Abstract
Background
Hormone replacement therapy use (HRT) is associated with increased breast cancer risk. Our primary objective was to explore hormone levels in plasma according to HRT use, body mass index (BMI) and menopausal status. A secondary objective was to validate self-reported questionnaire information on menstruation and HRT use in the Norwegian Women and Cancer postgenome cohort (NOWAC).
Methods
We conducted a cross-sectional study of sex hormone levels among 445 women aged 48–62 who answered an eight-page questionnaire in 2004 and agreed to donate a blood sample. The samples were drawn at the women's local general physician's offices in the spring of 2005 and sent by mail to NOWAC, Tromsø, together with a two-page questionnaire. Plasma levels of sex hormones and Sex Hormone Binding Globulin (SHBG) were measured by immunometry. 20 samples were excluded, leaving 425 hormone measurements.
Results
20% of postmenopausal women were HRT users. The plasma levels of estradiol (E2) increased with an increased E2 dose, and use of systemic E2-containing HRT suppressed the level of Follicle Stimulating Hormone (FSH). SHBG levels increased mainly among users of oral E2 preparations. Vaginal E2 application did not influence hormone levels. There was no difference in BMI between HRT users and non-users. Increased BMI was associated with increased E2 and decreased FSH and SHBG levels among non-users. Menopausal status defined by the two-page questionnaire showed 92% sensitivity (95% CI 89–96%) and 73% specificity (95% CI 64–82%), while the eight-page questionnaire showed 88% sensitivity (95% CI 84–92%) and 87% specificity (95% CI 80–94%). Current HRT use showed 100% specificity and 88% of the HRT-users had plasma E2 levels above the 95% CI of non-users.
Conclusion
Users of systemic E2-containing HRT preparations have plasma E2 and FSH levels comparable to premenopausal women. BMI has an influence on hormone levels among non-users. NOWAC questionnaires provide valid information on current HRT use and menopausal status among Norwegian women who are between 48 and 62 years old.
Background
Plasma concentrations of steroid hormones influence the risk of breast cancer among both premenopausal and postmenopausal women, and estrogen is regarded as a carcinogen in cancer development [1,2]. Several epidemiological studies have examined female sex hormone levels, but hormone replacement therapy (HRT) users were either excluded [3-7] or they were not classified according to the type of HRT used [8,9]. One exception is a prospective case-control study nested within the Nurses' Health Study (NHS) [10]. However, it is uncertain whether results from the USA can be generalized to the Norwegian female population, due to different types of HRT preparation dominating the two markets, i.e. conjugated equine estrogens in the USA and micronized 17-β-estradiol or estradiol valerate in Norway. Several clinical studies have examined the relationship between HRT use and hormone levels, although in relatively small and highly selected populations [11,12]. Elevated estrogen levels may also be a result of high body mass index (BMI), through the conversion of androstenedione to estrone in adipose tissue [6,13].
The Norwegian Women and Cancer study (NOWAC) is a population-based, nation-wide cohort study which prospectively measures risk factors and biomarkers by means of repeat questionnaires and blood sample collection. The study has previously shown [14] that current use of HRT is associated with increased breast cancer risk, in agreement with similar observational studies like the Million Women Study (MWS)[15] and the European Prospective Investigation into Cancer and Nutrition (EPIC) [16]. It should be noted that breast cancer risk may differ according to differing HRT regimens [17], and that self-reported use of HRT and menstruation status among NOWAC participants has not been validated and described through hormone levels in plasma. The quality of results from research into questionnaire information depends heavily on the questions asked, and validation of the variables used is essential in this respect [18]. A cross-sectional descriptive study of hormone levels is also important, to avoid misclassification of subjects in a subsequent gene expression analysis of the same material.
In this study, we explore hormone levels in plasma according to HRT use, BMI and menopausal status. We further use plasma hormone levels to investigate the validity of self-reported information on menstruation, current HRT use and different HRT regimens in the NOWAC postgenome cohort.
Methods
Study population
The Norwegian Women and Cancer Study (NOWAC) is a cohort study based on questionnaires mailed to women who are 30–70 years old [19]. Participants are randomly drawn from the Central Population Register. From 1991 up until June 2007, 171 977 women had been enrolled in NOWAC, of whom 167 058 are still participating. Questionnaire information on diet, lifestyle and the use of medication is available, with 1–2 repeat measurements at 4–6 year intervals. The NOWAC postgenome cohort consists of 49 233 participants born between 1943 and 1957, who contributed a blood sample between 2003 and 2006. Written informed consent is obtained from each participant and the collection and storing of questionnaire information and blood samples is approved by The Regional Committee for Medical Research Ethics and the Norwegian Data Inspectorate. Statistics Norway obtains updated information on deaths and migration and performs the sampling of women, thereby providing a complete follow-up of participants.
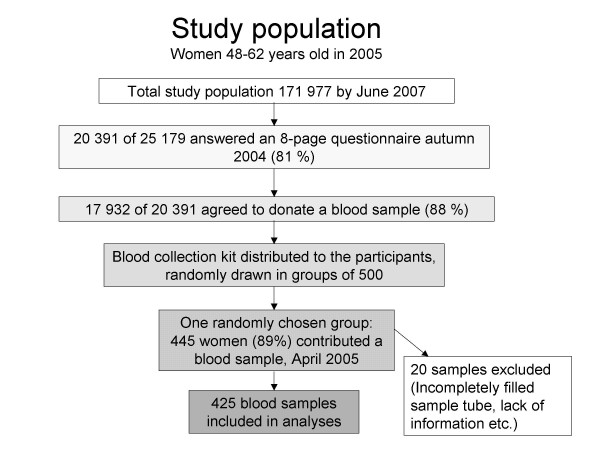
The present study is a cross-sectional analysis within the NOWAC postgenome cohort (Figure 1). Of the 20 391 women who answered an eight-page questionnaire in the autumn of 2004 (response rate 81%), 17 932 agreed to donate a blood sample. Women, randomly drawn in groups of 500, were mailed a blood collection kit and an accompanying two-page questionnaire in April 2005. One reminder was mailed after three weeks to non-responders. The overall response rate was 74%. The two-page questionnaire included questions regarding menopausal status, smoking, weight, height, use of HRT, oral contraceptives or other medication, omega-3 intake, intake of soy or other dietary supplements, and details concerning blood specimen collection (date, hour, posture). Our present study included 445 responders from one group of 500 women (89%); 3.2% declined to participate, 0.8% had died or migrated and 7.0% did not respond. Six samples were excluded due to incompletely filled blood collection tubes. Additionally, 14 women were excluded due to a lack of information concerning menopausal status, use of HRT or type of HRT used. This left plasma sample measurements for 425 women.
Figure 1.
Flow chart of the study population.
