Abstract
Endothelial progenitor cells (EPCs) have been shown to be involved in vascular regeneration and angiogenesis in experimental diabetes. Because insulin therapy mobilizes circulating progenitor cells, we studied the effects of insulin on outgrowth of EPCs from peripheral blood mononuclear cells of healthy volunteers and patients with type 2 diabetes. Insulin increased the formation of EPC colony-forming units in a dose-dependent manner, half-maximal at 1.5 nM and peaking at 15 nM. Inhibiting the insulin receptor with neutralizing antibodies or antisense oligonucleotides had no effect on EPC outgrowth.1 In contrast, targeting the human insulin-like growth factor 1 (IGF-1) receptor with neutralizing antibodies significantly suppressed insulin-induced outgrowth of EPCs from both healthy controls and patients with type 2 diabetes. This IGF-1 receptor–mediated insulin effect on EPC growth was at least in part dependent on MAP kinases2 and was abrogated when extracellular signal–regulated kinase 1/2 (Erk1/2) and protein kinase 38 (p38) activity was inhibited. To study the functional relevance of the observed insulin effects, we studied EPC-induced tube formation of bovine endothelial cells in vitro. Insulin-stimulated EPCs incorporated into the endothelial tubes and markedly enhanced tube formation. In conclusion, this is the first study showing an insulin-mediated activation of the IGF-1 receptor leading to an increased clonogenic and angiogenic potential of EPCs in vitro.
INTRODUCTION
Impaired outgrowth and clonogenic potential of endothelial progenitor cells (EPCs) in vitro has been defined as a marker for cardiovascular risk and endothelial dysfunction (1), predicting the occurrence of cardiovascular events and mortality in patients suffering from coronary artery disease (2). In experimental settings, EPCs have been shown to take part in angiogenesis and vascular repair (3) and seem to be involved in the process of wound healing (4). Clinical pilot studies indicate a beneficial effect of progenitor cell application in patients with myocardial infarction, peripheral artery disease, and wound healing (5–7); therapeutic application of CD34+ blood cells in wound healing and ischemia was particularly effective in animal models of diabetes (8–11). Originally, EPCs carrying antigens of hematopoietic progenitor cells were defined by sorting of CD34+ cells and subsequent outgrowth in endothelial cell growth medium in vitro (3). Later, different circulating mononuclear cells were isolated that gave rise to an endothelial phenotype under cell culture conditions. These cell lines can be divided into a) a true progenitor cell line differing from the CD34+/CD133+ hematopoietic progenitor cells of the nonadherent fraction of peripheral blood mononuclear cells (PBMCs) (3,12,13) and b) macrophage/monocyte–derived cells transdifferentiating under endothelial cell growth conditions (14,15).
In diabetes types 1 and 2, in vitro outgrowth and angiogenic function of EPCs is diminished (16,17), whereas numbers of circulating CD34+/133+ cells in patients with poorly controlled type 2 diabetes are not impaired (18). This implies a dysfunctional proliferation and differentiation of EPCs that can potentially be reversed by pharmaceutical intervention. Consistently, rosiglitazone (19), statins (20), and angiotensin II antagonists (21) have been shown to increase in vitro outgrowth of EPCs from PBMCs. Because insulin therapy led to an increase in the number of circulating CD34+/133+ progenitor cells in poorly controlled type 2 diabetes patients (18), it is crucial to understand the influence of human insulin and analogs on EPC outgrowth from PBMCs and cellular signaling cascades involved in this process.
Insulin binds to its receptor with high affinity (~0.01 nM), whereas the affinity of human insulin for the IGF-1 receptor is markedly lower (~200 nM) (22). Moreover, insulin/IGF-1 hybrid receptors containing the A isoform of the insulin receptor (IR) can bind human insulin with a higher affinity than IGF-1 receptors (IC50 ~ 3.7 nM) and are abundant on endothelial cells (23,24). In vitro, human insulin was shown to elicit mitogenic effects in an osteosarcoma cell line with an EC50 of ~ 4 nM, whereas metabolic effects were mediated at ~45 pM (22). In addition, insulin stimulated IGF-1 receptor Tyr phosphorylation in endothelial cells at concentrations ranging from 0.5 to 100 nM (25). Therefore, therapeutic concentrations of insulin might interact with insulin receptors, IGF-1, or hybrid receptors to stimulate the angiogenic potential of EPCs.
In this study, insulin effects on clonogenic potential of circulating EPCs, signaling cascades involved, and the functional relevance in vitro were studied in healthy volunteers and patients with type 2 diabetes to identify a possible new interventional target for the treatment of vascular complications in diabetes.
MATERIALS AND METHODS
Cell Culture, EPC Colony-Forming Assay, and Tube Formation
The outgrowth assay of EPCs in vitro was performed by a standard method indicating clonogenic potential of circulating EPCs as described in detail (1,26,27). In brief, mononuclear cells were isolated from 30–80 mL whole blood of healthy volunteers ages 25–30 years and 10 patients with type 2 diabetes by density gradient centrifugation (lymphocyte separation; PAA Laboratories, Pasching, Austria) according to the guidelines of the local ethics committee. The characteristics of the type 2 diabetes patients were as follows: 3 women and 7 men, age 62 ± 4 years, diabetes duration of 13 ± 7 years, HbA1c 7.5% ± 1.5%, fasting blood glucose 8.5 ± 3.9 mM, body mass index 32.4 ± 5.9. Five patients were treated with insulin and five with oral antidiabetic medication.
