Abstract
Background
The 10-item version of the Cocaine Craving Questionnaire (CCQ-Brief) has not been validated in a mixed-gender sample, and predictive validity of the CCQ-Now and CCQ-Brief in terms of their relationship with cocaine relapse has not been demonstrated.
Objective
To further validate the CCQ-Brief in a mixed gender sample and to determine the predictive validity of the CCQ-Now and CCQ-Brief.
Method
Seventy-two men and 51 women (Total N = 123) seeking inpatient cocaine dependence treatment were administered assessments upon admission, and a prospective design was employed to assess cocaine relapse outcomes during a 90-day follow-up period after discharge from inpatient treatment. Data were analyzed using Pearson’s correlation, Cox proportional hazards regression, and multiple regression.
Findings
The CCQ-Brief demonstrated good internal consistency and construct and concurrent validity. Both the CCQ-Now and the CCQ-Brief summary scores predicted time to cocaine relapse. In addition, the anticipation of a positive outcome from cocaine use, and intent and planning to use cocaine subscales of the CCQ-Now also predicted time to cocaine relapse.
Conclusions
The CCQ-Brief was found to be a reliable and valid measure in a mixed gender sample, and both the CCQ-Now and CCQ-Brief were predictive of cocaine relapse risk. Craving assessments that go beyond desire and take into account intent and planning to use cocaine and the patient’s anticipation of a positive outcome from using cocaine are likely to provide a sensitive index of cocaine relapse susceptibility. However, fear of social and clinical consequences could impact accurate reporting of cocaine craving and intent to use cocaine.
Keywords: Cocaine craving, relapse, psychometrics, CCQ
1. Introduction
Craving is a hallmark symptom of drug addiction. Specifically, its association with drug withdrawal, treatment outcome, and substance use relapse is noteworthy (Ludwig and Wikler, 1974; Weiss et al., 2003). In the treatment outcome literature, craving has primarily been used as a surrogate outcome measure, with craving reduction interpreted as treatment success (Singleton and Gorelick, 1998; Smelson et al., 2002). However, while researchers have commonly viewed craving as a primary factor motivating drug use, the empirical evidence supporting this claim is limited (Mello, 1978; Rohsenow et al., 1991; Tiffany, 1990). Some studies of cocaine dependent individuals support an association between craving and relapse (Bordnick and Schmitz, 1998; Robbins and Ehrman, 1998; Weiss et al., 1997) and subsequent drug use (Kranzler and Wallington, 1992; Weiss et al., 2003), whereas others do not (Miller and Gold, 1994; Weiss et al., 1995). Although studies of alcohol dependent individuals are inconsistent in their demonstration of a relationship between craving and treatment outcomes including relapse (Anton, 2000; Rohsenow and Monti, 1999), alcohol craving remains a useful indicator of positive treatment outcome in studies demonstrating the efficacy of pharmacological treatments such as naltrexone for alcoholism (Addolorato et al., 2005; O'Brien et al., 1996). Furthermore, a robust relationship between craving and outcomes has been reported in nicotine smokers (Doherty et al., 1995; Killen, 1997; Piasecki, 2006; Shiffman et al., 1997).
The inconsistent documentation of an association between cocaine craving and relapse is counterintuitive and may be a product of a lack of consensus about the theory and nature of craving (Drummond, 2001) and difficulties measuring craving (Sayette et al., 2000). It has also been noted that since craving can vary over time, assessments that measure craving some time before a relapse event may not capture the craving occurrences that are most relevant to relapse (Drummond, 2001; Sayette et al., 2000). Furthermore, with craving being a complex multidimensional concept, it is quite possible that the various dimensions of craving are differentially related to behavior, mood, and cognition, which can also vary over time.
A multidimensional instrument that measures various aspects of craving permits examination of the relationship between different components of craving and outcomes of interest. Yet, most studies of cocaine abusers either use a visual analog scale (Robbins and Ehrman, 1998) or a few questions (Weiss et al., 2003; Bordnick and Schmitz, 1998; Weiss et al., 1997; Weiss et al., 1995) to measure craving even though there exists more systematically developed and validated multi-item and multidimensional measures that take into account theories of craving. One such measure is the Cocaine Craving Questionnaire-Now (CCQ-Now) (Tiffany et al., 1993).
The CCQ-Now is a 45-item craving measure with established reliability and validity that comprehensively assesses five theoretically distinct elements of cocaine craving (Tiffany et al., 1993). An abbreviated version of the measure, the CCQ-Brief, has been developed and may be used in settings where administration of the longer version would be difficult. The CCQ-Brief consists of 10 of the original items from the CCQ-Now and was recently validated in a sample of primarily male (97%) cocaine dependent inpatients (Sussner et al., 2006). Advantages of using a brief measure of cocaine craving include shorter assessment time and ease of administration. However, the CCQ-Brief has not been validated in a mixed gender sample, and the predictive validity of both the CCQ-Now and the CCQ-Brief in terms of their relationship with relapse outcomes has not been demonstrated.
Therefore, the present study examined the psychometric properties of CCQ-Brief in a mixed-gender sample of cocaine dependent inpatients. Its association with the Beck Depression Inventory (Beck, 1961), cocaine craving from the Cocaine Severity Selective Assessment (CSSA; Kampman et al., 1998) and the CCQ-Now was assessed. Next, the predictive validity of the CCQ-Now and the CCQ-Brief was assessed prospectively by examining their associations with cocaine relapse outcomes (time to initial relapse, frequency of use following relapse, and amount of cocaine used per occasion following relapse). As a follow-up analysis, we also assessed whether the specific subscales the CCQ-Now separately predicted relapse outcomes. A potential moderating role of gender in studying the relationship between craving and cocaine relapse outcomes was also assessed. We hypothesized that 1) the CCQ-Brief will be a reliable and valid measure of cocaine craving in a mixed gender sample of cocaine dependent inpatients, and 2) the CCQ-Now and the CCQ-Brief will each predict cocaine relapse outcomes after discharge from inpatient treatment.
