for free text comments. The survey was field-tested on hospital pharmacy residents at The Ohio State University (OSU) Medical Center. Feedback provided by the OSU Medical Center residents on the clarity of the questions and time required for completion was used to refine the survey instruments. The survey instruments were loaded into Zoomerang (www.zoomerang.com; MarketTools, Inc., San Francisco, Calif) an online survey tool and an invitation to participate in the survey was sent via e-mail to the 53 CPRP residents identified. The invitation included a brief explanation of the research project and a link to the survey instrument. Completion of one or both survey instruments served as consent to participate in the study; CPRP residents were informed that survey responses would be kept confidential and data would only be reported in aggregate. The preliminary and follow-up survey instruments were sent in October 2005 and June 2006, respectively, and residents were given approximately 2 weeks to complete each. Reminder e-mails were sent on day 8 and day 15 for the initial survey instrument and on day 8, day 12, and day 14 for the follow-up survey instrument. Questions pertaining to resident demographics, residency program characteristics, and residents' anticipated and actual experiences in teaching, research, and clinical practice were included on the survey instruments. Residents were asked to indicate job preferences, characteristics of the ideal job, and interest in academia on the preliminary survey instrument. The follow-up survey instrument focused on job selection, with specific questions regarding the pursuit of academic positions, characteristics of the positions accepted by residents, and perceived level of preparedness in teaching, research, and clinical practice. For the questions pertaining to job characteristics, residents could choose from a list of 12 job characteristics adapted from the Careers Pathway Evaluation Program.13
Survey results were downloaded from Zoomerang and exported to SPSS, version 14.0 (SPSS, Inc., Chicago, Ill) as a Microsoft Excel spreadsheet for statistical analyses. Survey instruments were coded so that respondents' preliminary and follow-up survey responses could be matched. Descriptive statistics (means, standard deviations, and percentages) were used to report residency experiences, job preferences and selections, ideal job characteristics, and factors influencing decisions to pursue or not to pursue faculty positions. Demographics, residency program characteristics, residents' experiences, and perceived level of preparedness of respondents who applied for faculty positions were compared with those of respondents who did not apply for faculty positions. Differences in continuous variables were analyzed using a t test and categorical variables were compared using Fischer's exact test.
RESULTS
Forty-five (85%) of the 53 CPRP residents initially identified completed the preliminary survey instrument between October 31, 2005, and November 14, 2005. The majority of respondents (n = 41; 91%) were female and their average age was 25.4 years (±2.3 years). Forty-five (100%) respondents indicated that they anticipated participating in some aspect of teaching during their residency. All respondents (100%) also indicated that they anticipated precepting pharmacy students during their residency. Other teaching experiences anticipated by 80% or more of respondents included lecturing/presenting to pharmacy students, healthcare professionals, or community members, and facilitating workshops, recitations, or laboratories. However, less than half anticipated receiving any formal training in teaching (n = 16; 36%) or precepting (n = 10; 22%); “formal training” was defined as participating in a continuing education or certificate program specific to the discipline. In addition, only 7 (16%) anticipated receiving any formal training in research during their residency.
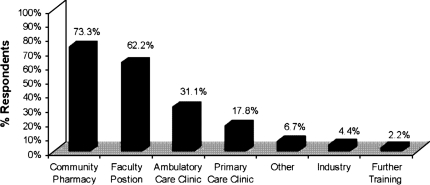
CPRP residents were asked to select (but not rank) their top 2 job preferences upon completion of their residency. Responses ranged from positions in community pharmacy to pursuing additional training (Figure 1). CPRP residents were also asked to rate their agreement with the following statement on a 5-point scale: “I am seriously considering a job/position in academia (ie, a faculty position) with a college of pharmacy upon completion of my residency,” (1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree). Sixteen respondents (36%) agreed or strongly agreed with this statement, while 19 (42%) were neutral and 10 (23%) disagreed or strongly disagreed. CPRP residents were also asked to indicate the top 3 characteristics of their ideal job. The ideal job characteristics listed most frequently by CPRP residents were flexibility (n = 23; 51%), variety of daily activities (n = 22; 49%), collaboration with other healthcare professionals (n = 22; 49%), and innovative/entrepreneurial environment (n = 18; 40%).
