Abstract
The objectives of this pilot study were to assess the feasibility of recruitment and adherence to an eight-session mindfulness meditation program for community-dwelling older adults with chronic low back pain (CLBP) and to develop initial estimates of treatment effects. It was designed as a randomized, controlled clinical trial. Participants were 37 community-dwelling older adults aged 65 years and older with CLBP of moderate intensity occurring daily or almost every day. Participants were randomized to an 8-week mindfulness-based meditation program or to a wait-list control group. Baseline, 8-week and 3-month follow-up measures of pain, physical function, attention, and quality of life were assessed. Eighty-nine older adults were screened and 37 found to be eligible and randomized within a 6-month period. The mean age of the sample was 74.9 years, 21/37 (57%) of participants were female and 33/37 (89%) were white. At the end of the intervention 30/37 (81%) participants completed 8-week assessments. Average class attendance of the intervention arm was 6.7 out of 8. They meditated an average of 4.3 days a week and the average minutes per day was 31.6. Compared to the control group, the intervention group displayed significant improvement in the Chronic Pain Acceptance Questionnaire Total Score and Activities Engagement subscale (P = .008, P = .004) and SF-36 Physical Function (P = .03). An 8-week mindfulness-based meditation program is feasible for older adults with CLBP. The program may lead to improvement in pain acceptance and physical function.
1. Introduction
Among older adults, chronic pain is a common condition that can have devastating consequences. Chronic pain is associated with depression (Fishbain, Cutler et al. 1997; Bair, Robinson et al. 2003) decreased appetite (Bosley, Weiner et al. 2004), impaired sleep (Benca, Ancoli-Israel et al. 2004) and overall decreased quality of life (Cooper and Kohlmann 2001). Not surprisingly, approximately 1/4-1/3 of older adults suffer from low back pain (Urwin, Symmons et al. 1998; Thomas, Peat et al. 2004). Many older adults’ chronic pain is inadequately treated (Roy 1987; Woo, Ho et al. 1994). This may be due to older adults increased susceptibility to medication side effects and increased number of co-morbidities that prohibit surgical interventions (Gagliese and Melzack 1997).
Approximately 1/3 of older adults have used complementary and alternative medicine (CAM) in the previous year (Foster, Phillips et al. 2000). Chronic pain is one of the top medical conditions for which they seek CAM modalities (Foster, Phillips et al. 2000; Astin 2004). The growing use of CAM presents researchers with the responsibility of studying it scientifically. We were interested in studying a mind-body technique called mindfulness meditation for the treatment of chronic pain in older adults.
Mindfulness meditation was introduced as a clinical intervention for conditions such as chronic pain and anxiety in 1979 (Kabat-Zinn 1982; Kabat-Zinn, Massion et al. 1992). It is currently taught and studied in many clinical trials as the Mindfulness-Based Stress Reduction Program (MBSR) (Kabat-Zinn 1990; Kabat-Zinn 2003). Previous research of Kabat-Zinn showed a significant reduction of chronic pain among 90 patients with a variety of chronic pain conditions (Kabat-Zinn, Lipworth et al. 1985). He then published 4-year follow-up data showing maintenance of pain improvement among 60-72% of 225 chronic pain patients (Kabat-Zinn, Lipworth et al. 1986). The studies did not include a comparison group. Sustained pain reduction up to 4-months after the MBSR intervention was noted in 28 fibromyalgia patients (Creamer, Singh et al. 2000). In a different study, fibromyalgia patients were randomized to an MBSR or an education program, both groups showed improvement in pain self-report, but the differences between the two groups did not reach statistical significance (Astin, Berman et al. 2003). None of these studies targeted older adults or chronic low back pain (CLBP). It is not known if older adults would differ from a younger population in terms of program adherence and effects. A recent review supports the use of meditation training in the older adult (Lindberg 2005; Morone and Greco 2007).
Kabat-Zinn states mindfulness is: “the awareness that emerges through paying attention on purpose, in the present moment, and nonjudgmentally to the unfolding of experience moment by moment” (Kabat-Zinn 2003).
The primary aim of this pilot study was to assess the feasibility of recruitment and adherence to an eight-session mindfulness meditation program for community-dwelling older adults ≥ age 65 with CLBP. The secondary aim was to develop initial estimates of treatment effects on measures of pain, physical function and quality of life.
2. Methods
2.1. Overview
This pilot feasibility study was designed as a randomized wait-list controlled trial of mindfulness meditation for CLBP. Eligibility was determined by self-report from a checklist reviewed with potential participants over the telephone. Prior to the intervention study participants completed informed consent procedures and baseline study measures were obtained. After consent and baseline measures, eligible participants were randomized to the intervention or to the control group. Participants in the intervention group received eight weekly 90-minute mindfulness meditation sessions and meditation homework assignments. Attendance was taken at every session. Controls did not receive any intervention during this time. Once the intervention was completed and participants and wait-list controls completed all post-intervention measures the mindfulness meditation program was offered to the wait-list controls. The controls were crossed over into the meditation program immediately after the intervention group finished the 8-week program. The reason for the immediate cross-over design was to minimize dropouts from the control group. Three months after all participants had undergone the 8-week program, they were asked to complete all of the measures a third time and any mindfulness meditation they continued to do at home was quantified. The study was approved by the University of Pittsburgh Institutional Review Board.
2.2. Subjects
Community-dwelling older adults were recruited from an adult pain clinic, flyers posted around the University of Pittsburgh Medical Center and newspaper advertisements. All participants were included if they 1) were 65 years of age or older, 2) had intact cognition (Mini-Mental Status Exam (MMSE) ≥ 23), 3) had CLBP, defined as moderate pain occurring daily or almost every day for at least the previous three months, and 4) spoke English. They were excluded if they 1) had previously participated in a mindfulness meditation program, and 2) had “red flags” suggestive of serious underlying illness (e.g. malignancy, infection, unexplained fever, weight loss or recent trauma) causing their pain.
