Abstract
Purpose
To define the incidence, clinical characteristics, and outcomes following treatment of symptomatic acquired lacrimal outflow obstruction (SALOO) in Olmsted County, Minnesota, from 1976 to 2000, and to test the hypothesis that the incidence of this disorder increased over this interval.
Methods
In this retrospective, population-based study, the Rochester Epidemiology Project was used to identify patients above the age of 5 years with SALOO. Patient medical records were reviewed, and the incidence and localization of lacrimal obstruction were determined.
Results
Five-hundred eighty-seven patients with SALOO were identified, with an average annual incidence rate of 30.47 per 100,000. Nasolacrimal duct obstruction was most common, with an incidence of 20.24 per 100,000. The increase in incidence from 1976–1979 to 1996–2000 was statistically significant (P=.01). Among 397 patients with nasolacrimal duct obstruction, 107 (27%) were male and 290 (73%) female, with a mean age of 59.5 ± 22 years. SALOO and nasolacrimal duct obstruction incidence increased with age. Glaucoma, dry eye, cataract, diabetes mellitus, systemic malignancy, cigarette smoking, and hypertension were noted in 5.5%, 8.7%, 37.5%, 10.9%, 18.5%, 26.4%, and 41.1% of patients, respectively. One hundred eleven patients underwent dacryocystorhinostomy, with a success rate of 94.1%.
Conclusions
SALOO incidence increased during the study interval, although a possible plateau effect was noted during the last 5 years of the study period. The majority of patients were female above the age of 66 years. The latter finding, in conjunction with US demographic trends, suggests that the frequency of SALOO may continue to increase in the future. External dacryocystorhinostomy appeared to be effective in the management of nasolacrimal duct obstruction.
INTRODUCTION
Symptoms attributable to lacrimal outflow obstruction were, according to the renowned ophthalmic historian Julius Hirschberg,1 described in the papyrus documents of the ancient Egyptians. Lacrimal sac abnormalities were mentioned in the Talmud.2 The term epiphora dates back to ancient Greece and is based on the Greek word epifora, which is in turn derived from the root words ferein (to bring) and epi (upon).3 Hirschberg4 noted that the school of Hippocrates recognized the relationship between epiphora and aging. Lacrimal sac abscess (agchiloph) and fistula formation (aigiloph) were reported by the ancient Greeks, and the Roman Celsus wrote about surgical management of these problems.5 Wafai6 wrote that the prominent Arabian ophthalmologist Ali Ibn Isa described dacryocystitis in his encyclopedic ophthalmic reference published 900 years ago.
The relationship between lacrimal fistula and underlying inflammation was reported by Stahl in Germany approximately 300 years ago.7,8 Shortly thereafter, Dominique Anel of France ushered in the era of contemporary lacrimal evaluation utilizing lacrimal system probing and irrigation.9 Current surgical approaches to the correction of acquired lacrimal outflow obstruction date back to the descriptions of intranasal and external dacryocystorhinostomy in 1893 and 1904 by Caldwell10 and Toti,11 respectively. In 1920, Dupuy-Dutemps and Bourguet12 described their modified technique of external dacryocystorhinostomy (utilizing flaps of lacrimal sac and nasal mucosa), which remains a mainstay of treatment of acquired nasolacrimal duct obstruction today.
BACKGROUND AND SIGNIFICANCE
Despite the long-standing recognition of lacrimal symptoms summarized in the historical perspective above, relatively little information is available concerning the epidemiology of acquired lacrimal outflow obstruction. Several investigators have found that symptomatic congenital dacryostenosis is a common disorder, with previous studies revealing incidence rates of 0.79%13 to 1.2%14 to 6%15,16 in Western populations and up to 12% in Japanese populations.17 Although symptomatic acquired dacryostenosis is also commonly encountered in clinical practice, it is difficult to define the incidence of this problem. In one study, Dalgleish18 reported an incidence of lacrimal obstruction of 11% increasing with patient age to over 30% in a series of 3487 patients undergoing lacrimal irrigation prior to intraocular surgery at one eye hospital; this study did not, however, address associated symptoms or systemic disorders, did not specify the location(s) of obstruction, and was not population-based. Indeed, MEDLINE- and EMBASE-assisted searches performed with the assistance of a certified medical reference librarian failed to reveal any population-based studies that attempted to describe the incidence of this disorder. A current population-based study providing this information would be useful in terms of determining the appropriate allocation of health care research and care delivery resources directed toward lacrimal obstruction. On a related note, it is the author’s personal impression that the incidence of symptomatic acquired lacrimal outflow obstruction (SALOO) has been increasing over the past 25 years, but such impressions are likely to be highly unreliable owing to a number of factors, including referral bias. A population-based study evaluating trends in SALOO incidence would potentially be helpful in estimation of the future incidence of this disorder.
While ocular disorders including herpes simplex19 and/or treatments including glaucoma medications20 have been associated with the development of lacrimal obstruction, the frequency of these potential contributory factors in a defined population of patients with lacrimal obstruction has not been determined. In addition, numerous systemic disorders,21–23 including environmental allergy,24 sarcoidosis,25 Wegener granulomatosis,26 and lymphoma,27 may be associated with lacrimal obstruction, but the frequency of these associated disorders is similarly unclear.
Specific Aims
The specific aims of this study were as summarized below:
To define the age-specific incidence of SALOO in Olmsted County, Minnesota, during intervals from 1976–2000.
To test the hypothesis that the incidence of SALOO has increased from the beginning of the study period (during the interval 1976–1979) to the end of the study period (during the interval 1995–2000).
To describe the demographics and presenting signs and symptoms of SALOO in this population.
To estimate the incidence of selected ocular disorders in this patient population, including glaucoma, herpes simplex and zoster virus infection, dry eye syndrome, ectropion, entropion, and ocular cicatricial pemphigoid.
To determine the incidence of the selected ocular treatments in this patient population, including topical glaucoma medications, topical antiviral medications, and previous punctual occlusion.
To determine the incidence of selected medical disorders in this patient population, including sinusitis, environmental allergy, sinonasal neoplasm or surgery, Wegener granulomatosis, sarcoidosis, asthma, hypertension, diabetes mellitus, leukemia, lymphoma, other systemic neoplasms, systemic chemotherapy, other systemic medications including hormonal therapy, and cigarette smoking.
For patients with acquired dacryostenosis, to define location(s) of obstruction, treatment option(s) elected, and treatment outcomes.
For patients undergoing dacryocystorhinostomy (DCR) surgery, to define risk factors for failure, including age, gender, use of topical medications, associated ocular or systemic disorders, and initial clinical presentation (epiphora, conjunctivitis, dacryocystitis, or a combination thereof).