Figure 1.
Results of preliminary survey of pharmacists' job preference upon completion of a community pharmacy residency (n = 45). Respondents were asked to select their top 2 preferences.
Forty of the 53 CPRP residents (75%) completed the follow-up survey instrument in June 2006. In accordance with their expectations, all respondents indicated they had participated in some form of teaching during their residency. Thirty-seven (93%) had precepted pharmacy students, 36 (90%) had lectured to pharmacy students, 32 (80%) had presented to healthcare professionals and community members, and 36 (90%) had facilitated workshops, recitations, or laboratories. Only 14 (35%) had participated in a formal training program in teaching. All of those who had not participated in a formal training program in teaching indicated the reason was because they were not given the opportunity rather than they chose not to participate. Thirteen (33%) had the opportunity to participate in a formal training program in precepting but only 9 (23%) actually did so. Only 7 (18%) resident had the opportunity to participate in a formal training program in research and all 7 did so.
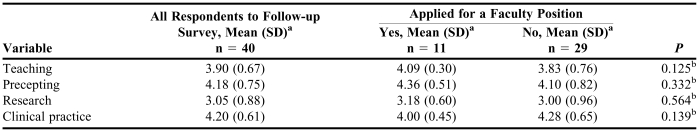
CPRP residents were asked to rate on a 5-point scale how prepared they felt at the end of their residency to successfully perform in the following areas: teaching, precepting, research, and clinical practice (Table 1). Overall, research was the area that most respondents (n = 7; 18%) indicated feeling unprepared or very unprepared for at the end of their residency.
Table 1.
Community Pharmacy Residents' Perceived Level of Preparedness
aLikert Scale 1 = very unprepared, 2 = unprepared, 3 = neutral, 4 = prepared, 5 = very prepared
bDetermined by t test
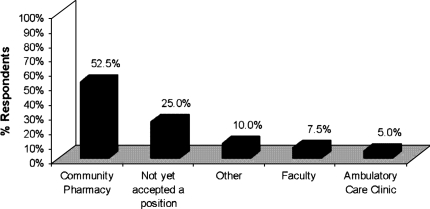
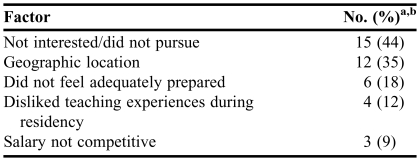
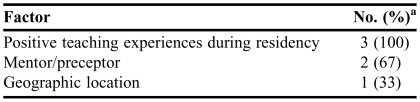
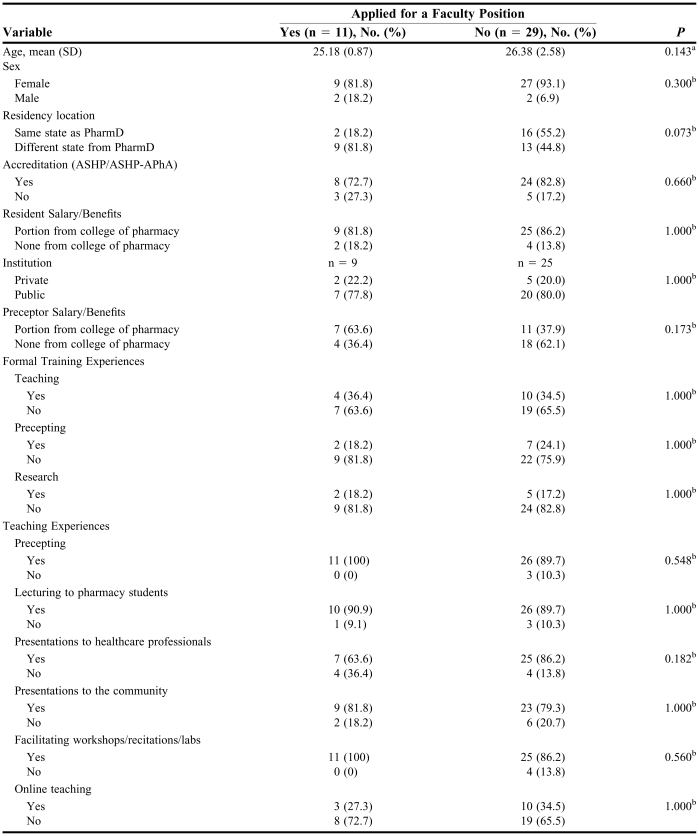
The majority of respondents (n = 21; 52.5%) accepted a position in community pharmacy practice upon completion of their residency, while one fourth of respondents (n = 10; 25%) had not accepted any position by the time the follow-up survey instrument was completed (Figure 2). Eleven (28%) respondents had applied for a faculty position: 3 had accepted a faculty position, 3 were still awaiting interviews or offers, 2 turned down a position, 2 were not offered a position, and 1 withdrew his/her application. Of those respondents who did not apply for or accept a faculty position, the reasons ranged from a lack of interest to the salary not being competitive (Table 2). Of the 3 residents who accepted faculty positions, all indicated that positive teaching experiences during their residency program were influential in making their decision and 2 indicated mentorship as a positive influence (Table 3).