Collection and processing of blood samples
The blood samples were drawn at the women's local general physician's offices, using the blood collection kit. For collection of plasma and buffy coat we used a Vacuette® Coagulation Tube (Greiner Bio-One GmbH, Kremsmünster, Austria) containing citrate buffer 0.109 mol/L (3.2%); 1 part citrate to 9 parts blood. For collection of RNA we used a PAXgene™ Blood RNA tube (PreAnalytiX GmbH, Hombrechticon, Switzerland), which is a BD Vacutainer™ containing a proprietary reagent that immediately stabilizes intracellular RNA. The samples were mailed overnight to the Institute of Community Medicine at the University of Tromsø, Norway. The women were requested not to have their blood samples drawn on Thursdays and Fridays, in order to avoid a weekend mail delay. The blood samples were generally received by the NOWAC biobank staff within 1–2 days (92%). Upon arrival, the Vacuette® Coagulation Tubes were centrifuged at 3000 rpm for 15 minutes. Plasma (2 × 1.8 mL) and buffy coat (1.0 mL) were frozen at -20°C and subsequently transferred to -70°C within one week. PAXgene™ Blood RNA tubes were frozen directly at -20°C and transferred to -70°C without pre-processing. The results of gene expression analyses will be published at a later stage.
Laboratory analysis
All the hormone analyses were performed at the Department of Medical Biochemistry, University Hospital of North Norway, Tromsø, Norway. Plasma levels of estradiol (E2), progesterone (P4) and Follicle Stimulating Hormone (FSH) were measured by immunometry, using an electrochemiluminescence immunoassay (ECLIA) on Modular Analytics E170 (Roche Diagnostics GmbH, Mannheim, Germany). Plasma levels of Sex Hormone Binding Globulin (SHBG) were measured by chemiluminescent immunometric assay (CLIA) on Immulite® 2000 (Diagnostic Products Corporation, Los Angeles, CA, USA). The respective detection limits and analytic coefficients of variation (CV) were 0.018 nmol/L and 5.2% for E2; 0.100 IU/L and 2.3% for FSH; 0.095 nmol/L and 6.9% for P4; and 0.02 nmol/L and 5.0% for SHBG. For the sake of convenience, SHBG will be referred to as a hormone throughout this paper. According to the laboratory, the postmenopausal reference values for FSH and E2 were FSH > 26 IU/L and E2 < 0.20 nmol/L. Three measurements of P4 were below the detection limit and values were defined as half of the detection limit (0.048 nmol/l). Two measurements of SHBG were above the calibration range, and values were defined as the upper limit of the range (180 nmol/L).
The analysis of Modular Analytics E170 of SHBG is not validated for citrate plasma by the manufacturer. The Department of Medical Biochemistry performed a small verification analysis, using serum and citrate plasma from 21 healthy volunteers (data not published). The results indicated a good correlation between measurements in serum and citrate plasma for all hormones measured (0.9899 ≤ r2 ≤ 0.9997).
Statistical methods
We used SPSS® 14.0 for Windows for the statistical analyses. Geometric mean plasma levels across different categories of HRT use or BMI were compared using univariate analysis of covariance (ANCOVA) through the general linear model approach. Additionally, we used multiple linear regression to test the association between BMI (continuous variable) and hormone levels. Covariates tested for potential confounding: age, alcohol consumption (units per week), parity and BMI (ANCOVA across HRT categories). In the analysis of the association between BMI and hormone level among HRT users, we also included HRT category as a potential confounder. With the exception of age, only covariates that contributed significantly to the model were included in the final analysis. Time since menopause was excluded as a covariate, due to 25% missing values among postmenopausal women. Sidak corrected post hoc comparisons were used to determine which group means differed. Levene's homogeneity-of-variance test was used to check the equality of group variances. The association between natural log-transformed hormone levels and time since menopause were tested by partial correlation, controlling for BMI. Difference in hormone levels according to time since last HRT dose (0 or 1 day) or fasting (≥10 hours since last meal [10]), and difference in SHBG level between the use of oral and other HRT regimens were analysed with Student's t-test for independent samples. We used the McNemar's test for correlated proportions to check for differences in sensitivity and specificity between the two questionnaires [20]. All p-values are two-tailed and the level of statistical significance is 5%.
BMI was categorized as underweight (<18.5 kg/m2), overweight (≥25.0 kg/m2) and obesity (≥30.0 kg/m2) [21]. The two lowest categories (underweight and normal weight, <25.0 kg/m2) were merged, due to there being few underweight women.
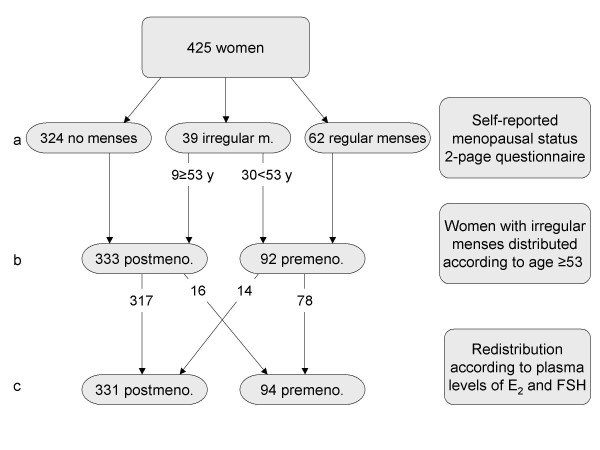
Menopausal status at blood draw was determined for each woman, based on her answers in the two-page questionnaire as to whether she still had regular menstrual periods, whether the periods were irregular or whether they had stopped. Women were classified as postmenopausal if their periods had stopped and premenopausal if their periods were regular. Women with irregular menses were classified as postmenopausal if they were 53 years or older. This cut-off point was used in a previous NOWAC report [14], based on the definition used in the MWS [15]. The eight-page questionnaire additionally included questions regarding the reason why periods had stopped (natural stop, bilateral oophorectomy, hysterectomy or other reasons) and the age when periods had stopped. When classifying according to plasma levels, we used the postmenopausal reference values, both FSH > 26 IU/L and E2 < 0.20 nmol/L, as cut-off. Women with either high FSH or low E2 levels were not classified as postmenopausal. The menopausal classification used as a basis for the between group analyses is a combination of these classification procedures. We used the plasma level classification as the gold standard to validate self-reported menopausal status defined by each questionnaire.
HRT use was categorized according to E2 content: no HRT, HRT without E2 (i.e. estriol, tibolone and other progestogens), E2 for vaginal application, E2 patches (all dosages), oral 1 mg E2 (continuous and sequential preparations), and oral 2 mg E2 (continuous, but also sequential preparations with 1 mg E2 in 6 out of 28 tablets).
To assess the validity of HRT use, we compared plasma E2 levels among HRT users with the 95% CI for plasma E2 levels among postmenopausal non-users, and we examined to what extent plasma E2 levels among non-users exceeded 0.20 nmol/L.
Results
Table 1 shows an overview of population characteristics. Based on self-reported age when their periods stopped, 90% of postmenopausal women experiencing natural menopause were postmenopausal by the age of 53. Figure 2 shows the combined classification of menopausal status.
Table 1.