For patients undergoing failed DCR, to define the time course to failure.
SUBJECTS AND METHODS
OVERVIEW
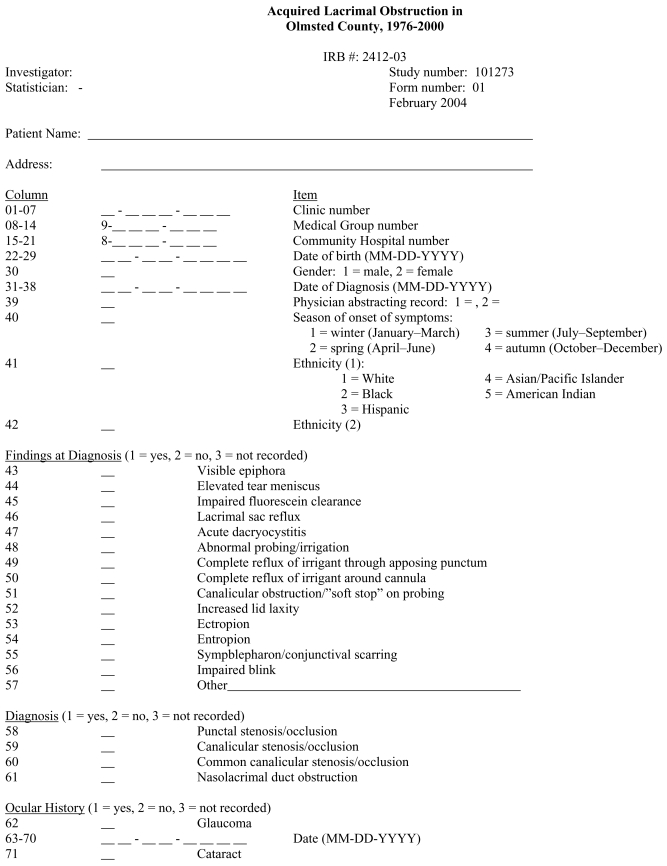
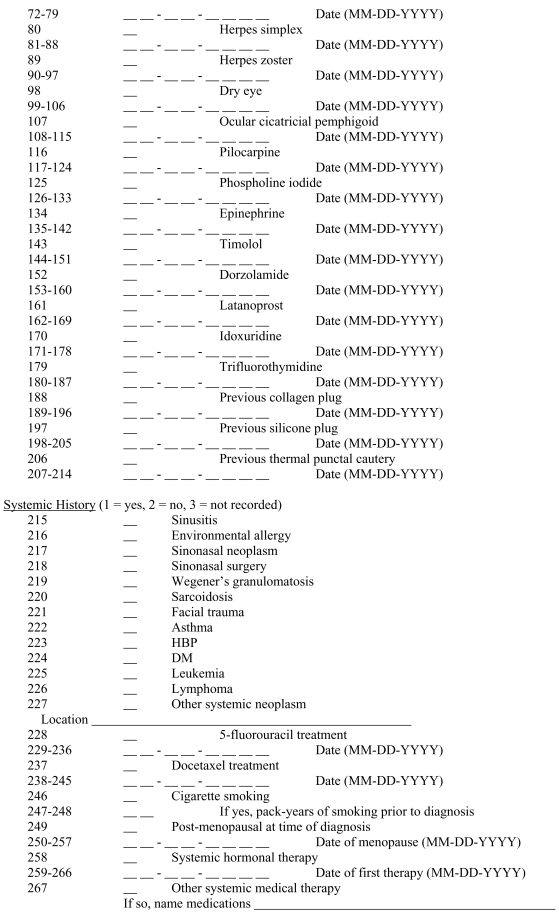
In this study, residents of Olmsted County, Minnesota, with a new diagnosis of acquired lacrimal outflow obstruction made during the period 1976–2000 were identified. Potential cases were identified using relevant diagnostic indices through the Rochester Epidemiology Project. A 1-year residency period in Olmsted County was required for potential patients. Once the diagnosis of each potential case had been confirmed and residency established, the complete inpatient and outpatient medical record was reviewed and pertinent information abstracted using a standardized data form. Incidence rates for the study period and for each 5-year period therein were calculated. This information was used to detect changes in the distribution of cases by age and gender as well as overall age- and gender-adjusted incidence rates during the intervals studied. Information regarding ocular and systemic disorders potentially associated with lacrimal outflow obstruction was abstracted for each patient. Data regarding treatment(s) performed and the outcomes thereof were recorded as well.
Setting
Numerous epidemiologic studies have been performed in Olmsted County, Minnesota. Its population is largely served by a unified medical care system that has accumulated comprehensive medical records over a long period of time. Olmsted County lies within the southeastern portion of Minnesota. Approximately 80% of the county population (according to census data for the year 2000, 124,277; above age 5, 113,576) reside within Rochester, the county seat. The extrapolation of findings from this study to groups not represented within Olmsted County may, however, be problematic.
Data Resource
Epidemiologic research in Olmsted County is possible because nearly all medical care is delivered to patients in the county by a limited number of providers. Much of this medical care is provided by the Mayo Clinic, a major referral center with over 1600 full-time physicians representing every medical and surgical specialty. The Mayo Clinic system also encompasses the 2 major hospitals in Olmsted County, St Mary’s Hospital and Rochester Methodist Hospital, with a combined total of 1900 beds. While being a major secondary and tertiary referral center, Mayo Clinic provides as well a significant portion of the primary care received by the local population. Approximately 40 years ago, the Olmsted Medical Center and its hospital, the Olmsted Community Hospital, joined the Mayo Clinic and its hospitals in providing medical care in Olmsted County.
From the epidemiologic viewpoint, each provider uses a unit medical record system whereby all data collected on an individual are assembled in one place. The Mayo Clinic unit record, for example, contains the details of every inpatient hospitalization at its 2 large affiliated hospitals, every outpatient visit to the office, clinic, or emergency room, every physician house or nursing home visit, every laboratory result, and correspondence. The Mayo Clinic system now contains over 6,000,000 histories, and the record storage system has allowed an extremely high percentage of record retrieval.
Utilization of the medical records has been facilitated by the maintenance at the Mayo Clinic of extensive indices based on clinical, radiologic, and histologic diagnoses and surgical procedures since the early 1900s. The Rochester Epidemiology Project has developed a similar index for the records of all other providers of medical care to Rochester and Olmsted County residents. These include the Olmsted Medical Group, the Olmsted Community Hospital, the University of Minnesota Hospitals and VA Medical Center in Minneapolis, community hospitals in the surrounding counties, and the few sole medical practitioners in Olmsted County. Through the Rochester Epidemiology Project, there is thus effective linkage of medical records from essentially all sources of medical care to the Olmsted County population. The Rochester Epidemiology Project has served as the basis for a large number of population-based studies.
