Abstract
Objective
To evaluate the curricula content of Thai pharmacy schools based on the Thai pharmacy competency standards.
Methods
Course syllabi were collected from 11 pharmacy schools. A questionnaire was developed based on the Thai pharmacy competency standards. Course coordinators completed the questionnaire assessing the curricula content.
Results
The curricula for both the bachelor of science in pharmacy degree (BS Pharm) and doctor of pharmacy (PharmD) degree programs included the minimum content required by the 8 competency domains. The dominant content area in BS Pharm degree programs was product-oriented material. The content ratio of patient to product to social and administrative pharmacy in the BS Pharm degree programs was 2:3:1, respectively. However, the content ratio suggested by the Thai Pharmacy Council was 3:2:1, respectively. For the PharmD programs, the largest content area was patient-oriented material, which was in agreement with the framework suggested by the Thai Pharmacy Council.
Conclusions
The curricula of all Thai pharmacy schools met the competency standards; however, some patient-oriented material should be expanded and some product-oriented content deleted in order to meet the recommended content ratio.
Keywords: pharmacy education, curriculum, competency, evaluation, Thailand
INTRODUCTION
Pharmacy education in Thailand has undergone many changes in the past 90 years.1 The first phase of pharmacy education was from 1914-1935, during which all students studied 3 years to receive a certificate of pharmaceutical production. Pharmacy education expanded to a 4-year program in 1941, and then to a 5-year bachelor's degree program in pharmacy in 1957. Many courses were added to the 4- and 5-year curricula, especially addressing subjects that supported pharmacists working in settings other than hospitals. Currently, another transition in pharmacy education is occurring in Thailand. Several Thai pharmacy schools have recently expanded to a 6-year doctor of pharmacy curriculum (PharmD).
Many factors have influenced these changes in pharmacy curricula.2,3 One crucial factor has been the Thai society's increasing need for pharmaceutical products and services. Changes in the health care system have also influenced these changes in health care needs. Thai schools of pharmacy have revised their curricula in order to produce highly educated pharmacists to meet the health care needs of patients and society.
In addition, there is interest by many pharmacy schools globally in moving pharmacy curricula toward more patient-oriented content, as well as interest in professional collaboration among countries. The US-Thai Consortium was originally formed in 1993 between all Thai schools of pharmacy, the American Association of Colleges of Pharmacy, and 10 US colleges of pharmacy (University of Florida, Purdue University, Ohio State University, University of Wisconsin, University of Arizona, University of Minnesota, University of Illinois at Chicago, University of Maryland at Baltimore, University of North Carolina, and Rutgers University). The consortium has resulted in an exchange of many students and faculty and has created a strong bond between Thai and US pharmacy faculty members.
In many countries, national governments and/or pharmacy professional organizations have developed competency standards or guidelines which pharmacy students must meet before entering professional practice.4-8 In 2002, the Thai Pharmacy Council established their first competency standards with the goal that new pharmacy graduates will know how to apply the knowledge and skills they have attained during pharmacy school. Currently, all Thai pharmacy graduates from either the 5-year bachelor's degree or 6-year PharmD degree have to take the same licensure examination, which is based on the Thai competency standards. These standards contain 8 domains, 40 competencies, and 71 subcompetencies.9 These standards are not only used as a basis for the pharmacy licensure examination, but Thai schools of pharmacy use them to base curricula changes and existing pharmacists use them as guidelines for maintaining their standards of practice. In order for pharmacy schools to ensure their graduates possess the required skills to practice and to respond to new competency standards, it is important for schools to have ongoing educational curricula evaluations10 to examine their educational processes and outcomes, focus attention on meeting more global societal needs for services by pharmacists, and provide feedback for their instructional processes.11 In addition, the results of curricula evaluations will hopefully guide schools to more appropriately modify their curricula. Curricula evaluations may occur with an individual course assessment, within broader school or institutional changes, and within more global changes at a national level.10 For example, Assemi and colleagues implemented a cultural competency-training course in their curriculum. Subsequently, the authors surveyed students' awareness, knowledge, and skills to evaluate the course outcomes.12 In contrast, Kirkpatrick and Pugh conducted an overall evaluation of curricula competency outcomes at Virginia Commonwealth University. The researchers assessed curriculum content to ensure that all desired curricula outcomes were included, no outcomes were unreasonably duplicated, and there were no omissions in the curriculum content.13 Additionally, the Accreditation Council on Pharmaceutical Education (ACPE) released its revised competency standards and guidelines, which require colleges and schools of pharmacy in the United States to evaluate their educational outcomes for accreditation.14
In Thailand, curricula evaluations have been routinely conducted at the individual course and institutional levels. Currently, there have been no Thai studies that have assessed and compared the Thai pharmacy curricula with pharmacy competency standards created by the Thai Pharmacy Council. Therefore, the purpose of this study was to evaluate the undergraduate core curricula content of all 12 Thai pharmacy schools based on the Thai pharmacy competency standards, and compare the curricula content between the bachelor's degree and PharmD degree programs.
