Abstract
Purpose
To evaluate clinical features and risks for transformation of conjunctival primary acquired melanosis (PAM) into melanoma.
Methods
Retrospective chart review and Kaplan-Meier estimates of times to PAM enlargement, recurrence, and transformation into melanoma. Main outcome measures: PAM enlargement, recurrence, and transformation into melanoma.
Results
The mean patient age at diagnosis of PAM was 56 years; 62% were female and 96% Caucasian. The conjunctival quadrant(s) affected by PAM and its extent in clock hours were recorded. Initial management included observation in 62%, biopsy combined with cryotherapy in 34%, and other methods in 4%. Of PAM that was observed, Kaplan-Meier estimates at 10 years revealed PAM enlargement in 35% and transformation into melanoma in 12%. Of those that underwent incisional or excisional biopsy, 10-year estimates of PAM recurrence and transformation into melanoma were 58% and 11%, respectively. Progression to melanoma occurred in 0% of PAM without atypia, 0% of PAM with mild atypia, and 13% of PAM with severe atypia. Multivariable analysis revealed that the most significant factor for both PAM recurrence and progression to melanoma was extent of PAM in clock hours.
Conclusion
PAM without atypia or with mild atypia shows 0% progression into melanoma, whereas PAM with severe atypia shows progression into melanoma in 13%. The greater the extent of PAM in clock hours, the greater the risk for transformation into melanoma.
INTRODUCTION
Primary acquired melanosis of the conjunctiva (PAM) is a potentially serious melanocytic lesion that can lead to the development of melanoma.1–29 In a practice of ocular oncology, PAM accounted for 11% of all conjunctival tumors and 21% of melanocytic lesions.2 There has been controversy regarding the terminology, incidence, clinical and histopathologic criteria for diagnosis, frequency of progression to melanoma, and management of PAM.4,8,13,14
It has been estimated that approximately 75% of conjunctival melanomas arise in association with PAM.4,10–12 Most studies regarding PAM have emphasized its relationship to melanoma, and less attention has been given to the clinical features of PAM or clinical factors of PAM that are predictive of progression to melanoma. In this study, an analysis of PAM was performed in a tertiary referral setting to determine demographic features, clinical characteristics, management, and frequency of PAM enlargement, recurrence, and progression to melanoma. Clinical features predictive of PAM transformation to melanoma were assessed.
METHODS
The charts of patients with the diagnosis of PAM on the Ocular Oncology Service of Wills Eye Institute (WEI) were reviewed. Institutional review board approval was obtained for this retrospective study. Patients with PAM only were included in this analysis. Patients with PAM and melanoma at presentation were excluded. PAM was defined clinically as 1 or more patches of acquired asymmetric, flat, discrete, conjunctival and/or corneal brown pigmentation of at least 1 mm in diameter.
We defined PAM histopathologically using a slight modification of the criteria employed in previous reports from the Armed Forces Institute of Pathology (AFIP).7 PAM without atypia was defined as pigmentation of the conjunctival epithelium with or without benign melanocytic hyperplasia. PAM with atypia was characterized by the presence of atypical melanocytic hyperplasia. PAM with mild atypia was defined as atypical melanocytes confined to the basal layer of the epithelium. PAM with severe atypia was defined as atypical melanocytic hyperplasia that extended into the more superficial nonbasal portion of the epithelium in a pagetoid fashion and/or contained epithelioid cells.
Data were collected regarding patient and ocular features, including age at presentation, gender, race, and iris color. Ocular symptoms, tumor laterality, number of lesions per eye, and anatomic and quadrantic location of PAM were determined. The tumor extent was measured in millimeters and by clock hour involvement. The initial tumor management was recorded, and cases that had undergone biopsy were assessed for the presence and degree of cytologic atypia.
Outcomes of PAM were separately evaluated for cases initially managed with observation and those initially managed with incisional or excisional biopsy and cryotherapy. For those cases managed by observation, a series of univariate Cox proportional hazards regressions assessed the degree of relationship of all of the variables to rates of PAM enlargement and progression into melanoma. For cases that underwent biopsy, a series of univariate Cox proportional hazards regressions assessed the degree of relationship of all of the variables to rates of PAM recurrence and progression to melanoma. All of the variables were analyzed as discrete variables except for patient age at presentation, PAM basal dimension in millimeters, and number of clock hours of PAM, which were evaluated as continuous variables. Subsequent multivariate models included variables that were significant on a univariate level (P < .05) to identify the combination of factors best related to the outcomes. Kaplan-Meier survival estimates calculated for the observed group included time to PAM enlargement and time to melanoma development. Kaplan-Meier survival estimates calculated for the biopsied group included time to PAM recurrence and time to melanoma development.
RESULTS
There were 311 eyes with PAM included in this analysis. Patient demographic data are shown in Table 1. The mean patient age at diagnosis was 56 years (range, 15–90 years), 62% were female, 96% were Caucasian, and 58% had brown irides. The clinical features of PAM are shown in Table 2. The quadrant(s) of the conjunctiva affected were temporal (57%), inferior (45%), nasal (42%), and superior (37%). The anatomic location was bulbar conjunctiva (91%), limbal conjunctiva (55%), cornea (23%), forniceal conjunctiva (13%), palpebral conjunctiva (12%), and caruncle (11%). PAM involved a mean of 3 clock hours of conjunctiva (range, up to 12 clock hours).
TABLE 1.
CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) IN 311 EYES OF 276 PATIENTS: DEMOGRAPHIC FEATURES*
| FEATURE | ALL PATIENTS N = 276 PATIENTS, 311 EYES | PAM OBSERVED n = 165 PATIENTS, 194 EYES | PAM BIOPSIED n = 107 PATIENTS, 107 EYES |
|---|---|---|---|
| Age, yr | |||
| mean [median, range] | 56 [56, 15–90] | 55 [56, 16–90] | 56 [57, 15–89] |
| Gender | |||
| Male | 105 (38%) | 73 (44%) | 30 (28%) |
| Female | 171 (62%) | 92 (56%) | 77 (72%) |
| Race | |||
| Caucasian | 265 (96%) | 163 (99%) | 97 (91%) |
| African American | 4 ( 1%) | 1 (<1%) | 4 (4%) |
| Hispanic | 6 ( 2%) | 0 ( 0%) | 6 (6%) |
| Asian | 1 (<1%) | 1 (<1%) | 0 (0%) |
| Laterality | |||
| Unilateral | 241 (87%) | 130 (79%) | 102 (95%) |
| Bilateral | 35 (13%) | 35 (21%) | 5 (5%) |
| Eye color | |||
| Brown | 181 (58%) | 118 (61%) | 60 (56%) |
| Blue | 110 (35%) | 62 (32%) | 43 (40%) |
| Green | 16 ( 5%) | 10 ( 5%) | 4 (4%) |
| Unknown | 4 ( 1%) | 4 ( 2%) | 0 (0%) |
Ten eyes were treated by methods other than excision (topical chemotherapy or cryotherapy alone) and are not included in the calculations for this table. Therefore the total number of eyes for the observed group and the excised group was 301 (194+107).
