Abstract
The present study was undertaken to identify the factors responsible for hip joint dislocation after total hip arthroplasty, laying emphasis on analysis of the background variables of the patients. Of the 317 hips included in the study, ten (3.2%) dislocated. Only the anteversion angle of the cup differed significantly between the dislocation group and the dislocation-free group. The safe zone of the anteversion angle seems to be between 20 and 30 degrees. but it is also essential to set the antetorsion angle of the stem to match the shape of individual bones to create a more stable hip joint. This safe zone may be expanded by the additive effect of antetorsion angle of the stem.
Résumé
Le but de cette étude a été d’identifier les facteurs responsables d’uneluxation de la hanche après arthroplastie totale en insistant sur l’analysedes différents paramètres de chaque patient. Sur les 317 hanches inclusesdans cette étude, 10 (3,2%) ont présenté une luxation. La seule différencesignificative entre le groupe des sujets ayant présenté une luxation et ceuxn’en ayant pas présenté est l’angle d’antéversion de la cupule. L’angleoptimum d’antéversion de la cupule semble être compris entre 20 et 30 degrésmais il est également essentiel de lier l’angle d’antéversion avec l’angled’antétorsion de la pièce fémorale, celles-ci ayant été manufacturées surmesure et adaptées à la géométrie osseuse de chaque individu de façon àcréer une hanche parfaitement stable. Cette zone de sécurité peut êtreaméliorée par l’addition, à l’angle d’antéversion de la cupule de l’angled’antétorsion de la pièce fémorale.
Introduction
Dislocation occurring after total hip arthroplasty can cause great pain and mental stress to the patient. This type of dislocation tends to be repeated and can destroy parts of the hip prosthesis, leading to functional deterioration of the prosthesis. To reduce the frequency of such dislocation, it would be essential to clarify the factors predisposing to its occurrence. The present study was undertaken to identify the factors responsible for hip joint dislocation after total hip arthroplasty, laying emphasis on analysis of the background variables of the patients (especially the component alignment).
Subjects and methods
The subjects of this study were 266 patients (317 hips in total) who were followed up for 5 years or more after primary total hip arthroplasty (THA) conducted for osteoarthritis of the hip between 1989 and 2000. The patients ranged in age from 23 to 84 years (mean: 61.6 years). There were 55 men and 211 women, and the follow-up period ranged from 5.0 to 14.7 years (mean: 8.0 years).
The prosthesis used was a product of Biomet, Inc. (Warsaw, IN, UAS) in all subjects. The stem used was a Bi-Metric® stem (neck-shaft angle, 135 degrees; with no antetortion angle; one quarter of the central part was porous-coated) for all the 317 hips. The cup was a Mallory-Head Finned porous cup for 162 hips and a metal-back cup for 155 hips. These cups had a 5-mm high wall in the range of 120 degrees on the open plane of the cup. The head diameter was 28 mm and the oscillating angle was 103 degrees in all cases. The posterior approach was used and the joint capsule was resected in all cases. The short external rotator muscles were re-sutured.
Postoperative rehabilitation in the sitting position was started one week after the operation in all cases, and rehabilitation involving walking on the feet was started two weeks after the operation.
In all these cases, the age, sex and body weight of the patients, the abductor muscle strength, inclination angle of the cup, anteversion angle of the cup, antetorsion angle of the stem, and upper and lower deviation of the head center and the greater trochanter tip were analyzed to identify the cause of the dislocation. The abductor muscle strength was evaluated manually. The inclination angle of the cup was defined as the angle formed by the line connecting the two tear drops and the line connecting the upper and lower end of the open plane of the cup on a frontal radiograph. The anteversion angle of the cup was measured by the method of Lewinnek [4], using the following equation:
 |
where a indicates the maximum vertical dimension on the open plane of the cup that passes through its center, b indicates the length of the line passing through the center and perpendicular to the aforementioned line, and β denotes the anteversion angle of the cup. The antetorsion angle of the stem was measured according to the method of Shirasu et al. [7], in an axial radiograph of the anterior plane of the knee taken at an angle of 45 degrees to the femoral axis; the angle was calculated using the following equation:
 |
where θo indicates the apparent antetorsion angle of the stem, and θa denotes the true antetorsion angle of the stem. The upper and outer deviation of the head center were calculated using the following equations:
 |
 |
where c indicates the head center, L denotes the distance between the tear drops, ca indicates the length of a line drawn perpendicular from c to the line connecting both the tear drops, cl represents the length of a line drawn perpendicular from c to a line drawn from the lower end of the postoperative teardrop perpendicular to the line connecting the two tear drops.