METHODS
This study assessed the curricula content of all core (ie, required) courses from each pharmacy school in Thailand using a written questionnaire that was distributed to course coordinators. The pharmacy competency standards (http://www.pharm.su.ac.th/prof/thai_competency.pdf) established and approved by the Thai Pharmacy Council in 2002 were reviewed and a draft questionnaire was developed for respondents to indicate which competencies were addressed in their courses.
The next step involved having the content validity of the questionnaire tested by experts. Researchers identified courses that had 2 course coordinators at Silpakorn University. The pilot test of the draft questionnaire was completed by 10 pharmacy faculty members. One coordinator of a course was invited to participate in the pilot test. For completion of the final questionnaire, the second course coordinator was invited to participate. The pilot test assessed the clarity of wording and content of the cover letter, instructions, and questions. The questionnaire was then modified based on feedback from the pilot test. The final questionnaire (written in Thai) was 16 pages in length, containing 2 pages with a cover letter and instructions and 14 pages of competency statements.
The 14 pages contained 71 competency statements that covered 8 domains and 40 competencies. The following 3 questions were asked about each competency statement:
A. Do you teach this competency statement in your class? If yes, please continue to questions B and C.
B. How do you teach this competency statement to your students? Please check all teaching methods used in your class.
C. Please specify the amount of time spent on teaching the competency statement.
In addition, descriptive course-related information was requested. This information included the subject code, subject title, type of curriculum, number of subject credits, the year the material was taught, and the name of the school where it was taught. At the end of the questionnaire, there was a question asking the course coordinator to specify other content not covered in the competency statements that was included in their course.
All 12 Thai pharmacy schools were officially contacted in writing by the researchers and requested to participate in the study. In addition, each school was requested to provide their current pharmacy curriculum document and all of their required course syllabi for the 2004-2005 academic year. Criteria for including courses in the analysis were: (1) that the course was a required pharmacy course; and (2) reflected the latest curricula taught during the 2004-2005 academic year.
Data regarding the pharmacy practice experiential courses were excluded from this analysis. The experiential course requirements could be met by a diverse range of practice sites including hospitals, community pharmacies, the Thai Food and Drug Administration, and a pharmaceutical manufacturer, and covered a range of domains.
The cover letter and questionnaire were mailed to the associate dean of academic affairs at each school of pharmacy. The associate deans were then requested to distribute the cover letter and questionnaire to each of the required course coordinators. Two to 4 weeks after the questionnaires were distributed, a researcher visited each school to collect the questionnaires. The researcher reviewed the course content from each course syllabus to determine which competencies were currently being met and compared those data to the questionnaires received from the course coordinators.
If needed, the researchers contacted the course coordinators to clarify their responses and discuss any course content issues. A new questionnaire and a stamped return envelope were provided to nonrespondents during the site visits. Two weeks after visiting a school, nonrespondents were sent an electronic mail message or received a telephone call requesting that the questionnaire be completed and mailed to the researchers. If a completed questionnaire was not received from a faculty member, the researcher reviewed the course syllabus and estimated which competencies were met based on the faculty member's syllabus listing the course content. A Microsoft Excel spreadsheet was developed to summarize the data collected from each course at all participating Thai pharmacy schools.
The collected course content data were analyzed to determine which Thai competency standards were met by which courses. From the completed questionnaires, the time devoted to each competency statement was converted into credit hour units (1 credit hour unit was equivalent to 15 hours). Afterward, total credit hours spent for each school were summed within the 8 competency domains. The curricula content, which was not covered in 8 domains, were classified into the domain “others”. The competency domains are shown in Table 1. With the 71 subcompetencies and domain “others,” competency statements were categorized into 3 areas: patient-oriented, product-oriented, and social and administrative pharmacy (SAP)-oriented areas. The total competency credits for each school were categorized into the 3 subject-oriented areas. The data were analyzed using SPSS statistical software, version 11.5. A p value < 0.05 was used for all analyses to determine statistical significance. Descriptive statistics including the mode, mean, standard deviation, outliers, and percentage were calculated for demographic variables and competency coverage.