PBMCs were preplated in tissue culture flasks (Sarstedt, Nuembrecht, Germany) in Medium199 (Invitrogen, Karlsruhe, Germany) supplemented with 20% fetal calf serum (PAA Laboratories) and penicillin/streptomycin/glutamine (Bio Whittacker, Walkersville, MD, USA) to allow adhesion of fast-adherent, differentiated cells. No endothelial cell growth factors were added, to avoid activation of signaling cascades studied. After 48 h, nonadherent cells were counted, and 106 cells were plated on 24-well plates coated with 25 μg/mL fibronectin (Sigma, St. Louis, MO, USA) and cultured in the same growth medium (see above) without additional growth factors. Medium was changed after 3 days. Outgrowth of EPCs was quantified by counting of colony-forming units (CFUs) (Figure 1a). EPCs were grown under different conditions using different concentrations of human insulin (0.015 to 1500 nM; Sanofi Aventis) and insulin analogs that were purchased from the respective suppliers (lispro, Lilly Germany; aspart and detemir, Novo Nordisk; glulisin and glargine, Sanofi Aventis). In addition, EPCs were grown in medium supplemented with different concentrations (20–600 ng/mL) of recombinant human IGF-1 (Biosource, Camarillo, CA, USA).
Figure 1.
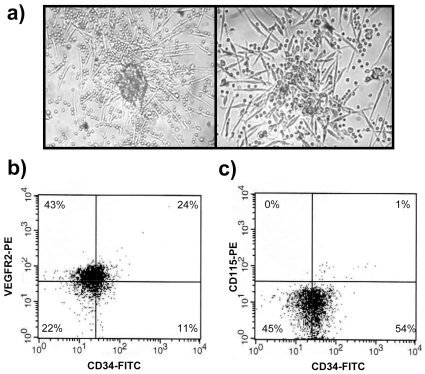
(a) Images of EPC colony-forming units (right 10×, left 20×). Mononuclear cells were preplated for 2 days to remove the population of fast-adhering, already differentiated cells. Pictures show representative colonies on day 6 after plating of the nonadherent cell fraction in culture. Representative flow cytometric analyses of cells positive for CD34/VEGFR-2 (b) and CD34/CD115 (c) antigen after 6 days in culture are shown.
For study of in vitro tube formation, insulin-stimulated and control EPCs growing from 2 × 106 cells in the CFU assay on day 6 were cocultured with 105 bovine aortic endothelial cells (BAECs) on matrigel (BD Biosciences, Heidelberg, Germany) after washing of EPCs to avoid transfer of significant amounts of insulin. Tube formation and incorporation of EPCs into tubes was studied after 12 h. To study the incorporation of EPCs into endothelial tubes, EPCs were marked using CM-DiI cell tracker (Molecular Probes/Invitrogen, Carlsbad, CA, USA) at a concentration of 2 μM as described by the manufacturer. Briefly, EPCs were harvested on day 6 in the CFU assay, washed, and stained with CM-DiI for 5 min at room temperature and 15 min at 4°C. EPCs were washed again and cultured on matrigel with 105 BAECs.
Characterization of EPCs
EPCs were characterized by flow cytometric analysis as described in detail (18) using antibodies specific for CD34 (Miltenyi Biotec GmbH, Germany), VEGFR-2 (R&D Systems, Minneapolis, MN, USA ), CD133 (Miltenyi Biotec GmbH), CD31, CD45, CD146 (BD Biosciences Pharmingen, Franklin Lakes, NY, USA), CD115 (E-Bioscience, San Diego, CA, USA), and CD62E (Cymbus Biotechnology Ltd., Chandlers Ford, UK). All measurements were normalized for autofluorescence and unspecific receptor binding using FITC- (Pharmingen BD Biosciences) and PE-labeled isotype controls, and sorted on a FACScalibur fluorocytometer (BD Biosciences). In addition, cells were stained with a FITC-labeled anti-CD34 antibody (Miltenyi Biotec GmbH) and isotype controls in vitro and visualized on a fluorescence microscope (Olympus, Hamburg, Germany).
Receptor Inhibition Using Neutralizing Antibodies
The neutralizing IGF-1 receptor antibody (Calbiochem, San Diego, CA, USA) was used at a concentration of 1 μg/mL and a neutralizing IR antibody (Chemicon International, Temecula, CA, USA) at a concentration of 10 nM, as suggested by the manufacturers, as well as 100 nM. The antibodies were added to the medium on day 2 after preplating.
Gene Silencing Using Antisense Oligonucleotides
For silencing of the IR gene, the cells were incubated with 0.1 μM antisense oligonucleotides (28). The antisense oligonucleotide was designed using the region from 107 to 131 bp of the published sequence for the human IR (acc. no. NM_000208.1). Scrambled oligonucleotide served as control. Oligonucleotides were chemically modified by introduction of phosphorothioate (PTO) links, in which a nonbridging phosphate oxygen molecule was substituted by sulfur to protect oligonucleotides from serum- and nuclease-mediated degradation as described in detail (28). The following sequences were used: 5′-cCC CCG CcG GCC CCc GGT GCC cAT-3′ antisense and 5′-cGC TCC GcC CCC GGc ATC CGC gCC-3′ scrambled (small letters indicate positions of PTO modifications). Antisense oligonucleotides were added to the medium on day 2 after preplating, and renewed every 48 h. To study the efficiency of this experiment, cells were harvested on days 3 and 6, RNA was isolated (RNeasy Mini Kit, Qiagen GmbH, Germany), and RT-PCR was performed using primers for the human IR (forward: 5′-CAA TGG TCT GAT CGT GCT GT-3′; reverse: 5′-GCA TGG AAA CAC ATC ACT GG-3′) and the following PCR conditions: 95° 180 s; 1 × [94° 60 s; 55° 180 s; 72° 90 s]; 3 × [94° 30 s; 60° 60 s; 72° 60 s]; 30 × [94° 60 s; 65° 60 s; 72° 60 s]; 1 × 72° 360 s.