Characteristics of the study population
| Postmenopausal* | Pre/perimenopausal* | Total | |||||||
| N | Mean | 95% CI | N | Mean | 95% CI | N | Mean | 95% CI | |
| Age (years) | 331 | 55.8 | (55.4–56.2) | 94 | 50.1 | (49.6–50.5) | 425 | 54.5 | (54.1–54.9) |
| Years since menopause | 247 | 8.1 | (7.4–8.2) | - | - | - | - | - | - |
| BMI (kg/m2) | 331 | 25.6 | (25.1–26.0) | 93 | 25.2 | (24.2–26.1) | 424 | 25.5 | (25.1–25.9) |
* Defined by the combined classification based on both questionnaires and hormone levels (Fig. 2 level c)
Figure 2.
Flow chart of menopausal status classification in the study sample. Level c: 16 postmenopausal women not using HRT had premenopausal plasma levels of E2 and FSH, including 2 of the 9 women reporting irregular menses, while 14 of the 30 women reporting irregular menses had postmenopausal plasma levels.
Hormone levels according to HRT use among postmenopausal women
Of 331 postmenopausal women, 66 were current HRT users. Among oral preparations, 84% were combinations of E2 and norethisterone actetate (NETA), while 16% were E2-only preparations. Most patches were E2-only preparations, except one woman using a transdermal combination of E2 and NETA. Three of the 66 users showed signs of non-compliance, based on their reported date of last HRT dose. Six women did not report the date.
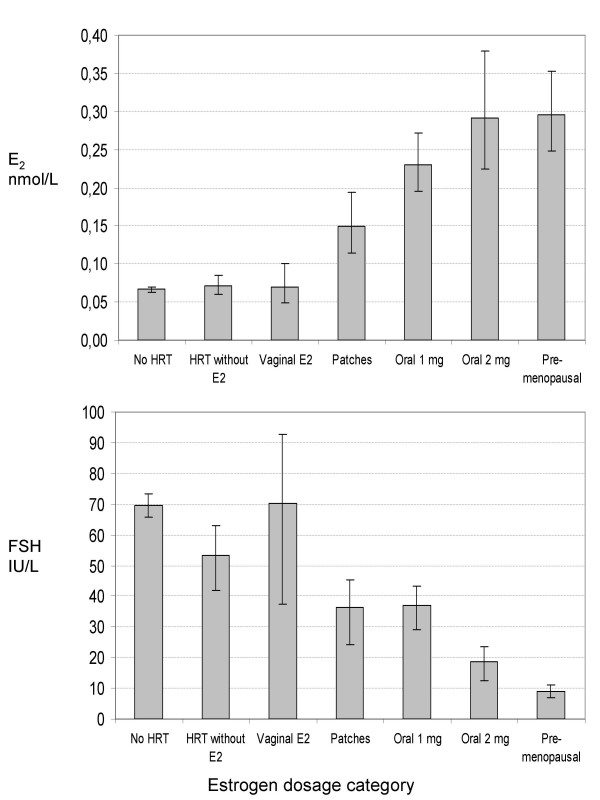
Table 2 shows the distribution of women and geometric mean plasma levels of hormones for each HRT user category. The plasma levels of E2 increased with increasing E2 dose (Table 2, Figure 3). Moreover, use of systemically-administered HRT (patches and tablets) containing E2 suppressed the level of FSH (Table 2, Figure 3). There were statistically significant differences in P4 and SHBG levels across categories of HRT use (Table 2), although not in a dose-dependent manner in the case of P4. The assumption of homogeneity of variance was violated in the analysis of E2 and FSH (Levene's test p < 0.01). The ratio between highest and lowest variance was 7.6 for E2 and 8.7 for FSH.
Table 2.
Geometric mean plasma levels3 of E2, FSH, P4 and SHBG according to use of HRT among postmenopausal women
| E2 dosage category | E2¤ nmol/L | FSH¶ IU/L | P4 nmol/L | SHBG‡ nmol/L | |
| n | 95% CI | 95% CI | 95% CI | 95% CI | |
| No HRT | 2651 | 0.07 (0.06–0.07) | 69.6 (65.9–73.5) | 0,82 (0.76–0.89) | 42.4 (40.2–44.8) |
| HRT | |||||
| HRT without E2 | 20 | 0.07 (0.06–0.08) | 53.4 (44.0–64.9) | 0,65 (0.49–0.87) | 34.9 (28.7–42.4) |
| Vaginal E2 | 5 | 0.07 (0.05–0.10) | 70.4 (47.8–104) | 0,99 (0.56–1.76) | 33.4 (22.6–49.4) |
| Patches | 9 | 0.15 (0.12–0.19) | 36.4 (27.3–48.5) | 1,05 (0.68–1.61) | 47.0 (35.1–62.8) |
| Oral 1 mg | 232 | 0.23 (0.20–0.27) | 36.9 (30.6–44.6) | 0,46 (0.35–0.60) | 52.1 (43.4–62.5) |
| Oral 2 mg | 9 | 0.29 (0.22–0.38) | 18.7 (14.1–25.0) | 0,79 (0.51–1.21) | 62.5 (46.8–83.6) |
| ANCOVA3 | p < 0.01 | p < 0.01 | p < 0.01 | p < 0.01 |
1FSH: n = 252
2 FSH: n = 21
3 Covariates included in addition to age: ‡ BMI, ¶ BMI and alcohol, ¤ BMI and BMI*age interaction term. Parity did not contribute significantly to the model for any of the analyses, and was omitted.
Figure 3.
Plasma levels of estradiol and FSH according to estradiol dosage and rout of administration. Geometric mean ± 95% CI, premenopausal levels are included for comparison.
The post hoc comparisons showed that there was no difference in plasma E2 level between vaginal E2 application and no E2 use (i.e. no HRT use and HRT without E2). The main difference was between no/vaginal E2 use and systemically administered HRT (p ≤ 0.01). The same tendency was seen for FSH levels, although not as conclusive as for E2 levels. The post hoc comparison did not reveal any systematic pattern of differences for P4 and SHBG levels across HRT categories. There was, however, a statistically significant difference (p = 0.02) in SHBG level between use of oral HRT (54.5 nmol/L, 95% CI: 45.8–64.9) and the other HRT users (39.8 nmol/L, 95% CI: 32.6–48.6). There was a borderline significant difference in E2 level (p = 0.05) between those who had taken their last tablet on the day of blood sampling (n = 17) and those who had taken their last tablet the day before (n = 11).
BMI and hormone levels
There was no significant difference in BMI between premenopausal and postmenopausal women (Table 1). Among postmenopausal women there was no significant difference in BMI between HRT users (25.1 kg/m2, 95% CI: 24.0–26.2) and non-users (25.7 kg/m2, 95% CI: 25.2–26.2) (p = 0.30).