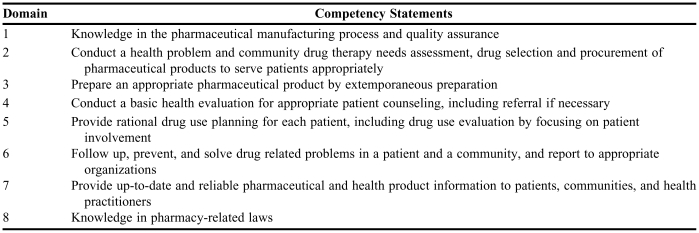
Table 1.
Thai Pharmacy Competency Guidelines For Licensure Examination
RESULTS
Of 12 pharmacy schools in Thailand, 11 (92%) agreed to participate in the study, including 9 public and 2 private schools (Table 2). Two schools (U4 and U10) were undergoing curricula revision during the data collection for this study. Of the 11 participating schools, 9 schools had bachelor of science in pharmacy (BS Pharm) degree programs. The 2 exceptions were U10 and U11, which offered only the doctor of pharmacy (PharmD) degree. PharmD programs were offered in 5 public schools, including U3, U5, U7, U10 and U11. However, the PharmD programs in the first 3 schools listed had not fully implemented their PharmD curricula until after the data were collected for the present study. These 3 schools (U3, U5, and U7) began implementation of their PharmD programs in 2002, 2004, and 2004, respectively. Therefore, the data for the BS programs from these 3 schools were included, but their PharmD programs were not included in the current study. The 2 PharmD programs offered by U10 and U11 were included in the present study.
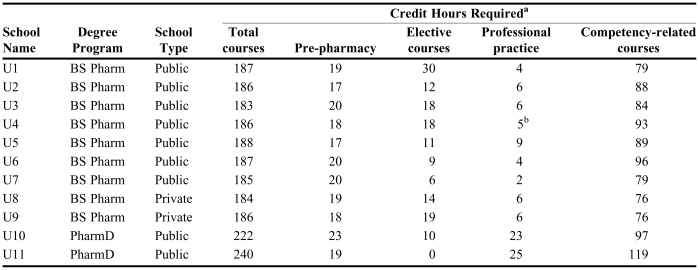
Table 2.
Demographic Data of Thai Pharmacy Schools
Abbreviations: BS Pharm = bachelor of science in pharmacy; PharmD = doctorate of pharmacy
aFor lecture courses, 1 credit is equivalent to 1 hour/week for 1 semester; for practical courses, 1 credit is equivalent to 3 hours/week for 1 semester
bincluded 2 credits of professional practice in elective courses
After reviewing the curricula documents, the prepharmacy courses (biochemistry, physiology, anatomy, microbiology, parasitology, and immunology), the professional elective, professional practice, and noncompetency-related courses were excluded from this analysis because they either did not directly apply to the Thai pharmacy competencies or they were not taught to all students. The professional practice courses in the BS programs consisted of 500 hours of experiential practice at sites where pharmacists worked. Because different competency domains were covered by this range of practice sites, they were not able to be categorized into a single course and were excluded from the analysis. The total competency-related courses and other course credits are shown in Table 2.
The professional practice average course credits at U10 and U11 PharmD programs were 4.5 times higher than that of the BS programs. In this analysis, 1 credit hour of a professional practice course was equivalent to 90 hours of practice. In the professional practice course category, the professional practice credits at U4 included 2 credits of professional practice courses for elective classes and 3 credits of the required course professional practice, since at least 2 credits of the professional practice in all tracks were mandated for all students. The mean number of competency-related credits was 84.4 (SD = 7.4) and 108 (SD = 15.6) in BS and PharmD programs, respectively.
Of the 11 pharmacy schools participating in this study, the response rates of the individual course coordinators who returned their completed questionnaires ranged from 48% to 100% (median 91%). The range of course coordinators per school was 22 to 59. The completed questionnaires were reviewed and the length of time dedicated to each subcompetency in a course was converted into credit hours. The formula of 1 credit hour being equivalent to 15 hours of lecture or 45 hours of laboratory was used for the conversion. A review of the competency domain results revealed that each competency domain was met by a different percentage across the 11 pharmacy schools. In addition, the information gathered from the course coordinators and course syllabi provided evidence that all competencies were addressed in current Thai pharmacy curricula, with the exception of competency 7.9, Keep drug information service records. This single competency did not appear to be addressed at 4 of the schools (U1, U3, U5, and U9). In contrast, competency 1.2, General knowledge in chemicals, particles, and their application in pharmaceutical manufacturing process and quality assurance, was the competency most frequently addressed by all 11 pharmacy schools.