2. Method
2.1. Participants and Procedures
One hundred and thirty two individuals (75 men and 57 women) meeting DSM-IV criteria for current cocaine dependence (which was documented by self-reports of regular weekly cocaine use and a positive urine toxicology screen) were admitted to the Clinical Neuroscience Research Unit (CNRU) of the Connecticut Mental Health Center (CMHC) for an average of three weeks (Mean length of stay = 22 days, SD = 6.63) of inpatient treatment and research participation. The CNRU is a locked inpatient treatment and research facility with no access to alcohol or drugs and limited access to visitors. Individuals who met current DSM-IV criteria for dependence on another psychoactive substance other than alcohol, marijuana and nicotine were excluded. In addition, individuals on medications for medical or psychiatric conditions, and those in need of an immediate alcohol detoxification were excluded from the study. All subjects underwent a complete medical evaluation, including electrocardiography and laboratory tests of renal, hepatic, pancreatic, hematopoietic, and thyroid functions, to ensure good physical health. The Human Investigation Committee of the Yale University School of Medicine approved the study procedures, and all subjects signed a written informed consent.
All participants were given an appointment for a follow-up interview 90 days after discharge from the inpatient unit. Reminders were sent in the month of the appointment. Ninety days following discharge, subjects returned for a face-to-face follow-up interview where they provided a urine toxicology screen and answered questions to assess relapse and subsequent drug use during the 90-day follow-up period. One hundred and twenty three of the 132 patients (93.2%) who completed inpatient treatment were successfully followed for 90 days. Thus, the data analysis for the current study is based on the follow-up sample of 123 cocaine dependent individuals (72 men and 51 women).
Upon treatment entry, subjects were interviewed using the Structured Clinical Interview for the DSM-IV Axis I disorders (SCID-I) (First et al., 1995) and were administered a battery of self-report assessments. While on the unit, they participated in specialized substance abuse treatment that included weekly individual therapy provided by psychiatry residents and twice weekly group drug counseling provided by an addiction specialist (Mercer et al., 1994). The group drug treatment was part of the inpatient treatment program that was initiated upon admission and included additional group programming from 9:00 AM to 3:30 PM that covered daily life skills and other structured activities. Drug testing was conducted regularly to ensure continued abstinence.
2.2. Measures
2.2.1. CCQ-Now and CCQ-Brief (Tiffany et al., 1993; Sussner et al., 2006)
The CCQ is a 45 item self-report questionnaire that assesses specific aspects of current craving for cocaine (the Now version) and average craving over the past week (the General version). Both versions include items that assess the following content areas: 1) desire to use cocaine (Desire), 2) intent and planning to use cocaine (Intent), 3) anticipation of positive outcome from using cocaine (Positive), 4) anticipation of relief from withdrawal or dysphoria from using cocaine (Relief), and 5) lack of control over use (Lack Cont). It has been shown to have high reliability (α= 0.93) and very good concurrent validity in cocaine users with no intention of achieving abstinence. In our inpatient sample too, reliability of the CCQ-Now was found to be excellent (α = 0.90). The CCQ-Brief provides a short measure of current cocaine craving and is comprised of the 10-items from the CCQ-Now that loaded heavily on the general craving factor of the scale during the full scale’s initial validation (Tiffany et al., 1993).
The psychometric properties of the CCQ-Brief has recently been tested in a sample of treatment engaged cocaine dependent men (Sussner et al., 2006). The internal consistency coefficient for the CCQ-Brief was found to be strong at .90. It correlated significantly with the CCQ-Now (r = .85) and with a version of the CCQ-Now that had items in common with the brief form removed (r = .78). It also correlated significantly, but less strongly, with the craving intensity (r = .47), mood (r = .27), energy (r = 30), and sick feelings (r = .28) subscales of the Voris Cocaine Craving Scale (VCCS). Finally, the CCQ-Brief significantly correlated with the Beck Depression Inventory-II (BDI-II) (r = .39), the Beck Anxiety Inventory (BAI) (r = .35), and with days of use in the past 30 days (r = .26).
In the current study, the CCQ-Brief was recreated from the CCQ-Now which was administered at the end of the first week of admission. In addition, for a large majority of patients (N=102), we also had available the CCQ-Brief version obtained on day 1 of admission to the inpatient unit. The recreated CCQ-Brief (from the CCQ-Now) and the Day 1 CCQ-Brief were almost perfectly correlated (r = .995, p < .0001). Furthermore, the CCQ-Brief (both versions) and the CCQ-Now were also highly correlated (r’s_= .87, p < .0001). We selected to use the recreated version of the CCQ-Brief for the purposes of the current study for the following reasons: First, it was available on all the patients being studied (N=123). Second, the CCQ-Now was administered during the later part of the first week of the inpatient stay, after the acute cocaine withdrawal period, and hence is more generalizable to other treatment seeking cocaine patients.
2.2.2. The Beck Depression Inventory (Beck et al., 1961)
The BDI is a widely used and sensitive self-report measure of depression. The total score ranges from 0–63. Higher scores indicate greater levels of depressive symptomatology. The BDI has demonstrated high internal consistency, with alpha coefficients of .86 and .81 for psychiatric and non-psychiatric populations, respectively (Beck et al., 1988). For the current study, the BDI was used to assess concurrent validity of the CCQ since the BDI is a well established index of emotional distress, and emotional distress is often associated with drug craving ((Sinha et al., 1999; Sinha et al., 2000; Sinha et al., 2003; Sinha et al., 2006).