Identification of Cases
Potential cases of lacrimal obstruction were identified through diagnostic indices for 1976 through 2000. The HICDA and ICDM-9 diagnostic codes used for potential case retrieval corresponded to those including “lacrimal duct obstruction NOS,” “epiphora,” “punctal stenosis,” “canalicular stenosis,” ”canaliculitis,” “dacryocystitis,” and “dacryostenosis.” A complete list of diagnostic codes utilized during record retrieval is presented in Appendix A. These terms were cross-referenced with patient age to allow retrieval of potential cases where patients were greater than 5 years of age. Other codes associated with lacrimal obstruction included “lacrimal duct obstruction, neonatal” and “congenital lacrimal duct obstruction.” Potential cases associated with these codes were not included from the study. Residency verification was performed for each potential patient.
Following preliminary case identification, the complete inpatient and outpatient medical record of each potential subject was obtained and reviewed to confirm the diagnosis of acquired lacrimal outflow obstruction. Diagnostic criteria included at least one of the following for each patient: a visibly elevated tear meniscus or visible epiphora, impaired fluorescein dye clearance, punctal stenosis, reflux upon lacrimal sac compression, acute dacryocystitis, abnormalities upon lacrimal probing or irrigation, and abnormalities on dacryocystography or dacryoscintigraphy. The year of initial diagnosis was used to establish the time period for incidence calculation purposes; each patient was therefore counted only once in this regard to ensure true calculation of incidence as opposed to prevalence.
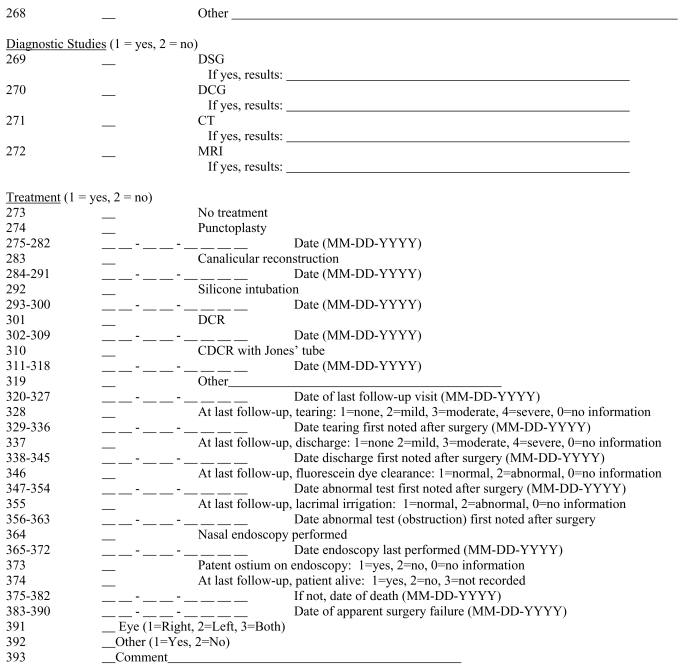
Once the diagnosis of lacrimal obstruction was confirmed, each record was abstracted to ascertain age at diagnosis, signs and symptoms at presentation, pertinent past ocular history, past medical history, medical or surgical treatment, and subsequent clinical course, using the Data Form presented in Appendix B. Past ocular and past medical historical factors were listed as positive for a given patient if present at or before the time lacrimal obstruction was diagnosed. In this study, surgical success was defined as resolution or improvement of symptoms to the point that no further treatment would be contemplated as documented in the medical record.
IRB Review and Research Authorization
Appropriate institutional review board (IRB) approval of this study was obtained from the Mayo Clinic and the Olmsted Medical Center. Records were reviewed of only those potential subjects who provided authorization for review of their medical records for research purposes. This project was limited to a retrospective review of medical records and did not involve experimentation on human subjects. The data were analyzed anonymously, and the policies and safeguards of the Rochester Epidemiology Project, the Olmsted Medical Center Research Committee, and the Mayo Clinic Department of Health Sciences Research were used to ensure confidentiality. Data reported below are listed only in the aggregate.
Data Analysis
Age- and gender-specific incidence rates were calculated for Olmsted County. The frequency of each associated condition noted above was analyzed. Outcomes data were then analyzed by subgroups pertaining to the location of obstruction and the treatment performed as well as the potential associated conditions listed above. Data were analyzed using Poisson regression analysis, and Kaplan-Meier survival curve analysis was performed for individuals undergoing DCR surgery and punctoplasty.
RESULTS
Case Identification
Using the diagnostic terms listed above, a total of 1161 charts were identified for review. Of these charts, research authorization for participation in the Rochester Epidemiology Project was denied for 49 patients. The majority of the patients who denied research authorization were female and above the age of 40, corresponding to the distribution of patients in this study. It is therefore unlikely that the absence of these patient records from this review significantly altered the demographic composition of this patient cohort. No other information is available regarding these patients. It should be noted, however, that the denial of permission for record review for these patients was generic and applied to all retrospective studies, and it is therefore unlikely that refusal to participate was related specifically to lacrimal status.
Upon chart review, 525 charts did not meet the diagnostic criteria listed above for lacrimal obstruction or Olmsted County residency. Analysis of the remaining 587 charts served as the basis for the current study.
Incidence
The age- and gender-specific annual incidence rates of lacrimal outflow obstruction by site of obstruction in the Olmsted County population during the period 1976–2000 are presented in Tables 1 through 9. Localization of the site of obstruction is summarized in Table 10. As noted, nasolacrimal duct obstruction was the most common form of obstruction, occurring in over two-thirds of patients in this series.
TABLE 1.
STATISTICAL ANALYSIS OF INTERVAL INCIDENCE DIFFERENCES OF ALL FORMS OF DACRYOSTENOSIS DURING STUDY PERIOD
| TIME INTERVALS | P VALUE (STUDENT T TEST) |
|---|---|
| 1995–2000 vs 1990–1994 | .003 |
| 1995–2000 vs 1985–1989 | .06 |
| 1995–2000 vs 1980–1984 | .77 |
| 1995–2000 vs 1976–1979 | .01 |
| 1990–94 vs 1985–1989 | .33 |
| 1990–94 vs 1980–1984 | .005 |
| 1990–94 vs 1976–1979 | <.001 |
| 1985–89 vs 1980–1984 | .06 |
| 1985–89 vs 1976–1979 | <.001 |
| 1980–84 vs 1976–1979 | .03 |
TABLE 9.