A broad age range (≥ 65) and few exclusion criteria of participants with CLBP were selected to permit study of the effect of the intervention on a representative sample of community-dwelling older adults, increasing the generalizability of the study findings.
2.3. Intervention
2.3.1. Frequency and Setting
Participants were seen in a group format once a week for 90 minutes for eight weeks. Two of the investigators (NM and CG) led all sessions. They had a combined experience of 30 years in mindfulness meditation and had each undergone teacher training in an MBSR program for health professionals directed by staff from the Center for Mindfulness (such as Kabat-Zinn) prior to the intervention.
2.3.2. Program Techniques
The intervention was modeled on the work of Jon Kabat-Zinn and the MBSR program he pioneered at the University of Massachusetts Medical Center (Kabat-Zinn 1990). Three techniques of mindfulness meditation were taught. These techniques take regular activities such as sitting, walking and lying down and transform them into a meditation through directed breathing and mindful awareness of thoughts and sensations.
The techniques used were: 1) the body scan, where in a lying position, the participant is guided to place their attention non-judgmentally on each area of the body from the toes to the top of the head, 2) sitting practice, which is focused attention on breathing while sitting on a chair or on a meditation cushion on the floor, 3) walking meditation, which is mindful slow walking with focused attention on body sensation and/or breathing.
Several attitudes that support mindfulness meditation were emphasized throughout the eight classes. These were patience, non-judging, “beginner’s” mind, acceptance, letting go, non-striving and trust, see reference for further details (Kabat-Zinn 1990).
2.3.3. Program Protocol
During the first week participants were introduced to the principles and practice of mindfulness meditation. The homework recommendation of daily meditation (six of seven days/week) lasting 50 minutes (45 minutes of meditation, 5 minutes to complete a diary) were reviewed. Support materials of audiotape, daily diary and reading materials were provided. The audiotape was a guided 45 minute recording of the steps in the body scan meditation on one side and a guided 30 minute recording of sitting meditation on the other side. The reading materials were reviewed during the sessions and were not a part of the homework. The body scan technique was taught at the first session. If physical discomfort arose during any meditation practice, participants were encouraged to change to a more comfortable position.
During the second and following weeks the sessions included a general discussion of the participants’ experience with the meditation technique, including problem solving regarding obstacles to the meditation practice. Theoretical material related to meditation, pain, stress and the mind/body connection were presented during these sessions. Approximately 45 minutes were spent at each session in these discussions. Also during the second week, quiet sitting meditation was introduced. The group practiced together using the sitting meditation technique for approximately 15 minutes during the second session and at the beginning of all subsequent sessions.
At the fifth week’s session, walking meditation was introduced. Therefore, the structure of each session was approximately 45 minutes of meditation and 45 minutes of discussion. We did not include a yoga component or an all-day silent retreat that are usual components of an MBSR program. This was for practical reasons: we did not have a fully developed yoga program that would be safe for all participants to do, and due to time limitations did not offer the full-day retreat.
2.4. Outcome Measures
Measures were obtained pre-randomization by NM. Post-intervention and 3-month follow-up measures were obtained by a research assistant trained in their administration and masked to group assignment. Because this was a preliminary study we were exploring participant outcomes on a variety of outcome measures. As a result, we do not consider any one of the outcome measures as primary. Rather, we were interested in which measures had at least a minimal effect size which would be used to calculate sample size in future planned studies. All of the following outcome measures were obtained at three time points for the intervention group: before randomization, immediately after the eight-week intervention, and 3-months later. All of the following measures were also obtained for the control group at four time points: before randomization, immediately after the 8-week active intervention group period, immediately after the control group had completed the 8-week program, and three months after the control group had completed the program.
2.4.1. Pain intensity was assessed with two measures: the McGill Pain Questionnaire Short Form (MPQ-SF) (Melzack 1987), that has reliability and validity in an older population (Helme, Katz et al. 1989) with lower scores indicating less pain. Pain was also measured with the SF-36 Pain scale (Hays, Prince-Embury et al. 1998) with higher scores indicating less pain.
2.4.2. Pain acceptance was measured with the Chronic Pain Acceptance Questionnaire (CPAQ) (McCracken, Vowles et al. 2004), that has been shown to correlate with reports of lower pain and greater physical function (McCracken, Carson et al. 2004). The Activity Engagement subscale was separately analyzed but not the Pain Willingness subscale as the former is a more robust predictor of pain-related outcomes (Nicholas and Asghari 2006). Improvement is reflected in higher scores.
2.4.3. Quality of life (QOL) was measured with the SF-36 Health Status Inventory (Hays, Prince-Embury et al. 1998). The three summary scores (Global, Physical and Mental Health), and the scales for Pain and Physical Function were included. Higher scores reflect improvement.
2.4.4. Physical function was measured using three scales: the Roland and Morris Questionnaire (Roland and Morris 1983) that assesses self-reported disability related to low back pain with lower scores indicating less disability. It has good reliability and validity in community dwelling older adults with CLBP (Weiner, Pieper et al. 1996). The second scale used was the Short Physical Performance Battery (Guralnik, Simonsick et al. 1994) that measures standing balance, gait speed and ability to rise from a chair. It has been shown to predict disability in community dwelling older adults (Guralnik, Ferrucci et al. 2000). The third scale used was the SF-36 Physical Function scale with higher scores indicating improved physical function.