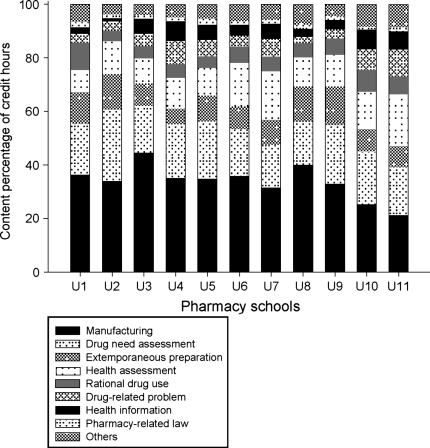
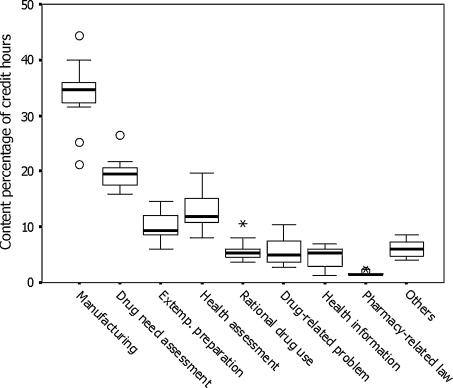
The content percentage of credit hours (proportion of credit hours for each competency domain) is graphically presented in Figure 1. The figure shows the distribution of content percentage for the 8 competency domains. The largest percentage was found in Domain 1 (Manufacturing and quality assurance) for all schools and the smallest percentage was found in Domain 8 (Pharmacy-related laws).
Figure 1.
Content percentage of credit hours contributed to each competency domain.
The percentage of time (%) spent teaching each competency domain in terms of credit hours is shown in Table 3. Approximately one third of the required content in the BS programs and one fourth of the core content in the PharmD programs were addressed in competency Domain 1 (Manufacturing and quality assurance). The 4 domains in which the average credit hours spent was less than 10% were: Domain 5 (Rational drug use planning), Domain 6 (Prevention and solving of drug-related problems), Domain 7 (Provision of health information), and Domain 8 (Pharmacy-related laws). However, a mean of 6% ± 1.63% of total credit hours were spent in the Domain “others,” which were areas not addressed in the domains covered by the pharmacy licensure examination and pharmacy competencies. The content in the Domain “others,” such as pharmacy administration, behavioral science, and sociology were grouped within social and administrative pharmacy-oriented material.
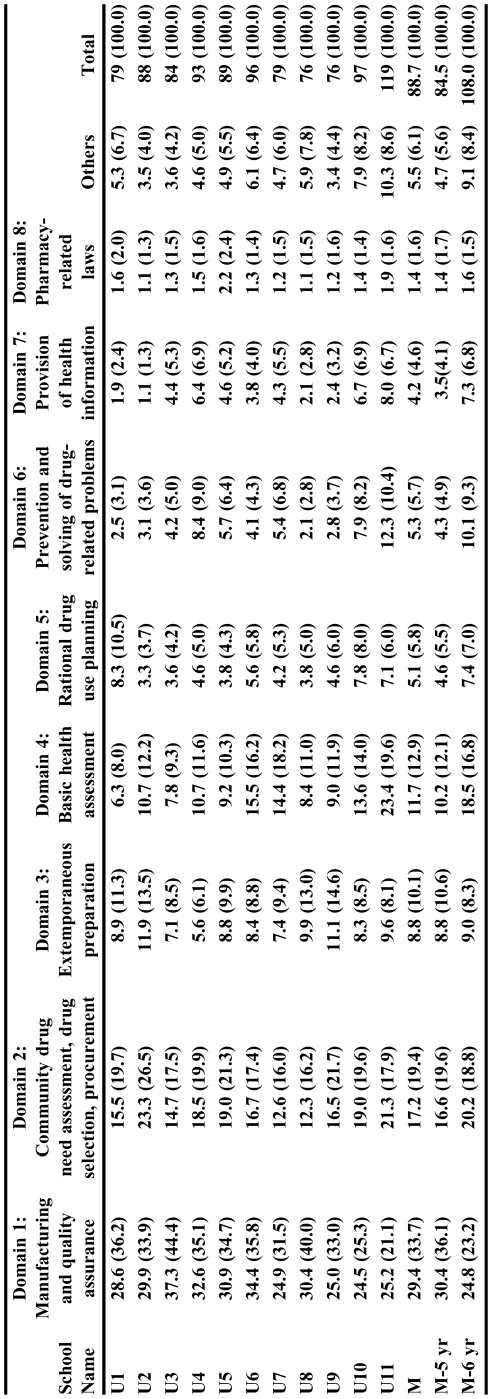
Table 3.
