Abstract
We reviewed 81 consecutive ABG I primary total hip replacements implanted in 72 patients between January 1993 and December 1998. The mean follow-up was 8.2 (range 7–12) years. There was significant polyethylene wear and osteolysis associated with the acetabular cup .The cumulative survival of the cup with revision being the end point at 8.2 years was 95.1% (95% CI: 92–97.6%). However, the cumulative survival of the cup with revision and aseptic loosening together was 72% (95% CI: 61–78%) and survival of the acetabular liner for wear was 62% (95% CI: 48–74%). Stem survival with revision being the end point was 100%. In spite of significant radiological failures of the cups, most patients remained asymptomatic. Though results of the ABG stems in this series were good, we advocate a regular follow-up of all these hips in view of the poor outcome of the cups.
Résumé
Nous avons examiné 81 prothèses totales primaires consécutives de la hanche de type ABG I chez 72 malades opérés entre janvier 1993 et décembre 1998. Le suivi moyen était de 8,2 ans (7–12 ans). Il y avait une usure notable du polyéthylène avec ostéolyse cotyloidienne . La survie à 8,2 ans de la cupule acétabulaire avec une révision comme événement final est de 95,1% (95% CI:92–97.6). Cependant la survie cumulative de la cupule acétabulaire avec révision ou descellement aseptique est de 72% (95% CI:61–78%) et la survie des inserts acétabulaires pour usure est de 62% (95% CI:48–74%). La survie de la tige avec révision comme événement final est de 100%. Malgré les échecs radiologiques des cupules, la plupart des malades sont restées asymptomatiques. Bien que les résultats des tiges ABG dans cette série soient bons, nous préconisons une surveillance régulière de ces prothèses vu le résultat médiocre des cupules cotyloidiennes.
Introduction
Failure of cemented total hip replacement (THR) led to the use of uncemented implants. The uncemented THR was devised to achieve permanent bone–implant bonding so that wear particles did not penetrate the bone–implant interface causing early loosening.
The uncemented THR has gained popularity in the young patients. Several authors have reported good early results [1, 2, 5, 10, 25, 29, 30]. However, other authors have reported early to medium-term failures with uncemented THRs [3, 6–8, 13, 19, 26, 28]. We report our medium-term clinical and radiological results of ABG I (Anatomique Benoist Gerard, Stryker Howmedica Osteonics, Newbury, UK) in young patients with the aim of determining their stability and efficacy.
Patients and methods
Between January 1993 and December 1998, 81 consecutive THRs were performed in 72 patients using the ABG I system. The mean age at operation was 52 (range 28–62) years. There were 47 male (52 hips) and 25 female (29 hips) patients. The mean follow-up was 8.2 (range 7–12) years. Preoperative diagnosis was primary osteoarthritis is 58 patients, rheumatoid arthritis in 11, secondary arthritis due to trauma in one and developmental dysplasia of the hip in one.
Clinical evaluation of all hips was done using the Harris Hip score, radiological evaluation and migration measurements were done using Johnston’s criteria and radiolucency around the acetabulum using the DeLee and Charnley zones and around the femur using Gruen zones [11, 12, 16]. Polyethylene wear of acetabular liner was measured on AP radiographs of hips using the edge-defection method .The centre of the femoral head was assumed to be the centre of the acetabulum, and each measurement was repeated to reduce intra-observer error [24]. According to Martell and Pierson, a change in the position of the acetabular component (a linear change of 2 mm or angular change of 2°) and increasing circumferential lucency were considered “definitely unstable” and loose. Any acetabular component that did not migrate but was associated with radiolucent lines in at least four of the five DeLee and Charnley zones with at least one zone having radiolucent line >2-mm wide was designated “probably unstable”. Any acetabular component that had not migrated but was associated with radiolucent lines in four of the five zones with no zone having a radiolucent line more than 2 mm was designated “possibly unstable” [17]. Areas of localised expansile cortical erosion that were at least 5-mm long or wide with discrete borders were considered “osteolytic” [30].