Inhibition of Intracellular Signaling Pathways
Cells were incubated with different pathway inhibitors on day 2 after plating. Medium was changed after 12 h, and EPC-CFUs were counted on days 3 and 6. The following pathway inhibitors were used in previously tested concentrations (29): pertussis toxin (G-protein inhibitor, 400 ng/mL), cholera toxin (G-protein inhibitor, 5 μg/mL), sulindac acid (RAS inhibitor, 50 μM), AFC (RAS-methylation inhibitor, 50 μM), ZM336372 (RAF inhibitor, 1 μM), genistein (PTK inhibitor, 50 μM), H7 (PKA/PKC inhibitor, 100 μM), GF109203X (PKC inhibitor, 5 μM), wortmannin (PI3/Akt inhibitor, 100 nM), U0126 (MEKK inhibitor, 10 μM), iodotubericidin (ERK inhibitor, 20 μM), p38 inhibitor (p38 MAPK inhibitor, 10 nM), PD98059 (p42/p44 MAPK [ERR1/2] inhibitor, 30 μM), and SB 203580 (p38 MAPK/JNK inhibitor, 10 nM). All inhibitors were purchased from Sigma except U0126 and ZM336372, which were from Calbiochem.
Statistical Analysis
Outgrowth of EPCs under different culture conditions was compared by t test and one-way ANOVA. P < 0.05 was considered statistically significant. SPSS 12.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical testing. All data are given as mean ± SD.
RESULTS
Influence of Human Insulin and Analogs on the Outgrowth of EPC-CFU In Vitro
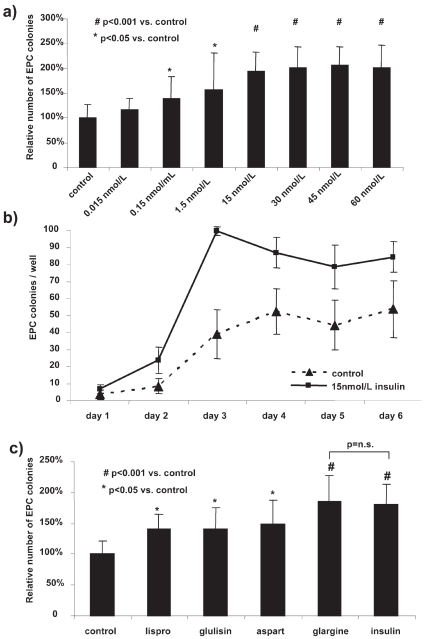
In line with previous publications (1,13), a substantial part of the cells in culture on day 6 (Figure 1a) coexpressed CD34 and VEGF-R2 (Figure 1b), whereas only a few cells expressed the myelomonocytic marker CD115 (Figure 1c) or markers of differentiated endothelial cells (~2% CD146, ~4% CD62E, not shown). Incubation of nonadherent mononuclear cells 2 d after preplating with increasing concentrations of human insulin led to a significant increase in EPC-CFU outgrowth on day 6. The effect of insulin on EPC outgrowth was half-maximal at 1.5 nM and peaked at 15 nM human insulin (100% ± 28% versus 195% ± 39%, P < 0.001, Figure 2a), but did not increase further upon incubation with higher doses (Figure 2a). Most importantly, therapeutic insulin concentrations of 0.15 and 1.5 nM led to an increase in EPC-CFU outgrowth of 139% ± 44% (P = 0.02) and 156% ± 75% (P = 0.02), respectively, compared with untreated controls (100% ± 27%) (Figure 2a).
Figure 2.
a) Dose response of EPC outgrowth upon incubation with human insulin. The dose response was performed with mononuclear cells of three healthy volunteers in triplicate. Cells were incubated with the indicated dose of human insulin for 6 d. Data are shown as relative increase of EPC-CFU outgrowth compared with untreated cells for each healthy volunteer (mean of untreated cells/control taken as 100%). P values given as calculated by t test compared with controls. (b) Time curve of EPC outgrowth upon incubation with 30 nM human insulin. There is a slight artificial decrease in EPC colonies after change of culture medium on day 3. Data are shown as number of EPC colonies of three volunteers in triplicate per culture well. (c) Influence of insulin analogs on EPC outgrowth. Cells were incubated with insulin and the respective analogs (30 nM each). Human insulin and glargine showed the strongest effect on EPC outgrowth. Data are given as relative number of EPC colonies per well of three volunteers in triplicate compared with untreated cells of each volunteer. P values as calculated by t test versus untreated cells.
The time course of EPC outgrowth upon stimulation with 30 nM human insulin showed maximum CFU counts on day 3, suggesting the highest proliferative activity between days 2 and 3 after preplating. This was reflected by a 4.4-fold increase in EPC-CFUs compared with untreated controls (24 ± 8 vs. 100 ± 3, P < 0.001, Figure 2b). The slight decrease in CFUs observed on days 4–6 was most likely artificial and due to the required medium change at day 3 (Figure 2b). To test the potential of equivalent doses of insulin analogs on the proliferation of EPCs, cells were incubated with 30 nM of each insulin analog (Figure 2c). Insulin lispro (141% ± 24%, P = 0.01), glulisin (141% ± 34%, P = 0.02), and aspart (149% ± 39%, P = 0.02) increased EPC outgrowth compared with untreated controls (100% ± 21%). However, only stimulation with 30 nM glargine led to EPC outgrowth (186% ± 41%, P < 0.001) similar to that of human insulin (180% ± 33%, P < 0.001) (Figure 2c). The dose-dependent effect of insulin on EPC outgrowth was observed between 0.15 and 15 nM, reflecting concentrations at which the IR is saturated (22,30). Therefore, we speculated that the effects are not mediated by the IR, and examined alternative receptors and signaling cascades involved in the increased outgrowth of EPCs upon stimulation with human insulin.