The upper and outer deviation were also expressed by the following equations, in which t denotes the tip of the greater trochanter:
 |
 |
Each of the parameters was compared between the dislocation group and the dislocation-free group. The significance of inter-group differences in these parameters was tested using the χ2 test and Mann-Whitney U test. P<0.05 was regarded as denoting statistical significance.
Results
Of the 317 hips included in the study, ten (3.2%) dislocated (posterior dislocation in eight hips and anterior dislocation in two hips). Of the ten hips, eight had dislocated within three months after the operation. Repeated dislocation was seen in 2 hips in which the first dislocation had occurred within one month after operation, and in one hip in which the first dislocation had occurred within three months after operation. In all of these 3 hips, the dislocation was posterior. Anterior dislocation was seen in 2 hips (one of these developed dislocation immediately after the operation and in the other, dislocation occurred two days after the operation). Recurrent dislocation was not seen in any of the cases with anterior dislocation of the hip.
The mean age of the patients did not differ significantly between the dislocation-free group (mean±SD=61.7±10.9 years) and the dislocation group (59.1±6.7 years). The male-to-female ratio did not differ significantly between the dislocation-free group (male/female=58/249) and the dislocation group (3/7). The body weight did not differ significantly between the dislocation-free group (53.6±9.3 kg) and the dislocation group (60.4±12.4 kg). The abductor muscle strength did not differ significantly between the dislocation-free group (3.90±0.67) and the dislocation group (4.0±0.38).
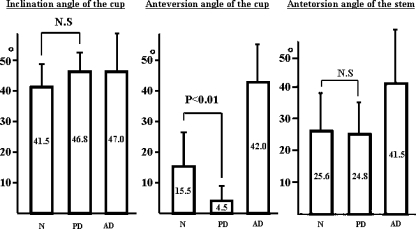
The inclination angle of the cup was 41.5±8.7 degrees in the dislocation-free group, 46.8±6.5 degrees in the posterior-dislocation group, and 47.0±12.7 degrees in the anterior-dislocation group. This parameter did not differ significantly between the dislocation-free group and the posterior-dislocation group. The anterior-dislocation group was not included in the statistical test for determining the significance of inter-group differences, since this group included only 2 hips.
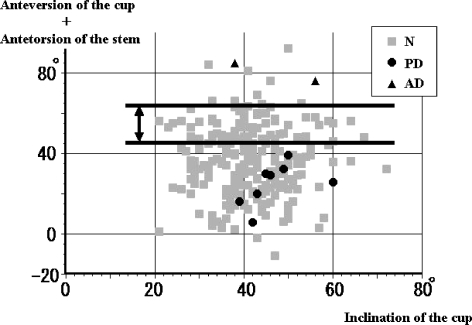
The anteversion angle of the cup was significantly smaller in the posterior-dislocation group (4.5±6.6 degrees) than in the dislocation-free group (15.5±11.9 degrees) (P<0.01). This angle was, however, rather large in the anterior-dislocation group (42.0±12.7 degrees). The antetorsion angle of the stem did not differ significantly between the dislocation-free group (25.6±11.7 degrees) and the posterior-dislocation group (24.8±9.4 degrees). This angle was large in the anterior-dislocation group (41.5±17.7 degrees) (Fig. 1).
Fig. 1.