Figure 2.
Positions accepted by respondents completing the second survey (n = 40).
Table 2.
Factors Influencing Community Pharmacy Residents' Decisions Not to Apply for/Accept a Faculty Position (n = 34)
aN includes 29 respondents who did not apply for faculty positions and 5 respondents who applied but did not accept or receive a faculty position offer
bRespondents could indicate more than one response
Table 3.
Factors Influencing Community Pharmacy Residents' Decisions to Accept a Faculty Position (N = 3)
aRespondents could indicate more than one response
Demographics, residency program characteristics, and residents' experiences in teaching and formal training programs did not differ significantly between the residents who pursued a faculty position and those who did not (Table 4). Likewise, no significant difference was found between those respondents who applied for a faculty position and those who did not with respect to level of preparedness in any area (Table 1); however, some trends were observed. The average perceived level of preparedness in teaching for those who applied for a faculty position versus those who did not was 4.09 (±0.30) and 3.83 (±0.76), respectively (p = 0.125). Of the 11 residents who applied for a faculty position, 9 (82%) had relocated to complete their residency, while only 13 of the 29 who did not apply for a faculty position (45%) had relocated (p = 0.073). Seven (64%) of those who applied for a faculty position had a preceptor who received a portion of his/her salary/benefits from a college of pharmacy compared to only 11 (38%) of those who did not apply for a faculty position (p = 0.173).
Table 4.
Follow-up Survey Demographics, Residency Program Characteristics, and Teaching and Formal Training Experiences by Application for Faculty Position
aDetermined by t test;
bDetermined by Fischer's exact test
CPRP residents were asked to indicate the 3 most important characteristics of the job they accepted. Residents could choose from the same 12 characteristics listed on the preliminary survey instrument. For those respondents who had accepted a postresidency position (n = 29), the job characteristics listed most frequently were flexibility (n = 17; 59%), variety of daily activities (n = 16; 55%), collaboration with other healthcare professionals (n = 13; 45%), and innovative/entrepreneurial environment (n = 11, 38%). These characteristics did not change over the survey period (approximately 7 months) from what the residents indicated they were looking for in their ideal job early in their residency training.
DISCUSSION
Our findings show that a majority of 2005-2006 CPRP residents had an interest in faculty positions during the beginning of their residency; however, this did not result in a significant number pursuing and/or accepting faculty positions. Compared to the study of current/former community pharmacy residents conducted by Unterwagner et al in 2000, our study showed that a smaller percentage of CPRP residents went into faculty positions immediately upon completion of residency: 4 of 18 (22%) in the previous study versus 3 of 40 (7.5%) in our study.12 Although, a larger percentage of residents in our study had not accepted a position at the time of survey completion—10 of 40 (25%) in our study versus 3 of 18 (17%) in the previous study—3 residents in our study were still awaiting interviews or offers for faculty positions. Despite the growth in CPRPs, our results do not show an increase in the number of community pharmacy residents accepting faculty positions. From our follow-up survey instrument, we found that a lack of interest and preparedness were among the most commonly listed barriers to pursuing an academic position. The 2007 Required and Elective Educational Outcomes, Goals, Objectives and Instructional Objectives for Postgraduate Year One (PGY1) Community Pharmacy Residency Programs includes an elective educational outcome focused on demonstrating skills required to function in an academic setting.14 CPRPs and affiliated colleges of pharmacy should consider including this as a required residency educational outcome to increase CPRP residents' interest and preparedness in academia and encourage the pursuit of faculty positions.