Among non-users, there was a significant difference in FSH and SHBG levels across the three categories of BMI, but not in E2 or P4 levels (Table 3). The regression coefficients (β) showed that one unit increase in BMI was significantly associated with a -3.5% decreased FSH level (95% CI: -4.5% – -2.4%), a -5.4% decreased SHBG level (95% CI: -6.6% – -4.3%), and a 1.6% increased E2 level (95% CI: 0.5% – 2.7%), after adjusting for age. Among HRT users (data not shown), there was significant association between BMI and FSH (p < 0.01), but not between BMI and the other hormones analysed (adjusted for age and estrogen dosage category).
Table 3.
Geometric mean plasma levels* of E2, FSH, P4 and SHBG according to BMI among postmenopausal women not using HRT
| E2 nmol/L | FSH IU/L | P4 nmol/L | SHBG nmol/L | ||
| n | 95% CI | 95% CI | 95% CI | 95% CI | |
| BMI (kg/m2) | |||||
| BMI < 25 | 137 | 0.07 (0.06–0.07) | 76.7 (71.8–81.9) | 0.87 (0.78–0.97) | 51.8 (48.2–55.7) |
| 25 ≤ BMI < 30 | 91 | 0.07 (0.06–0.07) | 66.3 (61.2–71.9) | 0.78 (0.68–0.89) | 35.9 (32.8–39.2) |
| BMI ≥ 30 | 37 | 0.08 (0.07–0.09) | 52.0 (45.8–59.1) | 0.74 (0.61–0.91) | 29.1 (25.3–33.5) |
| ANCOVA* | p = 0.08 | p < 0.01 | p = 0.25 | p < 0.01 |
* Adjusted for age. The covariates alcohol and parity did not contribute significantly to the model for any of the analyses, and was omitted.
Hormone levels among postmenopausal women not taking HRT
There was negative correlation between time since menopause and plasma E2 levels (r = -0.16, p = 0.03) and P4 (r = -0.29, p < 0.01), and positive correlation between SHBG levels and time since menopause (r = 0.15 and p = 0.04). FSH levels were not significantly correlated with time since menopause.
There was no statistically significant difference in hormone levels between the samples received within 24 hours and those transported over 2, 3 or 4 or more days among either pre-/perimenopausal or postmenopausal women (data not shown). Similarly, there was no statistically significant difference in plasma level between fasting and non-fasting subjects for any of the hormones measured, and lipaemia (n = 13) and haemolysis (n = 30), encountered by visual examination, did not influence the hormone levels (data not shown).
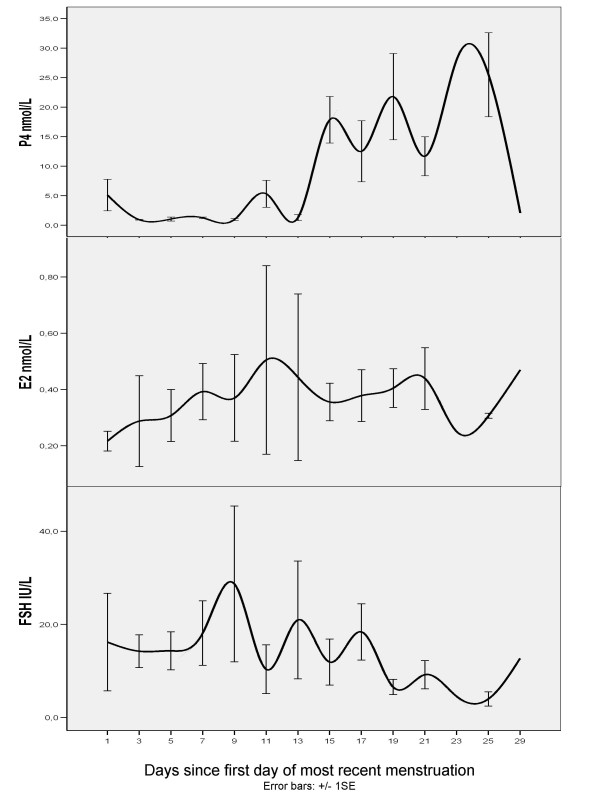
Premenopausal women
Figure 4 shows plasma levels of E2, P4 and FSH, according to days since menstruation among premenopausal women who reported having regular periods and who filled in the date of the first day of their most recent menstruation (n = 62). Although there were few women in each two-day period (n = 1–8), the pattern of hormonal variation throughout the menstrual cycle was recognizable both for the gonadal hormones and FSH. Progesterone levels > 20 nmol/L were only found among women in their luteal phase (≥15. day). There was no recognizable cyclic hormone pattern among the 20 perimenopausal women who had reported their menstruation date. One woman used an oral contraceptive, a progestagen-only pill.
Figure 4.
Plasma levels of progesterone, estradiol and FSH according to days since most recent menstruation among 62 premenopausal women. Geometric mean ± 1SE, 2 period moving average.
Validation of self-reported questionnaire information on menopausal status and hormone use
Sensitivity and specificity for the variable "menopausal status" defined by the two questionnaires used is shown in Table 4. The 66 HRT users were excluded from this analysis. Sensitivity was higher in the two-page questionnaire accompanying the blood sample (p < 0.05). The eight-page questionnaire scored higher on specificity (p < 0.01).
Table 4.
Validation of the menstrual status definition according to questionnaire information
| Classification according to plasma E2 and FSH levels | |||
| Post- | Pre- | Total | |
| Classification according to two-page questionnaire | |||
| Post- | 240 | 27 | 267 |
| Pre- | 20 | 72 | 92 |
| Total | 260 | 99 | 359 |
| Sensitivity: 240/260 = 92% (95% CI 89–96%) | |||
| Specificity: 72/99 = 73% (95% CI 64–82%) | |||
| Classification according to eight-page questionnaire | |||
| Post- | 229 | 11 | 240 |
| Pre- | 29 | 86 | 115 |
| Unknown | 2 | 2 | 4 |
| Total | 260 | 99 | 359 |
| Sensitivity: 229/260 = 88% (95% CI 84–92%) | |||
| Specificity: 86/99 = 87% (95% CI 80–94%) | |||
Out of 41 self-reported users of systemically-administered E2 preparations, 39 women (88%) had E2 levels above the confidence interval of non-users. Thus, self-reported HRT use was confirmed by the hormone levels. Among the 265 self-reported non-users, seven women had E2 levels ≥ 0.20 nmol/L. According to the preceding eight-page questionnaire, six out of the seven women reported being pre- or perimenopausal or uncertain regarding menopausal status six months before the blood draw. At the same time, they also reported being non-users, they did not state their age at menopause, and all seven were younger than 53 years old. Hence, they were probably perimenopausal at the time of blood draw, and not misclassified HRT users. On the basis of this, we conclude that the specificity of the questionnaire variable "current HRT use" is 100%.
Among 78 women with uncertain menopausal status due to hysterectomy, use of HRT, etc., who according to the eight-page questionnaire were defined as postmenopausal, based on age ≥ 53 years, 4 were misclassified according to plasma hormone levels.
