Abstract
Between 1974 and 1987, 276 intertrochanteric osteotomies were performed in 217 patients. In 48 hips the osteotomy was done for idiopathic osteoarthritis. In 166 hips the osteoarthritis was secondary to acetabular dysplasia, in 23 to trauma, in 14 to slipped capital femoral epiphysis, in five to Legg–Calvé–Perthes' disease and in 20 to avascular necrosis of the femoral head. Good results were achieved in young females with mild osteoarthritis secondary to acetabular dysplasia, and in patients with posttraumatic osteoarthritis. All other indications showed a poorer long-term survival. Our study shows that acetabular dysplasia and posttraumatic arthritis remain valid indications for intertrochanteric osteotomy.
Résumé
Entre 1974 et 1987, 276 ostéotomies intertrochantériennes ont été exécutées chez 217 malades. Pour 48 hanches, l'ostéotomie a été faite pour une arthrose idiopathique. Pour 166 hanches, l'arthrose était secondaire à une dysplasie acétabulaire, pour 23 à un traumatisme, pour 14 à une épiphysiolyse fémorale, pour cinq à une maladie de Legg–Calvé–Perthes et pour 20 à une nécrose avasculaire de la tête fémorale. Les bons résultats ont été obtenus chez des jeunes femmes avec une arthrose modérée secondaire à une dysplasie acétabulaire, et chez les malades avec une arthrose post-traumatique. Toutes les autres indications ont montrées une plus mauvaise survie à longue échéance. Notre étude montre que la dysplasie acétabulaire et l'arthrose post-traumatique restent des indications valables pour l'ostéotomie intertrochantérienne.
Introduction
Whilst total hip replacement (THR) may be the best treatment option for hip osteoarthritis (OA) in the elderly, it is uncertain whether this also holds true for younger patients [6, 12]. In the short term THR shows excellent results; but in the long term, high revision rates have been reported [2, 4, 14, 16]. It is therefore important to delay the need for hip replacement in younger patients. Joint-preserving surgery can therefore be looked upon as a valid investment in a future where further hip surgery is not unusual [3, 9, 10, 15, 17, 18].
The authors report on the outcome of 276 intertrochanteric osteotomies performed for primary and secondary OA in 217 patients with 15- to 29-year follow up. Although this is a historical series that includes patients who would never undergo an intertrochanteric osteotomy today, we believe that lessons can be learned, and we wanted to identify the degenerative hip disorders for which an intertrochanteric osteotomy is still a valid option.
Patients and methods
Between 1974 and 1987 217 patients (276 hips) with primary or secondary OA of the hip underwent an intertrochanteric osteotomy. Their average age was 45.5 years (range 16–78). Sixty–three percent of the patients were female.
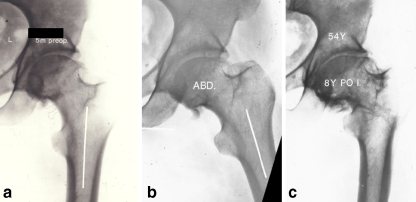
In the preoperative planning, all patients had functional radiographs in adduction and abduction [13, 14] (Fig. 1). The decision to perform an osteotomy, including which type of osteotomy, was based on radiographic improvement of congruency and containment.
Fig 1.
a A 47-year-old female with idiopathic OA. b Abduction radiograph shows improvement of congruency. A 15° varus, 15 mm medial offset and 15° extension osteotomy was performed. c After an initially good period, THR was performed for pain after 8.6 years
All separate indications combined with demographic data are listed in Table 1. The corrections performed are included. Osteoarthritis was graded according to Tönnis [22]. The CE angle [24] and Sharp angle [19] were measured where applicable. In dysplastic hips dislocation was classified according to Crowe [5]. In Legg–Calvé–Perthes' disease (LCPD) the deformity of the femoral head was classified according to Stullberg [21]. In cases with avascular necrosis of the femoral head (AVN) the Ficat as well as the Arlet stage is given.
Table 1.