Results
We reviewed 81 ABG THRs with 72 patients at a mean follow up of 8.2 years (range 7–12 years). Three patients had died, with THRs in situ, of causes not related to the surgery. None of the patients were lost to follow-up. Clinical and radiological evaluation was carried out at six weeks, three months, six and 12 months and then annually.
Clinical results
The mean preoperative Harris Hip score of 42 (range 28–52) improved to 80 (range 58–86) postoperatively at the most recent follow-up. Of the hips, 38 were rated excellent, 21 good, 13 fair and ten poor.
Radiological results
According to Martell's criteria [17], 16 hips were probably loose, 11 had possible loosening and in three the acetabular component had migrated and necessitated revision. Significant supero-lateral polyethylene wear (front-side wear) was seen in 32 liners of the acetabulum (Fig. 1). Accordingly, four liners had wear of 5 mm (0.4/year), four had a wear of 7 mm (0.3/year), 14 had a wear of 9 mm (0.3/year) and ten had a wear of 13 mm (0.4/year). The highest wear rate was seen in small cups with large heads (46-mm cups with 28-mm heads); 28 of these hips are awaiting urgent revision as failure seems imminent. None of the stems were deemed unstable, and none have been revised to date.
Fig. 1.
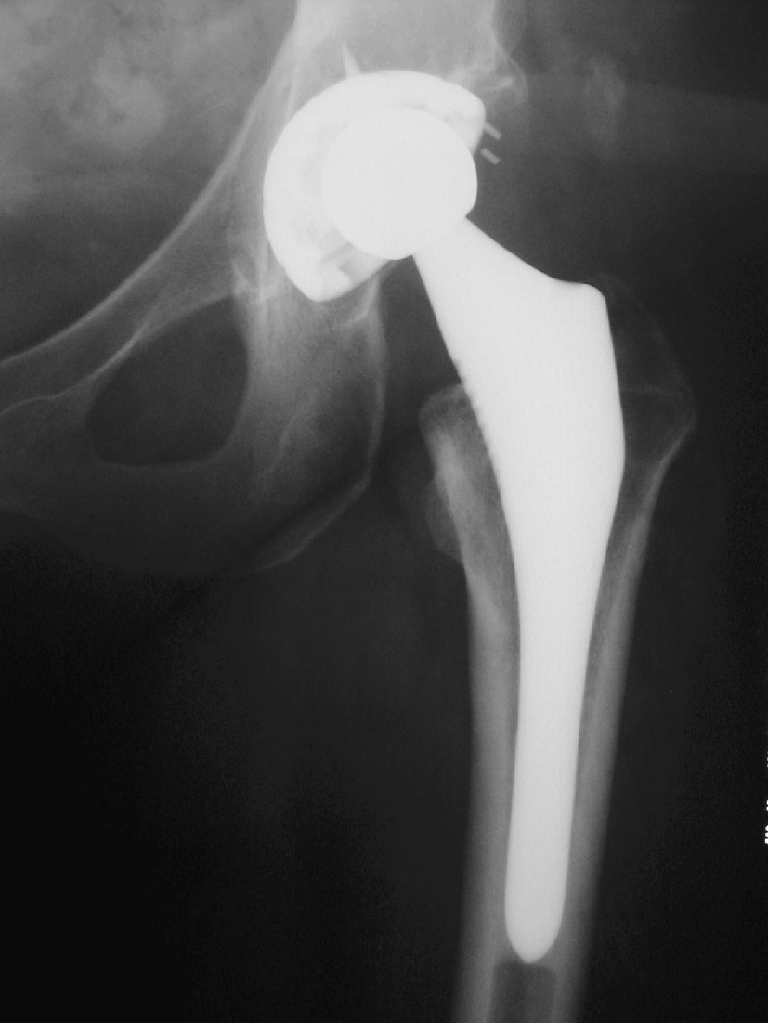
ABG acetabular cup showing significant superolateral polyethylene wear
Kaplan Meier survival analysis with revision being the end point was 95.7% (95% CI: 92–97.6%). However, because of increased polyethylene wear, the survival analysis of ABG I acetabular cup with revision and cups awaiting revision for liner wear being the end point is 57.2% (95% CI: 48–68.5%); survival analysis of the acetabular cup for liner wear awaiting revision being the end point is 60.5% (95% CI: 52–72%); polyethylene wear and aseptic loosening being the end point is 42% (95% CI: 32–52%) and revision of acetabular cups and aseptic loosening being the end point is 72% (95% CI: 61–78%). Thus, acetabular cups with increased polyethylene wear necessitating revision have contributed significantly to the deterioration of survival of the ABG I cups. However, none of the femoral stems have been revised to date.