Discussion
The associations found between current HRT use and plasma levels of E2 confirm previous reports [10-12]. Transdermal E2 50 μg/day, which is the Defined Daily Dose (DDD) [22] for E2 patches, should give approximately the same plasma E2 levels as oral 1 mg E2. We merged use of patches into one category because there were only 9 users; 5 did not report the dose and the remaining 4 used 50 μg/day or less. Assuming that women in 2005 used the lowest possible dose, it is likely that the average dose among these women was lower than 50 μg/day, and that the plasma levels of E2 should be lower for patches than for oral 1 mg E2. Users of HRT for vaginal application were not expected to differ much from non-users regarding plasma level of E2. The vaginal tablet is applied twice a week (maintenance dosage) and reports from clinical trials show that blood E2 levels remain within the normal range of postmenopausal women, even with long-term treatment [23,24]. The confidence intervals of the three systemically-administered HRT groups are partly overlapping, reflecting insufficient power to conclude that the plasma levels are different.
The increase in FSH levels as a woman approaches menopause is a result of reduced ovarian inhibin synthesis and increased activin synthesis [25], and it has been assumed that FSH is not influenced by exogenous estrogen supplements during menopause [26]. Pharmacokinetic studies of HRT rarely measure FSH levels, nor did NHS [10] in their population-based study on HRT users. However, there are some reports which show a decrease in FSH levels during the long-term use of both oral [27,28] and transdermal E2 [29]. Our results suggest that exogenous E2 has some effect on FSH levels.
It was not expected that P4 levels would be influenced by HRT use. Although we found differences in P4 levels across categories of HRT use, there was no association with E2 dosage. For the purpose of validation, it would have been rational to measure plasma levels of NETA rather than P4 among HRT users, however this was not feasible with our available methods at the time of analysis.
During daily use of oral HRT, the half life of E2 at a steady state is 15–25 hours, due to sequestration in adipose tissue and enterohepatic recycling [30]. Several reports also show that the use of E2 preparations increases the SHBG plasma concentration, which would increase the blood depot of E2. However, this applies to the use of CEE to a greater extent than 17-β-estradiol preparations [31,32]. In addition, oral rather than topical preparations seem to increase SHBG levels, due to the liver first pass effect [11,12,31,32]. This is in accordance with our results, showing that differences in SHBG levels across HRT categories are mainly due to significantly increased levels among the users of oral preparations.
The results on the correlation between time since menopause and levels of E2, FSH and SHBG are in accordance with previous reports [33,34]. Plasma FSH levels are already high at menopause, while the E2 levels are still dropping.
The lack of association between BMI and HRT use supports conclusions from previous reports [35-37]. The association found between BMI and hormone levels is also in accordance with established knowledge. The absence of a stronger relationship than the one found between E2 and BMI may be due to the assay used. There are reports showing that direct immunoassays are hampered by insufficient sensitivity and specificity when measuring low concentrations of steroids, e.g. E2 among postmenopausal women [38]. If the E2 levels are artificially high in the low range, this would weaken the association. It could also be the reason why the ANCOVA did not show any significant increase across BMI categories, or alternatively this could be due to lack of power. We may also suggest a possible effect of BMI in increasing the bioavailability of estradiol through lower levels of SHBG, which is in accordance with previous findings [6,13]. We did not measure estrone (E1), which may be a better biomarker of estrogen synthesis in adipose tissue among postmenopausal women, although levels of endogenous estradiol and estrone are highly correlated [6,39].
Using plasma levels of sex hormones to define a woman as premenopausal would be difficult, due to the variation in hormone levels throughout the menstrual cycle. In addition, the menstrual cycle changes as the woman approaches menopause [33,34,40]. The follicular phase shortens; FSH levels begin to increase, and E2 levels subsequently decrease. Although we are not trying to validate the self-reported day of menstrual cycle, the fact that the cyclic pattern of plasma sex hormones is visible at all in this rather small group of older premenopausal women provides some assurance in this matter.
We have used plasma levels of E2 and FSH as the gold standard in our validation of self-reported questionnaire information on HRT use and menopausal status. Whether the gold standard chosen is a proper gold standard is always debatable. However, hormone levels were considered to be the best available instrument. To draw the line between pre- and postmenopause, we have used plasma levels of FSH > 26 IU/L and E2 < 0.20 nmol/L as the cut-off point. Several clinical trials conducted among postmenopausal subjects use FSH levels > 30–50 IU/L and/or E2 levels < 0.07–0.15 nmol/L as inclusion criteria [11,12,30]. These rather strict criteria are imperative in clinical trials, to ensure that all the participants are postmenopausal. However, this generates a rather large group of false negatives, which is inappropriate to a validation. Furthermore, since the premenopausal E2 and FSH plasma levels for 14 out of the 16 women reclassified as premenopausal may be explained from information from the eight-page questionnaire (hysterectomy, use of hormone containing intrauterine device, etc.), our cut-off point seems to be well-chosen.
Since the plasma E2 levels among women using vaginal E2-preparations were no different from those of non-users, our validation of the variable "current HRT use" had to be based on the women using systemically-administered E2-containing preparations. However, we see no reason why the route of administration should influence the women's ability to answer the question, and have extended the result to include all HRT use. The agreement found between self-reported HRT use and plasma E2 levels supports previous findings from validation studies comparing self-reported HRT use with prescription data [41,42].
It makes sense to find a lower sensitivity for the eight-page questionnaire, because some women could have become postmenopausal during the six-month lapse until the blood draw. On the other hand, the specificity for the eight-page questionnaire may be artificially high, since some of the premenopausal women will be reported as postmenopausal on the two-page questionnaire six months later, although they are probably in a perimenopausal state. Due to the low misclassification rate, it seems reasonable to continue using age ≥53 as the cut-off point when defining menopausal status in cases of uncertainty.
Strengths and limitations
The NOWAC study has the advantage of being population-based and prospective. The opportunity of random sampling from the complete Central Population Register, together with high response rates, provides a representative sample of the Norwegian female population aged 48–62 years [43]. The two-page questionnaire accompanying the blood sample provides detailed and updated information on central variables such as menstruation status, weight and HRT use, which are complementary to the preceding eight-page questionnaire. Results show that it is especially valuable to be able to differentiate between different types of HRT. The effect of HRT exposure will vary between populations using different HRT regimens, particularly with respect to estrogenic carcinogenicity.
Compliance with HRT is an important determinant for the accurate measurement of HRT use. With 86–95% of the women showing compliance with HRT use, we do not consider lack of compliance to be a significant source of bias in our study.
Probably due to small sample sizes, the assumption of equal variances was violated in the ANCOVA analysis of differences between HRT categories. This causes some concern and the results must be interpreted accordingly. Even so, the very low p-values suggest that the results for E2 and FSH are valid.
Reports on the validity of self-reported body-size generally show that particularly obese people tend to underestimate their weight/waist circumference [44,45]. In the present study, there is an increase in weight (mean: +0.6 kg) between the eight-page questionnaire and the two-page questionnaire six months later and the increase is higher among the women who had their weight measured at their general physician's office (n = 49). This should not influence our analyses to the degree that the associations found are artefacts. However, if the BMI is under-estimated, the change in hormone levels per increased unit of BMI could be over-estimated.