Prosthesis setting angles N: Dislocation_free group, PD: Posterior dislocation group, AD: Anterior dislocation group
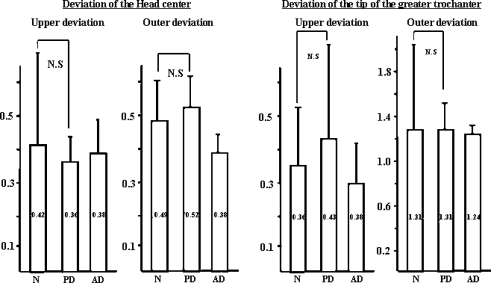
The upper deviation of the head center did not differ significantly between the dislocation-free group (0.42±0.58) and the posterior-dislocation group (0.36±0.09). This parameter in the anterior-dislocation group (0.38±0.11) was also close to that in the other two groups. The outer deviation of the head center did not differ significantly between the dislocation-free group (0.49±0.14) and the posterior-dislocation group (0.52±0.10). This parameter was slightly lower in the anterior-dislocation group (0.38±0.07). The upper deviation of the tip of the greater trochanter did not differ significantly between the dislocation-free group (0.36±0.18) and the posterior-dislocation group (0.43±0.31). This parameter in the anterior-dislocation group (0.38±0.14) was close to that in the other two groups. The outer deviation of the tip of the greater trochanter did not differ significantly between the dislocation-free group (1.31±0.76) and the posterior-dislocation group (1.31±0.26). This parameter in the anterior-dislocation group (1.24±0.09) was close to that in the other two groups (Fig. 2).
Fig. 2.
Deviation of the head center and tip of the greater trochanter
Discussion
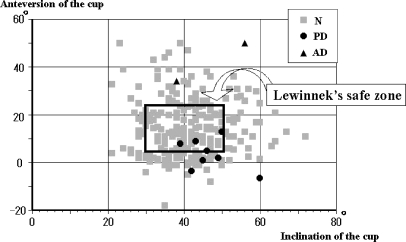
The incidence of dislocation following total hip arthroplasty varies among different reports, but it has most often been reported as 3–4% [3, 5, 8, 9]. The incidence in the present study was also in this range. Of the ten hips which dislocated eight occured within 3 months after the operation. Therefore, the period until the surrounding soft tissues are repaired completely and the pseudo-capsule of the joint is formed to an adequate extent after surgery may be deemed as the period for increased risk of dislocation. In the present study, recurrent dislocation was seen in only 3 hips. This suggests the importance of patient awareness and education about dislocation. According to the classification of dislocation proposed by Dorr [1], by which dislocation is etiologically classified as positional (Type 1), soft tissue imbalance (Type 2) and component malposition (Type 3), 4 of our cases were judged as Type 1, and 6 cases were judged as Type 3. No definite Type 2 case was determined. However, since multiple factors appeared to be involved in the etiology of the dislocation observed in some cases, it would seem difficult to simply divide the dislocation into three types. Regarding the angles of the hip prosthesis, Lewinnek et al. [4] proposed the safe zone as 30–50 degrees for the inclination angle of the cup, and 5–25 degrees for the anteversion angle of the cup. In this study, however, these angles in four of the ten dislocated hips were within the safe zone proposed by Lewinnek et al. Therefore, these safe zones may not be valid under all circumstances (Fig. 3).
Fig. 3.
Relationship of dislocation to the inclination and anteversion angles of the cup
Kadakia et al. [2] performed total hip arthroplasty using cadavers and examined the angle of hip joint flexion at varying anteversion angles and a constant inclination angle (40 degrees) of the cup, as well as the angle of adduction causing impingement and dislocation. They reported that when the angle of flexion was 105 degrees, a change in the anteversion angle of the cup from neutral to 15-degree anteversion resulted in an increase of the minimal adduction angle causing impingement from 20.9 to 31.6 and dislocation from 29.9 to 43.8 degrees. They also reported that when the adduction angle was 20 degrees, the minimal angle of flexion causing dislocation increased from 93 to 115 degrees as the anteversion angle of the cup was changed from 15-degree retroversion to neutral. Thus, they reported the importance of the anteversion angle of the cup as a factor influencing the occurrence of dislocation.
Also in our study, only the anteversion angle of the cup differed significantly between the dislocation group and the dislocation-free group, and no other setting angles were significantly different between these two groups. Therefore, the anteversion angle of the cup must be viewed as a very important factor.