2.4.5. Follow-up at 3-months to assess continued meditation practice and feedback on the program was also obtained with a short questionnaire (available from authors). Participants were asked if they continued to meditate, and if so how often. They were asked if they slept or concentrated better after the class and if they had recommended the class to others. They were also asked to give general feedback or comments on the program.
2.5. Statistical Methods
Sample Size
Formal sample size calculation was not performed due to the pilot feasibility nature of the study. Sample size was calculated based on the proportion of subjects expected to complete the program. We estimated that approximately 70% of participants would complete the 8-week program (26/37 participants would have adequately met an adherence standard of attending 75% of the 8 weekly sessions or, if randomized to the wait-list control group, sufficient number of participants would be available to complete the follow-up measures) (Kabat-Zinn, Lipworth et al. 1986; Astin, Berman et al. 2003). We calculated the confidence interval around the 70% proportion of subjects completing the program and found that it was 14%. Thus, with a sample size of 37 individuals 56%-84% of participants would be expected to complete the study.
Randomization
Participants were randomized in blocks of 6 with no stratification using a software generated randomization plan. Randomization assignment was kept in opaque, sealed envelopes and handed out sequentially to participants after consent and baseline measures were obtained.
Data Analysis
Descriptive statistics for the sample as a whole and the two groups were generated and the two groups compared with the chi square test for dichotomous variables and the two-sample t-test for continuous variables. In the estimation of effect sizes the outcome variables of interest were pain, physical function, attention and QOL. Our main independent variable was patient group. An intention-to-treat approach using last value carried forward was used in all analysis and included all randomized participants even if they were lost to follow-up or dropped out of the study. All variables were tested for normality. Change scores were generated between the pre-intervention measures and the post-intervention measures for the meditation group and control group and a two sample t-test was used to establish the significance of change between the meditation and control groups. We did not use MANOVA because we were interested in the individual results for each measure given the pilot nature of this study. A 3-month follow-up analysis was done on the intervention group only since the comparison group was no longer available as they had been crossed over into the meditation program. We used a one-sample t-test for the 3-month follow-up analysis. Cohen’s d was used to calculate the effect size difference between meditation and control groups. Analysis was done with Stata statistical software, version 8 (Stata Corp., College Station, TX). The data obtained from the control group after they had crossed-over and completed the MBSR program was analyzed with repeated measures ANOVA and missing values imputed by carrying the last value forward. The most proximal pre-treatment data from the control group was used to evaluate the effects of the mindfulness meditation program.
3. RESULTS
3.1. Recruitment and Follow-up of Participants
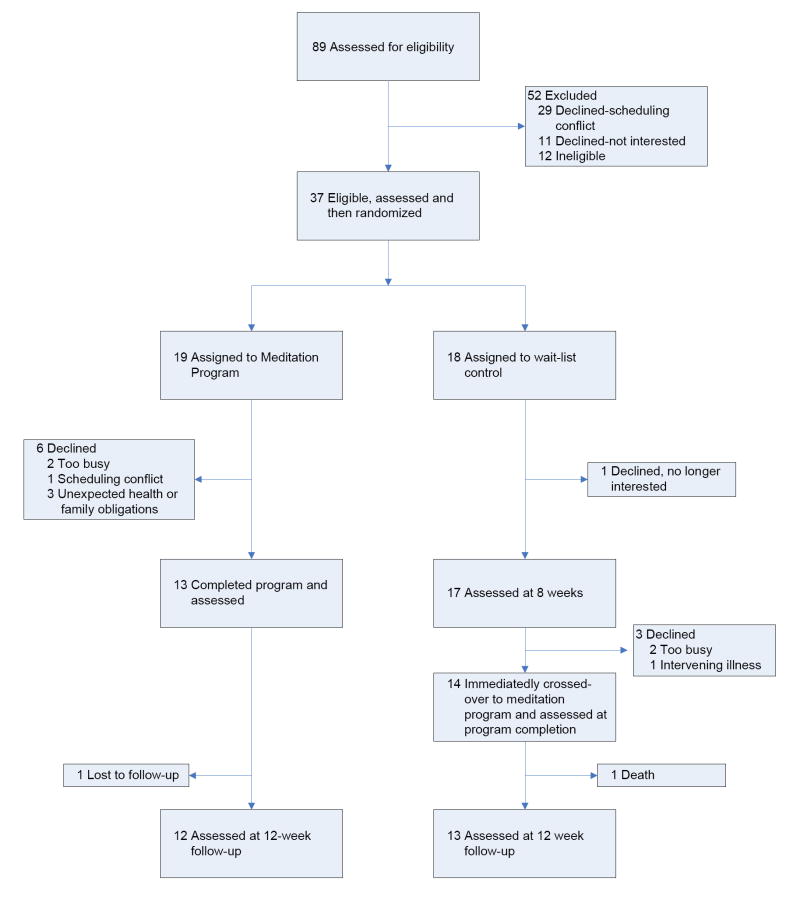
Eighty-nine subjects responded to posted flyers or ads and were assessed for eligibility (see figure 1 for trial profile). Thirty-seven were enrolled in the study between May and October 2004. Those who were not enrolled were ineligible, had scheduling conflicts with the day and time of the program or were not interested. Nineteen were randomized to the meditation intervention group and eighteen to the wait-list control group. Thirteen participants completed the 8-week program and were available for assessment. Seventeen subjects in the wait-list control group were available for assessment at week eight. Twelve subjects were available for 3-month follow-up in the meditation intervention group. Thirteen subjects from the control group crossed over and completed the 8-week meditation program and completed 3-month follow-up measures.
Figure 1.