Choosing plasma or serum is a trade-off between rational collection logistics and the broadest assortment of feasible analyses. Not all general physicians' offices have equipment for blood centrifugation, and at the beginning of the NOWAC blood specimen collection in 2002 the range of future analyses had not yet been determined. With the aim of collecting blood from as many participants as possible, it was decided to build a plasma biobank. Citrate was chosen as the anticoagulant, due to the collaboration of NOWAC with EPIC and their collection of citrate plasma. Citrate plasma is not the optimum matrix for immunometry analyses. Although the verification analysis performed by the laboratory did not show alarming inconsistencies, the results must be interpreted accordingly, especially in view of the general limitations of direct immunoassays mentioned above.
A transport delay of over two days could potentially interfere with our measurements. Several studies have concluded that sex hormones FSH and SHBG are fairly stable with regard to transport conditions, temperature variations and delayed processing [46-50]. These reports are not based on an analysis of citrate plasma. However, in our sample there were no statistically significant differences due to transport delay, and we did not exclude any blood samples on these grounds. The analytical methods used are fairly robust with regard to interference by haemoglobin and triglycerides, and since we found no differences due to lipaemia or haemolysis these samples were not excluded from the analysis. Due to the study design, blood samples were not drawn at the same time of day, nor were the women requested to be fasting. However, we found no differences in hormone levels due to fasting and have not adjusted our results according to time since last meal.
Because of the cross-sectional nature of this study, we cannot draw any conclusions regarding causal association based on our results. However, imminent gene-expression analyses and future follow-up of the women in our population sample will contribute to our knowledge on causal relationships.
Conclusion
Users of systemically-administered E2-containing HRT preparations have plasma E2 and FSH levels comparable to those of premenopausal women, while users of vaginal E2 preparations remain within postmenopausal levels. There is no difference in BMI between HRT users and non-users, but increased BMI is associated with increased E2 and decreased FSH and SHBG levels among non-users. The NOWAC questionnaires provide valid information on current hormone use and menopausal status among Norwegian women who are 48–62 years old.
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
MW, VD and EL participated in the design of the study. MW performed the statistical analysis and drafted the manuscript. VD, KB, KSD, CR and EL helped to draft the manuscript. YF was in charge of the immunoassays. EL is the principal investigator of the NOWAC study. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
We are grateful for the assistance of Marita Melhus with the statistical analyses.
Contributor Information
Marit Waaseth, Email: marit.waaseth@ism.uit.no.
Kjersti Bakken, Email: kjersti.bakken@ism.uit.no.
Vanessa Dumeaux, Email: Vanessa.Dumeaux@rr-research.no.
Karina S Olsen, Email: karina.standahl.olsen@ism.uit.no.
Charlotta Rylander, Email: zcr@nilu.no.
Yngve Figenschau, Email: Yngve.Figenschau@unn.no.
Eiliv Lund, Email: eiliv.lund@ism.uit.no.
References
- Cogliano V, Grosse Y, Baan R, Straif K, Secretan B, El Ghissassi F. Carcinogenicity of combined oestrogen-progestagen contraceptives and menopausal treatment. Lancet Oncol. 2005;6:552–553. doi: 10.1016/S1470-2045(05)70273-4. [DOI] [PubMed] [Google Scholar]
- Yager JD, Davidson NE. Estrogen Carcinogenesis in Breast Cancer. N Engl J Med. 2006;354:270–282. doi: 10.1056/NEJMra050776. [DOI] [PubMed] [Google Scholar]
- Key TJ, Appleby P, Barnes I, Reeves G. (The Endogenous Hormones and Breast Cancer Collaborative Group) Endogenous Sex Hormones and Breast Cancer in Postmenopausal Women: Reanalysis of Nine Prospective Studies. J Natl Cancer Inst. 2002;94:606–616. doi: 10.1093/jnci/94.8.606. [DOI] [PubMed] [Google Scholar]
- Missmer SA, Eliassen AH, Barbieri RL, Hankinson SE. Endogenous Estrogen, Androgen, and Progesterone Concentrations and Breast Cancer Risk Among Postmenopausal Women. J Natl Cancer Inst. 2004;96:1856–1865. doi: 10.1093/jnci/djh336. [DOI] [PubMed] [Google Scholar]
- Kaaks R, Berrino F, Key T, Rinaldi S, Dossus L, Biessy C, Secreto G, Amiano P, Bingham S, Boeing H, de Mesquita HBB, Chang-Claude J, Clavel-Chapelon F, Fournier A, van Gils CH, Gonzalez CA, Gurrea AB, Critselis E, Khaw KT, Krogh V, Lahmann PH, Nagel G, Olsen A, Onland-Moret NC, Overvad K, Palli D, Panico S, Peeters P, Quiros JR, Roddam A, Thiebaut A, Tjonneland A, Chirlaque MD, Trichopoulou A, Trichopoulos D, Tumino R, Vineis P, Norat T, Ferrari P, Slimani N, Riboli E. Serum Sex Steroids in Premenopausal Women and Breast Cancer Risk Within the European Prospective Investigation into Cancer and Nutrition (EPIC) J Natl Cancer Inst. 2005;97:755–765. doi: 10.1093/jnci/dji132. [DOI] [PubMed] [Google Scholar]
- Rinaldi S, Key TJ, Peeters PHM, Lahmann PH, Lukanova A, Dossus L, Biessy C, Vineis P, Sacerdote C, Berrino F, Panico S, Tumino R, Palli D, Nagel G, Linseisen J, Boeing H, Roddam A, Bingham S, Khaw KT, Chloptios J, Trichopoulou A, Trichopoulos D, Tehard B, Clavel-Chapelon F, Gonzalez CA, Larrañaga N, J. AB, Quirós R, Chirlaque MD, Martinez C, Monninkhof E, Grobbee DE, Bueno-de-Mesquita HB, Ferrari P, Slimani N, Riboli E, Kaaks R. Anthropometric measures, endogenous sex steroids and breast cancer risk in postmenopausal women: A study within the EPIC cohort. Int J Cancer. 2006;118:2832–2839. doi: 10.1002/ijc.21730. [DOI] [PubMed] [Google Scholar]