Discussion
Advanced cementing techniques have led to improved survival of cemented stems in total hip arthroplasty. However, aseptic loosening of the acetabular cup still remains a problem in the outcome of total hip arthroplasty. These observations have led to a move away from cemented cup designs to uncemented implants. There are varying reports of success with the use of uncemented cups. Ali and Kumar reported a 10-year survival of 97.9% using a hydroxyapatite-coated RM (Robert Mathys) cup with revision of acetabular component for any cause as the end point [1]. Wilkinson et al. reported a 98% survival of the plasma cup at five years [29]. Spicer et al., in their series of 199 total hip arthroplasty performed using porous-coated hemispherical press-fit acetabular cups, had no revision at 91.5 months. They reported increased polyethylene wear requiring liner replacement in two cases. All the cups were classified as stable radiologically.[25]
However, varying reports of failure of uncemented acetabular cups have prompted the need for regular follow-up of these patients. Effenberger et al. reported a survival of 72% at 13 years using a Zweymuller (ZM) acetabular cup [7]. Fernandez-Gonzales et al. reported a ZM cup failure of 16% at six years [8]. Hernandez-Vasquero et al. reported a survival of 77.5% at 5.5 years using the threaded acetabular cup [15]. Brujin et al. reported a migration of 25% of threaded cups at 4.5 years [4].
Various studies have reported good early results with ABG hips. Tonino et al., Giannikas et al. and Rogers et al. reported an ABG I cup survival of 99.2%, 96.8% and 95% at 4.8–6 years, respectively [10, 20, 27]. However, contrasting with these results, Blacha et al., Gallo et al. and Duffy et al. reported an ABG cup survival of 89%, 82% and 76% at five–six years [3, 6, 9]. The main concerns of all of the above studies were increased polyethylene wear of up to 60% (Table 1).
Table 1.
ABG I acetabular cup survival
| No. | Authors | No. of hips | Follow-up (mean) (years) | Cup survival (revision)(%) | Concerns |
|---|---|---|---|---|---|
| 1. | Giannikas [10] | 71 | 4.8 | 96.8 | Increased wear (60%) |
| 2. | Tonino [27] | 398 | 6 | 99.2 | – |
| 3. | Rogers A [20] | 100 | 6 | 95 | Increased wear |
| 4. | Blacha J [3] | 65 | 5 | 89 | Increased wear (59%) |
| 5. | Gallo J [9] | 506 | 6 | 82 | Increased wear |
| 6. | Duffy P [6] | 97 | 5.9 | 76 | Increased wear |
| 7. | Present study | 81 | 8.2 | 95.7 | Increased wear (60%) |
Duffy et al. suggested that the ABG cups failed because of poor locking mechanism of the polyethylene liner, causing increased back-side wear [6]. Gallo et al. suggested that a thin polyethylene liner in a small cup caused increased polyethylene wear [9]. Salvati et al. suggested that these wear particles were the most important causative factors for secondary wear and osteolysis [21]. McKellop et al. reported the effect of sterilisation on wear characteristics of acetabular cups. They suggested that gamma irradiation of the polyethylene liner in air leads to increased oxidative degeneration and poor wear characteristics, causing front-side wear [18]. Schmalzried et al. reported the effect of inclination of the acetabular component and its impact on osteolysis and poyethylene wear. They suggested that an increase in inclination of the acetabular component caused point loading and eccentric polyethylene wear [22]. They further reported increased polyethylene wear in young patients with increased activity [23]. Hendrix et al. reported that polyethylene wear was the main cause of osteolysis [14]. All the above factors have been suggested to contribute to the failure of the ABG I acetabular cup with increased polyethylene wear.
