Abstract
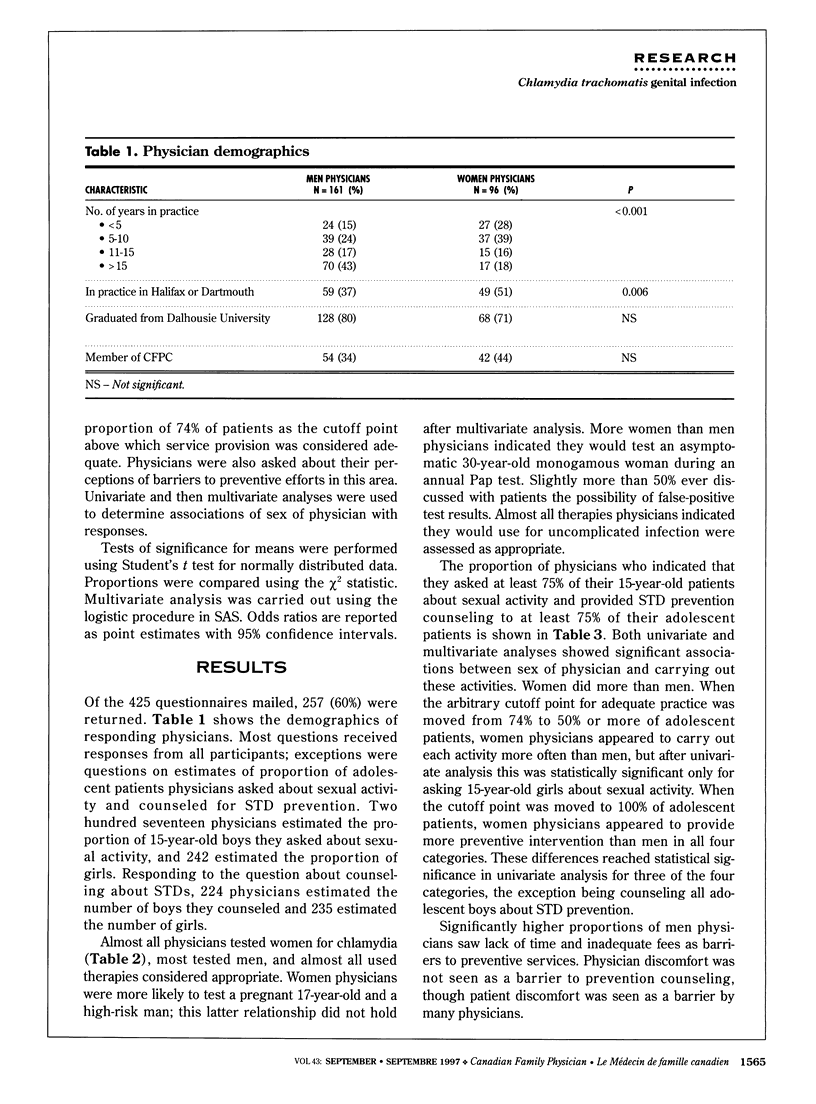
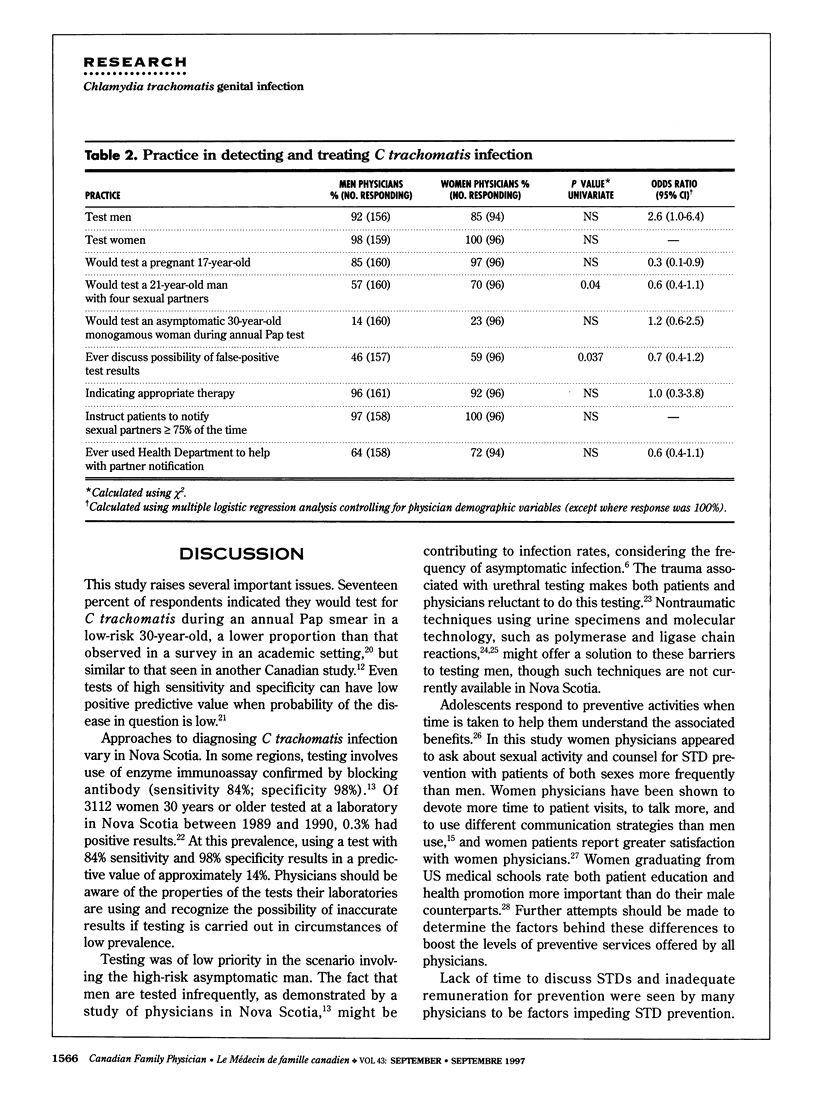
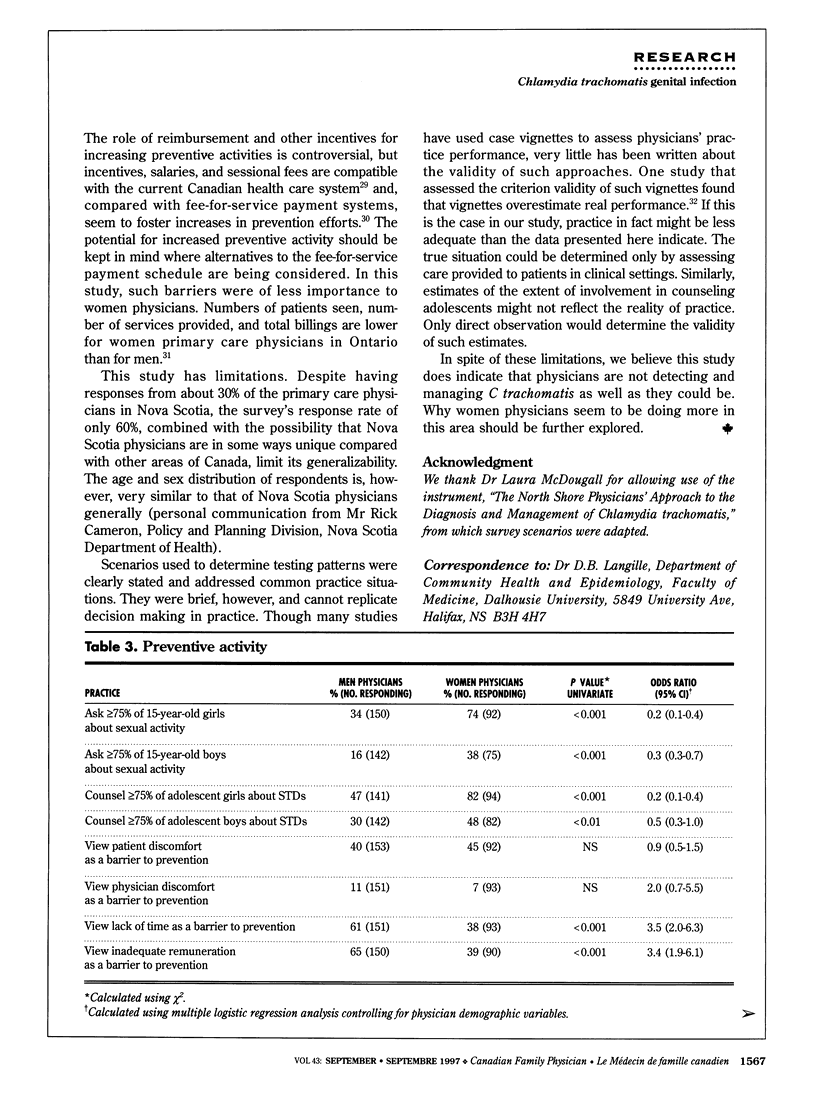
OBJECTIVE: To determine family physicians' approaches to detecting, managing, and preventing genital Chlamydia trachomatis infection and their perceptions of barriers to prevention. To determine whether sex of physician is associated with differences in clinical approach to chlamydia, with levels of effort aimed at its prevention, and with perceived barriers to preventive efforts. DESIGN: Questionnaires were sent to a random sample of family physicians. SETTING: All health regions in Nova Scotia. PARTICIPANTS: Two hundred fifty-seven Nova Scotia family physicians. MAIN OUTCOME MEASURES: Responses to survey questions analyzed for association of practice behaviours with sex of physician. RESULTS: Response rate was 60%. Most physicians performed diagnostic tests for chlamydia on all patients. Responses indicated that 17% would test for C trachomatis during an annual Papanicolaou test in a low-risk 30-year-old, 61% would test a high-risk 21-year-old man, and 89% would test a pregnant 17-year-old. Therapies physicians might use were judged appropriate in 96% of responses. Only 51% indicated they would ever discuss false-positive test results with patients. Men physicians were less likely than women to ask 75% or more of their adolescent patients about sexual activity or to educate them about prevention of sexually transmitted diseases. Women physicians saw time and the fee schedule as less serious barriers to prevention than men did. CONCLUSIONS: Some physicians are not managing C trachomatis well. We should explore situations where gaps in performance are associated with sex of physician.