- Eliassen AH, Missmer SA, Tworoger SS, Spiegelman D, Barbieri RL, Dowsett M, Hankinson SE. Endogenous Steroid Hormone Concentrations and Risk of Breast Cancer Among Premenopausal Women. J Natl Cancer Inst. 2006;98:1406–1415. doi: 10.1093/jnci/djj376. [DOI] [PubMed] [Google Scholar]
- Rexrode KM, Manson JAE, Lee IM, Ridker PM, Sluss PM, Cook NR, Buring JE. Sex Hormone Levels and Risk of Cardiovascular Events in Postmenopausal Women. Circulation. 2003;108:1688–1693. doi: 10.1161/01.CIR.0000091114.36254.F3. [DOI] [PubMed] [Google Scholar]
- Shakir YA, Samsioe G, Khatibi E A, Nyberg P, Lidfeldt J, Agardh CD, Nerbrand C. Health Hazards in Middle-Aged Women with Cardiovascular Disease: A Case-Control Study of Swedish Women. The Women's Health in the Lund Area (WHILA) Study. Journal of Women's Health. 2007;16:406–414. doi: 10.1089/jwh.2006.0056. [DOI] [PubMed] [Google Scholar]
- Tworoger SS, Missmer SA, Barbieri RL, Willett WC, Colditz GA, Hankinson SE. Plasma Sex Hormone Concentrations and Subsequent Risk of Breast Cancer Among Women Using Postmenopausal Hormones. J Natl Cancer Inst. 2005;97:595–602. doi: 10.1093/jnci/dji099. [DOI] [PubMed] [Google Scholar]
- Slater CC, Zhang C, Hodis HN, Mack WJ, Boostanfar R, Shoupe D, Paulson RJ, Stanczyk FZ. Comparison of Estrogen and Androgen Levels After Oral Estrogen Replacement Therapy. J Reprod Med. 2001;46:1052–1056. [PubMed] [Google Scholar]
- Hofling M, Carlström K, Svane G, Azavedo E, Kloosterboer H, Schoultz BV. Different effects of tibolone and continuous combined estrogen plus progestogen hormone therapy on sex hormone binding globulin and free testosterone levels - an association with mammographic density. Gynecol Endocrinol. 2005;20:110–115. doi: 10.1080/09513590400021151. [DOI] [PubMed] [Google Scholar]
- Key TJ, Appleby PN, Reeves GK, Roddam A. (The Endogenous Hormones and Breast Cancer Collaborative Group) Body Mass Index, Serum Sex Hormones, and Breast Cancer Risk in Postmenopausal Women. J Natl Cancer Inst. 2003;95:1218–1226. doi: 10.1093/jnci/djg022. [DOI] [PubMed] [Google Scholar]
- Bakken K, Alsaker E, Eggen AE, Lund E. Hormone replacement therapy and incidence of hormone-dependent cancers in the Norwegian Women and Cancer study. Int J Cancer. 2004;112:130–134. doi: 10.1002/ijc.20389. [DOI] [PubMed] [Google Scholar]
- Million Women Study Collaborators Breast cancer and hormone-replacement therapy in the Million Women Study. The Lancet. 2003;362:419–427. doi: 10.1016/S0140-6736(03)14065-2. [DOI] [PubMed] [Google Scholar]
- Fournier A, Berrino F, Riboli E, Avenel V, Clavel-Chapelon F. Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort. Int J Cancer. 2005;114:448–454. doi: 10.1002/ijc.20710. [DOI] [PubMed] [Google Scholar]
- Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study. Breast Cancer Res Treat. 2008;107:103–111. doi: 10.1007/s10549-007-9523-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen T, Olsen J. Invited Commentary: The Art of Making Questionnaires Better. Am J Epidemiol. 2006;164:1145–1149. doi: 10.1093/aje/kwj348. [DOI] [PubMed] [Google Scholar]
- Lund E, Dumeaux V, Braaten T, Hjartåker A, Engeset D, Skeie G, Kumle M. Cohort Profile: The Norwegian Women and Cancer Study NOWAC Kvinner og kreft. Int J Epidemiol. 2007 doi: 10.1093/ije/dym137. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- Hawass NE. Comparing the sensitivities and specificities of two diagnostic procedures performed on the same group of patients. Br J Radiol. 1997;70:360–366. doi: 10.1259/bjr.70.832.9166071. [DOI] [PubMed] [Google Scholar]
- Body Mass Index (BMI) http://www.euro.who.int/nutrition/20030507_1
- The WHO Collaborating Centre for Drug Statistics Methodology. http://www.whocc.no/atcddd/
- Dugal R, Hesla K, Sørdal T, Aase KH, Lilleeidet O, Wickstrøm E. Comparison of usefulness of estradiol vaginal tablets and estriol vagitories for treatment of vaginal atrophy. Acta Obstet Gynecol Scand. 2000;79:293–297. doi: 10.1034/j.1600-0412.2000.079004293.x. [DOI] [PubMed] [Google Scholar]
- Weisberg E, Ayton R, Darling G, Farrell E, Murkies A, Neill SO, Kirkegard Y, Fraser IS. Endometrial and vaginal effects of low-dose estradiol delivered by vaginal ring or vaginal tablet. Climacteric. 2005;8:83–93. doi: 10.1080/13697130500087016. [DOI] [PubMed] [Google Scholar]
- Santoro N, Adel T, Skurnick JH. Decreased inhibin tone and increased activin A secretion characterize reproductive aging in women. Fertil Steril. 1999;71:658–662. doi: 10.1016/S0015-0282(98)00529-9. [DOI] [PubMed] [Google Scholar]
- Stenchever MA, Droegemueller W, Herbst AL, Mischell DR. Chapter 42 Menopause; Endocrinology, Consequences of Estrogen Deficiency, Effects of Hormonal Replacement Therapy, Treatment Regimens. In: Stenchever MA, editor. Comprehensive Gynecology. 4. St.Louis, Mo , Mosby Inc.; 2001. pp. 1217–1245. [Google Scholar]
- Sipinen S, Lähteenmäki P, Luukkainen T. Pharmacokinetic studies on low dose estradiol 17β administered orally to postmenopausal women. Acta Obstet Gynecol Scand. 1980;59:149–153. doi: 10.3109/00016348009154632. [DOI] [PubMed] [Google Scholar]
- Castelo-Branco C, de Osaba MJM, Fortuny A, Iglesias X, Gonzalez-Merlo J. Circulating Hormone Levels in Menopausal Women Receiving Different Hormone Replacement Therapy Regimens. J Reprod Med. 1995;40:556–560. [PubMed] [Google Scholar]
- Bowen AJ, John VA, Ramirez ME, Good WR. Bioavailability of oestradiol from the Alora TM (0.1 mg/day) oestradiol matrix transdermal delivery system compared with Estraderm (0.1 mg/day) J Obstet Gynaecol. 1998;18:575–580. doi: 10.1080/01443619866408. [DOI] [PubMed] [Google Scholar]
- Vree TB, Timmer CJ. Enterohepathic Cycling and Pharmacokinetics of Oestradiol in Postmenopausal Women. J Pharm Pharmacol. 1998;50:857–864. doi: 10.1111/j.2042-7158.1998.tb04000.x. [DOI] [PubMed] [Google Scholar]