SUMMARY AGE- AND GENDER-ADJUSTED ANNUAL INCIDENCE RATES FOR NASOLACRIMAL DUCT OBSTRUCTION, 1976–2000*†
| SUMMARY RATES | INCIDENCE RATE PER 1000 | SE (POISSON) | 95% LOWER | CI UPPER | |
|---|---|---|---|---|---|
| Age-adjusted | Females | 0.2610 | 0.015567 | 0.2305 | 0.2916 |
| Age-adjusted | Males | 0.1329 | 0.013654 | 0.1061 | 0.1596 |
| Age-adjusted | Total | 0.2054 | 0.010530 | 0.1847 | 0.2260 |
| Age- and sex-adjusted | Total | 0.202 | 0.010 | 0.182 | 0.223 |
CI, confidence interval.
Case Dataset = naso, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 10.
SITE(S) OF LACRIMAL OBSTRUCTION IN 587 PATIENTS
| SITE | NO. (%)* |
|---|---|
| Anatomic obstruction | |
| • Punctum | 153 (26.1) |
| • Canaliculus | 25 (4.3) |
| • Common canaliculus | 14 (2.4) |
| • Nasolacrimal duct | 397 (67.6) |
| Functional obstruction | 33 (5.6) |
Percentages exceed 100% owing to multifocal obstruction in some patients.
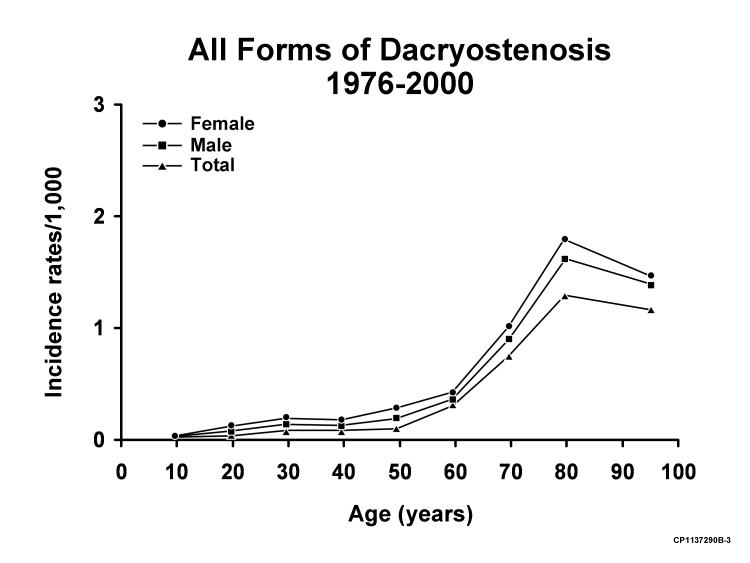
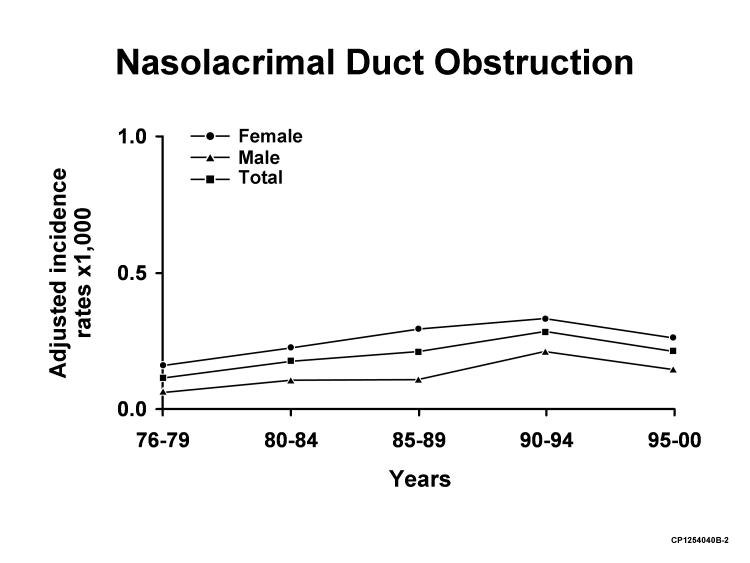
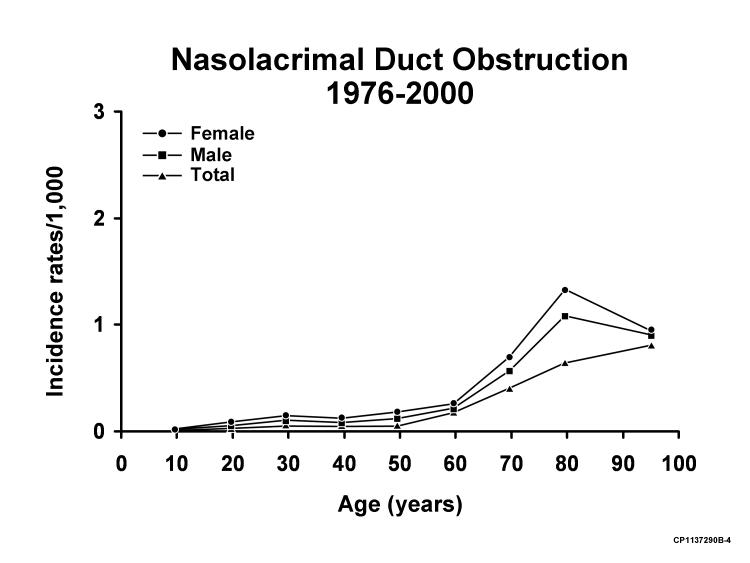
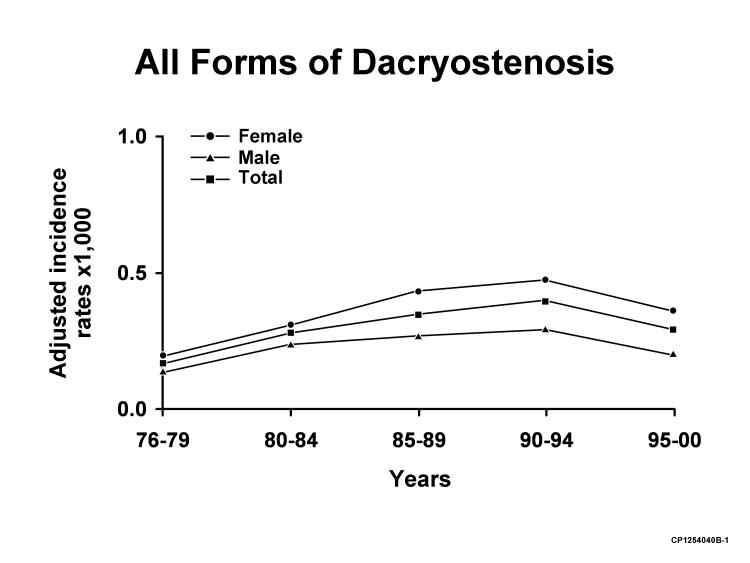
As seen in Figure 1, there was a statistically significant increase in incidence in diagnosis of all forms of lacrimal obstruction between the periods 1976–1980 and 1991–1995, with an apparent decrease in incidence during the period 1996–2000. The overall increase in incidence from 1976–1979 to 1996–2000 was, however, statistically significant (P=.01, Student t test). Statistical analysis of differences in incidence between other intervals during the study period is shown in Table 1. As shown in Figures 1 through 4, the incidence of all forms of lacrimal obstruction and of nasolacrimal duct obstruction alone was higher in females than males in all age ranges and throughout all time intervals during the study. The incidence of nasolacrimal duct obstruction and of all forms of lacrimal obstruction increased slowly beginning at age 40, with a more rapid rate of increase beginning at age 60. Over one-half of all patients with nasolacrimal duct obstruction in this study were older than the age of 65 years.