2.2.3. The Cocaine Selective Severity Assessment (CSSA) (Kampman et al., 1998)
The CSSA is a reliable and valid clinician-administered instrument that measures cocaine withdrawal signs and symptoms. It is comprised of a Likert scale of 18 items, with 0 representing no symptoms and 7 the maximum score. The items include questions about hyperphagia, hypophagia, carbohydrate craving, cocaine craving, frequency of craving, brachycardia, sleep, anxiety, energy level, tension, attention, paranoid ideation, anhedonia, depression, suicidality and irritability. The Cronbach’s alpha coefficient for the CSSA was 0.80 for a cocaine dependent sample, .80 for a cocaine/alcohol dependent sample, and .69 for a strictly alcohol dependent sample (Kampman et al., 1998). The CSSA was able to discriminate between recently abstinent cocaine and alcohol dependent subjects. It demonstrated concurrent validity by correlating significantly with a measure of addiction severity in cocaine and cocaine/alcohol dependent subjects. Finally, predictive validity was demonstrated by the measure’s ability to predict poor treatment outcome and showing that scores declined with continued abstinence. Notably, the sample used for these analyses was mixed gender but predominantly (75%) male (Kampman et al., 1998). We used the cocaine craving item and craving frequency subscales of the CSSA to assess the construct validity of CCQ-Brief, and we used the CSSA mean score as an index of cocaine abstinence symptoms to assess the concurrent validity of CCQ-Brief.
2.2.4. Assessment of Cocaine Relapse at 90 Days Post Inpatient Treatment
Cocaine use during the follow-up period was assessed using the Form 90 Substance Use Calendar (SUC; Miller and Delboca, 1994) which is based on the Timeline Follow-Back (TLFB) method (Sobell and Sobell, 1996). The SUC uses a calendar prompt and a number of other memory aids to facilitate accurate recall of daily drug use during the targeted period. The instrument that has been validated in drug abusing samples (Hersh et al., 1999; Fals-Stewart et al., 2000). Urine and breathalyzer samples were also obtained at the 90-day follow-up appointment. In order to capture both relapse to drug use (any use) and return to regular patterns of drug use (Rohsenow and Monti, 2001), “relapse” in this study was examined both as a dichotomous variable (no use/success vs. any use/failure) and as continuous measures of drug use (e.g., number of days of use and amounts of use per occasion) in the 90-day follow-up period. The following outcomes were computed from the follow-up SUC and urine screen and used for the relapse analysis: (a) Time to relapse was defined as a dichotomous variable that documented the first day when any cocaine use occurred during the 90 day follow-up period, (b) frequency of use was defined as the total number of days of cocaine use during the follow-up period, and (c) quantity of use was defined as the average amount of cocaine used per occasion (in grams) during the follow-up period.
3. Data Analysis
The CCQ-Now and CSSA craving scale were used to assess the construct validity of the CCQ-Brief. The BDI, CSSA, drug use history (age of first use, number of years of use) and baseline cocaine use (amount and frequency) for the 90 days prior to inpatient treatment were used to examine concurrent (or convergent) validity. Predictive validity of the CCQ-Now, the CCQ-Now subscales, and the CCQ-Brief was established by studying their association with relapse outcomes. Time to cocaine relapse was examined using Cox proportional hazards regression models (Cox, 1972). Linear regression analyses were conducted to examine associations with frequency and amount of cocaine used during the follow-up period. Any demographic variable, baseline psychiatric or substance use measure, or treatment related measure that was associated with a particular relapse outcomes was included as a covariate in that specific regression analysis. While examining the predictive validity of both CCQ versions, gender was included in both analyses. An interaction between gender and the craving measures was also included to investigate whether gender moderated the relationship between craving and relapse.
4. Results
4.1. Demographics and Sample Characteristics
Demographic data, substance use history variables, and lifetime and current rates of psychiatric and substance use disorders for the entire sample (N=132) and the follow-up sample (N = 123) were found to be highly similar (see Table 1).
Table 1.