TABLE 2.
CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) IN 311 EYES: TUMOR CHARACTERISTICS AT INITIAL EXAMINATION
| TUMOR FEATURES | ALL EYES N = 311 EYES | PAM OBSERVED n = 194 EYES | PAM BIOPSIED n = 107 EYES |
|---|---|---|---|
| Symptoms | |||
| None | 170 (55%) | 129 (66%) | 36 (34%) |
| Spot | 138 (44%) | 64 (33%) | 70 (65%) |
| Stable | 89 (29%) | 46 (24%) | 42 (39%) |
| Growing | 49 (16%) | 18 (9%) | 28 (26%) |
| Redness | 3 (1%) | 1 (<1%) | 1 (1%) |
| No. of lesions per eye | |||
| mean [median, range] | 2 [1,1–7] | 2 [1, 1–7] | 2 [1, 1–7] |
| Quadrantic location* | |||
| Superior | 116 (37%) | 69 (36%) | 42 (39%) |
| Temporal | 178 (57%) | 108 (56%) | 64 (60%) |
| Inferior | 139 (45%) | 80 (41%) | 52 (49%) |
| Nasal | 131 (42%) | 79 (41%) | 47 (44%) |
| Conjunctival anatomic location* | |||
| Cornea | 70 (23%) | 25 (13%) | 42 (39%) |
| Limbal conjunctiva | 172 (55%) | 94 (48%) | 70 (65%) |
| Bulbar conjunctiva | 284 (91%) | 180 (93%) | 96 (90%) |
| Forniceal conjunctiva | 39 (13%) | 13 (7%) | 23 (21%) |
| Palpebral conjunctiva | 35 (12%) | 10 (5%) | 21 (20%) |
| Caruncle | 34 (11%) | 17 (9%) | 16 (15%) |
| Extent of PAM (No. of clock hours) | |||
| mean [median, range] | 3 [2,1–12] | 2 [2, 1–12] | 3 [3, 1–12] |
| Extent of PAM | |||
| Focal (≤3 clock hours) | 238 (76%) | 166 (86%) | 67 (63%) |
| Diffuse (>3 clock hours) | 70 (23%) | 25 (13%) | 40 (37%) |
| Unknown | 3 (1%) | 3 (1%) | 0 (0%) |
| Size of largest PAM, mm | |||
| mean [median, range] | 8 [5,1–36] | 6 [4, 1–36] | 11 [8, 1–35] |
Totals are greater than 100% because in some eyes more than 1 quadrant or radial location of conjunctiva was involved by PAM.
Initial PAM management is listed in Table 3. Of the 311 affected eyes, initial management was observation in 194 (62%), incisional or excisional biopsy combined with cryotherapy in 107 (34%), and topical chemotherapy and/or cryotherapy without biopsy in 6 (3%). Eyes managed with observation showed smaller PAM size (median, 4 mm) as compared to eyes managed with biopsy and cryotherapy (median, 8 mm) (Table 2).
TABLE 3.
INITIAL MANAGEMENT OF CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) IN 311 EYES
| INITIAL MANAGEMENT | ALL EYES N = 311 EYES | PAM OBSERVED n = 194 EYES | PAM BIOPSIED n = 107 EYES |
|---|---|---|---|
| Observation | 194 (62%) | 194 (100%) | … |
| Incisional/excisional biopsy | 107 (34%) | … | 107 (100%) |
| Mitomycin C only | 4 ( 1%) | … | … |
| Cryotherapy only | 1 (<1%) | … | … |
| Mitomycin C and cryotherapy | 1 (<1%) | … | … |
| No information | 4 ( 1%) | … | … |
In our series, Kaplan-Meier estimates at 10 and 15 years for progression to melanoma in the initially observed group were 12% and 21%, whereas in the initially biopsied group the estimates were 11% and 11% (Table 8). The only multivariable factor predictive of progression to melanoma in the observed group was extent of PAM in clock hours (P < .0001) (Table 9). There were no factors on the multivariable level predictive of melanoma development in the biopsied group, but the most important factor predictive of PAM recurrence in this group was extent of PAM in clock hours (P < .0001) (Table 10).
Of those eyes managed with observation and with at least 3-year follow-up, PAM enlargement was detected in 16% and progression to melanoma in 5%. The mean interval to melanoma development was 56 months (Table 4). Of those eyes managed with biopsy and cryotherapy and with at least 3 years follow-up, PAM recurrence was detected in 27% and progression to melanoma in 3%. The mean interval to melanoma development was 39 months (Table 5).
TABLE 4.
ENLARGEMENT WITH AND WITHOUT DEVELOPMENT OF MELANOMA IN 131 EYES WITH CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) IN WHICH PAM WAS INITIALLY OBSERVED WITH FOLLOW-UP OF AT LEAST 3 YEARS
| TUMOR OUTCOME | PAM OBSERVED WITH ≥3-YEAR FOLLOW- UP n = 131 EYES |
|---|---|
| PAM enlargement | |
| Without development of melanoma | 21 (16%) |
| With development of melanoma | 6 (5%) |
| Time* to PAM enlargement without development of melanoma, mo | 32 [25, 3–126] |
| mean [median, range] | |
| Time* to PAM enlargement with development melanoma, mo | 56 [47, 25–126] |
| mean [median, range] | |
Time from date of first visit on the Ocular Oncology Service, Wills Eye Institute.
TABLE 5.
RECURRENCE AND PROGRESSION TO MELANOMA IN 98 EYES WITH CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) IN WHICH PAM WAS INITIALLY MANAGED WITH EXCISION AND CRYOTHERAPY WITH FOLLOW-UP OF AT LEAST 3 YEARS
| TUMOR OUTCOME | PAM BIOPSIED WITH ≥3-YEAR FOLLOW- UP n = 98 eyes |
|---|---|
| PAM recurrence | |
| Without development of melanoma | 26 (27%) |
| With development of melanoma | 3 ( 3%) |
| Time* to PAM recurrence without development of melanoma, mo | 19 [15, 2–70] |
| mean [median, range] | |
| Time* to PAM recurrence with development melanoma, mo | 39 [41, 13–62] |
| mean [median, range] | |
Time from date of first visit on the Ocular Oncology Service, Wills Eye Institute.