Number of patients per indication with demographic data and preoperative radiological measurements
| Indication | Number of patients/hips | Average age | % female | Grade OA† (Tönnis) [22] (n hips) | Radiological measurements† [15, 17, 19] (Averages) | Dislocation† Crowe [5] (n hips) | Osteotomy (n hips) | Additional Corrections (n hips) |
|---|---|---|---|---|---|---|---|---|
| Idiopathic | 44/48 | 56.7 (34–79) | 50% | I 4 | CE 37.9 (20–62) | 26 valgus | 14 extension | |
| II 22 | Sharp 33.0 (30–46) | 22 varus | 13 IR* | |||||
| III 14 | 23 medial offset | |||||||
| Dysplasia | 114/166 | 45.8 (16–75) | 87% | 0 18 | CE 20.6 (0–46) | I 135 | 28 valgus | 166 medial offset |
| I 64 | Sharp 42.9 (32–63) | II 15 | 138 varus | 58 ER** | ||||
| II 54 | III 1 | 20 IR | ||||||
| III 20 | IV 5 | 29 extension | ||||||
| Posttraumatic | 22/23 | 37.0 (17–68) | 42% | I 8 | 16 valgus | 3 flexion | ||
| II 10 | 5 varus | 6 extension | ||||||
| III 2 | 2 rotation | 7 IR | ||||||
| SCFE | 13/14 | 43.9 (25–55) | 25% | I 2 | 11 valgus | 2 flexion/IR | ||
| II 6 | 3 varus | 5 extension | ||||||
| III 6 | 9 medial offset | |||||||
| LCPD | 5/5 | 35.6 (18–62) | 0% | I 3 | Stullberg | 5 valgus | 1 flexion | |
| II 2 | III 3 | 2 extension | ||||||
| IV 2 | 1 medial offset | |||||||
| AVN | 19/20 | 38.0 (16–60) | 40% | Ficat and Arlet | 13 valgus | 2 extension | ||
| III 8 | 6 varus | 4 ER | ||||||
| IV 12 | 1 rotation | 10 medial offset |
*IR=internal rotation
**ER=external rotation
†For some patients the preoperative radiological information could not be retrieved
All osteotomies were performed using a standard lateral approach [1, 13]. Fixation was performed with an AO 90° or 100° blade-plate with medial offsets between 10 and 20 mm. A compression device was always used.
Survival rates were analysed using the Life Table method. Clinical outcome was rated using Merle d'Aubigné's hip score (Table 2). To calculate if a correlation between sphericity, age, sex, pre-operative grade of OA, uni- or bilateral involvement, radiological measurements and the outcome was present, a Pearson correlation analysis was performed.
Table 2.
Merle d'Aubigné score
| Pain | Mobility | Ability to walk | |
|---|---|---|---|
| 0 | Intense and permanent | Ankylosis with bad position of the hip | None |
| 1 | Severe even at night | No movement; pain or slight deformity | With crutches/walking device only |
| 2 | Severe when walking; prevents any activity | Flexion under 40 degrees | With canes only |
| 3 | Tolerable with limited activity | Flexion between 40 and 60 degrees | With one cane, less than one hour; very difficult without cane and with a limp |
| 4 | Mild when walking; it disappears in rest | Flexion between 60 and 80 degrees; patients can reach his foot | A long time with a cane; short time without a cane and with a limp |
| 5 | Mild and inconstant; normal activity | Flexion between 80 and 90 degrees; abduction of at least 15 degrees | Without cane but with a slight limp |
| 6 | None | Flexion more than 90 degrees; abduction to 30 degrees | Normal |
The total score consists of the sum of the three criteria
A total of 18 points is classified as excellent, 15–17 points as good, 12–14 points as fair, and less than 12 points as poor
Results
There were 18 complications during or after the surgical procedure, of which ten were wound infections. All infections were treated with surgical debridement followed by intravenous antibiotics, and all resolved. Two osteotomies resulted in overcorrection, of which one was revised. One osteotomy resulted in undercorrection. Two patients had their plate revised due to instability, and two patients fell shortly after surgery and required a revision.
After an average of 9.5 years (range 1–25 years), 143 patients had their osteotomy converted to a THR. A further three patients required a hip fusion after 8.1 years. In ten patients, a second intertrochanteric osteotomy was performed after 10.4 years (range 5–21 years) and three patients had a periacetabular osteotomy after 9.3 years. Thirty-three patients (38 osteotomies) had died at the time of follow up, and 21 patients (22 osteotomies) were lost-to-follow-up. The 79 remaining hips in 54 patients were seen after an average follow-up of 19.4 years (range 15–28 years). All follow-up data is summarised in Table 3, including survival rates at 10 and 15 years.
Table 3.