Credit Hours and the Percentage of Time Spent on Each Competency Domain
M = mean; M-5 yr = mean credit hours in BS Pharm programs; M-6 yr = mean credit hours in PharmD programs.
The stratification of credit hour percentage devoted to each domain is shown in Figure 2. The findings illustrate the curricula content pattern between the 4 subject categories based on the applicable number of credit hours reported by each school of pharmacy. The results indicate that domain 1 (manufacturing and quality assurance) was the largest domain for all pharmacy schools. The percentage of credit hours in this domain was the highest compared to the other domains. Its median value was approximately 25 to 30 credit hours within each school. Domain 2 (community drug needs assessment, drug selection and procurement) was the second largest percentage of credit hours across the curricula. The median for domain 2 was approximately 20% of credit hours. Domain 3 (extemporaneous preparation) and domain 4 (basic health assessment) were categorized into one group because of their low proportions and the combined median credit hours was about 10%. Lastly, the lowest percentages of credit hours were in domain 5 (rational drug use planning), domain 6 (prevention and solving of drug-related problems), domain 7 (provision of health information) and domain 8 (pharmacy-related laws), with each of these domain receiving less than 6% of the median value across all pharmacy schools. However, Figure 2 demonstrates there were outliers found in 4 of these domains.
Figure 2.
Stratification of the percentage of credit hours of competency domains.
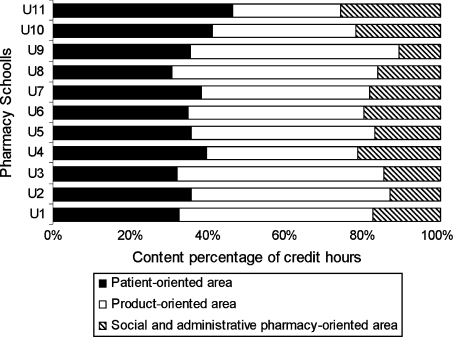
The percentage of credit hours spent in each competency area is presented in Figure 3. The predominant content area for the BS program was product-oriented material. The average percentage of credit hours spent on product-oriented content was nearly 50%. The SAP-oriented content consisted of less than 20% of curricula in all BS programs except U4. In contrast, the predominant content area in the PharmD programs was patient-oriented content. One third and one fourth of the core curriculum content of PharmD programs were addressed in product-oriented and SAP-oriented material, respectively.
Figure 3.
Percentage of competency area in all schools.
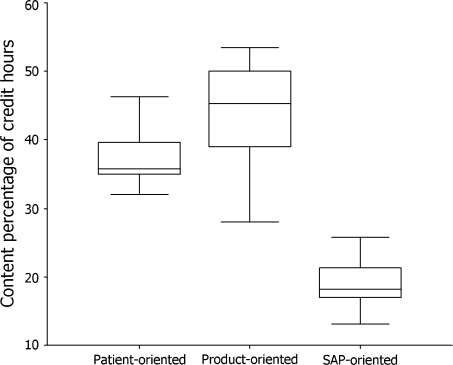
The stratification of credit hour percentages in the competency-oriented material for all schools is demonstrated in Figure 4. The content areas were ranked from the highest percentage to the lowest percentage as product-oriented, patient-oriented, and SAP-oriented content, respectively. There were no outliers found in any of these competency-oriented materials. However, the greatest variation of content among schools was in the product-oriented material.
Figure 4.
Stratification of the percentage of credit hours of competency-oriented area.
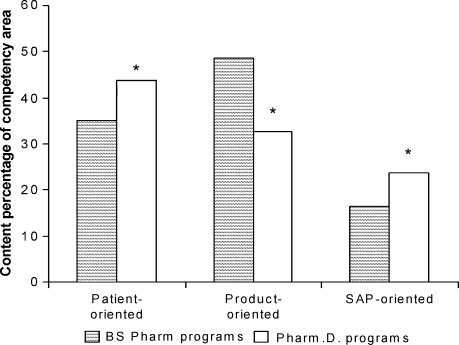
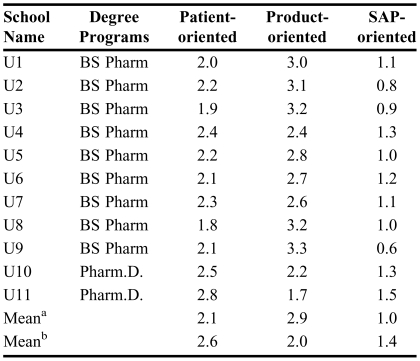
The competency-oriented material was compared between the BS and PharmD programs (Figure 5). The PharmD programs had more content (44%) in patient-oriented material than in product-oriented material (33%). Conversely, the BS programs had more product-oriented content (49%) than patient-oriented content (35%). There was a significant difference between the BS and PharmD programs in the 3 competency-oriented areas (p = 0.005, 0.004, and 0.018 in patient-, product-, and SAP-oriented areas, respectively). Patient-, product-, and SAP-oriented content ratios were 2.1:2.9:1.0 and 2.6:2.0:1.4 in BS and PharmD programs, respectively.