Of the 112 eyes with biopsy (initial or follow-up) and histopathologic assessment of PAM with at least 3 years of follow-up, PAM recurrence was found in 11% of those without atypia, 26% with mild atypia, and 50% with severe atypia. None of the cases in the biopsied group with no cytologic atypia or mild atypia progressed to melanoma. In contrast, progression to melanoma occurred in 13% of those with PAM with severe atypia (Table 6). A comparison of the findings from the AFIP4,7,8 with our results from WEI is shown in Table 7. In biopsied eyes with cytologic atypia, overall progression was remarkably lower in the WEI series as compared to the AFIP series.
TABLE 6.
OUTCOME ACCORDING TO DEGREE OF ATYPIA IN 112 EYES WITH CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) THAT ULTIMATELY WERE MANAGED WITH EXCISION AND CRYOTHERAPY WITH FOLLOW-UP OF AT LEAST 3 YEARS
| GRADE OF ATYPIA | OUTCOME | ||
|---|---|---|---|
| NO PAM RECURRENCE (n = 80 EYES) | PAM RECURRENCE WITHOUT DEVELOPMENT OF MELANOMA (n = 29 EYES) | PAM RECURRENCE WITH DEVELOPMENT OF MELANOMA (n = 3 EYES) | |
| None (n = 44) | 39 (89%) | 5 (11%) | 0 (0%) |
| Mild (n = 44) | 32 (73%) | 12 (26%) | 0 (0%) |
| Severe (n = 24) | 9 (38%) | 12 (50%) | 3 (13%) |
TABLE 7.
COMPARISON OF THE RATE OF PROGRESSION OF CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) TO MELANOMA IN THE ARMED FORCES INSTITUTE OF PATHOLOGY (AFIP) SERIES AND THE WILLS EYE INSTITUTE (WEI) SERIES
| DEVELOPMENT OF MELANOMA | AFIP4,7,8 n = 41 eyes | WEI (current series) n = 233 eyes |
|---|---|---|
| Inclusive all cases with and without biopsy | NA | n = 233 |
| Progression to melanoma | NA | 4% |
| Inclusive cases with biopsy | n = 41 | n = 112 |
| Overall progression to melanoma | 32% | 3% |
| If no atypia | 0% | 0% |
| If any atypia (overall) | 46% | 3% |
| If mild atypia | NA | 0% |
| If severe atypia | 75%–90% | 13% |
NA, not addressed.
In our series, Kaplan-Meier estimates at 10 and 15 years for progression to melanoma in the initially observed group were 12% and 21%, whereas in the initially biopsied group the estimates were 11% and 11% (Table 8). The only multivariable factor predictive of progression to melanoma in the observed group was extent of PAM in clock hours (P < .0001) (Table 9). There were no factors on the multivariable level predictive of melanoma development in the biopsied group, but the most important factor predictive of PAM recurrence in this group was extent of PAM in clock hours (P < .0001) (Table 10).
TABLE 8.
SUMMARY OF OUTCOMES IN 311 EYES WITH CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) USING KAPLAN-MEIER ESTIMATES
| KAPLAN-MEIER ESTIMATES | ||||
|---|---|---|---|---|
| OUTCOMES | 2 yr | 5 yr | 10 yr | 15 yr |
| Initially observed group (n = 194 eyes) | ||||
| PAM enlargement without development of melanoma | 9% | 26% | 35% | 43% |
| PAM enlargement with development of melanoma | 0 | 8% | 12% | 21% |
| Initially biopsied group (n = 107 eyes) | ||||
| PAM recurrence without development of melanoma | 38% | 52% | 58% | 58% |
| PAM recurrence with development of melanoma | 2% | 5% | 11% | 11% |
TABLE 9.
FACTORS PREDICTIVE OF CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) PAM ENLARGEMENT WITH AND WITHOUT DEVELOPMENT OF MELANOMA IN INITIALLY OBSERVED GROUP (N = 194) USING MULTIVARIABLE ANALYSIS
| MULTIVARIABLE ANALYSIS | P VALUE | RR | 95% CI |
|---|---|---|---|
| PAM enlargement without development of melanoma (n = 21) | |||
| Previous excision elsewhere (present vs absent*) | .001 | 5.63 | 1.20–15.87 |
| PAM enlargement with development of melanoma (n = 6) | |||
| Extent of PAM (No. of clock hours) | <.0001 | 1.70† | 1.29–2.23 |
CI, confidence interval; RR, relative risk.
Reference variable.
Per 1-hour increase.
TABLE 10.
FACTORS PREDICTIVE OF CONJUNCTIVAL PRIMARY ACQUIRED MELANOSIS (PAM) ENLARGEMENT WITH AND WITHOUT DEVELOPMENT OF MELANOMA IN INITIALLY BIOPSIED GROUP (N = 107) USING MULTIVARIABLE ANALYSIS
| MULTIVARIABLE ANALYSIS | P VALUE | RR | 95% CI |
|---|---|---|---|
| PAM recurrence without development of melanoma (n = 26) | |||
| PAM involvement of caruncle (present vs absent*) | .006 | 3.53 | 1.44–8,68 |
| Extent of PAM (No. of clock hours) | <.0001 | 1.43† | 1.22–1.69 |
| PAM recurrence with development of melanoma (n = 3) | |||
| No significant variables | … | … | … |
CI, confidence interval; RR, relative risk.
Reference variables.
Per 1-hour increase.
There were no variables significant on the multivariable level. The only significant univariable factor was the presence of skin cancer (P = .013, RR = 34.70, 95% CI, 2.14–563.67).
DISCUSSION
Primary acquired melanosis of the conjunctiva has been the subject of changing concepts and controversy with regard to demographics, terminology, clinical definition, histopathologic definition, incidence, natural course, and management.1–29 This study was designed to address some of these issues.
Concerning demographics, PAM is mainly a condition of adult Caucasians, with a median age at diagnosis of 56 years (Table 1). However, in this series, classic PAM was seen in patients as young as 15 years of age. We have no explanation for the slight preponderance of females (62%). PAM does not occur exclusively in Caucasians. Of our 276 patients, 4% were non-Caucasian. In dark-skinned individuals, PAM must be differentiated from racial melanosis, which is usually bilateral and symmetrical.1 We have treated several African American patients who presented with aggressive conjunctival melanoma that had clearly arisen from PAM (unpublished observations). PAM is generally considered to be a unilateral disease. The finding that 13% of cases in this series were bilateral could partly be related to the fact that patients underwent a meticulous examination of both eyes, and small foci of PAM in the fellow eye were detected, recorded, and coded.