FIGURE 1.
Adjusted annual incidence rates of all forms of dacryostenosis for 5-year intervals from 1976 through 2000.
FIGURE 4.
Annual incidence rates of nasolacrimal duct obstruction for the period of 1976–2000 by age.
Two hundred nine of all patients (35.6%) demonstrated only left eye involvement, 176 (30%) only right eye involvement, and 202 (34.4%) bilateral involvement. One hundred fifty-seven (39.6%), 132 (33.3%), and 102 (27.2%) patients with nasolacrimal duct obstruction demonstrated left, right, and bilateral involvement, respectively. Ninety-eight patients (24.6%) with nasolacrimal duct obstruction were diagnosed with partial obstruction.
Presenting Signs and Symptoms
Incomplete recording of data in the source medical records regarding presenting signs and symptoms precluded statistical analysis of some of the common modes of presentation and initial findings on examination. Eighty-seven (22%) of 397 patients with nasolacrimal duct obstruction presented with acute dacryocystitis.
Associated Ocular and Systemic Conditions
The frequencies of associated ocular and systemic conditions and treatments are summarized in Tables 11 through 13. Systemic neoplasms noted in the patient cohort are listed in Table 14.
TABLE 11.
FREQUENCY OF SELECTED OCULAR CONDITIONS PRECEDING OR NOTED AT TIME OF DIAGNOSIS OF LACRIMAL OBSTRUCTION IN 587 PATIENTS
| CONDITION | FREQUENCY (%) |
|---|---|
| Glaucoma | 32 (5.45) |
| Cataract | 220 (37.48) |
| Herpes simplex virus infection | 6 (1.02) |
| Herpes zoster virus infection | 1 (0.17) |
| Dry eye syndrome | 51 (8.69) |
| Ectropion | 60 (10.2) |
| Entropion | 3 (0.51) |
| Ocular cicatricial pemphigoid | 1 (0.17) |
TABLE 13.
FREQUENCY OF SELECTED SYSTEMIC DISORDERS PRECEDING OR NOTED AT TIME OF DIAGNOSIS OF LACRIMAL OBSTRUCTION IN 587 PATIENTS
| CONDITION | NO. (%) |
|---|---|
| Sinusitis | 26 (4.43) |
| Environmental allergy | 2 (0.34) |
| Sinonasal neoplasm | 0 |
| Sinonasal surgery | 10 (1.70) |
| Facial trauma | 18 (3.07) |
| Wegener granulomatosis | 0 |
| Sarcoidosis | 2 (0.34) |
| Asthma | 35 (5.96) |
| Hypertension | 241 (41.06) |
| Diabetes mellitus | 64 (10.90) |
| Leukemia | 5 (0.85) |
| Lymphoma | 2 (0.34) |
| Other systemic neoplasms | 110 (18.74) |
| 5-Fluorouracil | 6 (1.02) |
| Docetaxel | 0 |
| Postmenopausal at diagnosis* | 290 of 408 (71.08) |
| Hormonal therapy* | 90 of 408 (22.06) |
| Cigarette smoking | 155 (26.41) |
Female patients only.
TABLE 14.
FREQUENCY OF SELECTED SYSTEMIC NEOPLASMS PRECEDING OR NOTED AT TIME OF DIAGNOSIS OF LACRIMAL OBSTRUCTION
| ANEOPLASM | NO. |
|---|---|
| Leukemia | 6 |
| Lymphoma | 2 |
| Acoustic neuroma | 1 |
| Basal cell carcinoma (brow, eyelid, lip, cheek, shin, shoulder, nose, temple, forehead) | 32 |
| Squamous cell carcinoma (brow, eyelid, lip, cheek, shin, shoulder, nose, temple, hand, vocal cord, scalp, arm) | 21 |
| Breast carcinoma | 25 |
| Bile duct adenoma | 1 |
| Bladder carcinoma | 4 |
| Uterine carcinoma | 6 |
| Colorectal carcinoma | 9 |
| Esophageal carcinoma | 1 |
| Gastric carcinoma | 3 |
| Lung carcinoma | 8 |
| Ovary carcinoma | 1 |
| Pharyngeal carcinoma | 1 |
| Prostatic carcinoma | 9 |
| Thyroid carcinoma | 1 |
| Total | 123* |
Some patients have 2 or more neoplasms.