Participant flow diagram
3.2. Baseline Characteristics
The two groups did not differ significantly on demographic factors of age, gender, ethnicity, education, religion, income and marital status as displayed in Table 1. The mean age of the study participants was 75 years (range 65-84), 22 (59%) of the participants had at least some college education and 24 (65%) made $50,000 or less.
Table 1.
Demographic Characteristics of Study Participants
| Treatment Condition
|
|||
|---|---|---|---|
| Variable | Meditation
n=19 |
Control
n=18 |
P-value |
| Age, mean ± SD | 74.1 ± 6.1 | 75.6 ± 5.0 | .41 |
| Gender, n | |||
| Male | 9 | 7 | .63 |
| Female | 10 | 11 | |
| Ethnicity, n | |||
| White | 17 | 16 | .98 |
| African American | 1 | 1 | |
| Asian | 1 | 1 | |
| Education, n | |||
| High School Graduate | 5 | 5 | .96 |
| Technical School | 2 | 3 | |
| Some College | 3 | 2 | |
| College | 6 | 4 | |
| Master’s or greater | 3 | 4 | |
| Religion, n | |||
| Catholic | 10 | 8 | .97 |
| Jewish | 6 | 7 | |
| Protestant | 2 | 2 | |
| Other | 1 | 1 | |
| Income, n | |||
| $10,000-$19,999 | 4 | 5 | .80 |
| $20,000-$29,999 | 2 | 1 | |
| $30,000-$39,999 | 3 | 6 | |
| $40,000-49,999 | 2 | 1 | |
| $50,000-$59,999 | 0 | 0 | |
| $60,000-$69,999 | 1 | 1 | |
| Marital status, n | |||
| Single | 1 | 2 | .22 |
| Married | 14 | 9 | |
| Separated/divorced | 0 | 3 | |
| Widowed | 4 | 4 | |
| Low back pain cause, n | |||
| Osteoarthritis | 17 | 16 | .26 |
| Injury | 0 | 1 | |
| Fibromyalgia | 0 | 1 | |
| Not sure | 2 | 0 | |
| Medications, n | |||
| Opioids | 4 | 3 | .84 |
| Other analgesics | 13 | 12 | |
| None | 2 | 3 | |
| *CAM use in last year, n | |||
| Yes | 8 | 10 | .86 |
| No | 9 | 10 | |
| Folstein Mini-Mental State | |||
| Examination, mean ± SD | 29.2 ±1.1 | 29.3 ± .7 | .56 |
CAM = Complementary and Alternative Medicine; SD = standard deviation. Use of any one or more of the following CAM treatments in the previous 12 months for any reason: acupuncture/acupressure, chiropractic, herbal medicine, yoga, tai chi, homeopathy, magnets, guided imagery or relaxation techniques such as progressive muscle relaxation.
3.3. Adherence
Six subjects dropped out of the intervention group and one subject from the wait-list control group, resulting in an overall completion rate of 81% (30/37) at 8-weeks. In the intervention group, two dropped out before the class started, three dropped out due to unexpected health or family obligations, and one due to a scheduling conflict. Dropouts were less educated than program completers (P = .05), but otherwise did not significantly differ in age, ethnicity, income, marital status or religion (P > .05). The completion rate of the mindfulness program for the intervention group was 68% (13/19). The completion rate for the control group after they crossed-over to the MBSR program was 78% (14/18).
The average number of classes attended by the intervention group was 6.7 (range 5-8). The average number of days per week they meditated was 4.3 (range 0-7) and the average minutes per day meditated was 31.6 (range 0-52).
3.4. Post-Intervention Outcomes
Table 2 compares the intervention and control groups change scores on study measures completed before and after the 8-week program. None of the baseline measures were significantly different from each other between the intervention and control groups. Although on visual inspection some of the baseline measures appear quite different from each other, because of the large variance in this small sample, they are not statistically different.
Table 2.
Comparison of the Effects of Meditation versus Wait-List Control in Outcomes During the 8-Week Trial and 3-Month Follow-Up
| Outcome
Measure |
Groupa | Baseline
mean ± SD |
8-Week
mean ± SD |
Effect Size db | P-
value |
3-Month follow-up,
meditation group only mean ± SD |
|---|---|---|---|---|---|---|
| Pain | ||||||
| McGill Pain
Questionnaire- Short Formc |
Meditation | 15.5 ± 10.0 | 13.7 ± 7.9 | 0.32 | 0.16 | 16.5 ± 11.6 d |
| Control | 15.2 ± 7.0 | 15.7 ± 9.1 | ||||
| SF-36
Pain Scale |
Meditation | 35.5 ± 6.0 | 39.9 ± 7.7 | 0.16 | 0.31 | 39.9 ± 8.4 d |
| Control | 35.7 ± 7.2 | 38.8 ± 8.3 | ||||
| Physical Function | ||||||
| Roland
Disability Questionnairec |
Meditation | 11.5 ± 3.7 | 9.4 ± 5.1 | 0.35 | 0.25 | 8.9 ± 5.7 d |
| Control | 11.8 ± 4.6 | 10.6 ± 5.3 | ||||
| SF-36
Physical Function Scale |
Meditation | 42.0 ± 10.9 | 45.7 ± 9.2 | 0.46 | 0.03 | 45.8 ± 11.5 d |
| Control | 45.1 ± 9.5 | 44.5 ± 10.1 | ||||
| Pain Acceptance | ||||||
| Chronic Pain
Acceptance Questionnaire Total Score |
Meditation | 72.2 ± 13.4 | 75.5 ± 16.0 | 0.83 | 0.008 | 74.5 ±15.9 d |
| Control | 68.1 ± 20.3 | 64.8 ± 23.0 | ||||
| Chronic Pain
Acceptance Questionnaire Activities Engagement |
Meditation | 47.7 ± 8.9 | 50.3 ± 12.3 | 0.95 | 0.004 | 48.1± 9.4 d |
| Control | 47.9 ± 12.3 | 43.4 ± 13.5 | ||||
| Quality of Life | ||||||
| SF-36
Physical Health Composite |
Meditation | 41.4 ± 8.7 | 43.9 ± 8.4 | 0.13 | 0.36 | 44.6 ± 10.4 d |
| Control | 41.2 ± 6.8 | 42.9 ± 9.0 | ||||
| SF-36
Global Health Composite |
Meditation | 40.4 ± 9.0 | 44.7 ± 8.9 | 0.21 | 0.27 | 43.9 ± 9.8 d |
| Control | 40.3 ± 10.4 | 42.9 ± 10.7 | ||||
| SF-36
Mental Health Composite |
Meditation | 41.7 ± 11.3 | 45.7 ± 10.3 | 0.17 | 0.30 | 45.1 ± 11.2 d |
| Control | 40.8 ± 13.7 | 43.2 ± 12.4 |
Meditation n = 19, control n= 18.