The terminology related to PAM has been controversial. Historically, Reese5 called the condition precancerous melanosis. Zimmerman6 objected to that term, since many cases had benign clinical and histopathologic features. He called it acquired melanosis and divided it into stage I (benign acquired melanosis) and stage II (cancerous acquired melanosis). The World Health Organization subsequently adopted the term primary acquired melanosis (PAM).4,7 Folberg and associates4,8–12 used that term in several publications and established histopathologic criteria to predict which cases are more likely to progress to melanoma. Ackerman,13 a dermatopathologist, has challenged this terminology and believes that PAM should be called melanoma-in-situ, similar to lentigo maligna of the skin. The term melanoma-in-situ could possibly apply to PAM with severe atypia, which comprises 21% of biopsied lesions (Table 6) and 8% of all cases of PAM seen in a clinical practice (Tables 1 and 6), but certainly not to all cases of PAM. We believe that the term melanoma-in-situ could unnecessarily alarm both clinicians and patients, particularly since many PAM lesions have little propensity to evolve into melanoma. The term PAM seems acceptable, since the condition is primary, acquired, and generally pigmented.
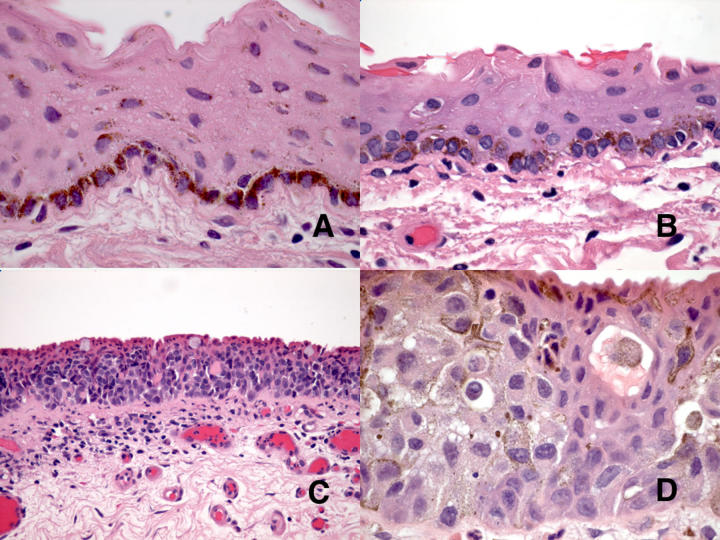
To date, there has not been a clear clinical definition of PAM. In this study, we chose to be inclusive and define PAM clinically as any acquired flat, noncystic pigmented lesion of the conjunctiva, cornea, or caruncle (Figures 1 through 4) that lacks the typical features of localized nevus or racial melanosis.1 Although the differentiation of these 2 conditions from PAM is straightforward in most instances, there are occasional cases where this distinction is challenging both clinically and histopathologically. The histopathologic definition of PAM is provided in the “Methods” section and is derived from the AFIP definitions.7–12 In some instances it may be extremely difficult to determine histopathologically if low-grade melanocytic hyperplasia is present or whether conjunctival pigmentation reflects melanin pigment within squamous epithelial cells. Immunohistochemical stains for melanocytic and epithelial markers can help to make this distinction in challenging cases. On the other hand, the results of this study suggest that this distinction actually is of little significance clinically because neither PAM without atypia nor PAM with mild atypia progresses to melanoma.
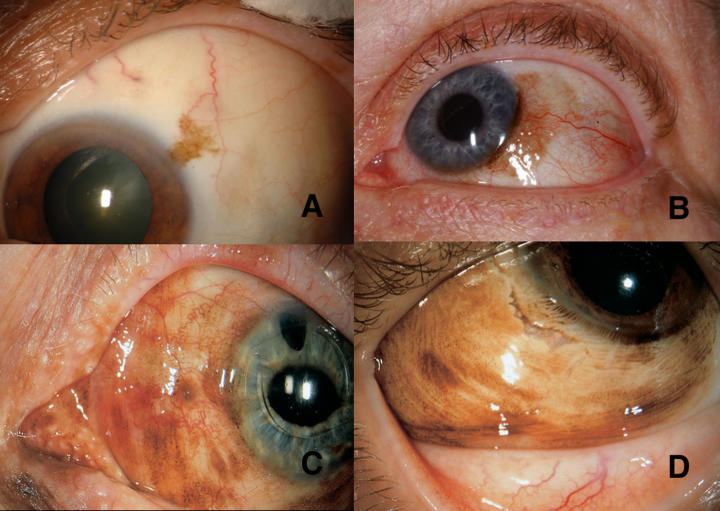
FIGURE 1.
Primary acquired melanosis (PAM) with varying extent of involvement. A, PAM involving less than 1 clock hour of bulbar conjunctiva. B, PAM involving 4 clock hours of conjunctiva with slight corneal extension. C, PAM involving more than 6 clock hours of bulbar conjunctiva with extension into the cornea. D, PAM involving entire bulbar conjunctiva (12 clock hours).
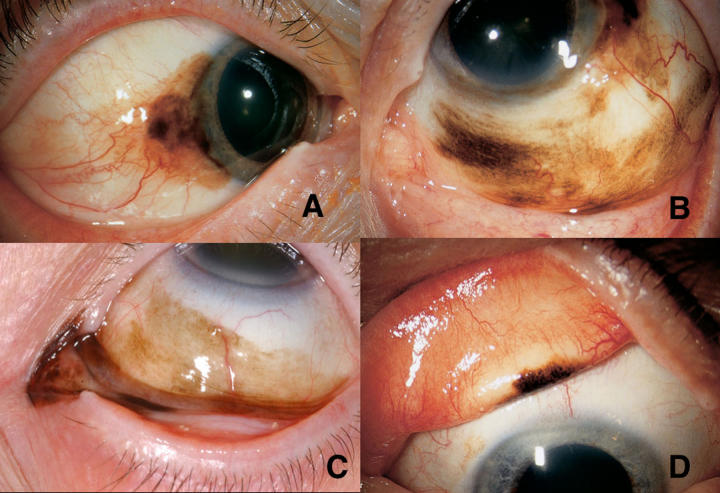
FIGURE 4.
Transformation of primary acquired melanosis (PAM) into melanoma. A, At initial presentation, flat PAM was detected on the bulbar and forniceal conjunctiva. The lesion was removed and cryotherapy performed. It proved to be PAM with atypia. B, The patient did not return for follow-up, and 5 years later a large conjunctival melanoma invading into the caruncle, orbit, and eyelids was found and managed by complete surgical excision, canthoplasty, and postexcision cyberknife radiotherapy. C, PAM with early transformation into melanoma. The elevated darker areas suggest foci of evolving melanoma. D, PAM giving rise to nodule of amelanotic melanoma. The melanoma that arises from pigmented PAM is often nonpigmented clinically.