Significant osteolysis and bone loss usually is seen by the time the patient becomes symptomatic. Clinical symptoms sometimes do not correlate with radiological acetabular loosening. Hence, uncemented hips need regular follow-up so that revision of the prosthesis can be carried out when prosthesis failure seems imminent, allowing the preservation of as much bone stock as possible. “Silent osteolysis” with significant polyethylene wear in young asymptomatic patients requires careful follow-up.
The clinical results in our study are good. However, radiological studies do reveal eccentric superolateral polyethylene wear (front-side wear) and osteolysis, and 28 of these hips are awaiting urgent revision. We suggest long-term follow-up of these patients with a view to evaluating polyethylene wear and osteolysis.
References
- 1.Ali MS, Kumar A (2003) Hydroxiapatite coated RM cup in primary hip arthroplasty 27:90–93 [DOI] [PubMed]
- 2.Araujo CG, Gonzales FJ, Tonino A (1998) International ABG study group. Rheumatoid Arthritis and hydroxyapatite coated hip prosthesis: five year results. J Arthroplasty 6:660–667 [DOI] [PubMed]
- 3.Blacha J (2004) High Osteolysis and revision rate with hydroxyapatite coated ABG hip prosthesis. 65 hips in 56 patients followed for 6–9 years. Acta Orthop Scand 75(3):276–282 [DOI] [PubMed]
- 4.Bruijn JD, Seelen RM, Feenstra RM, Hansen BE, Bernoski FP (1995) Failure of Mecring screw-ring acetabular component in total hip arthroplasty. A 3 to 7-year follow-up study. J Bone Joint Surg Am 77:760–766 [DOI] [PubMed]
- 5.DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 121:20–32 [PubMed]
- 6.Duffy P, Sher JL, Partington PF (2004) Premature wear and Osteolysis in HA coated uncemented total hip arthroplasty. J Bone Joint Surg Br 86:36–38 [PubMed]
- 7.Effenberger H Ramsaver T, Dorn U, Imhof M (2004) Factors influencing the revision rate of Zweymuller acetabular cup. Int Orthop 28:155–158 [DOI] [PMC free article] [PubMed]
- 8.Fernandez-Gonzalez J, Canosa Sevillano R, Garcia Araujo C (1997) Cementless total hip arthroplasty with threaded cup. Int Orthop 21:327–331 [DOI] [PMC free article] [PubMed]
- 9.Gallo J, Kaminek P, Zapletalova J (2003) Early failure of polyethylene liner in ABG I total hip prosthesis. Acta Chir Orthop Traumatol Cech 70:343–349 [PubMed]
- 10.Giannikas KA, Din R, Sadiq S, Dunningham TH (2002) Medium term results of ABG total hip arthroplasty in young patients. J Arthroplasty 17:184–188 [DOI] [PubMed]
- 11.Gruen TA, McNeice GM, Amstutz HC (1979) "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop 141:17–27 [PubMed]
- 12.Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures. Treatment by mould arthroplasty. J Bone Joint Surg Am 51:737–755 [PubMed]
- 13.Heekin RD, Callaghan JJ, Hopkinson WJ (1993) The porous coated anatomic total hip prosthesis inserted without cement. J Bone Joint Surg Am 75:77–91 [DOI] [PubMed]
- 14.Hendrix RW, Wixon RL, Rana NA, Rogers LF (1983) Arthrography after total hip arthroplasty. A modified technique used in the diagnosis of pain. Radiology 148:647–652 [DOI] [PubMed]