Identification of Signaling Cascades
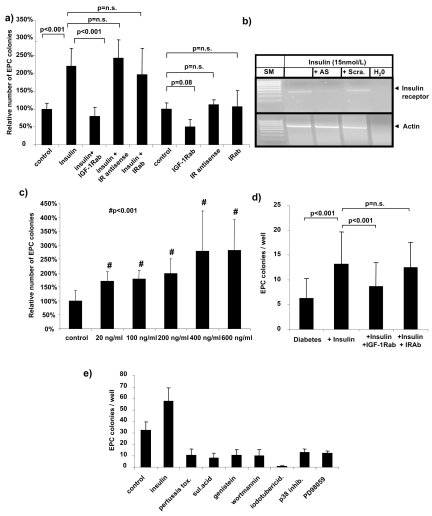
When cells were incubated with 30 nM insulin in the presence of IR antisense oligonucleotides or neutralizing IR antibodies, no significant inhibitory effect on insulin-mediated EPC outgrowth was observed (Figure 3a). Suppression of the IR gene transcription in the silencing experiment was confirmed by RT-PCR for IR mRNA on day 3 (not shown) and day 6 of culture (Figure 3b). Inhibition of the IGF-1 receptor by neutralizing antibodies, however, resulted in complete inhibition of the insulin-dependent enhanced outgrowth of EPCs (Figure 3a). In addition, increasing concentrations of recombinant human IGF-1 enhanced EPC-CFU outgrowth with a half-maximal effect at 20 ng/mL (~3 nM) (Figure 3c).
Figure 3.
(a) Incubation of EPCs with neutralizing IGF-1 receptor antibodies (IGF-1Rab), 0.1 μM IR PTO-antisense oligonucleotides (IR antisense), and IR blocking antibodies (IRab). The stimulatory effect of human insulin was completely blocked by coincubation with IGF-1Rab. Coincubation with IR antisense or neutralizing IR antibodies had no effect on increased EPC outgrowth. Incubation with IGF-1Rab alone led to a decrease of EPC outgrowth, whereas incubation with IR antisense or IRab did not change EPC outgrowth. Data are given as relative number of EPC colonies of three volunteers in triplicate per culture well compared with untreated cells of each volunteer. P values as calculated by ANOVA. (b) Efficiency of IR silencing was shown by RT-PCR. EPCs treated with IR antisense (AS) had markedly suppressed IR mRNA, whereas cells treated with scrambled (Scra) oligonucleotides did not downregulate receptor mRNA. Picture shows representative data of EPCs treated with 30 nM human insulin on day 6 in culture. (c) To show the stimulatory effect of IGF-1 receptor signaling, mononuclear cells of two volunteers were treated with increasing doses of recombinant IGF-1 in the colony-forming assay. Six wells were counted for each volunteer, and data are given as relative EPC outgrowth compared with mean of untreated cells. P values as given by t test compared with controls. (d) Human insulin (30 nM) significantly increased the outgrowth of EPCs from PBMCs of 10 type 2 diabetes patients by ~208%. Addition of neutralizing IGF-1 receptor antibodies blocked the increased formation of EPC colonies, whereas addition of neutralizing IR antibodies had no effect. Data are given as absolute numbers of EPC colonies/well. (e) Identification of kinases involved in the outgrowth of EPCs from PBMCs of two healthy volunteers in triplicate. Data are shown for kinase inhibitors significantly decreasing EPC outgrowth (P < 0.05 by ANOVA) under stimulation with 30 nM insulin.
To prove that IGF-1 receptor–dependent effects of human insulin on the clonogenic potential of circulating EPCs were also relevant in diabetes, PBMCs of 10 type 2 diabetes patients were isolated, cultured, and stimulated with 30 nM insulin in the absence or presence of neutralizing insulin and IGF-1 receptor antibodies. As was observed in healthy volunteers, EPC colony forming from PBMCs of diabetes patients was significantly increased by insulin to ~208% (P < 0.001), and suppressed upon addition of IGF-1 receptor antibodies (13.3 ± 6.4 versus 8.7 ± 4.8 CFU/well, P < 0.001, Figure 3d).
Downstream signaling of the IGF-1 receptor was characterized using different pathway inhibitors. EPC outgrowth was significantly suppressed by pertussis toxin (Gi/o), sulindac acid (RAS), genistein (PTK), wortmannin (PI3), iodotubericidin (ERK), p38 inhibitor, and PD98059 (p42/44) (Figure 3e), suggesting a G-protein–dependent activation of MAP kinases that will be the focus of follow-up studies.