The reported incidence of PAM varies greatly in different clinical settings. Motivated by the AFIP reports that recommended biopsy for most cases, Gloor and Alexandrakis14 attempted to establish the true incidence by screening all Caucasian patients over age 10 years who were referred to a cornea clinic for unrelated conditions. Using minimally stringent criteria for diagnosis, they concluded that PAM was present in 36% of adult Caucasians. They emphasized that many PAM lesions were small and did not require surgical biopsy, since the vast majority were not destined to transform into melanoma. In a report of 1643 conjunctival lesions from an ocular oncology practice, PAM comprised 11% of all conjunctival tumors and pseudotumors and 21% of pigmented conjunctival lesions.2 Nevus and melanoma were more common than PAM, reflecting referral bias for these more obvious and more suspicious conditions. Based on our experience and review of the literature, we believe the incidence of PAM actually is much higher than generally believed, because many lesions that meet the diagnostic criteria for PAM never come to clinical attention and may even be ignored by the patient and the physician.
The clinical features of PAM were elucidated in this study (Table 2). Most patients were asymptomatic or noticed only the patch of pigment. The extent of PAM was 3 clock hours or less in 76% and more than 3 clock hours in 23%. Corneal involvement with PAM was noted in 23%. The extent of PAM is best determined by making large detailed drawings during meticulous preoperative slit-lamp examination. Careful preoperative assessment is important because the precise extent of PAM is often less obvious in photographs or during intraoperative examination with the operating microscope. Accurate information concerning the extent of the lesion is critical in planning therapeutic strategies.
The natural course of PAM with regard to progression, recurrence, and evolution to melanoma has not been previously elucidated. In the frequently cited histopathologic series from the AFIP, the investigators reported that 32% of 41 eyes with PAM progressed to melanoma. If the PAM showed microscopic evidence of atypia, progression to melanoma occurred in 46%, but if there was no atypia, the chances were nil.8–11 The study included mainly cases that were referred to the AFIP for histopathologic diagnosis. Hence, they generally were larger lesions with more bothersome histopathologic features. The investigators concluded that biopsy or removal of all PAM lesions was warranted. However, that study did not include potential cases in the general population that were not subjected to biopsy.
Neither the studies of Folberg and associates7–11 nor the study of Gloor and Alexandrakis14 addressed the natural course of PAM following the initial clinical diagnosis. In this study, we attempted to address that question. All patients in our series had a lesion that appeared sufficiently suspicious to the referring ophthalmologist to prompt consultation at our ocular oncology center. Hence, this study presumably provides a somewhat more reliable estimate of the true risk of the progression of PAM to melanoma. However, this study also has selection bias, because lesions that are more suspicious clinically are more likely to be directed to a tertiary referral center.
The majority of PAM lesions in this series were small, allowing for observation (62%), and only 21% of these observed lesions showed enlargement during the course of follow-up (Tables 3 and 4). Hence, it appears that many small, bland lesions can cautiously be followed and are likely to remain stable and require no treatment.
Of the larger lesions that were managed by initial biopsy and cryotherapy (Table 5), 27% recurred and 3% eventually evolved to melanoma. The mean interval from initial surgery to recurrence was 19 months, and the mean interval to development of melanoma was 39 months. The latter observations stress the need for periodic long-term follow-up of all patients who have had observation or excision of PAM, particularly if histopathologic studies reveal atypia.
Some differences were found in the AFIP series and the WEI series with regard to PAM progression to melanoma (Table 7). In the WEI series that included all cases (observed and biopsied), the incidence of progression to melanoma was 4%. In comparing only cases with available histopathology, overall progression to melanoma was 32% in the AFIP series and 3% in the WEI series. Both studies found no progression to melanoma if there was no cytologic atypia.
With regard to the assessment of the effect of the degree of cellular atypia and progression to melanoma, the current WEI series attempted to use the same criteria for atypia and severe atypia that were used in the AFIP series. The lower incidence of progression to melanoma in the WEI series probably reflects a variety of factors, including the probable referral of cases with more severe histopathologic features to the AFIP in contradistinction to cases with no atypia or mild atypia. Furthermore, patients in the WEI clinical series were followed up periodically by the same group of experienced ocular oncologists, and residual or recurrent PAM was treated promptly before it progressed to a more advanced stage.
In the WEI series, Kaplan-Meier estimates showed that the rate of PAM enlargement in the initially observed group was 26% at 5 years, 35% at 10 years, and 43% at 15 years. The estimates for evolution into melanoma were 8% at 5 years, 12% at 10 years, and 21% at 15 years (Table 8). These findings show the slow but potentially malignant progression of PAM. In the initially biopsied group, Kaplan-Meier estimates showed that the rate of PAM recurrence was 52% at 5 years and 58% at 10 and 15 years, and the rate of melanoma development was 5% at 5 years and 11% at 10 and 15 years. Despite apparent resolution of PAM on clinical inspection after meticulous treatment by excisional or incisional biopsy followed by cryotherapy, patients should be followed closely, because PAM recurrence with melanoma development can pose a serious threat.
The greater the extent of PAM on the surface of the globe, the greater the risk for PAM recurrence following biopsy and the greater the risk for melanoma (RR 1.70) development (Tables 9 and 10). For example, in patients who were observed, PAM involving 4 clock hours carried a 6.8 times greater risk for melanoma development than PAM of only 1 clock hour. If PAM involved 12 clock hours, the risk for melanoma development was 20.4 times greater than with a 1-clock-hour lesion.
Our philosophy for PAM management is based on long-term clinical experience and the results of this study. All patients with PAM (or any conjunctival tumor) should have a large detailed drawing performed in the office using slit-lamp biomicroscopy. The surgical plan is made on the basis of this drawing. If PAM is confined to the bulbar conjunctiva and is less than 1 clock hour in extent, we generally recommend observation once or twice a year unless the patient requests excision. In this analysis, 62% of cases were managed with observation, the majority of which were small lesions (Tables 3 and 4). If PAM is 1 to 2 clock hours in extent, the patient is counseled and offered the options of observation or treatment with the advice that excision is probably preferable. If the lesion is greater than 2 clock hours in extent, we generally recommend complete surgical excision and cryotherapy for those up to 5 clock hours and wide incisional biopsy plus cryotherapy for larger lesions.