Demographics and Sample Characteristics
| Subject Variable | Intent to treat sample (N=132) | Follow-up sample (n=123) |
|---|---|---|
| Gender (N,%) | ||
| Female | 57 (43.2%) | 51 (41.5%) |
| Male | 75 (56.8%) | 72 (58.5%) |
| Ethnicity (N,%) | ||
| African American | 75 (56.8%) | 72 (58.5%) |
| Caucasian | 44 (33.3%) | 39 (31.7%) |
| Hispanic | 4 (3.0%) | 4 (3.2%) |
| Other | 9 (6.8%) | 8 (6.5%) |
| Age (M,SD) | 36.9 (6.4) | 37 (6.3) |
| Marital Status (N,%) | ||
| Never Married | 69 (52.3%) | 66 (53.7%) |
| Separated/Divorced | 11 (8.3%) | 9 (7.3%) |
| Widowed | 31 (23.5%) | 28 (22.8%) |
| others | 21 (15.9%) | 20 (16.3%) |
| Employment (N,%) | ||
| Full Time | 17 (12.9%) | 14 (11.4%) |
| Part Time | 18 (13.6%) | 16 (13.0%) |
| Unemployed | 97 (73.5%) | 93 (75.6%) |
| Years of Education (M,SD) | 12.3 (1.6) | 12.3 (1.7) |
| Route of Administration- Smoking (N,%) | 120 (90.9%) | 112 (91.1%) |
| Age first used Cocaine (M,SD) | 20.2 (5.6) | 20.2 (5.8) |
| Age first used Alcohol (M,SD) | 14.1 (3.2) | 14.0 (3.2) |
| Years of Cocaine Use (M,SD) | 9.1 (6.3) | 9.1 (6.2) |
| Years of Alcohol Use (M,SD) | 11.9 (8.2) | 11.8 (8.2) |
| Lifetime Diagnoses (N,%) | ||
| Mood DX | 37 (28.0%) | 33 (26.8%) |
| Anxiety DX w/out PTSD | 18 (13.6%) | 15 (12.2%) |
| PTSD | 39 (30.0%) | 36 (29.3%) |
| ETOH Dependence | 72 (54.5%) | 67 (54.5%) |
| Cannabis Dependence | 53 (40.1%) | 47 (38.2%) |
| Opioid Dependence | 5 (3.8%) | 5 (4.1%) |
| Current Diagnoses (N,%) | ||
| Mood DX | 13 (10.0%) | 10 (8.1%) |
| Anxiety DX w/out PTSD | 14 (10.8) | 12 (9.8%) |
| PTSD | 18 (13.9%) | 15 (12.2%) |
| ETOH Dependence | 45 (36.9%) | 47 (36.4%) |
| Cannabis Dependence | 20 (16.4%) | 23 (18.0%) |
| Opioid Dependence | 0 (0.00%) | 0 (0.00%) |
4.2. Psychometrics of CCQ-Brief
4.2.1. Internal Consistency
The CCQ-Brief as a global measure of craving demonstrated very good reliability (α = 0.87).
4.2.2. Construct Validity of the CCQ-Brief
To assess the validity of the “craving” construct, we found that the CCQ-Brief summary score was highly correlated with the CCQ-Now summary score (r = 0.87; p < 0.001). Data from the CSSA was available for 94 subjects. The CCQ-Brief summary score was moderately and significantly correlated with the CSSA cocaine craving (r = 0.46; p < 0.001), craving frequency (r = 0.46; p < 0.001), desire visual analog (VA) subscale (r = .47; p < 0.001) and urge VA subscale (r = 0.49; p < 0.001).
4.2.3. Concurrent Validity of the CCQ-Brief
BDI data was available for 111 subjects. The CCQ-Brief summary score (r = 0.43; p < 0.001) moderately correlated with the BDI score. The CSSA mean score was available for 94 subjects and positively correlated with CCQ-Brief summary score (r = 0.38; p < 0.001). Moreover, drug use history (age at first use, number of years of use, and baseline amount and frequency of cocaine use during the 90 days prior to entering treatment) was not related to any cocaine craving measure.
4.2.4. Predictive Validity of the CCQ-Now, Its Subscales, and the Brief Version
Eighty-nine (72.4 %) subjects relapsed during the 90 day follow-up period. Seventeen of the 123 patients (14%) showed discordance between their negative self-report of cocaine use and the positive urine toxicology results obtained at the follow-up interview. For these subjects, their day of relapse was coded on day 1 immediately after discharge (day 1 of follow-up), and their frequency and amount of cocaine use during the 90-day follow-up period was coded as missing. Amount of cocaine used per occasion during the 90 days prior to inpatient admission was significantly associated with time to cocaine relapse (X² = 3.89; p < .05). No other demographic variable, sample characteristic, or treatment history variable (including previous treatment history or treatment during the follow-up period) was associated with time to cocaine relapse. Frequency of cocaine use after relapse was significantly associated with baseline frequency of cocaine use (R² = 0.06; t = 2.72; p<.01) and lifetime history of PTSD (R² = 0.03; t = −2.03; p<.05). Amount of cocaine use after relapse was significantly associated with baseline amount of cocaine use (R² = 0.04; t = 2.01; p<.05) and lifetime history of PTSD (R² = 0.04; t = −2.17; p<.04).
Cox proportional hazard regression analyses, including baseline amount of cocaine use as a covariate, indicated that the CCQ-Now score (X² = 7.23; p < .008; HR = 1.01; CI:1.00–1.01) was significantly associated with time to relapse. Further, examining the specific CCQ-Now subscales for their relationship with relapse outcomes revealed that intent and planning to use cocaine (X² = 4.44; p < .04; HR = 1.03; CI:1.00–1.05) and anticipation of positive outcome from using cocaine (X² = 5.35; p<.02; HR = 1.02; CI:1.00–1.04) were each significantly associated with risk of relapse. Anticipation of relief from cocaine withdrawal or dysphoria showed a significant trend (X² = 3.3; p<.07; HR = 1.03; CI:1.00–1.06) towards an association with risk of relapse, while desire to use cocaine and lack of control over cocaine use were not associated with relapse risk.
For the CCQ-Brief Summary score, the Cox proportional hazard regression model, after controlling for baseline amount of cocaine use, revealed a significant association with time to cocaine relapse (X² = 6.44; p<.02; HR = 1.024; CI: 1.01–1.04).
None of the craving measures (CCQ-Now or CCQ-Brief summary scores, or the specific CCQ-Now subscales) were associated with frequency of use or amount of cocaine used per occasion after the initial relapse.