In Vitro Angiogenesis Assay
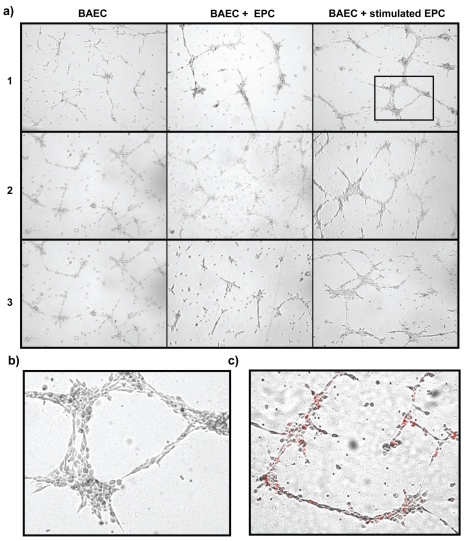
To study the functional relevance of the increase in insulin-dependent outgrowth of EPCs in an in vitro angiogenesis assay, insulin-stimulated EPCs grown from 2 × 106 mononuclear cells were cultured with 105 BAECs. EPCs of healthy volunteers stimulated with 30 nM human insulin led to an increase in tube formation compared with BAECs alone or untreated EPCs (Figure 4a). Most importantly, insulin-stimulated EPCs increased the thickness of tubes resembling vascular-like structures (Figure 4b). Incorporation of insulin-stimulated EPCs into these structures could be tracked using a fluorescent cell tracker (Figure 4c).
Figure 4.
(a) Coincubation of BAECs with EPCs in an in vitro tube formation assay. Data are shown for EPCs of three healthy volunteers. Whereas unstimulated EPCs only marginally increased tube formation (middle column), EPCs incubated with human insulin in the EPC-CFU assay increased tube formation and led to vascular-like structures after 12 h. (b) Digitally enlarged section of the far right picture in volunteer 1. (c) Tracking of insulin-stimulated EPCs with a lipophil fluorescent cell marker (CM-DiI) showed incorporation of EPCs into the vascular-like structures. A representative picture is shown as an overlay image of light and fluorescence microscopy.
DISCUSSION
In this study, human insulin is identified as a factor enhancing the clonogenic potential of circulating EPCs from PBMCs via activation of the IGF-1 receptor. The concentration of insulin needed to observe this effect corresponds to high physiologic serum levels around 0.15 nM (31) and increased at concentrations of ≥1.5 nM, which are present in patients treated with high doses of insulin or analogs (31–33). It seems reasonable that the high concentrations of human insulin studied are needed to elicit this growth effect, because affinity of insulin for its receptor is two to three orders of magnitude higher than for the cognate IGF-1 receptor (30). The efficient silencing of the IR [which has a half life of ~6–12 h (34,35)] through blocking its synthesis by a 3-day antisense knockdown, as well as the lack of an effect of IR-neutralizing antibodies, make involvement of the IR in this novel effect of insulin unlikely. Even a concentration of IR-neutralizing antibodies 10 times higher than suggested by the manufacturer did not influence the observed effects on EPC outgrowth (not shown). In contrast, neutralizing the IGF-1 receptor led to a significant suppression of insulin-stimulated EPC outgrowth and a non-significant inhibition of basal outgrowth in untreated cells. The impact of these considerations is restricted by the fact that the colony-forming assay used in this study is limited by differentiation of progenitor cells in the peripheral mononuclear cell fraction. Hence, although previous studies showed half-maximal effects on tumor cell growth at 4 nM and IGF-1 receptor activation in vitro starting at 0.5 nM (22,25) (concentrations corresponding to the half-maximal effects on insulin-dependent EPC outgrowth in this study), the dose needed to elicit half-maximal effects of insulin in artificial cell systems might be higher.
Involvement of the IR in the insulin-dependent outgrowth of EPCs could be excluded using two different experimental approaches. In addition, glargine, which was shown to have a 6- to 8-fold increased affinity to the IGF-1 receptor in a human osteosarcoma cell line overexpressing this receptor (22), was found to be the only analog inducing EPC outgrowth to a similar extent as human insulin. The maximum effect of insulin on EPC outgrowth in this study was reached at 15 nM. There was no significant induction of EPC proliferation at 0.015 nM insulin, a concentration corresponding to the binding affinity of insulin to its receptor. Recently published data on IGF-1 effects on EPCs are in line with the results presented here showing IGF-1 receptor–dependent effects of IGF-1 in vitro and in vivo (36,37). In conclusion, these considerations, in addition to the missing effects of blocking or silencing the IR, strongly imply an IGF-1 receptor–dependent signaling of human insulin.
The insulin-dependent EPC outgrowth could be blocked by incubation with pertussis toxin and genistein, suggesting a receptor tyrosine kinase–mediated activation of G proteins, which was previously shown in rat fibroblasts and human smooth muscle cells (38,39). This signaling is mediated by Ras and leads to activation of the MAP kinases Erk1/2 and p38 independent of PKC. Consistently, we did not observe significant inhibition of EPC outgrowth by the PKC inhibitor GF109203. Although this observation contradicts previously published data showing inhibitory effects of p38 activation for the outgrowth of EPC (40), there is ample evidence for a distinct role of p38 activation for proliferation of hematopoietic precursors (41–43). A possible explanation for these divergent findings could be the differentiation stages of EPCs studied. A change in the role of p38 activation for proliferation and differentiation of progenitor cells during maturation and upon lineage commitment seems plausible, because inhibition of p38 was shown to enhance proliferation in mature endothelial cells (44–46) and less than 4% of EPCs used in this study expressed markers of differentiated endothelial cells like CD146 or CD62E (not shown).
Yet phosphorylation of p38 and ERK 1/2 in Western blot analysis could not consistently be shown on days 3 and 6 of the outgrowth assay (not shown), which might be a consequence of methodological bias caused by the EPC outgrowth assay itself (i.e., EPC in different states of differentiation), or a rate of kinase phosphorylation that is below the detection threshold of the antibodies used. The exact mechanisms leading to the observed effects of human insulin on EPC outgrowth will therefore be the focus of follow-up studies in suitable cell lines and in vivo models.