For more diffuse PAM, our approach is to perform small conjunctival map biopsies in each quadrant and double freeze thaw cryotherapy to all remaining areas of pigment.1,18–20 When extensive conjunctival tissue is removed and primary closure is difficult, amniotic membrane or buccal mucosal graft is employed.25,26 Corneal PAM is managed with either alcohol epitheliectomy or topical mitomycin C. Depending on subsequent clinical and histopathologic findings, supplemental treatment for residual or recurrent PAM might include in-office cryotherapy or topical chemotherapy using mitomycin C.20–22 Plaque brachytherapy can be used in selected instances.1
In conclusion, PAM appears to be more common than generally believed. Small foci of PAM (<1 clock hour) generally remain stable, but larger lesions carry greater potential for evolution into invasive melanoma. PAM without atypia and PAM with mild atypia carry almost no risk for progression into melanoma, whereas PAM with severe atypia shows 13% transformation to melanoma. Cautious, long-term follow-up is advised for all patients with PAM.
PEER DISCUSSION
DR HANS E. GROSSNIKLAUS
In this study, Dr. Jerry Shields and coauthors evaluated their extensive experience in 311 eyes of 276 patients with a clinical diagnosis of primary acquired melanosis (PAM). The most significant clinical risk factor for progression was size in clock hours, with a 1.7 relative risk for enlargement per clock hour of conjunctival involvement. The authors provide practical treatment recommendations based on number of clock hours involved. In a purely clinical study, Gloor and Alexandrakis1 found PAM in 36% of adult Caucasians. In a partly clinical and partly pathologic study, Dr Carol Shields and coworkers2 found that PAM accounted for 11% of all conjunctival tumors and 21% of all melanocytic conjunctival tumors. In a purely pathologic study, PAM accounted for 6.6% of pigmented conjunctival lesions.3 Therefore, even though PAM is fairly common, it is likely clinically overdiagnosed, as secondary melanosis and other lesions may clinically mimic PAM. Additionally, it is clinically impossible to distinguish between PAM without and PAM with atypia.
Of the 311 eyes in this series, 107 (34.4%) underwent biopsy as part of the initial management and 112 (36%) were ultimately biopsied. Of those 112 cases, 44 (39.3%) were histologically diagnosed as PAM without atypia, 44 (39.3%) as PAM with mild atypia, and 24 (21.4%) as PAM with severe atypia. Recurrence rates were 11%, 26%, and 50%, respectively, among those 3 groups, and melanoma developed in only 3 patients (13%), all of whom had PAM with severe atypia. Whereas the current series estimated a 13% progression of PAM to melanoma, the AFIP purely pathology series found a 32% progression of any type of PAM to melanoma.4,5 This discrepancy is likely due to clinically overdiagnosed PAM, the referral nature of the AFIP series, and other factors. Importantly, both the current study and the AFIP series demonstrate that there are pathologic risk factors, such as degree of atypia, that correspond to disease progression. This has recently been shown by another group.6
There has been some controversy regarding the nomenclature of PAM. Some have advocated for the term melanoma-in-situ. Shields and coauthors believe that the term melanoma-in-situ may unnecessarily alarm clinicians and patients. I agree that PAM is the best term for this condition,7 especially since ophthalmologists understand the implications of this diagnosis. Shields and coauthors use mild and severe atypia in their histopathologic classification scheme for PAM, yet there is no moderate category, as proposed by others.8 This study found that clinical size in clock hours correlated with disease progression. Did the authors evaluate for nodularity, thickening, or change in color? The authors advocate for map biopsies for diffuse PAM (>5 clock hours). In some instances, it is quite difficult to discern the extent of the PAM at the slit lamp. Are there any clinical clues that may help distinguish the extent of nonpigmented PAM, the so-called PAM sine pigmento9? The authors used topical mitomycin C in some instances. This should be used judiciously and only by experienced ophthalmic oncologists for PAM, as the PAM may become depigmented after treatment, thus masking underlying invasive melanoma. I wish to congratulate the authors on their extensive work and for bringing this important topic to our attention.
ACKNOWLEDGMENTS
Funding/Support: None.
Financial Disclosures: None.
REFERENCES
- 1.Gloor P, Alexandrakis G. Clinical characterization of primary acquired melanosis. Invest Ophthalmol Vis Sci. 1995;36:1721–1729. [PubMed] [Google Scholar]
- 2.Shields CL, Demirci H, Karatza E, Shields JA. Clinical survey of 1643 melanocytic and non-melanocytic tumors of the conjunctiva. Ophthalmology. 2004;111:1747–1754. doi: 10.1016/j.ophtha.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Grossniklaus HE, Green WR, Luckenbach M, Chan CC. Conjunctival lesions in adults. A clinical and histopathologic review. Cornea. 1987;6:78–116. doi: 10.1097/00003226-198706020-00002. [DOI] [PubMed] [Google Scholar]
- 4.Folberg R, McLean IW, Zimmerman LE. Primary acquired melanosis of the conjunctiva. Hum Pathol. 1985;16:129–135. doi: 10.1016/s0046-8177(85)80061-7. [DOI] [PubMed] [Google Scholar]
- 5.Folberg R, McLean IW. Primary acquired melanosis and melanoma of the conjunctiva: terminology, classification and biologic behavior. Hum Pathol. 1986;17:652–654. doi: 10.1016/s0046-8177(86)80175-7. [DOI] [PubMed] [Google Scholar]
- 6.Sugiura M, Colby KA, Mihm MC, Jr, Zembowicz A. Low-risk and high-risk histologic features in conjunctival primary acquired melanosis with atypia: clinicopathologic analysis of 29 cases. Am J Surg Pathol. 1997;31:185–192. doi: 10.1097/01.pas.0000213339.32734.64. [DOI] [PubMed] [Google Scholar]
- 7.Grossniklaus HE. Primary acquired melanosis of the conjunctiva is not melanoma-in-situ. Mod Pathol. 1992;5:473. [PubMed] [Google Scholar]
- 8.McLean IW, Burnier MN, Zimmerman LE, Jakobiec FA. Tumors of the Eye and Ocular Adnexa. Washington, DC: Armed Forces Institute of Pathology; 1994. Chapter 3. Tumors of the conjunctiva. AFIP Fasicle 12. [Google Scholar]
- 9.Griffith WR, Green WR, Weinstein GW. Conjunctival malignant melanoma originating in acquired melanosis sine pigmento. Am J Ophthalmol. 1971;72:595–599. doi: 10.1016/0002-9394(71)90857-9. [DOI] [PubMed] [Google Scholar]
DR. ALLAN J. FLACH
No conflicts. When you chose your suspicious lesions and performed biopsies of them, was there any change in growth or behavior after those biopsies? How did you select which ones were suspicious, and not more likely malignant, without the results of your present study?
DR. JOSE S. PULIDO
No conflict of interest. I really would like to thank both Dr. Shields for their wonderful presentation and their ability to bring forward clinical science. They both gave presentations that showed important valid interest to clinicians. My question for Dr. Shields relates to the patients who had the progressive enlargement in association with prior biopsy. What did the biopsy show? Was there a relationship between having had the biopsy and being referred? Was there a confounding effect from that?