d=M t -M c / σpooled. M t = mean change score for the treatment group, M c = mean change score for the control group, , σt = standard deviation of change score for treatment group, σc = standard deviation of change score for control group.
Lower scores indicate improvement.
No statistically significant difference (P>.05) between 8-week and 3-month scores with one sample t-test.
Pain acceptance as measured with the Chronic Pain Acceptance Questionnaire total score significantly improved for the meditation group while the control group worsened over the 8-week period (P =.008). The Activities Engagement subscale of the CPAQ was also significantly improved (P = .004).
Mean pain scores changed in the expected direction for the meditation group as compared to the control group at 8-week follow-up for the McGill Pain Questionnaire and SF-36 Pain Scale, though not significantly.
Physical function showed significant improvement for the meditation group (P =.03) in the Physical Function Scale of the SF-36. Disability due to low back pain as measured by the Roland Disability Questionnaire changed in the expected direction for the meditation group as compared to the control group but this change did not reach statistical significance. There was no significant change between the two groups on the Short Physical Performance Battery on the Mann-Whitney U test at 8-weeks. Because of space considerations these data are not included in the outcome tables.
QOL as reflected in the summary scores and scales of the SF-36 were not improved to a statistically significant extent (P>.05) relative to the control group, but changes in each scale were in the expected direction for the MBSR group.
3.5. Completers Analysis
Statistical analysis of only those intervention participants who completed the program was also done. The results did not vary from the intention-to-treat analysis. The CPAQ, CPAQ Activity Engagement subscale and Physical Function scale of the SF-36 remained significant (P = .008, .005, .02 respectively), while the other measures were not significant (P > .05).
No serious adverse events were reported.
3.6. 3-Month Follow-up
Of the 13 participants in the intervention group who completed the 8-week program 12 were available for 3-month follow-up (one was lost to follow-up). Table 2 shows 3-month follow-up scores for the intervention group only as the control group was no longer available for comparison since they had been crossed over into the meditation program. There was no significant difference between the 8-week and 3-month scores for any of the measures. Of the 14 participants in the wait-list control group who were crossed over into the 8-week program, 13 were available for the follow-up three months after they had completed the cross-over program (one died of natural causes at home).
3.7. Control Subjects Who Completed MBSR
Table 3 presents the data from the control group after they had crossed over into the mindfulness meditation program. These data are presented because of the exploratory nature of the clinical trial and allows the reader to evaluate the changes in this group independently of the intervention group. All the measures were in the expected direction at 8-weeks but did not reach statistical significance. Although the McGill Pain Questionnaire, Chronic Pain Acceptance Questionnaire Total Score and Activities Engagement subscale trended toward improvement as compared to the participants’ pre-intervention scores. A significant improvement at 3-months is seen in the McGill Pain Questionnaire but not in the other measures.
Table 3.
Outcomes for the Wait-List Control Group After They Completed the Mindfulness Meditation Program at 8-Weeks and 3-Months Follow-Up
| Outcome
Measure |
Baselinea mean ± SD n=18 |
8-Week
mean ± SD n=18 |
3-Month
mean ± SD n=18 |
P-Value
Baseline to 8-Weeks |
P-Value
Baseline to 3-Months |
|---|---|---|---|---|---|
| Pain | |||||
| McGill Pain
Questionnaire- Short Formb |
15.7 ± 9.1 | 12.4 ± 8.5 | 11.4 ± 6.5 | 0.098 | 0.03 |
| SF-36
Pain Scale |
38.8 ± 8.3 | 41.0 ± 10.0 | 39.5 ± 8.4 | 0.16 | 0.66 |
| Physical Function | |||||
| Roland
Disability Questionnaireb |
10.6 ± 5.3 | 8.8 ± 6.5 | 9.4 ± 5.5 | 0.17 | 0.35 |
| SF-36
Physical Function Scale |
44.5 ± 10.1 | 45.8 ± 9.3 | 46.8 ± 10.7 | 0.38 | 0.11 |
| Pain Acceptance | |||||
| Chronic Pain
Acceptance Questionnaire Total Score |
64.8 ± 23.0 | 69.3 ± 20.9 | 68.0 ± 16.8 | 0.07 | 0.19 |
| Chronic Pain
Acceptance Questionnaire Activities Engagement |
43.4 ± 13.5 | 47.2 ± 14.2 | 42.7 ± 11.5 | .057 | 0.71 |
| Quality of Life | |||||
| SF-36
Physical Health Composite |
42.9 ± 9.0 | 44.7 ± 9.5 | 43.9 ± 9.0 | 0.21 | 0.50 |
| SF-36
Global Health Composite |
42.9 ± 10.7 | 45.3 ± 10.9 | 42.2 ± 9.6 | 0.17 | 0.67 |
| SF-36
Mental Health Composite |
43.2 ± 12.4 | 45.4 ± 12.1 | 41.5 ± 10.7 | 0.30 | 0.42 |
The most proximal pre-treatment data was used as the control group’s baseline.