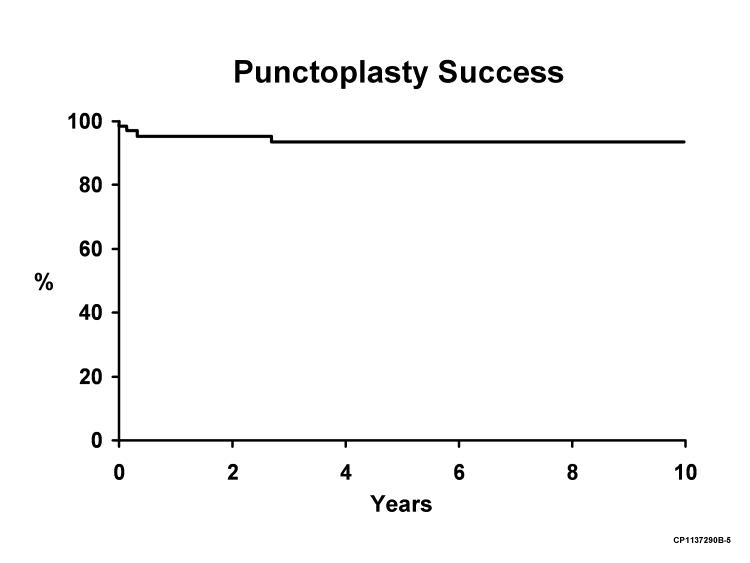
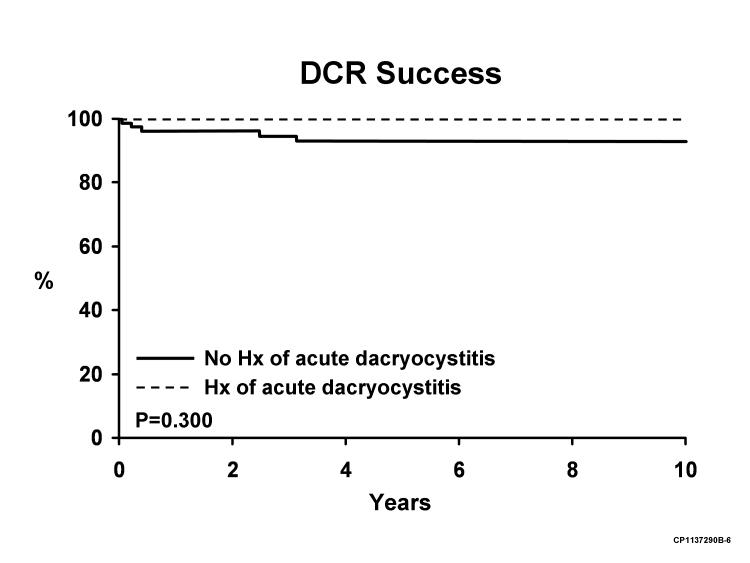
Treatment Outcomes
Surgical treatments performed and treatment outcomes are summarized in Table 15. Simple 5-year success rates for the most commonly performed procedures, DCR and punctoplasty, were 94.1% and 93.5%, respectively.
TABLE 15.
SURGICAL TREATMENTS PERFORMED FOR MANAGEMENT OF LACRIMAL OBSTRUCTION
| PROCEDURE | NO. TREATED | 5-YEAR % SUCCESS RATE |
|---|---|---|
| Punctoplasty | 71 | 93.5 |
| DCR (overall) | 106 | 94.1 |
| DCR (no dacryocystitis history) | 88 | 93.1 |
| DCR (dacryocystitis history) | 18 | 100 |
| CDCR with Jones tube | 6 | 66.6 |
CDCR, conjunctivodacryocystorhinostomy; DCR, dacryocystorhinostomy.
Kaplan-Meier survival curve analysis was performed for patients undergoing punctoplasty and DCR and is presented in Figures 5 and 6. An attempt was made to use a proportional hazards analysis to identify factors associated with DCR success. Neither age, gender, nor history of cigarette smoking appeared to be associated with differences in DCR success. There was a trend toward a higher success rate of surgery performed in patients with a history of acute dacryocystitis (with no surgical failures in 18 patients with such a history undergoing DCR) than in patients without a history of acute infection. This trend, however, did not achieve statistical significance (P=.30). It should be noted, however, that due to small numbers of surgical failures, this study lacked the statistical power to detect a difference between these 2 groups. It was not possible to calculate a risk ratio with confidence interval due to the lack of DCR failures in the acute dacryocystitis group. Similarly, due to the small number of DCR failures in this series, it was not possible to identify other factors that were associated with a higher risk of surgical failure. As noted in Figure 6, DCR failures in this series occurred within 3 years of surgery.
FIGURE 5.
Kaplan-Meier survival curve analysis for punctoplasty success.
FIGURE 6.
Kaplan-Meier survival curve analysis for dacryocystorhinostomy (DCR) success.
Lacrimal sac pathology studies were performed on 17 of 109 patients undergoing DCR surgery in this series. In 13 (76%) of these 17 patients, chronic inflammation was noted. Dacryolith formation was noted in 3 patients, and inverted papilloma was noted in 1 patient with previously diagnosed inverted papilloma involving the nasal cavity.
Two of 6 patients undergoing conjunctivodacryocystorhinostomy (CDCR) with Jones tube placement were considered to represent surgical successes after the initial procedure. Two additional patients underwent successful tube revision and replacement surgery, respectively. The remaining 2 patients were considered surgical failures and underwent tube removal.
DISCUSSION
Several investigators have studied the incidence of congenital nasolacrimal duct obstruction. Kendig and Guerry16 and Noda and colleagues17 noted incidence rates of 5.7% and 8% in series of American and Japanese infants, respectively, studied prospectively. These studies were performed on large consecutive series of neonates in the authors’ institutions, enhancing the accuracy of the resulting data. It is more difficult to determine the true incidence of acquired lacrimal obstruction, as this would entail prospective lacrimal evaluation of every individual in the population under study. The study performed by Dalgleish18 did entail lacrimal irrigation of every patient presenting for intraocular surgery at one hospital, but this population was not, therefore, necessarily representative of the population at large. In addition, this study did not provide information concerning the site(s) of obstruction or associated clinical symptoms.
An ideal study design to determine the incidence of both symptomatic and asymptomatic lacrimal obstruction would entail prospective evaluation of every patient in the population under study (including the performance of a history and physical examination incorporating lacrimal system irrigation and probing). The performance of lacrimal system irrigation and probing on asymptomatic patients for purely research purposes would not be approved according to current guidelines of the IRB at the author’s institution.
In view of the difficulties inherent in prospectively studying the incidence of lacrimal obstruction in the general population, we elected to study the incidence of symptomatic acquired lacrimal outflow obstruction (ie, lacrimal obstruction resulting in symptoms prompting medical evaluation). Even symptomatic acquired lacrimal outflow obstruction is challenging to study relative to congenital dacryostenosis due to difficulties in identifying a well-defined patient population in which disease incidence may be assessed.
A search by a certified medical reference librarian of multiple databases, including MEDLINE (back through 1957), EMBASE, Web of Science/Current Concepts, Journals@Ovid, and the Cochrane Library did not reveal previous population-based studies evaluating the incidence of symptomatic lacrimal obstruction in adult patients. This study revealed an overall age- and gender-adjusted incidence rate for all forms of symptomatic acquired lacrimal obstruction during the study period of 30.5 per 100,000 population (SE, 1.3; 95% confidence interval [CI], 28.0–33.0). The most common form of acquired dacryostenosis in this study, nasolacrimal duct obstruction, occurred with a frequency of 20.2 per 100,000 population (SE, 1.0; 95% CI, 18.2–22.3). The incidence of all forms of SALOO demonstrated a statistically significant increase (P = .01, Student t test) from the interval 1976–1979 to the interval 1996–2000.