In AACP's 2004-2005 survey of Vacant Budgeted and Lost Faculty Positions colleges of pharmacy indicated not enough qualified candidates (55.7%), budget limitations (18.5%), and geographic location (11.7%) as the top 3 reasons for vacant faculty positions.1 Preference for geographic location is clearly a factor in filling academic positions as noted both by CPRP residents and colleges of pharmacy. Thirty-five percent of 2005-2006 CPRP residents indicated geographic location as a reason for not pursuing or accepting a faculty position, which is higher than that listed by colleges of pharmacy. This may be because colleges of pharmacy are not aware of potential candidates who do not apply for open faculty positions in a nonpreferred geographic location. Colleges of pharmacy indicated that over 18% of faculty positions remained vacant due to budget limitations/inability to offer competitive salary, yet only 9% of CPRP residents listed this as a limiting factor.
Positive teaching experiences and mentorship were indicated as influential factors in residents' decisions to pursue academic positions. This study clearly identified that CPRP residents' have a broad range of teaching experiences during their residency, yet few had formal training. Teaching certificate programs, seminars, and roundtables should be considered not only to prepare residents for these teaching experiences, but to enhance these experiences and foster relationships between faculty members and residents in order to promote residents' interest in academia. Including these types of programs within CPRPs may also increase residents' perceived level of preparedness in teaching. While not significant, our study results showed a trend: CPRP residents who did not apply for faculty positions reported a lower perceived level of preparedness in this area compared to those who did apply. Another consideration is that increasing preparedness in teaching may increase overall preparedness, which was identified as a barrier to the pursuit of academic positions. An article published in the Journal in 2004 describes a teaching seminar series developed by a faculty member at Massachusetts College of Pharmacy and Health Services for pharmacy residents. According to the article, not only did the program receive positive evaluations from the residents, but 26% of participants accepted full-time faculty positions, while another 26% accepted clinical pharmacy positions with an adjunct academic appointment.15 No significant relationship was found between those who pursued a faculty position and those who participated in a teaching certificate program in our study; however our study was limited to a small population of CPRP residents. In addition, these types of programs can benefit all CPRP residents regardless of their career path as patient and healthcare provider education is a large part of contemporary community pharmacy practice.
Of those residents who applied for faculty positions, a larger percentage relocated for their residency compared to those who did not apply for faculty positions (82% vs. 45%). These residents may have been more inclined to apply for a faculty position because they were willing to relocate again for a job as they had for the residency program. Further research is needed to evaluate the association between residents' willingness to relocate and their decision to pursue a faculty position. Also, a larger percentage of those who applied for faculty positions had a preceptor who received salary/benefits from a college of pharmacy compared to those who did not apply (64% vs. 38%). This trend suggests that a preceptor's affiliation with a college of pharmacy may encourage their resident(s) to pursue a faculty position — a consideration further supported by our finding that mentors/preceptors are influential to those that accept faculty positions. Those residents who applied for faculty positions tended to rate themselves as feeling more prepared in teaching than those who did not apply (4.09 ± 0.30 versus 3.83 ± 0.76; p = 0.125); thus, reinforcing the need to enhance residents' teaching experiences. Also, those who did not apply for faculty positions ranked themselves as feeling most prepared in clinical practice compared to teaching, precepting, and research, which may explain why they chose clinical positions over academic positions.
