Abstract
Objective
To determine the extent of experience or exposure pharmacy residency candidates had in various areas of hospital pharmacy practice and to identify any candidate-specific variables that correlated with a larger extent of experience.
Methods
Over a 3-year period, a self-assessment survey instrument was administered to 116 postgraduate first-year (PGY1) pharmacy practice residency candidates to evaluate their extent of experience within various areas of hospital pharmacy practice such as patient care activities, drug information, and drug distribution/control.
Results
The residency candidates reported the greatest amount of experience in patient counseling, working with pharmacy databases, taking medication histories, pharmacokinetics, and outpatient dispensing procedures. They had less experience with medical emergencies, parenteral nutrition, and intravenous admixture techniques. Overall, there was no correlation between class rank, advanced pharmacy practice experiences, geographic region, or year of interview and the extent of candidates' experience in any specific area of pharmacy.
Conclusion
PGY1 residency candidates in this sample reported minimal experience in areas necessary for hospital pharmacy practice and this suggests possible deficiencies in the PharmD curriculum. PGY1 residency programs in acute care settings should recognize these educational deficits and assure that residents have exposure to and develop proficiency in critical areas such as medical emergencies, parenteral nutrition, and intravenous admixture techniques.
Keywords: pharmacy practice, residency, assessment, survey
INTRODUCTION
The role of the pharmacist is evolving to include more participation in and responsibilities for patient care-related activities. A recent publication of the Joint Commission of Pharmacy Practitioners (JCPP) proposed a vision of the profession such that “pharmacists will have the authority and autonomy to manage medication therapy and will be accountable for patients' therapeutic outcomes.”1,2 In anticipation of these proposed changes, the Accreditation Council for Pharmacy Education (ACPE) modified accreditation standards to reflect that the sole professional degree to be issued after 2005 would be the doctorate of pharmacy (PharmD). With the introduction of the first professional PharmD degree, the American Association of Colleges of Pharmacy (AACP) revised the Center for the Advancement of Pharmaceutical Education (CAPE) Educational Outcomes to assure that colleges of pharmacy maintain educational content consistent with pharmacists' evolving roles.3 The updated CAPE Educational Outcomes outline a vision of pharmacy curriculum to produce graduates who are able to “provide pharmaceutical care in cooperation with patients, prescribers, and other members of an interprofessional health care team based upon sound therapeutic principles and evidence-based data.”3 Despite these changes to curricula, the higher clinical demands placed upon pharmacists may exceed the education provided by colleges of pharmacy. Therefore, postgraduate residency training will likely play a larger role in pharmacy education as the responsibilities of pharmacists continue to evolve. Residencies can provide more extensive training in one particular area of pharmacy (eg, community or institutional setting) and prepare graduates for additional clinical responsibilities.4 This approach is supported by the American College of Clinical Pharmacy (ACCP), which maintains the vision that the completion of an accredited residency program will become a prerequisite for all pharmacists who provide direct patient care by the year 2020.5
The Medical University of South Carolina (MUSC) Medical Center and South Carolina College of Pharmacy's PGY1 Pharmacy Practice Residency program consists of 6 to 8 resident positions annually. Approximately 40 candidates from around the country interview for a residency position each year. During the interview, candidates are asked to complete a self-assessment survey instrument to determine the potential needs of the incoming residency class and identify areas to improve residency education opportunities. Because of the exposure to a large group of students from around the nation, self-assessment survey data were reviewed to determine the average amount of experience candidates reported within various areas of pharmacy practice. In addition, certain variables, such as class rank, clinical rotation experience, year of interview, and geographical region, were evaluated to determine whether significant differences existed between these variables and the extent of experience reported by the candidates.