As noted above, to the author’s knowledge there are no studies in other patient populations assessing the incidence of symptomatic lacrimal outflow obstruction in adult patients. It is of interest, however, to compare the incidence of SALOO to that of other ophthalmic disorders in the same population. Schoff and associates28 noted an overall age- and gender-adjusted annual incidence rate of open-angle glaucoma of 14.5 per 100,000 population in the Olmsted County population during the period 1965–1980. The rates increased with age from 1.6 in the fourth decade of life to 94.3 in the eighth decade. There was no significant difference in glaucoma incidence by gender. Similarly, while it is difficult to estimate the incidence of cataract per se in the Olmsted County population during the defined time period, Baratz and colleagues29 found the age- and gender-adjusted incidence of cataract extraction to be 470 per 100,000 population in Olmsted County in 1994. The incidence of all forms of acquired lacrimal obstruction and of nasolacrimal duct obstruction per se is thus somewhat higher than (but the same order of magnitude as) the incidence of glaucoma but significantly lower than the incidence of cataract extraction in the Olmsted County population.
This study also confirms the frequently made statement20 that acquired lacrimal obstruction is most commonly encountered in middle-aged or older female patients. The mean and median ages of patients with all forms of obstruction were 61 and 67 years, respectively. In this study, 69% of patients with all forms of obstruction and 73% of patients with nasolacrimal duct obstruction were female. It has been speculated that the smaller diameter of the inferior bony lacrimal fossa and lacrimal canal in females may contribute to the increased prevalence of nasolacrimal duct obstruction in female patients.30,31
As noted above, this study reveals an increase in the incidence of diagnosis of lacrimal obstruction from the interval 1976–1979 through the interval 1996–2000. It is difficult to determine whether this increase represented a true increase in incidence of obstruction, a greater tendency for patients to seek or be referred for medical evaluation of lacrimal obstruction as the study period progressed, more accurate diagnosis of obstruction, or some combination thereof. It is possible to comment superficially on at least the changes in potential availability of ophthalmic care during the study period. In specific, based on (1) Olmsted County population figures above age 5 years of 81,50632 in 1975 and 115,38733 in 2000 and (2) practicing ophthalmologist numbers in Olmsted County of 1434 and 3435 in 1975 and 2000, the number of ophthalmologists per 10,000 serving this population increased 71%, from 1.72 to 2.94, over the study interval. It remains difficult, however, to determine the degree, if any, to which the increasing number of ophthalmologists per capita in Olmsted County over the study period would have contributed to an increased frequency of diagnosis of lacrimal obstruction in the absence of data regarding other factors that could have influenced the frequency of diagnosis. Such factors could have included improved education with increased awareness of the symptoms and signs of lacrimal obstruction among referring physicians and/or patients over the study period and a resultant increase in physician- or self-referral for ophthalmic evaluation. The decrease in apparent incidence of obstruction during the period 1996–2000 compared with the period 1991–1995 would be consistent with a plateau in those factors reflecting increased case capture (as opposed to a true increase in incidence), such as more active patient referral or enhanced diagnostic accuracy. Ongoing studies would be required to determine whether the rates noted during the 1996–2000 period represent true current baseline incidence rates.
Several ocular disorders, including herpes simplex and herpes zoster infection,18,36,37 have been associated with acquired dacryostenosis. These disorders were noted in only 6 patients and 1 patient, respectively, in this series. Of the 6 patients with a history of herpes simplex infection, 3 had nasolacrimal duct obstruction, 2 had functional lacrimal outflow obstruction, and 1 had common canalicular obstruction. Idoxuridine, also associated with lacrimal obstruction,38 was used by only 1 patient in this cohort. Over 5% of patients in this study had a history of glaucoma, with a number of patients using topical medications, including pilocarpine hydrochloride and echothiophate iodide, which have been implicated in lacrimal obstruction.19 Three patients had a history of prior punctal plug placement, which may also be associated with outflow obstruction.39,40 This population-based study failed to reveal patients with lacrimal obstruction in association with ocular allergy, as has been previously reported.23
Case series have documented lacrimal obstruction in the context of a number of systemic disorders. Conditions such as sinusitis41 and sinonasal surgery42 were reported in 4.43% and 1.70%, respectively, of patients in this study. Facial trauma is a well-established risk factor for lacrimal obstruction43,44 and was encountered in 3.07% of patients in this series. Two patients in this series had sarcoidosis, another disorder associated with obstruction,24 and a total of 8 patients had leukemia or lymphoma.26 Several studies have documented the relationship between systemic 5-fluorouracil (5-FU) administration and dacryostenosis,45,46 and a history of 5-FU treatment was obtained in 6 patients in this study. In all, approximately 10% of patients in this cohort had a history of systemic disorders or treatments that have been associated with lacrimal outflow obstruction. In the absence of other associated predisposing factors, approximately 90% of patients in this study may be considered to have primary acquired nasolacrimal duct obstruction, as described by Linberg and McCormick.47 As noted in Table 13, there were a number of other systemic conditions occurring with a frequency exceeding 5% in patients, including asthma, hypertension, diabetes, cigarette smoking, hormonal replacement therapy, and various nonhematologic neoplasms. Assessment of the frequency of these disorders in an appropriate control population would be required to determine whether the coexistence of these disorders with lacrimal obstruction is more frequent than would be expected on the basis of chance alone.
From the outcomes perspective, the success rate of DCR in this study is comparable to that reported in numerous case series.48–50 As noted above, due to the small number of failures, we were not able to identify specific ocular or systemic risk factors associated with surgical failure, although as noted above, there appeared to be a trend to a higher success rate in association with a history of acute dacryocystitis. The outcomes of and problems associated with CDCR with Jones tube placement in the small number of patients undergoing this procedure in this cohort were similar to those noted in other reports.51
It is important to note that this study has a number of potential limitations. First, case identification is based on accurate diagnosis-based coding and retrieval of individual patient records through the Rochester Epidemiology Project. Fortunately, the infrastructure of this National Institutes of Health–funded data resource is robust with a trained coding staff, allowing the Rochester Epidemiology Project to serve as the basis for over 1,500 publications since 1966.52 In this retrospective study, data analysis was based only on the information that was present in each record, and in some cases these data were incomplete. In addition, the generalizability of the results of this study is limited by the fact that the demographics of Olmsted County are not necessarily representative of the United States in its entirety. A detailed comparison of the demographic characteristics of Olmsted County residents and the US population in 1990 is presented in Table 16.53 Based on the 2000 census, approximately 90% of Olmsted County residents were white,54 compared with 69% for the United States in general.55 The mean level of educational attainment56 and median household income57 is higher in Olmsted County than in the nation as a whole.56,57 Furthermore, access to ophthalmic and lacrimal subspecialty medical care (which may facilitate the diagnosis of acquired lacrimal obstruction) in Olmsted County may differ from that available nationwide. In terms of comparisons between study participants and other Olmsted County residents, study participants were more likely to be female (69% vs 51%) and older (mean/median ages 61/67 years vs 35/35 years). It is possible that study participants differed from other Olmsted County residents in other systematic ways that this retrospective study was unable to capture. Nonetheless, this study provides at least initial relatively current incidence information regarding a clinically important ophthalmic disorder. While this study suggests that the incidence of SALOO has increased from 1975–2000, it is difficult to reliably predict the future incidence of this disorder based on the findings of this study. Based on the significantly increased incidence of acquired lacrimal obstruction in female patients above the age of 60 years, the generalized aging of the US population58 and the increased preponderance of women in the elderly population,58 however, it appears possible that this condition may become more prevalent in the future. This likelihood supports the importance of continuing to improve our understanding of new factors that may be associated with lacrimal obstruction, such as docetaxel administration.59 The potentially increasing frequency of acquired lacrimal obstruction also supports the continued investigation of new, possibly less invasive options (including endonasal dacryocystorhinostomy60 and balloon dacryoplasty61) for the management of this common disorder.