Overall, residents felt least prepared in research skills, another important component for success in academia. This result is consistent with our finding that few residents received any formal training in the area of research. CPRPs should focus more attention on developing research skills and incorporating research training as this is an important aspect of pharmacy practice whether in an academic or clinical position. As with the educational outcome related to academia, the educational outcome related to research is an elective outcome in the Community Pharmacy Residency Standard.14 CPRPs should strongly consider making this a required educational outcome. In addition, CPRPs should consider the incorporation of research training or mentoring programs as this is a needed area of development for future pharmacy practice faculty members. Junior pharmacy faculty members have reportedly felt least satisfied in the area of research skills, with contributing factors being insufficient release time offered by the institution for research and lack of technical and data analysis assistance.16 In addition, orientation activities related to research/scholarship are reportedly lacking for first-year pharmacy practice faculty members and are where the most guidance is desired.17 Current literature shows that research workshops, seminars, and rotations have been incorporated into a variety of medical residency programs with positive results, such as increased numbers of national presentations and recognition, peer-reviewed publications, and competitiveness for fellowship, faculty, and leadership positions.18-21 Although the programs differed in length and scope, most incorporated training or participation in several of the following aspects: journal club, research methods and design, statistical analysis, grant writing, IRB approval, presentation skills, manuscript development, and faculty mentoring. CPRPs can use the experience of medical residency programs to design similar programs for pharmacy residents.
Although interest in faculty positions at the beginning of residency did not reflect pursuit of faculty positions at the end of residency, job characteristics that were important to CPRP residents did remain consistent. Colleges of pharmacy should consider promoting/advertising faculty positions, especially community or ambulatory care-focused positions, by emphasizing those aspects of the position that are most appealing to CPRP residents. For example, rewards of a faculty position include flexibility and “a wide variety of diverse activities and responsibilities,” both of which were highly regarded among CPRP residents.22 Highlighting these rewards/benefits of a faculty position may help offset less competitive salaries, a barrier identified by both CPRP residents and colleges of pharmacy. As our study indicates, a large percentage of CPRP residents are interested in academia at the beginning of their residency, though many do not pursue this path later in the year. Colleges of pharmacy may view this as an opportunity to develop programs that increase CPRP residents' exposure to academia as well as increase their level of preparedness. For instance, The Ohio State University College of Pharmacy has developed a PGY-2 Academic Practice Residency for residents with an interest in academia and community or ambulatory care. With the growing trend in distance education, colleges of pharmacy may also consider creating or restructuring vacant positions to accommodate the geographic location of qualified candidates, another barrier identified by both residents and colleges.
Although we were able to identify and engage a vast majority of the population (written communication, American Pharmacists Association, April 6, 2006) our study was limited to the perceptions and individual experiences of residents in a CPRP. In addition to CPRP residents, residents and fellows from ambulatory and institutional practice are also potential faculty candidates; therefore, future research with this population should be considered to evaluate perceptions and experiences of pharmacy residents and fellows in various practice settings.
CONCLUSION
Many CPRP residents are interested in pursuing faculty positions early in their residency, yet many do not apply for faculty positions and only a small number accept faculty positions by the end of their residency. CPRP directors and preceptors should incorporate the elective residency educational outcome for developing skills in academic practice within the residency curriculum. Methods for incorporation can include strategies that create positive teaching experiences for residents as well as provide one-on-one mentorship as our study suggests that these are influential factors in the pursuit of faculty positions. CPRPs should consider the development or enhancement of teaching and research training and mentorship programs as well as development of specialized or postresidency opportunities for future faculty development. With the expansion of direct patient care opportunities in community pharmacy and the need for advanced pharmacy practice experiences and residency sites, colleges of pharmacy should partner with CPRPs to foster resident's interest in academia and pursue CPRP graduates as qualified candidates for community pharmacy faculty positions.
REFERENCES
- 1.Vacant budgeted and lost faculty positions – academic year 2004-2005. AACP Institutional Research Brief Volume 6. Available at: http://www.aacp.org/site/pdf.asp?TP=/Docs/MainNavigation/InstitutionalData/7309_IRBNo6-Facultyvacancies.pdf Accessed July 19, 2007.
- 2.AACP COD-COF faculty recruitment and retention committee final report. June 2004. Available at: http://www.aacp.org/Docs/AACPFunctions/Governance/6212_FacultyRecruitRetentionCommReportJune142004.pdf Accessed July 19, 2007.