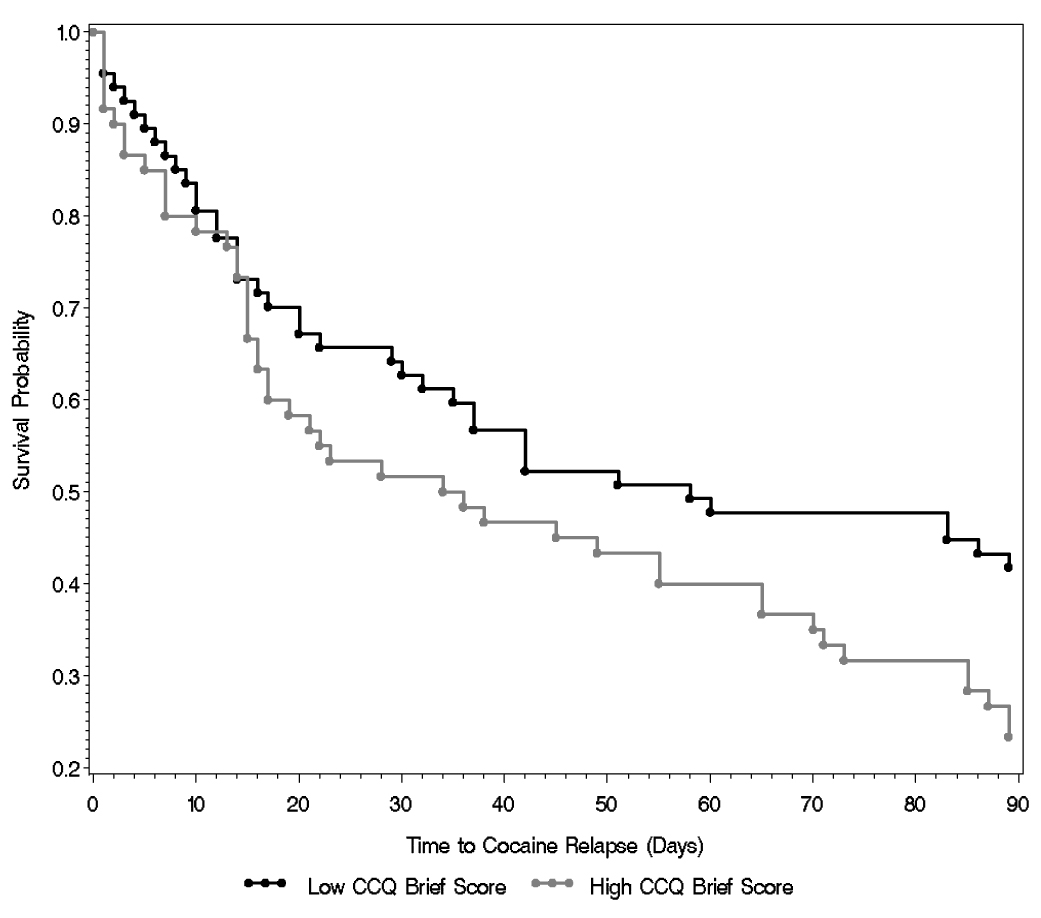
As a follow-up to the proportional hazard analyses, a median split of the CCQ-Now and the CCQ-Brief scales was conducted to divide the sample into high and low craving groups in order to examine the difference in survival probabilities for the two groups. The high craving groups had lower probabilities of survival (and higher probability of relapse) compared to the low craving group based on CCQ-Now summary score (X² = 4.42; p < 0.036) and the CCQ-Brief summary score (X² = 4.197; p < 0.041) (see Figure 1a–1b).
Figure 1.
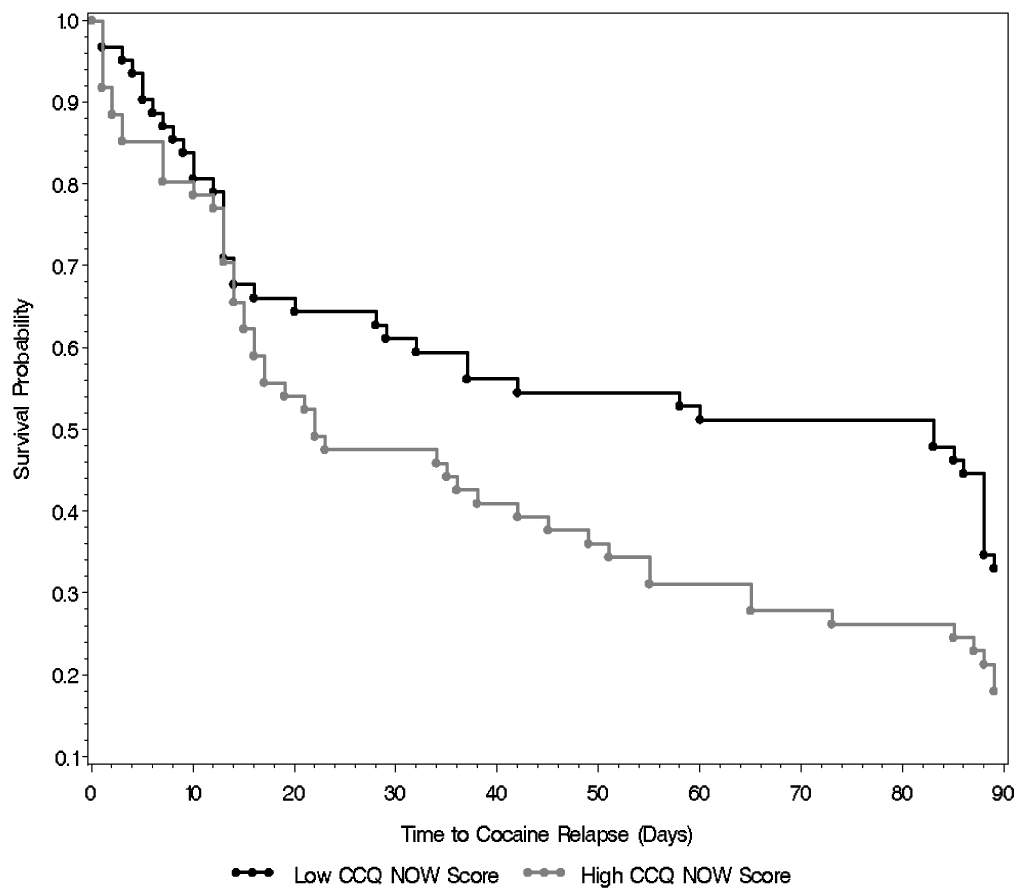
(a) Survival Curves for low (0–130) and high craving (>130) groups based on median split of CCQ-Now summary score. Log-rank test indicates survival curves for two groups are significantly different (X² = 4.42; p < 0.036).