- 15.Hernandez-Vaquero D, Suarez Vazquez A, Fernandez-Corona C, Menendez-Vinvela G, Alegre-Matio R, Garcia-Sandoval MA (1996) Loosening of threaded acetabular cups in arthroplasty of the hip. The association with different types of coxarthrosis. Int Orthop 20:70–74 [DOI] [PubMed]
- 16.Johnston RC, Fitzgerald RH, Harris WH (1990) Clinical and Radiological evaluation of total hip replacement. J Bone Joint Surg Am 72:161–168 [PubMed]
- 17.Martell JM, Pierson RH 3rd, Jacobs JJ (1993) Primary total hip reconstruction with titanium fibre coated prosthesis inserted without cement. J Bone Joint Surg Am 75:554–571 [DOI] [PubMed]
- 18.Mckellop H, Shen FW, Lu B, Campbell P, Salovey R (2000) Effect of sterilization method and other modifications on the wear resistance of acetabular cups made of ultra-high molecular weight polyethylene. A hip-simulator study. J Bone Joint Surg Am 82:1708–1725 [DOI] [PubMed]
- 19.Owen TD, Moran CG, Smith SR, Pinder IM (1994) Results of uncemented porous-coated anatomic total hip replacement. J Bone Joint Surg Br 76:258–262 [PubMed]
- 20.Rogers A, Kulkarni R, Downes EM (2003) The ABG hydroxyapatite-coated hip prosthesis: one hundred consecutive operations with average 6-year follow-up. J Arthroplasty 18:619–625 [DOI] [PubMed]
- 21.Salvati E, Lieberman J, Huko, Evans B (1995) Complications of femoral and acetabular modularity. Clin Orthop Relat Res 319:85–93 [PubMed]
- 22.Schmalzried TP, Guttmann D, Grecula M, Amstutz HC (1994) The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am 76:677–688 [DOI] [PubMed]
- 23.Schmalzried T, Shepherd EF, Dorey FJ (2000) The John Charnley Award. Wear is a function of use, not time. Clin Orthop Relat Res 381:36–46 [DOI] [PubMed]
- 24.Shih CH, Lee PC, Chen JH (1997) Measurement of polyethylene wear in cementless total hip arthroplasty. J Bone Joint Surg Br 79:361–365 [DOI] [PubMed]
- 25.Spicer DD, Scharper LA, Pomeroy DL, Badenhausen We Jr, Curry JI, Suthers KE, Smith MW (2001) Cementless cup fixation in total hip arthroplasty after 5–8 years. Int Orthop 25:286–289 [DOI] [PMC free article] [PubMed]
- 26.Tompkins GS, Jacobs JJ, Kull LR (1997) Primary total hip arthroplasty with a porous-coated acetabular component. Seven-to-ten-year results. J Bone Joint Surg Am 79:169–176 [DOI] [PubMed]
- 27.Tonino AJ, Rahmy AI (2000) The hydroxyapatite–ABG hip system: 5- to 7-year results from an international multicentre study. The International ABG Study Group. J Arthroplasty 15:274–282 [DOI] [PubMed]
- 28.Von Schewelow T, Sanzen L, Onsten I, Carlsson A (2004) Catastrophic failure of an uncemented acetabular component due to high wear and osteolysis: an analysis of 154 omnifit prostheses with mean 6-year followup. Acta Orthop Scand 75:283–294 [DOI] [PubMed]
- 29.Wilkinson JM, Gordan A, Stockley I (2003) Experiences with the Plasmacup—early stability, wear, remodelling and outcome. Int Orthop 27 (Suppl 1):16–19 [PubMed]
- 30.Zicat B, Engh CA, Gokcen E (1995) Patterns of osteolysis around total hip components inserted with and without cement. J Bone Joint Surg Am 77:432–439 [DOI] [PubMed]