Full text
PDF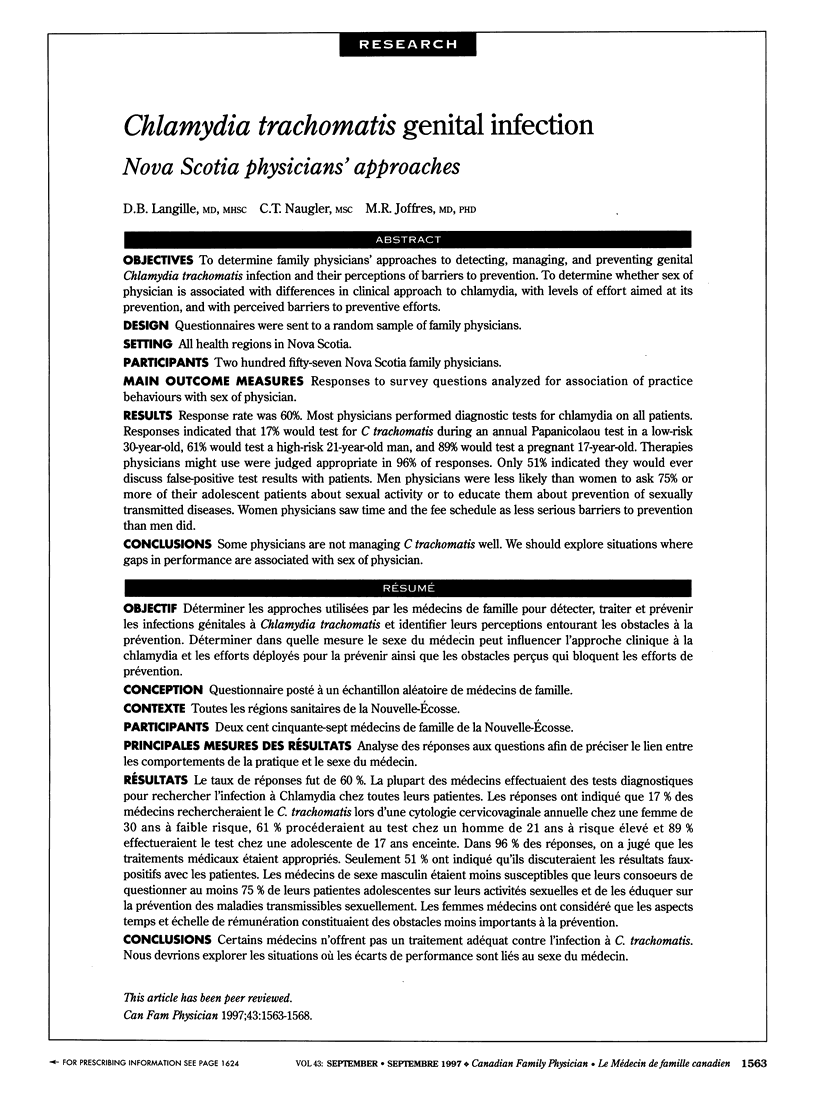

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Aronson M. D., Phillips R. S. Screening young men for chlamydial infection. JAMA. 1993 Nov 3;270(17):2097–2098. [PubMed] [Google Scholar]
- Battista R. N., Williams J. I., MacFarlane L. A. Determinants of preventive practices in fee-for-service primary care. Am J Prev Med. 1990 Jan-Feb;6(1):6–11. [PubMed] [Google Scholar]
- Bauwens J. E., Clark A. M., Loeffelholz M. J., Herman S. A., Stamm W. E. Diagnosis of Chlamydia trachomatis urethritis in men by polymerase chain reaction assay of first-catch urine. J Clin Microbiol. 1993 Nov;31(11):3013–3016. doi: 10.1128/jcm.31.11.3013-3016.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cates W., Jr Sexually transmitted organisms and infertility: the proof of the pudding. Sex Transm Dis. 1984 Apr-Jun;11(2):113–116. [PubMed] [Google Scholar]
- Chernesky M. A., Jang D., Lee H., Burczak J. D., Hu H., Sellors J., Tomazic-Allen S. J., Mahony J. B. Diagnosis of Chlamydia trachomatis infections in men and women by testing first-void urine by ligase chain reaction. J Clin Microbiol. 1994 Nov;32(11):2682–2685. doi: 10.1128/jcm.32.11.2682-2685.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chow J. M., Yonekura M. L., Richwald G. A., Greenland S., Sweet R. L., Schachter J. The association between Chlamydia trachomatis and ectopic pregnancy. A matched-pair, case-control study. JAMA. 1990 Jun 20;263(23):3164–3167. [PubMed] [Google Scholar]
- Comstock L. M., Hooper E. M., Goodwin J. M., Goodwin J. S. Physician behaviors that correlate with patient satisfaction. J Med Educ. 1982 Feb;57(2):105–112. doi: 10.1097/00001888-198202000-00005. [DOI] [PubMed] [Google Scholar]
- Fennema K., Meyer D. L., Owen N. Sex of physician: patients' preferences and stereotypes. J Fam Pract. 1990 Apr;30(4):441–446. [PubMed] [Google Scholar]
- Graham J. M., Blanco J. D. Chlamydial infections. Prim Care. 1990 Mar;17(1):85–93. [PubMed] [Google Scholar]
- Langille D. B., Shoveller J. Chlamydia trachomatis infection in rural Nova Scotia. CMAJ. 1993 Nov 1;149(9):1267–1272. [PMC free article] [PubMed] [Google Scholar]