DR. BALAMURALI AMBATI
What is the role of interferon alpha 2, mitomycin-C (MMC), and 5-fluourouracil (5-FU) for intralesional or topical chemotherapeutic of PAM or melanoma either as single agent applications or given in combination?
DR. JERRY A. SHIELDS
I would like to thank everyone for their comments. They are all very constructive. First, with regard to Dr. Grossniklaus and his point about the possible over-diagnosis of PAM based on the clinical features. In our series we adhered strictly to the definition that I provided. The lesions were primary, acquired, melanotic, and flat. Was there a rare case of some other condition like an atypical nevus? It might have occurred, but we were pretty strict in our diagnostic approach, and I do not think there were any errors due to over-diagnosis. Dr. Grossniklaus mentioned melanoma in situ. He has written a magnificent article on this in response to Dr. Bernie Ackerman, a dermatopathologist, who claims that all PAM should be called melanoma in situ and that ophthalmic pathologists use the wrong terminology. Opposition to that claim was presented by Dr. Grossniklaus in the journal Modern Pathology. I believe that we are going to continue to call it PAM in ophthalmology. With regard to the question regarding mild, moderate, and severe classification, our pathologist, Ralph Eagle, generally preferred to use the categories of mild and severe. Many are histological borderline cases. and are - difficult interpretations for pathologist.. Regarding nodularity and vascularity that Dr. Grossniklaus has mentioned, if there was nodularity or vascularity we generally excised the lesion and if they proved to be melanoma initially, they were excluded from this study of PAM. I think that answers that question. That also answers the question regarding amelanotic PAM. I think if you have PAM and you follow the patient and you see amelanotic thickening starting anywhere, you must assume that PAM is evolving into a melanoma. .Regarding question of Dr. Flach about change after biopsy, there many different cases here and indeed, some of them did change after biopsy and showed progression. Many of those were from patients who had undergone biopsy elsewhere before being referred to us. These were much more extensive lesions and we could not remove them entirely. Therefore, we performed the biopsy and applied cryotherapy so that the entire pigmented area was treated. Using that approach, recurrence is not common. Regarding how we select treatment, when a patient presents with 1 o’clock of PAM we generally advise observation. However, there are several factors you must consider, such as the age and general health of the patient, a personal history of cancer, family history of cancer,, and others. All of these findings are taken into account when making a therapeutic decision The last question was about chemotherapy and other topical agents. Topical mitomycin-C is effective for mild cases of PAM. It is less effective for more extensive cases, particularly if there is deeper stromal involvement. Mitomycin C is more squamous cell carcinoma in situ. I appreciate the attention of the audience and the comments of Dr. Grossniklaus and others.
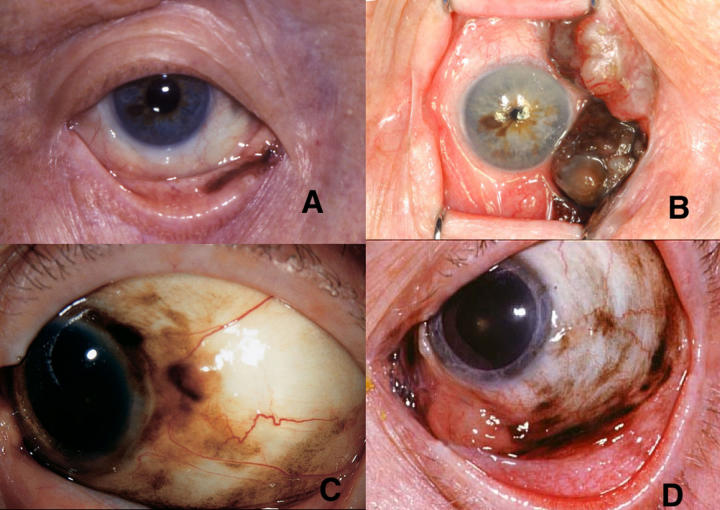
FIGURE 2.
Appearance of primary acquired melanosis (PAM) at various sites. A, PAM involving bulbar conjunctiva and adjacent cornea. B, Extensive multifocal PAM involving broad areas of bulbar conjunctiva and cornea. C, PAM involving bulbar and forniceal conjunctiva and caruncle. D, PAM confined to tarsal conjunctiva as seen with eyelid everted.
FIGURE 3.
Histopathology grading of primary acquired melanosis (PAM). A, PAM without atypia (hematoxylin-eosin, ×100 ). B, PAM with mild atypia (hematoxylin-eosin, ×100 ). C, PAM with severe atypia (hematoxylin-eosin, ×50). D, PAM with very severe atypia (hematoxylin-eosin, ×200).
ACKNOWLEDGMENTS
Funding/Support: Support for this study was provided by the Eye Tumor Research Foundation, Philadelphia, Pennsylvania; the Award of Merit in Retina Research, Houston, Texas (J.A.S.); the Macula Foundation, New York, New York (J.A.S.); a donation from Michael, Bruce, and Ellen Ratner, New York, New York (J.A.S., C.L.S.); and by the Noel T. and Sara L. Simmonds Endowment for Ophthalmic Pathology, Philadelphia (R.C.E.).
Financial Disclosures: None.