- 3.Lee ML, Bennett M, Chase P, et al. Final report and recommendations of the 2002 AACP task force on the role of colleges and schools in residency training. Am J Pharm Educ. 2004;68(1) Article S02. [Google Scholar]
- 4.Romanelli F, Smith KM, Brandt BF. Certificate program in teaching for pharmacy residents. Am J Health-Syst Pharm. 2001;58:896–8. doi: 10.1093/ajhp/58.10.896. [DOI] [PubMed] [Google Scholar]
- 5.Romanelli F, Smith KM, Brandt BF. Teaching residents how to teach: a scholarship of teaching and learning certificate program (STLC) for pharmacy residents. Am J Pharm Educ. 2005;69(2) Article 20. [Google Scholar]
- 6.Castellani V, Haber SL, Ellis SC. Evaluation of a teaching certificate program for pharmacy residents. Am J Health-Syst Pharm. 2003;60:1037–41. doi: 10.1093/ajhp/60.10.1037. [DOI] [PubMed] [Google Scholar]
- 7.Occupational Outlook Handbook, U.S. Department of Labor, Bureau of Labor Statistics. Available at: http://www.bls.gov/oco/ocos079.htm. Accessed July 19, 2007.
- 8.Medicare Prescription Drug, Improvement, and Modernization Act of 2003. H.R.1. Available at: http://www.cms.hhs.gov/EmplUnionPlanSponsorInfo/downloads/hr1.pdf. Accessed August 10, 2007.
- 9.Accreditation Standards and Guidelines for the Professional Program in Pharmacy leading to the Doctor of Pharmacy Degree. January 2006. Available at: http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed August 2, 2007.
- 10.Jacknowitz AI, Belsey MA. Joint college of pharmacy-community pharmacy residencies. Am J Pharm Educ. 2004;68(4) Article 97. [Google Scholar]
- 11.Murphy JE, Nappi JM, Bosso JA, et al. ACCP Position Statement. American College of Clinical Pharmacy's vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;26:722–33. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]
- 12.Unterwagner WL, Zeolla MM, Burns AL. Training experiences of current and former community pharmacy residents, 1986-2000. J Am Pharm Assoc. 2003;43:201–5. doi: 10.1331/108658003321480740. [DOI] [PubMed] [Google Scholar]
- 13.Schommer JC, Brown LM, Millonig MK, et al. Career Pathways Evaluation Program: 2002 Pharmacist Profile Survey. Am J Pharm Educ. 2003;67(3) doi: 10.5688/ajpe7480. Article 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Required and elective educational outcomes, goals, objectives, and instructional objectives for Postgraduate Year One (PGY1) Community Pharmacy Residency Standard. Available at: http://www.ashp.org/s_ashp/docs/files/accreditation/RTP_CommunityCareGoalsObj071107.doc. Accessed July 19, 2007.
- 15.Sylvia LM. Mentoring prospective pharmacy practice faculty: a seminar series on teaching for pharmacy residents. Am J Pharm Educ. 2004;68(2) Article 38. [Google Scholar]
- 16.Latif DA, Grillo JA. Satisfaction of junior faculty with academic role functions. Am J Pharm Educ. 2001;65:137–43. [Google Scholar]
- 17.Glover ML, Armayor GM. Expectations and orientation activities of first-year pharmacy practice faculty. Am J Pharm Educ. 2004;68(4) Article 87. [Google Scholar]
- 18.Neale AV, Pieper D, Hammel E. A consortium-based research education program for residents. Acad Med. 2000;75:298–301. doi: 10.1097/00001888-200003000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Chung R, Diaz J, Li P. A method of teaching clinical research in a community hospital residency program. The Am J Surgery. 1999;177:83–5. doi: 10.1016/s0002-9610(98)00295-5. [DOI] [PubMed] [Google Scholar]
- 20.Gay SB, Hillman BJ. Evaluation of a mandatory radiology resident research rotation. Acad Radiol. 2000;7:172–5. doi: 10.1016/s1076-6332(00)80119-1. [DOI] [PubMed] [Google Scholar]
- 21.Byrnes AB, McCormack FX, Diers T, Jazieh AR. The Resident Scholar Program: A research training opportunity for internal medicine house staff. J Cancer Educ. 2007;22:47–9. doi: 10.1007/BF03174375. [DOI] [PubMed] [Google Scholar]
- 22.Draugalis JR, DiPiro JT, Zeolla MM, Schwinghammer TL. A Career in Academic Pharmacy: Opportunities, Challenges, and Rewards. Am J Pharm Educ. 2006;70(1) doi: 10.5688/aj700117. Article 17. [DOI] [PMC free article] [PubMed] [Google Scholar]