- Langille D. B., Shoveller J. Partner notification and patient education for cases of Chlamydia trachomatis infection in a rural Nova Scotia health unit. Can J Public Health. 1992 Sep-Oct;83(5):358–361. [PubMed] [Google Scholar]
- Lomas J. Words without action? The production, dissemination, and impact of consensus recommendations. Annu Rev Public Health. 1991;12:41–65. doi: 10.1146/annurev.pu.12.050191.000353. [DOI] [PubMed] [Google Scholar]
- Lurie N., Slater J., McGovern P., Ekstrum J., Quam L., Margolis K. Preventive care for women. Does the sex of the physician matter? N Engl J Med. 1993 Aug 12;329(7):478–482. doi: 10.1056/NEJM199308123290707. [DOI] [PubMed] [Google Scholar]
- McDougall L., Mathias R. G., O'Connor B. A., Bowie W. R. Management of Chlamydia trachomatis genital infections: reported practices of primary care physicians. CMAJ. 1992 Mar 1;146(5):715–721. [PMC free article] [PubMed] [Google Scholar]
- Roter D., Lipkin M., Jr, Korsgaard A. Sex differences in patients' and physicians' communication during primary care medical visits. Med Care. 1991 Nov;29(11):1083–1093. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- Sandvik H. Criterion validity of responses to patient vignettes: an analysis based on management of female urinary incontinence. Fam Med. 1995 Jun;27(6):388–392. [PubMed] [Google Scholar]
- Thelin I., Wennström A. M., Mårdh P. A. Contact-tracing in patients with genital chlamydial infection. Br J Vener Dis. 1980 Aug;56(4):259–262. doi: 10.1136/sti.56.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weyman K., Lanning A. R. Screening guidelines for Chlamydia trachomatis infection. Evaluating physician awareness, agreement, and use. Can Fam Physician. 1995 Feb;41:228–236. [PMC free article] [PubMed] [Google Scholar]
- Woodward C. A., Hurley J. Comparison of activity level and service intensity of male and female physicians in five fields of medicine in Ontario. CMAJ. 1995 Oct 15;153(8):1097–1106. [PMC free article] [PubMed] [Google Scholar]
- Zyzanski S. J., Stange K. C., Kelly R., Flocke S., Shank J. C., Chao J., Jaén C. R., Smith C. K. Family physicians' disagreements with the US Preventive Services Task Force recommendations. J Fam Pract. 1994 Aug;39(2):140–147. [PubMed] [Google Scholar]