METHODS
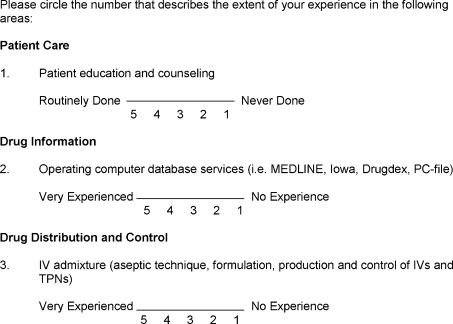
A 12-question self-assessment survey instrument was administered to PGY1 pharmacy practice residency candidates during onsite interviews from 2003 to 2005. Based on a 5-point Likert scale, the survey instrument assessed the extent of experience reported by the applicants within certain areas of general hospital practice, including patient care activities, drug information, and drug distribution/control (Figure 1). Candidates were informed that the survey results would not be reviewed prior to the residency match and would therefore have no impact on their ranking. Study design was reviewed and Institutional Review Board approval was obtained. The median score was evaluated for each of the activities included on the survey instrument. In addition, correlation statistics were performed with the candidates' self-reported level of experience and class rank, clinical rotation experience, year of interview, and geographical region. A series of ANOVA analyses were conducted between the variables. All statistical analyses were performed using StataTM statistical software (Stata Corporation, College Station, TX).
Figure 1.
Examples of questions on a self-assessment survey instrument given to pharmacy residents.
RESULTS
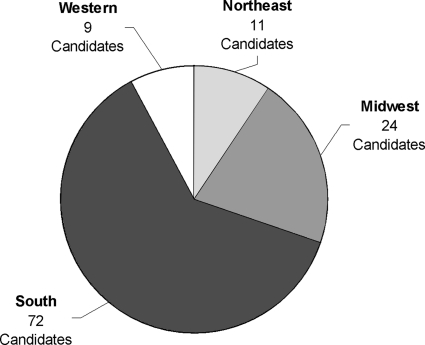
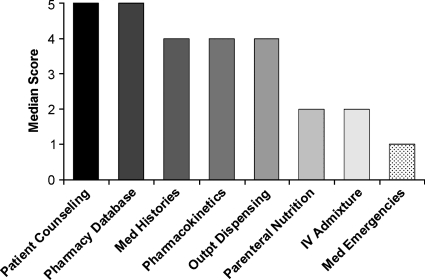
One hundred sixteen candidates from forty-one colleges of pharmacy completed the survey instrument from calendar years 2003 to 2005. The majority of candidates (n = 72, 62%) were from colleges of pharmacy in the southern United States (Figure 2). Results of the applicants' self-reported level of experience are summarized in Figure 3. Candidates described a greater amount of experience in patient counseling (median = 5), pharmacy databases (median = 5), medication histories (median = 4), pharmacokinetics (median = 4), and outpatient dispensing procedures (median = 4). Less experience was noted with participation in medical emergencies (median = 1.5), parenteral nutrition assessments (median = 2), and intravenous (IV) admixture techniques (median = 2). Overall, there was no correlation of class rank, clinical rotation experience, geographic region, or year of interview with the extent of experience reported in any topic area.
Figure 2.
College of Pharmacy Geographic Distribution.
Figure 3.
Applicants' Self-Reported Level of Experience.
DISCUSSION
Although colleges of pharmacy across the country have made curricula improvements in order to encompass more clinical activities, there are still many areas of pharmacy practice that may not be adequately covered. The results of this study suggest that PGY1 residency candidates from a variety of colleges across the country describe having the least exposure to medical emergencies, parenteral nutrition, and intravenous (IV) admixture. Proficiency in such areas is a general requirement for most hospital pharmacists. Therefore, pharmacy students interested in hospital pharmacy practice should consider an American Society of Health-System Pharmacists (ASHP)-accredited acute care residency program in order to increase their exposure to these areas.
As pharmacists' roles evolve to include more participation in and responsibility for direct patient care, residency training will likely become a vital part of pharmacy education. Therefore, residency programs should review their goals and outcomes to ensure graduates receive the training necessary to meet the growing demands of health systems and their patients. In particular, the survey results suggest that acute care PGY1 residency programs should make certain that residents are provided with sufficient exposure to medical emergencies, parenteral nutrition, and IV admixture techniques.