Follow up per indication
| Indication | Number of patients/hips | Follow-up yrs (range) | n patients died** (pat/hips) | n lost to follow-up (pat/hips) | THR*: n (hips) – yrs (range) | Merle score: n(hips) – avg score (range) | 10 year survival % (95% CI) | 15 year survival % (95% CI) |
|---|---|---|---|---|---|---|---|---|
| Idiopathic | 44/48 | 22.2 (15–29) | 14/14 | 4/4 | 30 – 7.4 (1–21) | 4 – 16.5 (13–18) | 50% (34%–65%) | 32% (16%–48%) |
| Dysplasia† | 114/166 | 21.1 (15–28) | 10/14 | 9/10 | 83 – 9.7 (1–25) | 62 – 15.4 (8–18) | 72% (65%–79%) | 56% (48%–63%) |
| Posttraumatic | 22/23 | 20.3 (15–25) | 5/5 | 3/3 | 8 – 10.3 (2–25) | 8 – 14.8 (5–18) | 91% (79%–100%) | 78% (59%–97%) |
| SCFE | 13/14 | 20.3 (17–27) | 3/4 | 2/2 | 8 – 11.7 (5–19) | 1 – 16 | 71% (48%–95%) | 56% (48–63%) |
| LCPD | 5/5 | 21.2 (15–26) | 1/1 | – | 3 – 22.3 (21–25) | 1 – 15 | 100% | 100% |
| AVN | 19/20 | 22.1 (16–26) | – | 3/3 | 14 – 9.7 (1–19) | 3 – 17 (16–18) | 60% (36%–83%) | 30% (6%–53%) |
*Including 3 arthrodeses
**Some patients died after the ITO was converted to THR; these are also mentioned in the THR listing
†3 patients had an additional periacetabular osteotomy after an average of 9.3 years
In hips with idiopathic osteoarthritis, there was a statistically-significant correlation between preoperative sphericity of the femoral head and clinical outcome. In dysplastic hips, there was a significant correlation between clinical outcome and sphericity of the femoral head, age, gender, uni- or bilateral affection and grade of OA.
The survival rate for patients younger than 45 years at the time of surgery and with hip OA grade 0 or I was 100% at 10 years, and 97% at 15 years (95% CI: 92%–100%). In patients with a preceding acetabular fracture the survival rate was 92% (95% CI: 76%–100%) at 10 years, and 71% (95% CI: 43%–99%) at 15 years. The survival rate in patients operated for impingement after a previous proximal femoral fracture was 90% (95% CI: 71%–100%) at 10 years.
Discussion
The aim of this retrospective analysis was to study which surgical indications for an intertrochanteric osteotomy remain valid today. The osteotomies performed for primary OA had a poor survival and outcome, with a 15 year survival rate of only 32%. Previous reports have also shown that the outcome of an intertrochanteric osteotomy in hips with primary osteoarthritis is unpredictable and generally poor [6, 10, 17, 23]. It should be stressed that patients were classified as having an idiopathic osteoarthritis if no obvious cause could be found. Several of these patients, especially the younger ones, may probably have had a biomechanically-insufficient hip joint as the cause of the arthritic changes.
Patients with AVN had survival rate of 60% at 10 years, and 30% at 15 years. Although most of these patients had AVN stage IV, which may partially explain the poor survival rate; good long-term results of an intertrochanteric osteotomy for AVN have never been described [3, 9, 18]. The aim of the intertrochanteric osteotomy—to rotate the avascular lesion away from the weight bearing area and thereby prevent bony collapse—was hampered by the fact that most patients already had collapse and radiographic degenerative changes. Having stated this, we do not find AVN to be a valid indication for intertrochanteric osteotomy.
Osteotomies in hips with changes after slipped capital femoral epiphysis (SCFE) had a survival rate of 71% at 10 years, and 63% at 15 years. The number of patients was, however, small, and the severity of the degenerative changes too different, to allow for any definite conclusion. We believe that young patients with femoro-acetabular impingement and an early osteoarthritis may be successfully treated with an Imhauser type of osteotomy. Most of the patients in this cohort had advanced radiographic changes (grade III), in which further development of osteoarthritis could not be altered by the osteotomy. Five patients with previous LCPD reached a survival rate of 100% after 20 years. These early results have motivated us to perform more osteotomies for LCPD in recent years [15].