Figure 5.
Competency-oriented content between the bachelor and PharmD programs.
The ratios of patient-, product-, and SAP-oriented content at each school are shown in Table 4. The highest ratio in product-oriented content was found in U9, U3 and U8, respectively. U11, which is a PharmD program, had the lowest ratio in product-oriented and the highest ratio in patient-oriented material compared to other schools. However, the ratio of patient-oriented and product-oriented content was comparable in U4.
Table 4.
Ratios of Patient-, Product-, and SAP-Oriented Content Each School
aAverage ratios in the bachelor of science in pharmacy programs
bAverage ratios in the PharmD programs
Although the course coordinators used several methods of teaching, the questionnaire did not ask the percentage of credit hours for which each teaching method was used. Therefore, the percentage of credit hours for which each teaching method was used was based on the course structure of either a lecture or laboratory. The mean proportion of credit hours taught by lectures was 79.4% ± 3.7%. The balance (20.6 ± 3.7%) of credit hours was taught by laboratory experiences. The most frequent teaching method used in all Thai pharmacy schools was lectures presented in classrooms. Other methods used were experiments, case studies, discussion groups, class assignments, demonstrations, and pharmacy practice experiences. In product-oriented laboratory classes, students could conduct experiments with actual products. Examples included formulating syrup preparations, making coated tablets, and analyzing drug label content. In patient-oriented and SAP-oriented laboratory classes, the teaching methods used included case studies, discussions, and self-learning (completion of in class or homework assignments).
Students rarely interacted with real patients in these required didactic courses. Only 3 schools reported that their students met actual patients when visiting hospitals and drug stores as part of course experiences. However, less than 1 credit hour was devoted to actual patient interactions. Thai pharmacy students were able to gain experience with actual patients in elective courses or professional practice courses.
DISCUSSION
All 8 competency domains and 70 competency statements were taught in all 11 pharmacy schools. This implied that the pharmacy curricula met the 8 domain requirements of the Thai Pharmacy Council. Although there was a difference between total credits required for/by the BS and PharmD programs, all pharmacy graduates from both types of programs had to take the same licensure examination before entering practice. Therefore, all competency domains were completed in all programs in order to prepare the pharmacy students for licensure. This finding correlated with Boss and Lowther's who concluded that one factor that influenced professional schools to change their curricula was to better prepare graduates to meet licensure requirements.2
Of the 8 competency domains, it was not surprising that the domain of “manufacturing and quality assurance” was the largest. This was because the main characteristic of the BS programs was to emphasize product-oriented topics. In contrast, the PharmD programs were less focused on the domain of manufacturing and quality assurance. However, the content percentage of credit hours in U3 was the highest compared to other schools in the domain “manufacturing and quality assurance.” Nevertheless, their percentage was not different from the other schools when this was combined with the domain “extemporaneous preparation.” This was because these 2 domains were both product-oriented areas and the focus of the content could probably be substituted.
This study categorized curricula content into 3 competency-oriented areas. The BS programs predominantly had product-oriented content. Similar to the undergraduate program in New Zealand and European countries, the major focus of pharmacy education was traditional, product-oriented topics.15 Patient-oriented, product-oriented, and social and administrative pharmacy (SAP)-oriented content ratios were 2.1:2.9:1.0, and were different from the standards established by the Thai Pharmacy Council (3:2:1). The ratio of 3:2:1 for patient-oriented, product-oriented, and SAP-oriented components developed by the Thai Pharmacy Council forms the basis of the Thai licensure examination and all Thai pharmacy schools were aware of this ratio. However, schools were not required to comply with this ratio as the Thai Pharmacy Council has no means of enforcement. The PharmD program ratios (2.6:2.0:1.4) were more aligned with those recommended by the Thai Pharmacy Council. Panucharus and colleague studied the correlation of the use of SAP knowledge among Thai pharmacists and found that SAP knowledge was not adequate for pharmacists to work in practice settings.16 This finding might be a controversial issue regarding whether the SAP-oriented content ratio (1 part of 6) was adequate for pharmacy graduates.