At MUSC, improvements have been made in order to increase PGY1 residents' exposure in these recognized areas of deficiency. Advanced cardiac life support (ACLS) certification continues to be a requirement for all residents. In addition, periodic “mock-code” sessions have been created. These sessions allow residents to prepare medications often required during code situations. Furthermore, a parenteral nutrition competency program has been designed for residents to complete during orientation. This program consists of a Web-based module reviewing important issues related to nutrition in both pediatric and adult patients. Upon completion of the module, residents are required to write parenteral nutrition orders for sample cases encompassing both age groups, which are then evaluated by pharmacy nutrition specialists. Incorrect cases are reviewed with residents and are required to be rewritten. Residents need to correctly complete all cases before the end of orientation. Finally, PGY1 resident operations experiences were expanded to include a central pharmacy-dispensing and IV preparation component. Historically, PGY1 residents completed 16 hours per month of operations requirements in a decentralized, clinically oriented environment. Eight hours per month of working in a centralized environment were added to this requirement.
Although many needed improvements have been made as a result of the survey results, shortcomings must be recognized. Most importantly, although candidates were informed that the results of this survey had no bearing upon ranking for residency, reporting bias may have still occurred if candidates felt the need to embellish their experience in an effort to appear more competitive. Also, selection bias may have occurred as only applicants from one residency program were surveyed. It should also be recognized that this survey only examined the amount of exposure candidates had in various areas rather than the overall quality of their experiences.
Based on the results of this study, it could be hypothesized that pharmacy schools may not be able to keep pace with the growing responsibilities afforded to pharmacists today. The typical pharmacy curriculum requires close to 20 credit hours of graduate-level courses each semester. This does not leave much time for incorporating new courses in order to increase exposure to medical emergencies, parenteral nutrition, and IV admixture techniques. As a result, students may only be exposed to these areas of pharmacy practice during experiential rotations and to varying degrees depending on preceptor and site availability. In areas where didactic exposure is minimal, improved preceptor and rotation site development are essential to ensure quality experiences. Given the challenges of identifying and developing quality experiences for a growing number of students, perhaps it is not the duty of pharmacy schools to improve education in these areas of deficiency, but rather that of residency programs. Acute care PGY1 residency programs should recognize these current deficits in pharmacy education and take measures to increase residents' exposure to these areas.
CONCLUSIONS
Pharmacy school curricula may not provide sufficient exposure to several areas of hospital pharmacy practice. Acute care PGY 1 residency programs should increase resident exposure to and ensure competency in medical emergencies, parenteral nutrition, and IV admixture.
ACKNOWLEDGEMENTS
The authors would like to acknowledge Elinor Chumney, PhD, and the MUSC Medical Center and South Carolina College of Pharmacy Residency Committee for their assistance with this project.
The results of this study were presented at the 2005 American College of Clinical Pharmacy Annual Meeting in San Francisco, Calif, and documented in Pharmacotherapy 2005;25:1525 (Abstract 416).
REFERENCES
- 1.American Council on Pharmaceutical Education. Accreditation standards and guidelines. Available from http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf Accessed May 23, 2006.
- 2.Miller WA. Changing the structure of pharmaceutical education to require doctor of pharmacy and postgraduate residency education and training. Pharmacotherapy. 2006;26:587–93. doi: 10.1592/phco.26.5.587. [DOI] [PubMed] [Google Scholar]
- 3.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education Educational Outcomes 2004. Available from http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf Accessed June 21, 2006.
- 4.American Society of Health-System Pharmacists. Pharmacy Residency (PGY1) Educational Goals and Objectives. Available from http://www.ashp.org/rtp/starting/specialized-residencies.cfm?cfid=20443899&CFToken=61557055 Accessed June 21, 2006.
- 5.Murphy JE, Nappi JM, Bosso JA, Saseen JJ, Hemstreet BA, et al. American College of Clinical Pharmacy's vision of the future: postgraduate pharmacy residency training as a prerequisite for direct patient care practice. Pharmacotherapy. 2006;26:722–33. doi: 10.1592/phco.26.5.722. [DOI] [PubMed] [Google Scholar]