(b) Survival Curves for low (0–19) and high craving (>19) groups based on median split of CCQ-Brief score. Log-rank test indicates survival curves for two groups are significantly different (X² = 4.197; p < 0.041).
A main effect for gender and the interaction between gender and craving were not significant in both analyses. Additionally, there was no difference in average craving levels between men and women.
5. Discussion
Findings from the present study indicate that the CCQ-Brief is a reliable and valid instrument that may be used to provide a comprehensive assessment of cocaine craving in treatment seeking cocaine dependent men and women. The CCQ-Brief also correlated positively with depressive and cocaine abstinence symptomatology, findings which are consistent with studies indicating that stress and negative affect increase cocaine craving (Sinha et al., 1999; Sinha et al., 2000; Sinha et al., 2003; Sinha et al., 2006). Consistent with previous findings (Sussner et al., 2006), the internal consistency of the CCQ-Brief was excellent. CCQ-Brief craving scores were strongly correlated with CCQ-Now craving scores and moderately associated with CSSA craving scores.
More importantly, both the CCQ-Now and the CCQ-Brief summary scores each significantly predicted time to cocaine relapse following discharge from inpatient treatment, thereby supporting the use of either version to assess relapse susceptibility and treatment outcome. For the CCQ-Now scale, for each point increase in the summary score, there was a corresponding 1% increases in relapse risk. For the CCQ-Brief summary score, for each point increase in the CCQ-Brief scores, there was a 3% increased risk of relapse. Upon examination of the specific subscales of the CCQ-Now, both the Anticipation of Positive Outcomes from Cocaine Use (Positive) and the Intent and Planning to Use Cocaine (Intent) subscales significantly predicted relapse risk. Each point increase on these two subscales indicated greater relapse risk by about 2% and 3% respectively. Desire and Lack of Control over Cocaine Use did not significantly predict relapse risk. These data suggest that studies that only assess desire for cocaine using visual analog scales would be using an inadequate measure for assessing cocaine craving and in estimating its effect on treatment outcome. This finding could partially explain why cocaine craving has not been a good indicator of relapse risk in previous studies that measured cocaine craving and desire synonymously using only a few items. From a clinical standpoint, our findings suggest that administering either the 10-item CCQ-Brief or the full CCQ-Now scale could be of benefit in treatment situations. If the goal is to quickly and easily assess relapse risk, the CCQ-Brief would be a more favorable measure. Alternatively, the specific positive outcome and intent/plan subscales may also be further developed to assess relapse susceptibility in clinical situations, but these subscales would need further validation prior to more widespread use.
An important caveat in the use of the CCQ-Now and Brief versions in clinical and research settings is the issue of patient reporting bias. Unlike alcohol and nicotine, cocaine is an illicit substance, and reporting of any intent to use cocaine may be seen by patients as risky with regard to social and clinical consequences. For instance, court mandated individuals may fear that expressing intent and a plan to use cocaine during treatment could be communicated to their probation officers and result in additional mandated treatment or even incarceration. The dominance of abstinence-based approaches in addiction treatment could lead patients to fear that reporting craving and the intent to use cocaine may convey decreased commitment and motivation for treatment and recovery. These psychosocial factors could contribute to the accuracy of reporting craving and intent to use cocaine or any other illicit drugs of abuse. Notably, patients in the current study were admitted to a treatment research unit and informed of the research confidentiality protection, with a clear expectation that reporting of craving or related symptoms would not impact their treatment or other drug related consequences in an adverse manner.
Although time to initial cocaine relapse was found to be significantly associated with the CCQ-Now and the CCQ-Brief summary scores, none of the other drug use outcomes (amount and frequency of use after relapse) were associated with cocaine craving. This finding suggests that cocaine craving is associated with the behavioral aspect of drug relapse, rather than the consummatory or binge aspects of drug use. Amount or frequency of cocaine use following an initial relapse may be more closely related to other factors such as drug availability or level of social tolerance for drug use and even biological markers such as stress or drug related hypothalamic-pituitary adrenal (HPA) responses (Sinha et al., 2006). Our findings are also consistent with Tiffany’s cognitive model of drug use (Tiffany, 1990) where he proposed that, if a drug user’s normal drug using routine is impeded (i.e., while in an inpatient treatment facility), urge responding will be controlled by non-automatic and effortful cognitive processes whereas ongoing drug use behavior will be well learned and automatic. As a consequence, general craving and intention to use a substance would be most strongly associated with latency to initial drug use and amount of effort used to obtain the drug whereas the amount and patterns of ongoing drug use would either show modest or no association with craving or intention to use a drug (Tiffany, 1990).
It is important to note that the CCQ-Now and the CCQ-Brief are self-report instruments and may not reflect actual levels of craving. Since participants were actively seeking treatment, it is possible that they may have reported lower craving ratings than they were actually experiencing. However, given that craving responses were associated with mood state measures and significantly predicted relapse risk, the possibility that participants were minimizing craving reports is unlikely. Another potential limitation of the study is that results may not extend to an outpatient treatment sample or to a more psychiatrically co-morbid sample. Furthermore, variability in length of inpatient stay, while difficult to control, may have influenced the findings. Nevertheless, the findings support the use of the CCQ-Now and Brief versions as multidimensional craving measures that can be used to obtain reliable and valid data on craving in men and women seeking inpatient treatment for cocaine dependence. Findings also support that both versions are good predictors of cocaine relapse risk.