Lower scores indicate improvement.
3.8 Meditation Adherence and Self-Reported Benefits at 3 Month Follow-up
There were a total of 25 participants who completed the 3-month follow-up questions, including 12 from the immediate intervention group and 13 crossed-over wait-list controls. Nineteen (76%) of the participants reported that they continued to meditate, 18 (72%) had recommended the class to others, 16 (64%) reported they could “concentrate better” and 12 (48%) reported taking less medication for pain or sleep.
4.0 DISCUSSION
This is the first published study to show the feasibility of an 8-week mindfulness-based meditation program for older adults with CLBP. Other studies of MBSR have included older adults, but the mean age is much younger. A recent review of mindfulness-based interventions reported the mean age for 18 studies ranged from 38-51 years (Baer 2003). In this pilot study, not only were older adults interested in meditation, with recruitment requiring only six months, but they were enthusiastic about the program, attended most of the classes and adhered to the daily meditation homework assignments. The program appeared to have a beneficial effect on pain acceptance and physical function as measured by the CPAQ and SF-36 Physical Function scale. Additionally, the majority of participants continued to meditate at 3-month follow-up, suggesting they found enough benefit in meditation to continue it on their own.
This study adds to previous studies on the possible benefits of the MBSR program to reduce chronic pain (Kabat-Zinn 1982; Kabat-Zinn, Lipworth et al. 1985; Kabat-Zinn, Lipworth et al. 1986; Randolph, Tacone et al. 1999; Creamer, Singh et al. 2000). It is also consistent with the early work of Kabat-Zinn who found significant improvements in measures of pain and psychological function in subjects with varied chronic pain conditions and a large age range. We particularly view acceptance of pain as measured by the CPAQ as an important outcome. There is growing evidence for acceptance-based approaches to suffering vs. control or avoidance techniques (McCracken, Carson et al. 2004). Letting go of struggle and accepting one’s condition without judgment is a critical concept in the MBSR program. Other non-pharmacologic approaches to pain management also teach patients how to “live” with pain, but may not place as much emphasis on the concepts of letting go or acceptance. This approach was easily grasped by participants and encouraged them to take a fresh look at their pain condition. This may have led them to change their behavior or perception of pain, which may have resulted in improvement of their pain experience. A program participant stated it best “Mindfulness meditation has a quieting effect on me. It gives me a peaceful feeling while doing it and I am able to reduce my back and leg pain by deflecting the pain and by focusing on other parts of my body”. Interestingly, there is evidence from EEG studies that meditation can result in a shift to a more positive affect (Davidson, Kabat-Zinn et al. 2003).
We believe the lower completion rate in the intervention group (i.e., 68%) was largely due to factors not related to the intervention itself. This is because two participants never attended any classes and 3 had unexpected health or family obligations. Taking this into consideration, if we exclude the two participants who dropped out before the 8-week program began the true dropout rate was 4/17 (24%) for a completion rate of 76%. We cannot state with certainty that the other three participants simply gave the excuse of unexpected health or family obligations to please the investigators. However, two of these participants gave detailed descriptions of their obligations. This is not an unusual scenario in the older adult population, and we will take this into consideration when determining sample size for future planned studies. Because of the pilot nature of this study we were constrained by the day of the week and time of day we could offer the MBSR program. This also impacted both recruitment and dropouts, since scheduling conflicts came up frequently as a barrier to recruitment and was one of the reasons cited for discontinuing the program. A future larger trial will offer more scheduling flexibility. Other potential reasons for the differential dropout rate between the intervention and control groups could be the time demand of the class and homework assignments or dissatisfaction with the program itself. The dropouts were less educated than completers, which reduces the generalizability of the study findings, but were otherwise not different from completers in demographic characteristics.
The majority of participants continued to meditate at 3-month follow-up suggesting that they had incorporated meditation into their daily lives and may indicate that they experienced ongoing benefit from mindfulness meditation. Other studies have similarly found that participants continue to practice meditation 6 months-4 years after program completion (Kabat-Zinn, Lipworth et al. 1986; Carlson, Ursuliak et al. 2001). Nearly one half of the participants reported reduction in pain and sleep medications 3 months after completing the study, which is a notable benefit in a group that may be prone to side effects.
In response to the mindfulness meditation program both the intervention and the control group (after cross-over into the program) showed similarities in their response to the measures as they were in the expected direction for most measures in both groups. At 3-month follow-up there was less stability in the control group’s maintenance of a positive response after receiving the program as compared to the intervention group. The one exception, however, was for the MPQ which continued to improve over the follow-up period, with the benefit reaching statistical significance bSSSy 3 months.
Overall, effect sizes varied from small to large. Previously reported effect sizes have been in the medium range (Baer 2003; Grossman, Niemann et al. 2004). Effect sizes should be interpreted with caution because of the small sample size and the increased variability in the control group data as compared to the intervention group. Although this variability might be expected given that the control group was not monitored for therapy changes during the study, it nevertheless makes the effect sizes more difficult to interpret, since the latter are calculated taking change relative to the control group into account. A more difficult question to answer is whether the findings have clinical significance. Measures where values for a clinically important difference (CID) have been reported include the SF-36. A CID on the SF-36 has been proposed to be a change of 3-5 points (Stewart, Greenfield et al. 1989), whereas others would argue a minimum of 5 points is required (Wyrwich, Tierney et al. 2005). The physical function subscale had an overall improvement of 4.1 points at 8-weeks for the intervention group, which would suggest it was clinically relevant. Anecdotally, two of the participants in our trial stopped using their canes by the end of the 8-week program.