Because EPCs take part in vascular regeneration and correlate with markers of endothelial function (1,3,47), we studied the angiogenic function of insulin-stimulated EPC in an in vitro angiogenesis model. In line with our hypothesis, insulin-stimulated cells markedly enhanced tube formation, leading to vascular-like structures in the matrigel assay (Figure 4). It can therefore be speculated that insulin therapy in humans could improve vascular function via stimulation of EPC mobilization, differentiation, and vascular regeneration. Increased mobilization of fetal endothelial progenitor cells by insulin therapy was recently shown in diabetic pregnancy (48). However, in view of the receptor affinities for human insulin, this might only be the case in patients treated with high daily doses of human insulin or glargine, which has a 6-fold increased affinity for the IGF-1 receptor (22). The mechanisms underlying the increased tube formation observed in the matrigel assay remain to be clarified and might partly rely on an increase in paracrine activity of these cells (17).
To overcome limitations due to defective outgrowth and function of EPCs in patients with diabetes (16,17), and because of the limited availability of patient material, we studied the signaling cascades involved in insulin-mediated EPC outgrowth as well as the angiogenic capacity of EPCs mainly in cells isolated from healthy volunteers. Yet we were also able to show an IGF-1 receptor–dependent increase in clonogenic potential of circulating EPCs derived from patients with type 2 diabetes. This is in line with a positive effect of insulin treatment on vascular function previously shown in patients with type 2 diabetes (49,50), although a direct involvement of EPCs in keeping vascular homeostasis in patients has yet to be shown. Specific therapeutic modulation of the IGF-1 receptor–dependent signaling cascades involved in EPC outgrowth offers potential targets for the treatment of vascular late diabetic complications and will be the focus of experimental and clinical follow-up studies.
ACKNOWLEDGMENTS
This study was partly supported by the Deutsche Diabetes Stiftung (PMH), the Manfred Lautenschläger Stiftung (PPN) and the Network Aging Research (NAR) (A.B./P.M.H.). The authors are grateful to Prof. G. Haensch, Institute for Immunology, University of Heidelberg, for support in FACS analysis.
Footnotes
Online address: http://www.molmed.org
REFERENCES
- 1.Hill JM, et al. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600. doi: 10.1056/NEJMoa022287. [DOI] [PubMed] [Google Scholar]
- 2.Werner NT, et al. Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med. 2005;353:999–1007. doi: 10.1056/NEJMoa043814. [DOI] [PubMed] [Google Scholar]
- 3.Asahara T, et al. Isolation of putative progenitor endothelial cells for angiogenesis. Science. 1997;275:964–7. doi: 10.1126/science.275.5302.964. [DOI] [PubMed] [Google Scholar]
- 4.Fathke C, et al. Contribution of bone marrow-derived cells to skin: collagen deposition and wound repair. Stem Cells. 2004;22:812–22. doi: 10.1634/stemcells.22-5-812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Assmus B, et al. Transplantation of Progenitor Cells and Regeneration Enhancement in Acute Myocardial Infarction (TOPCARE-AMI) Circulation. 2002;106:3009–17. doi: 10.1161/01.cir.0000043246.74879.cd. [DOI] [PubMed] [Google Scholar]
- 6.Tateishi-Yuyama E, et al. Therapeutic angiogenesis for patients with limb ischaemia by autologous transplantation of bone-marrow cells: a pilot study and a randomised controlled trial. Lancet. 2002;360:427–35. doi: 10.1016/S0140-6736(02)09670-8. [DOI] [PubMed] [Google Scholar]
- 7.Humpert PM, Eichler H, Lammert A, Hammes HP, Nawroth PP, Bierhaus A. Adult vascular progenitor cells and tissue regeneration in metabolic syndrome. Vasa. 2005;34:73–8. 80. doi: 10.1024/0301-1526.34.2.73. [DOI] [PubMed] [Google Scholar]
- 8.Schatteman GC, Hanlon HD, Jiao C, Dodds SG, Christy BA. Blood-derived angioblasts accelerate blood-flow restoration in diabetic mice. J Clin Invest. 2000;106:571–8. doi: 10.1172/JCI9087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sivan-Loukianova E, Awad OA, Stepanovic V, Bickenbach J, Schatteman GC. CD34+ blood cells accelerate vascularization and healing of diabetic mouse skin wounds. J Vasc Res. 2003;40:368–77. doi: 10.1159/000072701. [DOI] [PubMed] [Google Scholar]
- 10.Stepanovic V, Awad O, Jiao C, Dunnwald M, Schatteman GC. Leprdb diabetic mouse bone marrow cells inhibit skin wound vascularization but promote wound healing. Circ Res. 2003;92:1247–53. doi: 10.1161/01.RES.0000074906.98021.55. [DOI] [PubMed] [Google Scholar]
- 11.Humpert PM, et al. Locally applied mononuclear bone marrow cells restore angiogenesis and promote wound healing in a type 2 diabetic patient. Exp Clin Endocrinol Diabetes. 2005;113:538–40. doi: 10.1055/s-2005-872886. [DOI] [PubMed] [Google Scholar]