The low proportion of patient-oriented content in the Thai competency standards may be partially explained in how most Thai curriculum revisions have been made. New knowledge and skills on patient-oriented topics were incorporated into the Thai pharmacy curricula, but the large amount of product-oriented content was not decreased. Therefore, the ratio of patient-oriented content was not met. Expanding Thai pharmacy student experiences with actual patients and decreasing the product-oriented courses will further improve this ratio.
Although the experiential pharmacy practice rotations were not included in the data collection of this study because of the broad variety of rotations selected by students, its exclusion only had a minor impact on the overall results of this study. There are 2 main explanations for this. First, the length of the experiential rotations in the BS programs is only 500 hours. This is in contrast to 2,000 experiential hours required by the PharmD programs. Second, in the BS programs, pharmacy students were allowed to select experiential rotations from a broad range of options. If the students' experiential rotation was at a hospital or community pharmacy, the focus will be on a range of pharmacist roles and students will obtain excellent experience in domains 4, 5, and 6, and some experience in Domains 2 and 7. In contrast, if the students' experiential rotation was at a pharmaceutical industry site, the focus would be on pharmaceutical production and the student would gain excellent product-oriented competency experience within domains 1 and 3, and some experience in domain 2. Because the BS Pharm program is only 500 hours and the experiences gained impact a range of domains, there was actually a relatively small impact on the curriculum ratio of patient to product to social and administrative pharmacy. For example, if a student completed an experiential rotation that emphasized patient-oriented material (eg, at a hospital), the overall patient to product curriculum ratio would increase by 0.1. In contrast, if the student completed an experiential rotation that emphasized product-oriented material, the overall patient to product curriculum ratio would decrease by 0.1. Thus, the impact of the experiential rotation in the BS programs is relatively minor and would not appreciably impact the overall ratio of patient to product to social and administrative pharmacy curricular content.
A limitation of this study is that using course syllabi and surveying course coordinators for data collection may not actually match the actual time devoted to competency areas within the classroom. Because data were collected from a broad range of coordinators, the accuracy of their assessment of curriculum content may have varied, ie, some coordinators may sit through all the course material with the students and be more knowledgeable about details of the course content, while other coordinators may only attend some of the lectures in the courses they coordinated.
Revisions of pharmacy curricula have been undertaken in many countries based on many factors such as accreditation and licensure, changes within the profession, technology developments, and growing knowledge base.2 These experiences of pharmacy faculty members in Thailand will be useful to other countries as they move more toward a patient-oriented perspective in pharmaceutical care. For example, in Hungary, a new pharmacy curriculum was developed to emphasize clinical pharmacy skills and drug therapy in order to prepare pharmacists to practice effectively in that country's changing health care delivery system.17 The same situation was found in Saudi Arabia and Romania; schools of pharmacy revised their curricula in order to prepare pharmacy graduates to practice more effectively in their health care systems.18,19
In the United States, competency statements were initiated in order to revise the pharmacy curriculum.20 In addition, professional organizations in many countries such as Australia, Canada, and the United States have worked to develop pharmacy competency standards for pharmacists in their countries.5,7,14 These standards were used not only to maintain pharmacists' competencies, but also to guide pharmacy schools in updating their curricula.21 Similarly, in Thailand, the pharmacy curriculum has been revised in an ongoing manner based on changes in the profession. Although the Thai Pharmacy Council developed the competency standards for licensure examination, the patient-oriented competency proportion in the Thai didactic curricula does not satisfy these standards. The information from this study may be used as part of a competency-based curriculum development process. To meet the Thai Pharmacy Council standards and to meet societal needs, there must be an expansion in patient-oriented material.
CONCLUSIONS
Based on Thai pharmacy competency standards, the curricula of both the BS and PharmD degree programs addressed all 8 competency domain requirements. However, the patient-oriented portion did not meet the Thai pharmacy competency standards, which have a higher emphasis on patient-oriented material. The ratio of patient-oriented, product-oriented, and social and administrative pharmacy-oriented content areas was 2.1:2.9:1.0, which differed from the ratio recommended by the Thai pharmacy competency standard (3:2:1). The predominant content area was product-oriented material for the BS programs. In contrast, the predominant content area in the PharmD programs was patient-oriented content. Social and administrative pharmacy-oriented content was the lowest in both the BS and PharmD curriculums. As Thai pharmacy schools further revise their curricula, it may be useful to decrease the product-oriented content and expand patient-oriented material.