Of particular interest is the finding that having a desire to use cocaine may not be the best predictor of relapse risk. Rather, the strength of one’s intention and plan to use and the expectancy of positive outcome from cocaine use significantly predicts relapse risk. This finding may help explain why craving has historically been a poor indicator of cocaine relapse risk and suggests that using a multidimensional measure such as the CCQ may prove to be a methodological improvement in future studies. Craving assessments that go beyond desire and that take into account intent to use and positive expectancies may improve predictions of relapse for clinical and research purposes. Furthermore, as the pathway from craving to drug-seeking behavior may be modified by factors such as the availability of drugs, social constraints, stress, and exposure to cocaine related stimuli (Tiffany, 1990; Sinha et al., 2006; Wilson et al., 2005) it will be necessary to identify other factors that significantly impact the relationship between drug craving and relapse susceptibility and drug use behaviors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Addolorato G, Abenavoli L, Leggio L, Gasbarrini G. How many cravings? Pharmacological aspects of craving treatment in alcohol addiction: A review. Neuropsychobiology. 2005;51:59–66. doi: 10.1159/000084161. [DOI] [PubMed] [Google Scholar]
- Anton RF. Obsessive-compulsive aspects of craving: development of Obsessive Compulsive Drinking Scale. Addiction. 2000;95 Supplement 3:S211–S217. doi: 10.1080/09652140050111771. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology. Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Bordnick PS, Schmitz JM. Cocaine craving: an evaluation across treatment phases. Journal of Substance Abuse. 1998;10:9–17. doi: 10.1016/s0899-3289(99)80136-9. [DOI] [PubMed] [Google Scholar]
- Cattel RB. The Scientific Use of Factor Analysis in Behavioral and Life Sciences. New York: Plenum Press; 1978. [Google Scholar]
- Cox D. Regression models and life tables (with discussion) Journal of the Royal Statistical Society. B. 1972:187–220. [Google Scholar]
- Doherty K, Kinnunen T, Militello FS, Garvey AJ. Urges to smoke during the first month of abstinence: Relationship to relapse and predictors. Psychopharmacology. 1995;119:171–178. doi: 10.1007/BF02246158. [DOI] [PubMed] [Google Scholar]
- Drummond DC. Conceptualizing addiction: Theories of drug craving, ancient and modern. Addiction. 2001;96:33–46. doi: 10.1046/j.1360-0443.2001.961333.x. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, O'Farrell TJ, Freitas TT, McFarlin SK, Rutigliano P. The Timeline followback reports of psychoactive substance use by drug-abusing patients: Psychometric properties. Journal of Consulting & Clinical Psychology. 2000;68:134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer R, Williams J. User's Guide to the structured clinical interview for DSM-IV axis disorders (SCID-I, Version 2.0) 1995. [Google Scholar]
- Hendrickson AE, White PO. Promax: a quick method for rotation to oblique simple structures. British Journal of Statistical Psychology. 1964;17:65–70. [Google Scholar]
- Hersh D, Mulgrew CL, Van Kirk J, Kranzler HR. The validity of self-reported cocaine use in two groups of cocaine abusers. Journal of Consulting & Clinical Psychology. 1999;67:37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- Kaiser HF. An index for factorial simplicity. Psychometrika. 1974;39:31–36. [Google Scholar]
- Kampman KM, Volpicelli JR, McGinnis DE, Alterman AI, Weinrieb RM, D'Angelo L, Epperson LE. Reliability and validity of the Cocaine Selective Severity Assessment. Addictive Behaviors. 1998;23:449–461. doi: 10.1016/s0306-4603(98)00011-2. [DOI] [PubMed] [Google Scholar]
- Killen J, Fortmann SP. Craving is associated with smoking relapse: findings from three prospective studies. Exp Clin Psychopharmacol. 1997;5:137–142. doi: 10.1037//1064-1297.5.2.137. [DOI] [PubMed] [Google Scholar]
- Kranzler HR, Wallington DJ. Serum prolactin level, craving, and early discharge from treatment in cocaine-dependent patients. American Journal of Drug & Alcohol Abuse. 1992;18:187–195. doi: 10.3109/00952999208992831. [DOI] [PubMed] [Google Scholar]
- Ludwig AM, Wikler A. "Craving" and relapse to drink. Quarterly Journal of Studies on Alcohol. 1974;35:108–130. [PubMed] [Google Scholar]
- Mello NK. A semantic aspect of alcoholism. In: Cappell HD, LeBlanc AE, editors. Biological and Behavioral Approaches to Drug Dependence. Toronto: Addiction Research Foundation; 1978. pp. 73–87. [Google Scholar]
- Mercer D, Carpenter G, Daley D, Patterson C, Volpicelli J. Group drug counseling manual. University of Pennsylvania; 1994. In: Unpublished Manuscript. [Google Scholar]
- Miller NS, Gold MS. Dissociation of "conscious desire" (craving) from and relapse in alcohol and cocaine dependence. Annals of Clinical Psychiatry. 1994;6:99–106. doi: 10.3109/10401239409148988. [DOI] [PubMed] [Google Scholar]