- Nachtigall LE, Raju U, Banerjee S, Wan L, Levitz M. Serum Estradiol-Binding Profiles in Postmenopausal Women Undergoing Three Common Estrogen Replacement Therapies: AssociationsWith Sex Hormone-Binding Globulin, Estradiol, and Estrone Levels. Menopause. 2000;7:243–250. doi: 10.1097/00042192-200007040-00006. [DOI] [PubMed] [Google Scholar]
- Stomati M, Hartmann B, Spinetti A, Mailand D, Rubino S, Albrecht A, Huber J, Petraglia F, Genazzani AR. Effects of hormonal replacement therapy on plasma sex hormone-binding globulin, androgen and insulin-like growth factor-1 levels in postmenopausal women. J Endocrinol Invest. 1996;19:535–541. doi: 10.1007/BF03349013. [DOI] [PubMed] [Google Scholar]
- Overlie I, Moen MH, Morkrid L, Skjæraasen JS, Holte A. The endocrine transition around menopause - a five years prospective study with profiles of gonadotropines, estrogens, androgens and SHBG among healthy women. Acta Obstet Gynecol Scand. 1999;V78:642–647. doi: 10.1034/j.1600-0412.1999.780714.x. [DOI] [PubMed] [Google Scholar]
- Rannevik G, Jeppsson S, Johnell O, Bjerre B, Laurell-Borulf Y, Svanberg L. A longitudinal study of the perimenopausal transition: altered profiles of steroid and pituitary hormones, SHBG and bone mineral density. Maturitas. 1995;21:103–113. doi: 10.1016/0378-5122(94)00869-9. [DOI] [PubMed] [Google Scholar]
- Bakken K, Eggen AE, Lund E. Side-effects of hormone replacement therapy and influence on pattern of use among women aged 45-64 years. The Norwegian Women and Cancer (NOWAC) study 1997. Acta Obstet Gynecol Scand. 2004;83:850–856. doi: 10.1111/j.0001-6349.2004.00560.x. [DOI] [PubMed] [Google Scholar]
- Norman RJ, Flight IH, Rees MC. Oestrogen and progestogen hormone replacement therapy for peri-menopausal and post-menopausal women: weight and body fat distribution. Cochrane Database Syst Rev. 2000:CD001018. doi: 10.1002/14651858.CD001018. [DOI] [PubMed] [Google Scholar]
- Jensen LB, Vestergaard P, Hermann AP, Gram J, Eiken P, Abrahamsen B, Brot C, Kolthoff N, Sørensen OH, Beck-Nielsen H, Nielsen SP, Charles P, Mosekilde L. Hormone replacement therapy dissociates fat mass and bone mass, and tends to reduce weight gain in early postmenopausal women: a randomized controlled 5-year clinical trial of the Danish Osteoporosis Prevention Study. J Bone Miner Res. 2003;18:333–342. doi: 10.1359/jbmr.2003.18.2.333. [DOI] [PubMed] [Google Scholar]
- Stanczyk FZ, Lee JS, Santen RJ. Standardization of Steroid Hormone Assays: Why, How, and When? Cancer Epidemiol Biomarkers Prev. 2007;16:1713–1719. doi: 10.1158/1055-9965.EPI-06-0765. [DOI] [PubMed] [Google Scholar]
- Schairer C, Hill D, Sturgeon SR, Fears T, Mies C, Ziegler RG, Hoover RN, Sherman ME. Serum Concentrations of Estrogens, Sex Hormone Binding Globulin, and Androgens and Risk of Breast Hyperplasia in Postmenopausal Women. Cancer Epidemiol Biomarkers Prev. 2005;14:1660–1665. doi: 10.1158/1055-9965.EPI-05-0017. [DOI] [PubMed] [Google Scholar]
- Landgren BM, Collins A, Csemiczky G, Burger HG, Baksheev L, Robertson DM. Menopause Transition: Annual Changes in Serum Hormonal Patterns over the Menstrual Cycle in Women during a Nine-Year Period Prior to Menopause. J Clin Endocrinol Metab. 2004;89:2763–2769. doi: 10.1210/jc.2003-030824. [DOI] [PubMed] [Google Scholar]
- Løkkegaard EL, Johnsen SP, Heitmann BL, Stahlberg C, Pedersen AT, Obel EB, Hundrup YA, Hallas J, Sørensen HT. The validity of self-reported use of hormone replacement therapy among Danish nurses. Acta Obstet Gynecol Scand. 2004;83:476 –4481. doi: 10.1111/j.0001-6349.2004.00376.x. [DOI] [PubMed] [Google Scholar]
- Persson I, Bergkvist L, Adami HO. Reliability of Women's Histories of Climacteric Oestrogen Treatmen Assessed by Prescription Forms. Int J Epidemiol. 1987;16:222–228. doi: 10.1093/ije/16.2.222. [DOI] [PubMed] [Google Scholar]
- Lund E, Kumle M, Braaten T, Hjartaker A, Bakken K, Eggen E, Gram TI. External validity in a population-based national prospective study--the Norwegian Women and Cancer Study (NOWAC) Cancer Causes Control. 2003;14:1001–1008. doi: 10.1023/B:CACO.0000007982.18311.2e. [DOI] [PubMed] [Google Scholar]
- Leonhard ML, Barry NJ. Body image and obesity: effects of gender and weight on perceptual measures of body image. Addictive Behaviors. 1998;23:31–34. doi: 10.1016/S0306-4603(97)00017-8. [DOI] [PubMed] [Google Scholar]
- Tehard B, Liere MJV, Nougue CC, Clavel-Chapelon F. Anthropometric Measurements and Body Silhouette of Women: Validity and Perception. J Am Diet Assoc. 2002;102:1779–1784. doi: 10.1016/S0002-8223(02)90381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hankinson SE, London SJ, Chute CG, Barbieri RL, Jones L, Kaplan LA, Sacks FM, Stampfer MJ. Effect of transport conditions on the stability of biochemical markers in blood. Clin Chem. 1989;35:2313–2316. [PubMed] [Google Scholar]
- Taieb J, Benattar C, Birr AS, Lindenbaum A, Frydman R, Olivennes F. Delayed assessment of serum and whole blood estradiol, progesterone, follicle-stimulating hormone, and luteinizing hormone kept at room temperature or refrigerated. Fertil Steril. 2000;74:1053–1054. doi: 10.1016/S0015-0282(00)01546-6. [DOI] [PubMed] [Google Scholar]
- Evans MJ, Livesey JH, Ellis MJ, Yandle TG. Effect of anticoagulants and storage temperatures on stability of plasma and serum hormones. Clin Biochem. 2001;34:107–112. doi: 10.1016/S0009-9120(01)00196-5. [DOI] [PubMed] [Google Scholar]
- Ellis JM, Livesey JH, Evans MJ. Hormone stability in human whole blood. Clin Biochem. 2003;36:109–112. doi: 10.1016/S0009-9120(02)00440-X. [DOI] [PubMed] [Google Scholar]
- Tworoger SS, Hankinson SE. Collection, Processing, and Storage of Biological Samples in Epidemiologic Studies: Sex Hormones, Carotenoids, Inflammatory Markers, and Proteomics as Examples. Cancer Epidemiol Biomarkers Prev. 2006;15:1578–1581. doi: 10.1158/1055-9965.EPI-06-0629. [DOI] [PubMed] [Google Scholar]