We have previously shown that the outcome after intertrochanteric osteotomy in patients with degenerative changes after acetabular fractures is excellent [11]. Most patients have a flexion–adduction contracture of the hip, which can be corrected by a valgus-extension osteotomy. Besides a restored alignment, the osteotomy reduces contact pressure on the damaged cartilage and reduces the contracture by altering the muscle forces. In patients with a malunited femoral neck fracture, the degenerative changes may be caused by bony impingement. By restoring the normal anatomy, the causative factor will disappear and the degenerative process is halted. In the present study, 23 patients with post-traumatic OA had a good outcome, with a survival rate of 78% at 15 years.
Good results were also found in patients with OA secondary to acetabular dysplasia (Fig. 2). This is in agreement with Jingushi et al., who reported a survival rate of 72% after 15 years for patients with degenerative changes after acetabular dysplasia treated with an intertrochanteric osteotomy [7]. In patients younger than 50 years with unilateral changes, the survival rate was as high as 95%. Good results in young patients have also been reported by D'Souza et al. [6]. Both D'Souza et al. and Jingushi et al. showed an increased long-term survival in young and active patients. We found also a better outcome in patients younger than 40, with a survival rate of 82% and 70% at 15 and 20 years respectively. Besides the age of the patients, the preoperative grade of OA is of equal importance. In patients younger than 45 years with grade 0 or 1 OA, the survival rate was 100% at 10 years and 97% at 15 years. Reigstad et al., studying long term results in a group of patients older than 50 years, found a 10 year survival rate of 58% [17]. Maistrelli et al. showed that the outcome was better in patients younger than 40 years with unilateral changes, of which 39% improved [10].
Fig 2.
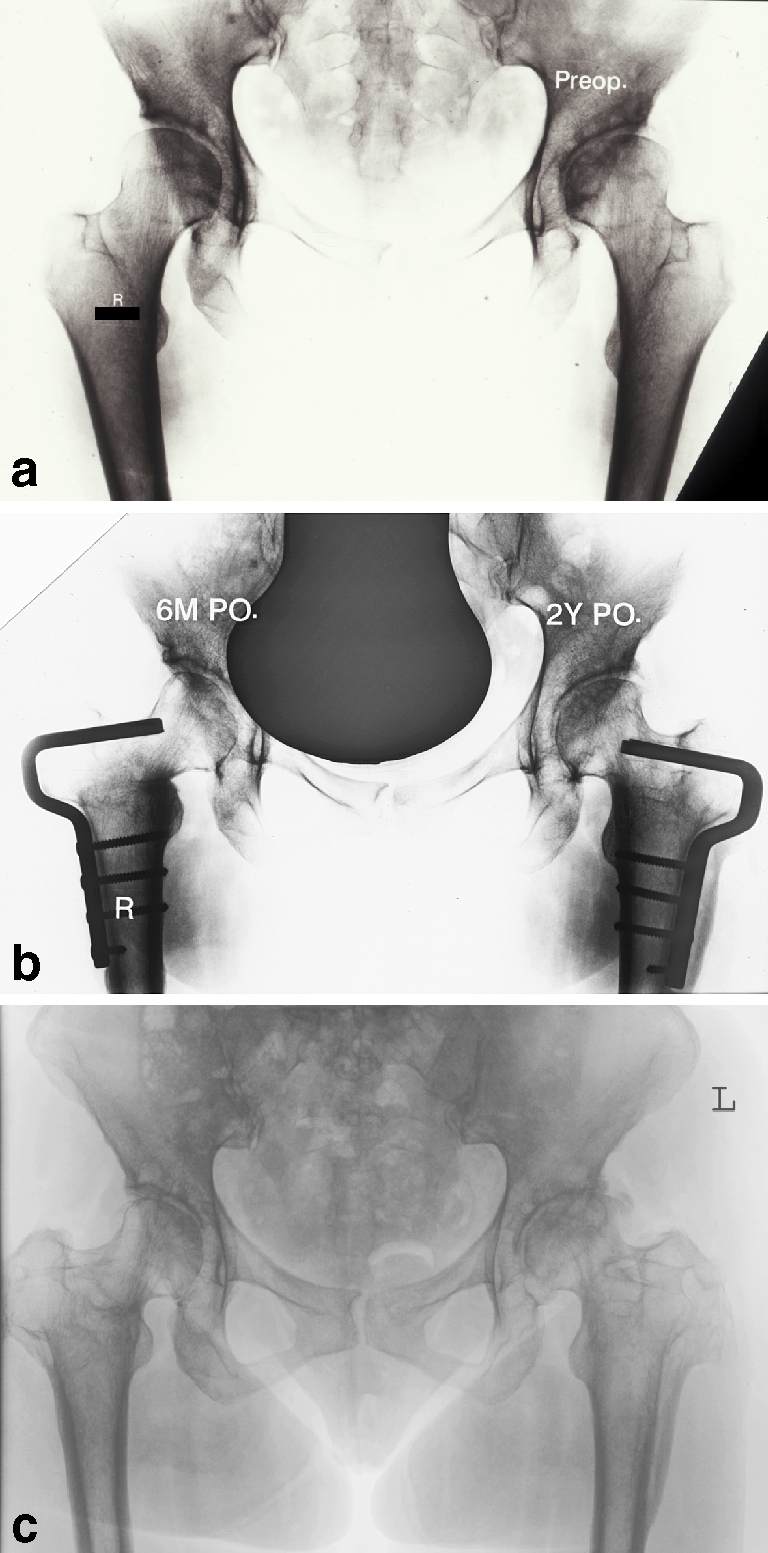
a A 35-year-old female with a dysplasia and coxa valga on both hips, the left hip is symptomatic. b Within 2 years a 15° varus osteotomy was performed in both hips. c Results after 16.5 years (right) and 18 years (left). The Merle d'Aubigné score is 13 for the left and 15 for the right hip