- 12.Harraz M, Jiao C, Hanlon HD, Hartley RS, Schatteman GC. CD34− blood-derived human endothelial cell progenitors. Stem Cells. 2001;19:304–12. doi: 10.1634/stemcells.19-4-304. [DOI] [PubMed] [Google Scholar]
- 13.Peichev M, et al. Expression of VEGFR-2 and AC133 by circulating human CD34(+) cells identifies a population of functional endothelial precursors. Blood. 2000;95:952–8. [PubMed] [Google Scholar]
- 14.Rehman J, Li J, Orschell CM, March KL. Peripheral blood “endothelial progenitor cells” are derived from monocyte/macrophages and secrete angiogenic growth factors. Circulation. 2003;107:1164–9. doi: 10.1161/01.cir.0000058702.69484.a0. [DOI] [PubMed] [Google Scholar]
- 15.Ingram DA, Caplice NM, Yoder MC. Unresolved questions, changing definitions, and novel paradigms for defining endothelial progenitor cells. Blood. 2005;106:1525–31. doi: 10.1182/blood-2005-04-1509. [DOI] [PubMed] [Google Scholar]
- 16.Loomans CJ, et al. Endothelial progenitor cell dysfunction: a novel concept in the pathogenesis of vascular complications of type 1 diabetes. Diabetes. 2004;53:195–9. doi: 10.2337/diabetes.53.1.195. [DOI] [PubMed] [Google Scholar]
- 17.Tepper OM, et al. Human endothelial progenitor cells from type II diabetics exhibit impaired proliferation, adhesion, and incorporation into vascular structures. Circulation. 2002;106:2781–6. doi: 10.1161/01.cir.0000039526.42991.93. [DOI] [PubMed] [Google Scholar]
- 18.Humpert PM, et al. SDF-1 genotype influences insulin-dependent mobilization of adult progenitor cells in type 2 diabetes. Diabetes Care. 2005;28:934–6. doi: 10.2337/diacare.28.4.934. [DOI] [PubMed] [Google Scholar]
- 19.Pistrosch F, et al. PPARgamma-agonist rosiglitazone increases number and migratory activity of cultured endothelial progenitor cells. Atherosclerosis. 2005;183:163–7. doi: 10.1016/j.atherosclerosis.2005.03.039. [DOI] [PubMed] [Google Scholar]
- 20.Dimmeler S, et al. HMG-CoA reductase inhibitors (statins) increase endothelial progenitor cells via the PI 3-kinase/Akt pathway. J Clin Invest. 2001;108:391–7. doi: 10.1172/JCI13152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bahlmann FH, de Groot K, Mueller O, Hertel B, Haller H, Fliser D. Stimulation of endothelial progenitor cells: a new putative therapeutic effect of angiotensin II receptor antagonists. Hypertension. 2005;45:526–9. doi: 10.1161/01.HYP.0000159191.98140.89. [DOI] [PubMed] [Google Scholar]
- 22.Kurtzhals P, et al. Correlations of receptor binding and metabolic and mitogenic potencies of insulin analogs designed for clinical use. Diabetes. 2000;49:999–1005. doi: 10.2337/diabetes.49.6.999. [DOI] [PubMed] [Google Scholar]
- 23.Pandini G, Frasca F, Mineo R, Sciacca L, Vigneri R, Belfiore A. Insulin/insulin-like growth factor I hybrid receptors have different biological characteristics depending on the insulin receptor isoform involved. J Biol Chem. 2002;277:39684–95. doi: 10.1074/jbc.M202766200. [DOI] [PubMed] [Google Scholar]
- 24.Nitert MD, Chisalita SI, Olsson K, Bornfeldt KE, Arnqvist HJ. IGF-I/insulin hybrid receptors in human endothelial cells. Mol Cell Endocrinol. 2005;229:31–7. doi: 10.1016/j.mce.2004.10.003. [DOI] [PubMed] [Google Scholar]
- 25.Li G, Barrett EJ, Wang H, Chai W, Liu Z. Insulin at physiological concentrations selectively activates insulin but not insulin-like growth factor I (IGF-I) or insulin/IGF-I hybrid receptors in endothelial cells. Endocrinology. 2005;146:4690–6. doi: 10.1210/en.2005-0505. [DOI] [PubMed] [Google Scholar]
- 26.Ingram DA, et al. Identification of a novel hierarchy of endothelial progenitor cells using human peripheral and umbilical cord blood. Blood. 2004;104:2752–60. doi: 10.1182/blood-2004-04-1396. [DOI] [PubMed] [Google Scholar]
- 27.Pelosi E, et al. Identification of the hemangioblast in postnatal life. Blood. 2002;100:3203–8. doi: 10.1182/blood-2002-05-1511. [DOI] [PubMed] [Google Scholar]
- 28.Bierhaus A, et al. Advanced glycation end product (AGE)-mediated induction of tissue factor in cultured endothelial cells is dependent on RAGE. Circulation. 1997;96:2262–71. doi: 10.1161/01.cir.96.7.2262. [DOI] [PubMed] [Google Scholar]
- 29.Bierhaus A, et al. A mechanism converting psychosocial stress into mononuclear cell activation. Proc Natl Acad Sci U S A. 2003;100:1920–5. doi: 10.1073/pnas.0438019100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kjeldsen T, et al. The ligand specificities of the insulin receptor and the insulin-like growth factor I receptor reside in different regions of a common binding site. Proc Natl Acad Sci U S A. 1991;88:4404–8. doi: 10.1073/pnas.88.10.4404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reaven GM, Bernstein R, Davis B, Olefsky JM. Nonketotic diabetes mellitus: insulin deficiency or insulin resistance? Am J Med. 1976;60:80–8. doi: 10.1016/0002-9343(76)90536-2. [DOI] [PubMed] [Google Scholar]