ACKNOWLEDGEMENTS
The authors acknowledge the graduate school of Silpakorn University for partly funding this study. In addition, we would like to recognize all course coordinators who provided valuable data for this study to be conducted.
REFERENCES
- 1.Pothiyanon P. Bangkok: Chulalongkorn University; 1998. 84 years of pharmacy in Thailand; Faculty of Pharmacy, Chulalongkorn University, ed. 84 years of pharmacy in Thailand ; pp. 15–25. [Google Scholar]
- 2.Boss MA, Lowther MA. Factors influencing curriculum change in professional programs. Paper presented at: 18th the Annual Meeting of the Association for the Study of Higher Education, 1993.
- 3.Hancox D. Current trends in pharmacy education. N Z Med J. 1982;95:121–2. [PubMed] [Google Scholar]
- 4.Summers R, Haavik C, Summers B, Moola F, Lowes M, Enslin G. Pharmaceutical education in the South African multicultural society. Am J Pharm Educ. 2001;65:150–4. [Google Scholar]
- 5.Professional competencies for Canadian pharmacists at entry to practice. National Association of Pharmacy Regulatory Authorities, Canada. Available at: http://www.napra.ca/pharmacists/becoming/competencies.pdf. Accessed August 20, 2004.
- 6.Educational outcomes 2004, American Association of Colleges of Pharmacy. Available at: http://www.aacp.org/Docs/MainNavigation/Resources/6075_CAPE2004.pdf. Accessed August 20, 2004.
- 7.Competency Standards for Pharmacists in Australia 2003. Pharmaceutical Society of Australia. Available at: http://www.psa.org.au/site.php?id=643&output=print. Accessed August 20, 2004.
- 8.Silva JAAD, Ramos F, Silva I. Implementing a new model for admission and qualification of Portuguese pharmacists. Pharm Educ. 2004;4:123–8. [Google Scholar]
- 9.Thai Pharmacy Council. Standard criteria for pharmacy practitioners 2002. Bangkok: Thai Pharmacy Council; 2002. [Google Scholar]
- 10.Anderson HM, Anaya G, Bird E, Moore DL. A Review of educational assessment. Am J Pharm Educ. 2005;69:84–100. [Google Scholar]
- 11.Ewell PT. National trends in assessing student learning. J Engl Educ. 1998;87:107–13. [Google Scholar]
- 12.Assemi M, Cullander C, Hudmon KS. Implementation and evaluation of cultural competency training for pharmacy students. Ann Pharmacother. 2004;38:781–6. doi: 10.1345/aph.1D402. [DOI] [PubMed] [Google Scholar]
- 13.Kirkpatrick MA, Pugh CB. Assessment of curricular competency outcomes. Am J Pharm Educ. 2001;65:217–24. [Google Scholar]
- 14.Accreditation Standards and Guidelines for The Professional Program in Pharmacy Leading to The Doctor of Pharmacy Degree. Accreditation Council for Pharmacy Education. Available at: http://www.aacp.org/Docs/MainNavigation/Resources/5833_lettertoACPE_standards.pdf. Accessed July 12, 2006.
- 15.Shaw JP. Undergraduate pharmacy education in the United States and New Zealand: towards a core curriculum? Pharm Educ. 2001;1:5–15. [Google Scholar]
- 16.Panucharus D, Chalongsuk R. Relationship between knowledge in social and administrative pharmacy and pharmacy practice. Srinakharinwirote J Pharm Sci. 2005;10:201–9. [Google Scholar]
- 17.Antal I, Matyus P, Marton S, Vincze Z. Developing the pharmacy curriculum in a Hungarian faculty. Pharm Educ. 2002;1:241–6. [Google Scholar]
- 18.Al-Sowaygh IA, Morad A-RM, Abdullah ME. Pharmacy curriculum and health care needs in Saudi Arabia. Am J Pharm Educ. 1981;45:20–4. [PubMed] [Google Scholar]
- 19.Popa A, Crisan O, Sandulescu R, Bojita M. Pharmaceutical Care and Pharmacy Education in Romania. Pharm Educ. 2002;2:11–14. [Google Scholar]
- 20.Munson JW. Interaction model of competency statements for use in curriculum development. Am J Pharm Educ. 1977;41:172–175. [PubMed] [Google Scholar]
- 21.Dobbert DJ. Experiences with and assessment of competency-based curriculum in disciplines outside of pharmacy. Am J Pharm Educ. 1975;39:560–566. [PubMed] [Google Scholar]