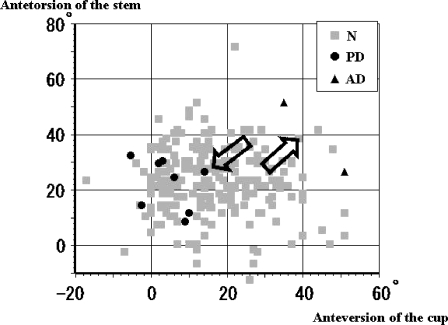
When the relationship between the anteversion angle of the cup and the antetorsion angle of the stem was analyzed, the incidence of posterior dislocation increased as the two angles became smaller, and that of anterior dislocation increased as the two angles became larger (Fig. 4). In our study, no dislocation was seen when the total of the anteversion angle of the cup and the antetorsion angle of the stem was between 45 and 65 degrees, irrespective of the magnitude of the inclination angle of the cup. As this total increased beyond this range, anterior dislocation tended to occur. As the total decreased below this range, posterior dislocation tended to develop (Fig. 5). These results suggest that the anteversion angle of the cup is the most important factor determining the development of postoperative dislocation of the hip joint, and the safe zone of this angle seems to be between 20 and 30 degrees. This safe zone may be expanded by the additive effect of antetorsion angle of the stem.
Fig. 4.
Relationship of dislocation to the anteversion angle of the cup and antetorsion angle of the stem
Fig. 5.
Relationship of dislocation to the inclination angle and the total of anteversion angle of the cup and the antetorsion angle of the stem
Like Kadakia et al. [2], Sahni et al. [6] also analyzed cup anteversion in relation to the adduction and flexion angles in a study of total hip arthroplasty in cadavers. They reported that 44% of all dislocations were caused by impingement of the stem with the acetabular line, 22% were caused by bony femur impingement on the pelvis, and 33% were independent of any impingement.
Therefore, when setting a hip prosthesis, the anteversion angle of the cup is the most important factor to be taken into consideration, but it is also essential to adjust the antetorsion angle of the stem to match the shape of individual bones to create a more stable hip joint. Finally, the tension in the soft tissues should also be borne in mind to avoid postoperative dislocation after total hip arthroplasty.
References
- 1.Dorr LD, Wolf AW, Chandler R, Conaty JP (1983) Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop 173:151–158 [PubMed]
- 2.Kadakia NR, Noble PC, Sugano N, Paravie V (1998) Posteror dislocation of the artificial hip joint: effect of cup anteversion. In: 44th Annual Meeting, Orthopaedic Research Society p 825
- 3.Levy BA, Berry DJ, Pagnano MW (2000) Long-term survivorship of cemented all-polyethylene acetabular components in patients>75 years of age. J Arthroplasty 15(4):461–467 [DOI] [PubMed]
- 4.Lewinnek GE, Lewis JL, Tarr R, Compere CL, Zimmerman JR (1978) Dislocation after total hip replacement arthroplasty. J Bone Joint Surg 60-A:217–220 [PubMed]
- 5.Li E, Meding JB, Ritter MA, Keating EM, Faris PM (1999) The natural history of a posteriorly dislocated total hip replacement 14(8):964–968 [DOI] [PubMed]
- 6.Sahni IK, Noble PC, Bartz R, Kadakia NR, Alexander JW, Paravie V (1998) Should acetabular cups be impingmented in a fixed degree of anteversion? In: 44th Annual Meeting, Orthopaedic Research Society p 826
- 7.Shirasu H, Yamamoto K, Shishido T, Masaoka T, Katori Y, Miyagawa N, Tateiwa T, Imakiire A (2003) The examination of measuring the anteversion of the stem using a simple X-ray lateral figure after THA. J Jpn Orthop Assoc S111
- 8.Woolson ST, Rahimtoola ZO (1999) Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty 14(6):662–668 [DOI] [PubMed]
- 9.Yuan L, Shih CH (1999) Dislocation after total hip arthroplasty. Arch Orthop Trauma Surg 119:263–266 [DOI] [PubMed]