During the 8-week program participants were required to fill out a daily diary of minutes spent in meditation and record comments related to their experience. Since participants readily admitted to not meditating, the diaries were likely an accurate reflection of their daily meditation and not simply filled out to please the class instructors. The diary comments revealed a depth and richness of experience that could not be captured with the quantitative measures of this study.
There are many challenges facing psychological interventions as pointed out in a recent editorial (Morley and Williams 2006). We recognize the limitations of our study, many due to its pilot nature. The study is limited by its small sample size and is not powered to detect between-group differences. Additionally, the wait-list control group design did not control for face-to-face time subjects spent in class with the instructors or the total time spent in class. As a result there could be an effect on subjects simply from being present in class with the instructors or from the support of the other class participants. Additionally, controls could worsen during the waiting period, simply due to the distress of waiting for the program to begin. An attention-control would be a more appropriate control for future studies. Treatment effect may be biased by possible regression to the mean. No data were collected about change in therapy during the initial 8-weeks for the wait-list control group and during the 3-month follow-up period for both groups, therefore, self-reported improvement in physical function and pain may reflect other treatments. We crossed over the control group to the meditation program immediately after the intervention group completed the program. Future studies should wait to cross-over the control group until after all follow-up has occurred, to preserve the integrity of the control group. Although we were concerned about dropouts and recruitment of subjects if they had to wait many months to receive the meditation program, participants showed enough enthusiasm for the program that this is of less concern to us for future studies. Finally, measures of mindfulness, such as the Kentucky Inventory of Mindfulness Skills (Baer, Smith et al. 2004; Baer, Smith et al. 2006) or the Mindful Attention Awareness Scale (Brown and Ryan 2003) should be included in future studies.
In summary, an 8-week mindfulness meditation program is feasible among community dwelling older adults with CLBP. Three-month follow-up suggested sustained benefit from the program as measured by continued meditation by program participants and sustained improvement in physical function and pain acceptance. Mind-body therapies such as the MBSR program are a promising non-pharmacologic adjunct to current pain treatment for older adults. However, larger more rigorous trials must be undertaken to convincingly demonstrate their effectiveness.
Acknowledgments
The authors thank the UPMC Shadyside Center for Integrative Medicine for providing office space and the classroom to teach the meditation program and Dr. James Bost and Dr. Subashan Perera for statistical support.
Supported by AG23641 K07 of Dr. Stephanie Studenski from the National Institutes of Health. During the time of this work Dr. Morone was supported by a primary care faculty development training grant (HRSA D55 HP05156) and by the NIH Roadmap Multidisciplinary Clinical Research Career Development Award Grant (1KL2RR024154-01) from the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Astin JA. Mind-body therapies for the management of pain. Clinical Journal of Pain. 2004;20:27–32. doi: 10.1097/00002508-200401000-00006. [DOI] [PubMed] [Google Scholar]
- Astin JA, Berman BM, et al. The efficacy of mindfulness meditation plus Qigong movement therapy in the treatment of fibromyalgia: a randomized controlled trial. Journal of Rheumatology. 2003;30:2257–62. see comment. [PubMed] [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology: Science & Practice. 2003;10:125–143. [Google Scholar]
- Baer RA, Smith GT, et al. Assessment of Mindfulness by Self-Report: The Kentucky Inventory of Mindfulness Skills. Assessment. 2004;11:191–206. doi: 10.1177/1073191104268029. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, et al. Using Self-Report Assessment Methods to Explore Facets of Mindfulness. Assessment. 2006;13:27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, et al. Depression and pain comorbidity: a literature review. Archives of Internal Medicine. 2003;163:2433–45. doi: 10.1001/archinte.163.20.2433. see comment. [DOI] [PubMed] [Google Scholar]
- Benca RM, Ancoli-Israel S, et al. Special considerations in insomnia diagnosis and management: depressed, elderly, and chronic pain populations. Journal of Clinical Psychiatry. 2004;8:26–35. [PubMed] [Google Scholar]
- Bosley BN, Weiner DK, et al. Is chronic nonmalignant pain associated with decreased appetite in older adults? Preliminary evidence. Journal of the American Geriatrics Society. 2004;52:247–51. doi: 10.1111/j.1532-5415.2004.52063.x. [DOI] [PubMed] [Google Scholar]
- Brown KW, Ryan RM. The benefits of being present: mindfulness and its role in psychological well-being. Journal of Personality & Social Psychology. 2003;84:822–48. doi: 10.1037/0022-3514.84.4.822. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Ursuliak Z, et al. The effects of a mindfulness meditation-based stress reduction program on mood and symptoms of stress in cancer outpatients: 6-month follow-up. Supportive Care in Cancer. 2001;9:112–23. doi: 10.1007/s005200000206. [DOI] [PubMed] [Google Scholar]
- Cooper JK, Kohlmann T. Factors associated with health status of older Americans. Age & Ageing. 2001;30:495–501. doi: 10.1093/ageing/30.6.495. [DOI] [PubMed] [Google Scholar]