In patients with dysplastic hips we found a significant correlation between clinical outcome and age, gender, grade of OA, and bi- or unilateral involvement. Young female patients with bilateral involvement and slight degenerative changes scored the best results. The ideal candidate for an intertrochanteric osteotomy is therefore a young female with (bilateral) mild OA and acetabular dysplasia.
Several authors have proposed an acetabular realigning osteotomy for the treatment of stage I+II hip OA. This is especially logical for OA due to acetabular dysplasia. Siebenrock et al. [20] reported a 10 year survival rate of the Bernese periacetabular osteotomy of 82% for osteoarthritis secondary to dysplasia. De Kleuver et al. [8] showed a minimum 8-year survival rate of 93% after a Tönnis triple pelvic osteotomy at a mean age of 28 years. In this study, the overall 10-year survival rate was 72% for hips with acetabular dysplasia. The reported long-term results of the Chiari and Salter osteotomies in the treatment of osteoarthritis are scarce, but lower than that of the periacetabular osteotomy and the triple osteotomy. Relatively young patients were included in the studies of Siebenrock and de Kleuver. The 10-year survival rate in young patients with OA secondary to dysplasia and congenital hip luxation was 100%. Even if the various populations are probably not comparable, it emphasises that good results can be achieved by an intertrochanteric osteotomy. In hips with acetabular dysplasia, the femoral side is often abnormal as well, and a coxa valga is often seen. In such hips, we find an intertrochanteric osteotomy an excellent solution. In patients where the biomechanical insufficiency is mainly caused by the acetabulum, this must be corrected. The definite border between these two indications is not clear.
Several other types of joint-preserving techniques have been reported. Arthroscopy of the hip and labral debridement, removal of osteophytes and debridement of the acetabular rim through mini-open techniques or via surgical dislocation may have a place, but no long-term results have yet been reported.
The results presented in this study show that there are still valid indications for an intertrochanteric osteotomy, if OA is not too advanced. In particular, OA secondary to acetabular dysplasia with coxa valga and post-traumatic osteoarthritis are still valid indications. In all other cases good results may be achieved, but the outcome is less predictable.