- Miller WR, DelBoca FK. Measurement of drinking behavior using the Form 90 family of instruments. Journal of Studies on Alcohol. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- O'Brien CP, Volpicelli LA, Volpicelli JR. Naltrexone in the treatment of alcoholism: a clinical review. Alcohol. 1996;13:35–39. doi: 10.1016/0741-8329(95)02038-1. [DOI] [PubMed] [Google Scholar]
- Piasecki TM. Relapse to smoking. Clinical Psychological Review. 2006;26:196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Robbins SJ, Ehrman RN. Cocaine use is associated with increased craving in outpatient cocaine abusers. Experiments in Clinical Psychopharmacology. 1998;6:217–224. doi: 10.1037//1064-1297.6.2.217. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM. Does urge to drink predict relapse after treatment? Alcohol Research and Health. 1999;23:225–232. [PMC free article] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM. Relapse among cocaine abusers: Theoretical, methodological, and treatment considerations. In: Platt JJ, Henkegend CG, editors. Relapse and Recovery in Addictions. New Haven: Yale University Press; 2001. pp. 355–378. [Google Scholar]
- Rohsenow DJ, Niaura RS, Childress AR, Abrams DB, Monti PM. Cue reactivity in addictive behaviors: Theoretical and treatment implications. International Journal of the Addictions. 1991;25:957–993. doi: 10.3109/10826089109071030. [DOI] [PubMed] [Google Scholar]
- Sayette MA, S S, Tiffany ST, Niaura RS, Martin CS, Shadel WG. The measurement of drug craving. Addiction. 2000;95 Supplement 2 doi: 10.1080/09652140050111762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shiffman S, Engberg J, Paty JA, Perz WG, Gnys M, Kassel JD, Hickcox M. A day at a time: predicting smoking lapse from daily urge. Journal of Abnormal Psychology. 1997;106:104–116. doi: 10.1037//0021-843x.106.1.104. [DOI] [PubMed] [Google Scholar]
- Singleton EG, Gorelick DA. Mechanisms of alcohol craving and their clinical implications. In: Galanter M, editor. Recent Developments in Alcoholism: The Consequences of Alcoholism. vol.14. New York: Plenum Press; 1998. pp. 177–195. [DOI] [PubMed] [Google Scholar]
- Sinha R, Catapano D, O'Malley S. Stress-induced craving and stress response in cocaine dependent individuals. Psychopharmacology (Berl) 1999;142:343–351. doi: 10.1007/s002130050898. [DOI] [PubMed] [Google Scholar]
- Sinha R, Fuse T, Aubin LR, O'Malley SS. Psychological stress, drug-related cues and cocaine craving. Psychopharmacology (Berl) 2000;152:140–148. doi: 10.1007/s002130000499. [DOI] [PubMed] [Google Scholar]
- Sinha R, Garcia M, Paliwal P, Kreek MJ, Rounsaville BJ. Stress-induced cocaine craving and hypothalamic-pituitary-adrenal responses are predictive of cocaine relapse outcomes. Archives of General Psychiatry. 2006;63:324–331. doi: 10.1001/archpsyc.63.3.324. [DOI] [PubMed] [Google Scholar]
- Sinha R, Talih M, Malison R, Anderson GA, Cooney N, Kreek M. Hypothalamic-pituitary-adrenal axis and sympatho-adreno-medullary responses during stress-induced and drug cue-induced cocaine craving states. Psychopharmacology (Berl) 2003;170:62–72. doi: 10.1007/s00213-003-1525-8. [DOI] [PubMed] [Google Scholar]
- Smelson DA, Losonczy MF, Davis CW, Kaune M, Williams J, Ziedonis D. Risperidone decreases craving and relapses in individuals with schizophrenia and cocaine dependence. Canadian Journal of Psychiatry. 2002;47:671–675. doi: 10.1177/070674370204700710. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback User's Guide: A Calendar Method for Assessing Alcohol and Drug Use. Toronto, Ontario, Canada: Addiction Research Foundation; 1996. [Google Scholar]
- Sussner BD, Smelson DA, Stephanie R, Kline A, Losonczy MF, Ziedoni D. The validity and reliability of a brief measure of cocaine craving. Drug and Alcohol Dependence. 2006;83:233–237. doi: 10.1016/j.drugalcdep.2005.11.022. [DOI] [PubMed] [Google Scholar]
- Tiffany S. A cognitive model of drug urges and drug-use behavior: The role of automatic and non-automatic processes. Psycholog Rev. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tiffany ST, Singleton E, Haertzen CA, Henningfield JE. The development of a cocaine craving questionnaire. Drug and Alcohol Dependence. 1993;34:19–28. doi: 10.1016/0376-8716(93)90042-o. [DOI] [PubMed] [Google Scholar]
- Weiss R, Griffin ML, Mazurik C, Berkman B, Gastfriend DR, Frank A, Barber JP, Blaine J, Salloum I, Moras K. The relationship between cocaine craving, psychosocial treatment and subsequent cocaine use. Am J Psychiatry. 2003;160:1320–1325. doi: 10.1176/appi.ajp.160.7.1320. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Hufford C. Craving in hospitalized cocaine abusers as a predictor of outcome. American Journal of Drug & Alcohol Abuse. 1995;21:289–301. doi: 10.3109/00952999509002698. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Hufford C, Muenz LR, Najavits LM, Jansson SB, Kogan J, Thompson HJ. Early prediction of initiation of abstinence from cocaine. American Journal on Addictions. 1997;6:224–231. [PubMed] [Google Scholar]
- Wilson S, Sayette M, Delgado M, Fiez J. Instructed smoking expectancy modulates cue-elicited neural activity: a preliminary study. Nicotine and Tobacco Research. 2005;7:637–645. doi: 10.1080/14622200500185520. [DOI] [PMC free article] [PubMed] [Google Scholar]