REFERENCES
- 1.Shields JA, Shields CL. Conjunctival primary acquired melanosis. In: Shields JA, Shields CL, editors. Eyelid, Conjunctival and Orbital Tumors. An Atlas and Textbook. Philadelphia: Lippincott, Williams & Wilkins; 2007. Forthcoming. [Google Scholar]
- 2.Shields CL, Demirci H, Karatza E, Shields JA. Clinical survey of 1643 melanocytic and nonmelanocytic tumors of the conjunctiva. Ophthalmology. 2004;111:1747–1754. doi: 10.1016/j.ophtha.2004.02.013. [DOI] [PubMed] [Google Scholar]
- 3.Shields CL, Shields JA. Tumors of the conjunctiva and cornea. Surv Ophthalmol. 2004;49:3–24. doi: 10.1016/j.survophthal.2003.10.008. [DOI] [PubMed] [Google Scholar]
- 4.Folberg R. Melanocytic lesions of the conjunctiva. In: Spencer WH, editor. Ophthalmic Pathology. An Atlas and Textbook. 4. Vol. 1. Philadelphia: WB Saunders; 1996. pp. 125–147. [Google Scholar]
- 5.Reese AB. Precancerous and cancerous melanosis. Am J Ophthalmol. 1966;61:1272–1277. doi: 10.1016/0002-9394(66)90256-x. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman LE. Criteria for management of melanosis. Arch Ophthalmol. 1966;61;76:307–308. [Google Scholar]
- 7.Folberg R, McLean IW, Zimmerman LE. Primary acquired melanosis of the conjunctiva. Hum Pathol. 1985;16:129–135. doi: 10.1016/s0046-8177(85)80061-7. [DOI] [PubMed] [Google Scholar]
- 8.Folberg R, McLean IW. Primary acquired melanosis and melanoma of the conjunctiva; terminology, classification, and biologic behavior. Hum Pathol. 1986;17:652–654. doi: 10.1016/s0046-8177(86)80175-7. [DOI] [PubMed] [Google Scholar]
- 9.Folberg R, Jakobiec FA, Bernardino VB, Iwamoto T. Benign conjunctival melanocytic lesions. Clinicopathologic features. Ophthalmology. 1989;96:436–461. doi: 10.1016/s0161-6420(89)32878-8. [DOI] [PubMed] [Google Scholar]
- 10.Folberg R, McLean IW, Zimmerman LE. Conjunctival melanosis and melanoma. Ophthalmology. 1984;91:673–678. doi: 10.1016/s0161-6420(84)34245-2. [DOI] [PubMed] [Google Scholar]
- 11.Folberg R, McLean IW, Zimmerman LE. Malignant melanoma of the conjunctiva. Hum Pathol. 1985;16:136–143. doi: 10.1016/s0046-8177(85)80062-9. [DOI] [PubMed] [Google Scholar]
- 12.Jakobiec FA, Folberg R, Iwamoto T. Clinicopathologic characteristics of premalignant and malignant melanocytic lesions of the conjunctiva. Ophthalmology. 1989;96:147–166. doi: 10.1016/s0161-6420(89)32920-4. [DOI] [PubMed] [Google Scholar]
- 13.Ackerman AB, Sood R, Koenig M. Primary acquired melanosis of the conjunctiva is melanoma in situ. Mod Pathol. 1991;4:253–263. [PubMed] [Google Scholar]
- 14.Gloor P, Alexandrakis G. Clinical characterization of primary acquired melanosis. Invest Ophthalmol Vis Sci. 1995;36:1721–1729. [PubMed] [Google Scholar]
- 15.Vereecken G, Gobert A, De Laey JJ, Hanssens M. Primary acquired melanosis and melanoma of the conjunctiva. Bull Soc Belge Ophthalmol. 1996;263:97–100. [PubMed] [Google Scholar]
- 16.Chalasani R, Giblin M, Conway RM. Role of topical chemotherapy for primary acquired melanosis and malignant melanoma of the conjunctiva and cornea: review of the evidence and recommendations for treatment. Clin Experiment Ophthalmol. 2006;34:708–714. doi: 10.1111/j.1442-9071.2006.01356.x. [DOI] [PubMed] [Google Scholar]
- 17.Jay V, Font RL. Conjunctival amelanotic malignant melanoma arising in primary acquired melanosis sine pigmento. Ophthalmology. 1998;105:191–194. doi: 10.1016/s0161-6420(98)92156-x. [DOI] [PubMed] [Google Scholar]
- 18.Shields JA, Shields CL, De Potter P. Surgical approach to conjunctival tumors. The 1994 Lynn B. McMahan Lecture. Arch Ophthalmol. 1997;115:808–815. doi: 10.1001/archopht.1997.01100150810025. [DOI] [PubMed] [Google Scholar]
- 19.Brownstein S, Jakobiec FA, Wilkinson RD, Lombardo J, Jackson WB. Cryotherapy for precancerous melanosis (atypical melanocytic hyperplasia of the conjunctiva) Arch Ophthalmol. 1981;99:1224–1231. doi: 10.1001/archopht.1981.03930020098009. [DOI] [PubMed] [Google Scholar]
- 20.Jakobiec FA, Rini FJ, Fraunfelder FT, et al. Cryotherapy for conjunctival primary acquired melanosis and malignant melanoma. Experience with 62 cases. Ophthalmology. 1988;95:1058–1070. doi: 10.1016/s0161-6420(88)33058-7. [DOI] [PubMed] [Google Scholar]
- 21.Frucht-Pery J, Pe’er J. Use of mitomycin C in the treatment of conjunctival primary acquired melanosis with atypia. Arch Ophthalmol. 1996;114:1261–1264. doi: 10.1001/archopht.1996.01100140461020. [DOI] [PubMed] [Google Scholar]
- 22.Paridaens AD, McCartney AC, Hungerford JL. Multifocal amelanotic conjunctival melanoma and acquired melanosis sine pigmento. Br J Ophthalmol. 1992;76:163–165. doi: 10.1136/bjo.76.3.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demirci H, McCormick SA, Finger PT. Topical mitomycin chemotherapy for conjunctival malignant melanoma and primary acquired melanosis with atypia: clinical experience with histopathologic observations. Arch Ophthalmol. 2000;118:885–891. [PubMed] [Google Scholar]
- 24.Yuen VH, Jordan DR, Brownstein S, Dorey MW. Topical mitomycin treatment for primary acquired melanosis of the conjunctiva. Ophthal Plast Reconstr Surg. 2003;19:149–151. doi: 10.1097/01.IOP.0000055826.30486.CC. [DOI] [PubMed] [Google Scholar]
- 25.Shields CL, Shields JA, Armstrong T. Management of conjunctival and corneal melanoma with surgical excision, amniotic membrane allograft, and topical chemotherapy. Am J Ophthalmol. 2001;132:576–578. doi: 10.1016/s0002-9394(01)01085-6. [DOI] [PubMed] [Google Scholar]
- 26.Paridaens D, Beekhuis H, van Den Bosch W, Remeyer L, Melles G. Amniotic membrane transplantation in the management of conjunctival malignant melanoma and primary acquired melanosis with atypia. Br J Ophthalmol. 2001;85:658–661. doi: 10.1136/bjo.85.6.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robertson DM, Hungerford JL, McCartney A. Malignant melanomas of the conjunctiva, nasal cavity, and paranasal sinuses. Am J Ophthalmol. 1989;108:440–442. doi: 10.1016/s0002-9394(14)73314-8. [DOI] [PubMed] [Google Scholar]
- 28.McNab AA, McKelvie P. Malignant melanoma of the lacrimal sac complicating primary acquired melanosis of the conjunctiva. Ophthalmic Surg Lasers. 1997;28:501–504. [PubMed] [Google Scholar]
- 29.Shields CL, Shields JA, Gunduz K, et al. Conjunctival melanoma: risk factors for recurrence, exenteration, metastasis and death in 150 consecutive patients. Arch Ophthalmol. 2000;118:1497–1507. doi: 10.1001/archopht.118.11.1497. [DOI] [PubMed] [Google Scholar]