References
- 1.Bombelli R, Aronson J (1984) Biomechanical classification of osteoarthritis of the hip with special reference to the treatment techniques and results. In: Schatzker J (ed) The intertrochanteric osteotomy, Springer-Verlag, Berlin Heidelberg New York, pp 67–134
- 2.Boos N, Krushell R, Ganz R, Muller ME (1997) Total hip arthroplasty after previous proximal femoral osteotomy. J Bone Joint Surg Br 79:247–253 [DOI] [PubMed]
- 3.Canadell J, Aguilella L, Azcarate JR, Valenti JR (1986) The place of intertrochanteric osteotomy in the treatment of idiopathic necrosis of the head of the femur. Int Orthop 10:41–46 [DOI] [PubMed]
- 4.Capello WN, D'Antonio JA, Feinberg JR, Manley MT (2003) Ten-year results with hydroxyapatite-coated total hip femoral components in patients less than fifty years old. A concise follow-up of a previous report. J Bone Joint Surg Am 85:885–889 [DOI] [PubMed]
- 5.Crowe JF, Mani VJ, Ranawat CS (1979) Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am 61:15–23 [PubMed]
- 6.D'Souza SR, Sadiq S, New AM, Northmore-Ball MD (1998) Proximal femoral osteotomy as the primary operation for young adults who have osteoarthrosis of the hip. J Bone Joint Surg Am 80:1428–1438 [DOI] [PubMed]
- 7.Jingushi S, Sugioka Y, Noguchi Y, Miura H, Iwamoto Y (2002) Transtrochanteric valgus osteotomy for the treatment of osteoarthritis of the hip secondary to acetabular dysplasia. J Bone Joint Surg Br 84:535–539 [DOI] [PubMed]
- 8.Kleuver de M, Kooijman MA, Pavlov PW, Veth RP (1997) Triple osteotomy of the pelvis for acetabular dysplasia: results at 8 to 15 years. J Bone Joint Surg Br 79:225–229 [DOI] [PubMed]
- 9.Maistrelli G, Fusco U, Avai A, Bombelli R (1988) Osteonecrosis of the hip treated by intertrochanteric osteotomy. A four- to 15-year follow-up. J Bone Joint Surg Br 70:761–766 [DOI] [PubMed]
- 10.Maistrelli GL, Gerundini M, Fusco U, Bombelli R, Bombelli M, Avai A (1990) Valgus-extension osteotomy for osteoarthritis of the hip. Indications and long-term results. J Bone Joint Surg Br 72:653–657 [DOI] [PubMed]
- 11.Marti RK, Chaldecott LR, Kloen P (2001) Intertrochanteric osteotomy for posttraumatic arthritis after acetabular fractures. J Orthop Trauma 15:384–393 [DOI] [PubMed]
- 12.Millis MB, Kim YJ (2002) Rationale of osteotomy and related procedures for hip preservation: a review. Clin Orthop 405:108–121 [DOI] [PubMed]
- 13.Muller ME (1984) Intertrochanteric Osteotomy: Indication, preoperative planning, technique. In: Schatzker J (ed) The intertrochanteric osteotomy, Springer-Verlag, Berlin Heidelberg New York, pp 25–66
- 14.Neumann L, Freund KG, Sorensen KH (1996) Total hip arthroplasty with the Charnley prosthesis in patients fifty–five years old and less. Fifteen to twenty–one–year results. J Bone Joint Surg Am 78:73–79 [DOI] [PubMed]
- 15.Pecasse GA, Eijer H, Haverkamp D, Marti RK (2004) Intertrochanteric osteotomy in young adults for sequelae of Legg–Calve–Perthes' disease—a long term follow-up. Int Orthop 28:44–47 [DOI] [PMC free article] [PubMed]
- 16.Raut VV, Siney PD, Wroblewski BM (1996) Revision of the acetabular component of a total hip arthroplasty with cement in young patients without rheumatoid arthritis. J Bone Joint Surg Am 78:1853–1856 [DOI] [PubMed]
- 17.Reigstad A, Gronmark T (1984) Osteoarthritis of the hip treated by intertrochanteric osteotomy. A long-term follow-up. J Bone Joint Surg Am 66:1–6 [PubMed]
- 18.Schneider R (1966) Mehrjahreresultate eines Kollektivs von 100 intertrochanteren Osteotomien bei Coxarthrose. Helvetica Chirurgica Acta 33:185–205 [PubMed]
- 19.Sharp IK (1961) Acetabular dysplasia, The acetabular angle. J Bone Joint Surg Br 43:268–273
- 20.Siebenrock KA, Scholl E, Lottenbach M, Ganz R (1999) Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:9–20 [DOI] [PubMed]
- 21.Stulberg SD, Cooperman DR, Wallensten R (1981) The natural history of Legg–Calvé–Perthes' disease. J Bone Joint Surg Am 63:1095–1108 [PubMed]
- 22.Tönnis D (1976) Normal values of the hip joint for the evaluation of X–rays in children and adults. Clin Orthop119:39–47 [PubMed]
- 23.Weisl H (1980) Intertrochanteric osteotomy for osteoarthritis. A long-term follow-up. J Bone Joint Surg Br 62:37–42 [DOI] [PubMed]
- 24.Wiberg G (1939) The anatomy and roentgenographic appearance of a normal hip joint. Acta Chir Scand 83(Suppl 58):7–38