- 32.Gennaro WD, Van Norman JD. Quantitation of free, total, and antibody-bound insulin in insulin-treated diabetics. Clin Chem. 1975;21:873–9. [PubMed] [Google Scholar]
- 33.Hedman CA, Lindstrom T, Arnqvist HJ. Direct comparison of insulin lispro and aspart shows small differences in plasma insulin profiles after subcutaneous injection in type 1 diabetes. Diabetes Care. 2001;24:1120–1. doi: 10.2337/diacare.24.6.1120. [DOI] [PubMed] [Google Scholar]
- 34.Kasuga M, Kahn CR, Hedo JA, Van Obberghen E, Yamada KM. Insulin-induced receptor loss in cultured human lymphocytes is due to accelerated receptor degradation. Proc Natl Acad Sci U S A. 1981;78:6917–21. doi: 10.1073/pnas.78.11.6917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reed BC, Lane MD. Insulin receptor synthesis and turnover in differentiating 3T3-L1 preadipocytes. Proc Natl Acad Sci U S A. 1980;77:285–9. doi: 10.1073/pnas.77.1.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thum T, et al. Age-dependent impairment of endothelial progenitor cells is corrected by growth-hormone-mediated increase of insulin-like growth-factor-1. Circ Res. 2007;100:434–43. doi: 10.1161/01.RES.0000257912.78915.af. [DOI] [PubMed] [Google Scholar]
- 37.Devin JK, et al. Low-dose growth hormone administration mobilizes endothelial progenitor cells in healthy adults. Growth Horm IGF Res. 2007 Dec 29; doi: 10.1016/j.ghir.2007.11.001. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 38.Kuemmerle JF, Murthy KS. Coupling of the insulin-like growth factor-I receptor tyrosine kinase to Gi2 in human intestinal smooth muscle: Gbetagamma-dependent mitogen-activated protein kinase activation and growth. J Biol Chem. 2001;276:7187–94. doi: 10.1074/jbc.M011145200. [DOI] [PubMed] [Google Scholar]
- 39.Luttrell LM, van Biesen T, Hawes BE, Koch WJ, Touhara K, Lefkowitz RJ. G beta gamma subunits mediate mitogen-activated protein kinase activation by the tyrosine kinase insulin-like growth factor 1 receptor. J Biol Chem. 1995;270:16495–8. doi: 10.1074/jbc.270.28.16495. [DOI] [PubMed] [Google Scholar]
- 40.Seeger FH, et al. p38 mitogen-activated protein kinase downregulates endothelial progenitor cells. Circulation. 2005;111:1184–91. doi: 10.1161/01.CIR.0000157156.85397.A1. [DOI] [PubMed] [Google Scholar]
- 41.Uddin S, Ah-Kang J, Ulaszek J, Mahmud D, Wickrema A. Differentiation stage-specific activation of p38 mitogen-activated protein kinase isoforms in primary human erythroid cells. Proc Natl Acad Sci U S A. 2004;101:147–52. doi: 10.1073/pnas.0307075101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rausch O, Marshall CJ. Cooperation of p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways during granulocyte colony-stimulating factor-induced hemopoietic cell proliferation. J Biol Chem. 1999;274:4096–105. doi: 10.1074/jbc.274.7.4096. [DOI] [PubMed] [Google Scholar]
- 43.Kapur R, Chandra S, Cooper R, McCarthy J, Williams DA. Role of p38 and ERK MAP kinase in proliferation of erythroid progenitors in response to stimulation by soluble and membrane isoforms of stem cell factor. Blood. 2002;100:1287–93. [PubMed] [Google Scholar]
- 44.Matsumoto T, Turesson I, Book M, Gerwins P, Claesson-Welsh L. p38 MAP kinase negatively regulates endothelial cell survival, proliferation, and differentiation in FGF-2-stimulated angiogenesis. J Cell Biol. 2002;156:149–60. doi: 10.1083/jcb.200103096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McGinn S, Saad S, Poronnik P, Pollock CA. High glucose-mediated effects on endothelial cell proliferation occur via p38 MAP kinase. Am J Physiol Endocrinol Metab. 2003;285:E708–17. doi: 10.1152/ajpendo.00572.2002. [DOI] [PubMed] [Google Scholar]
- 46.McMullen ME, Bryant PW, Glembotski CC, Vincent PA, Pumiglia KM. Activation of p38 has opposing effects on the proliferation and migration of endothelial cells. J Biol Chem. 2005;280:20995–1003. doi: 10.1074/jbc.M407060200. [DOI] [PubMed] [Google Scholar]
- 47.Asahara T, et al. Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res. 1999;85:221–8. doi: 10.1161/01.res.85.3.221. [DOI] [PubMed] [Google Scholar]
- 48.Fadini GP, et al. Maternal insulin therapy increases fetal endothelial progenitor cells during diabetic pregnancy. Diabetes Care. 2007 Dec 27; doi: 10.2337/dc07-1996. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 49.Vehkavaara S, Yki-Jarvinen H. 3.5 years of insulin therapy with insulin glargine improves in vivo endothelial function in type 2 diabetes. Arterioscler Thromb Vasc Biol. 2004;24:325–30. doi: 10.1161/01.ATV.0000113817.48983.c5. [DOI] [PubMed] [Google Scholar]
- 50.Rask-Madsen C, et al. Insulin therapy improves insulin-stimulated endothelial function in patients with type 2 diabetes and ischemic heart disease. Diabetes. 2001;50:2611–8. doi: 10.2337/diabetes.50.11.2611. [DOI] [PubMed] [Google Scholar]