- Creamer P, Singh BB, et al. Sustained improvement produced by nonpharmacologic intervention in fibromyalgia: results of a pilot study. Arthritis Care & Research. 2000;13:198–204. doi: 10.1002/1529-0131(200008)13:4<198::aid-anr4>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, et al. Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine. 2003;65:564–70. doi: 10.1097/01.psy.0000077505.67574.e3. see comment. [DOI] [PubMed] [Google Scholar]
- Fishbain DA, Cutler R, et al. Chronic pain-associated depression: antecedent or consequence of chronic pain? A review. Clinical Journal of Pain. 1997;13:116–37. doi: 10.1097/00002508-199706000-00006. [DOI] [PubMed] [Google Scholar]
- Foster DF, Phillips RS, et al. Alternative medicine use in older Americans. J Am Geriatr Soc. 2000;48:1560–5. doi: 10.1111/j.1532-5415.2000.tb03864.x. [DOI] [PubMed] [Google Scholar]
- Gagliese L, Melzack R. Chronic pain in elderly people. Pain. 1997;70:3–14. doi: 10.1016/s0304-3959(96)03266-6. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, et al. Mindfulness-based stress reduction and health benefits; A meta-analysis. Journal of Psychosomatic Research. 2004;57:35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Ferrucci L, et al. Lower extremity function and subsequent disability: consistency across studies, predictive models, and value of gait speed alone compared with the short physical performance battery. J Gerontol A Biol Sci Med Sci. 2000;55:M221–31. doi: 10.1093/gerona/55.4.m221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- Hays RD, Prince-Embury S, et al. RAND-36 Health Status Inventory. San Antonio: The Psychological Corporation; 1998. [Google Scholar]
- Helme RD, Katz B, et al. Can psychometric tools be used to analyse pain in a geriatric population? Clin Exp Neurol. 1989;26:113–7. [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain, and Illness. Delacorte; New York: 1990. [Google Scholar]
- Kabat-Zinn J. Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science & Practice. 2003;10:144–156. [Google Scholar]
- Kabat-Zinn J, Lipworth L, et al. The clinical use of mindfulness meditation for the self-regulation of chronic pain. Journal of Behavioral Medicine. 1985;8:163–90. doi: 10.1007/BF00845519. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J, Lipworth L, et al. Four-Year Follow-Up of a Meditation-Based Program for the Self-Regulation of Chronic Pain: Treatment Outcomes and Compliance. The Clinical Journal of Pain. 1986;2:159–173. [Google Scholar]
- Kabat-Zinn J, Massion AO, et al. Effectiveness of a meditation-based stress reduction program in the treatment of anxiety disorders. American Journal of Psychiatry. 1992;149:936–43. doi: 10.1176/ajp.149.7.936. [DOI] [PubMed] [Google Scholar]
- Lindberg DA. Integrative review of research related to meditation, spirituality, and the elderly. Geriatric Nursing. 2005;26:372–7. doi: 10.1016/j.gerinurse.2005.09.013. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Carson JW, et al. Acceptance and change in the context of chronic pain. Pain. 2004;109:4–7. doi: 10.1016/j.pain.2004.02.006. [DOI] [PubMed] [Google Scholar]
- McCracken LM, Vowles KE, et al. Acceptance of chronic pain: component analysis and a revised assessment method. Pain. 2004;107:159–66. doi: 10.1016/j.pain.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–7. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- Morley S, Williams AC. RCTs of psychological treatments for chronic pain: Progress and challenges. Pain. 2006;121:171–2. doi: 10.1016/j.pain.2006.01.017. [DOI] [PubMed] [Google Scholar]
- Morone NE, Greco CM. Mind-body interventions for chronic pain in older adults: A structured review. Pain Medicine. 2007 doi: 10.1111/j.1526-4637.2007.00312.x. in press. [DOI] [PubMed] [Google Scholar]
- Nicholas MK, Asghari A. Investigating acceptance in adjustment to chronic pain: is acceptance broader than we thought? Pain. 2006;124:269–79. doi: 10.1016/j.pain.2006.04.032. [DOI] [PubMed] [Google Scholar]
- Randolph P, Tacone A, et al. The long-term combined effects of medical treatment and a mindfulness-based behavioral program for the multidisciplinary management of chronic pain in West Texas. Pain Digest. 1999;9:103–112. [Google Scholar]
- Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine. 1983;8:141–4. doi: 10.1097/00007632-198303000-00004. [DOI] [PubMed] [Google Scholar]
- Roy R, T MR. Elderly persons with and without pain: A comparative study. Clin J Pain. 1987;3:102–106. [Google Scholar]
- Stewart AL, Greenfield S, et al. Functional status and well-being of patients with chronic conditions. Results from the Medical Outcomes Study. Jama. 1989;262:907–13. erratum appears in JAMA 1989 Nov 10;262(18):2542. [PubMed] [Google Scholar]
- Thomas E, Peat G, et al. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP) Pain. 2004;110:361–8. doi: 10.1016/j.pain.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Urwin M, Symmons D, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57:649–55. doi: 10.1136/ard.57.11.649. see comment. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner D, Pieper C, et al. Pain measurement in elders with chronic low back pain: traditional and alternative approaches. Pain. 1996;67:461–7. doi: 10.1016/0304-3959(96)03150-8. [DOI] [PubMed] [Google Scholar]
- Woo J, Ho SC, et al. Musculoskeletal complaints and associated consequences in elderly Chinese aged 70 years and over. J Rheumatol. 1994;21:1927–31. [PubMed] [Google Scholar]
- Wyrwich KW, Tierney WM, et al. A comparison of clinically important differences in health-related quality of life for patients with chronic lung disease, asthma, or heart disease. Health Services Research. 2005;40:577–91. doi: 10.1111/j.1475-6773.2005.00373.x. [DOI] [PMC free article] [PubMed] [Google Scholar]