FIGURE 2.
Adjusted annual incidence rates of nasolacrimal duct obstruction for 5-year intervals from 1976 through 2000.
FIGURE 3.
Annual incidence rates of all forms of dacryostenosis for the period 1976–2000 by age.
TABLE 2.
| INCIDENCE | INCIDENCE POPULATION | INCIDENCE RATES (×1000) | ADJUSTING POPULATION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | (B) | (C) | (D) | (E) | (F) | (G) | (H) | (I) | (J) | (K) | (L) | |
| AGE GROUP, yr | M | TOTAL | F | M | TOTAL | F | M | TOTAL | F | M | TOTAL | |
| 5–14 | 0 | 0 | 0 | 199220 | 210415 | 409635 | 0.0000 | 0.0000 | 0.0000 | 13746 | 14521 | 28267 |
| 15–24 | 3 | 0 | 3 | 200700 | 181833 | 382533 | 0.0149 | 0.0000 | 0.0078 | 13267 | 13965 | 27232 |
| 25-34 | 5 | 0 | 5 | 234948 | 222912 | 457860 | 0.0213 | 0.0000 | 0.0109 | 13983 | 14338 | 28321 |
| 35–44 | 10 | 5 | 15 | 197182 | 190156 | 387338 | 0.0507 | 0.0263 | 0.0387 | 17121 | 17176 | 34297 |
| 45–54 | 10 | 4 | 14 | 140977 | 137115 | 278092 | 0.0709 | 0.0292 | 0.0503 | 15146 | 14880 | 30026 |
| 55–64 | 11 | 12 | 23 | 99994 | 93979 | 193973 | 0.1100 | 0.1277 | 0.1186 | 10344 | 9708 | 20052 |
| 65–74 | 17 | 20 | 37 | 76862 | 59525 | 136387 | 0.2212 | 0.3360 | 0.2713 | 8528 | 7162 | 15690 |
| 75–84 | 26 | 18 | 44 | 56261 | 30919 | 87180 | 0.4621 | 0.5822 | 0.5047 | 6598 | 4341 | 10939 |
| 85–105 | 8 | 4 | 12 | 26564 | 8628 | 35192 | 0.3012 | 0.4636 | 0.3410 | 2689 | 1089 | 3778 |
| TOTAL | 90 | 63 | 153 | 1232708 | 1135482 | 2368190 | 0.0730 | 0.0555 | 0.0646 | 101422 | 97180 | 198602 |
Case Dataset = punctal, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 3.
| SUMMARY RATES | INCIDENCE RATE PER 1000 | SE (POISSON) | 95% LOWER | CI UPPER | |
|---|---|---|---|---|---|
| Age-adjusted | Females | 0.0843 | 0.008978 | 0.0667 | 0.1019 |
| Age-adjusted | Males | 0.0893 | 0.011603 | 0.0665 | 0.1120 |
| Age-adjusted | Total | 0.0846 | 0.006907 | 0.0711 | 0.0982 |
| Age- and sex-adjusted | Total | 0.085 | 0.0070 | 0.071 | 0.098 |
CI, confidence interval.
Case Dataset = punctal, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 4.
| INCIDENCE | INCIDENCE POPULATION | INCIDENCE RATES (×1000) | ADJUSTING POPULATION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | (B) | (C) | (D) | (E) | (F) | (G) | (H) | (I) | (J) | (K) | (L) | |
| AGE GROUP, yr | F | M | Total | F | M | Total | F | M | Total | F | M | Total |
| 5–14 | 1 | 0 | 1 | 199220 | 210415 | 409635 | 0.0050 | 0.0000 | 0.0024 | 13746 | 14521 | 28267 |
| 15–24 | 2 | 2 | 4 | 200700 | 181833 | 382533 | 0.0100 | 0.0110 | 0.0105 | 13267 | 13965 | 27232 |
| 25–34 | 7 | 2 | 9 | 234948 | 222912 | 457860 | 0.0298 | 0.0090 | 0.0197 | 13983 | 14338 | 28321 |
| 35–44 | 2 | 0 | 2 | 197182 | 190156 | 387338 | 0.0101 | 0.0000 | 0.0052 | 17121 | 17176 | 34297 |
| 45–54 | 2 | 0 | 2 | 140977 | 137115 | 278092 | 0.0142 | 0.0000 | 0.0072 | 15146 | 14880 | 30026 |
| 55–64 | 1 | 0 | 1 | 99994 | 93979 | 193973 | 0.0100 | 0.0000 | 0.0052 | 10344 | 9708 | 20052 |
| 65–74 | 1 | 1 | 2 | 76862 | 59525 | 136387 | 0.0130 | 0.0168 | 0.0147 | 8528 | 7162 | 15690 |
| 75–84 | 3 | 0 | 3 | 56261 | 30919 | 87180 | 0.0533 | 0.0000 | 0.0344 | 6598 | 4341 | 10939 |
| 85–105 | 0 | 1 | 1 | 26564 | 8628 | 35192 | 0.0000 | 0.1159 | 0.0284 | 2689 | 1089 | 3778 |
| Total | 19 | 6 | 25 | 1232708 | 1135482 | 2368190 | 0.015 | 0.005 | 0.011 | 101422 | 97180 | 198602 |
Case Dataset = cana, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 5.
| SUMMARY RATES | INCIDENCE RATE PER 1000 | SE (Poisson) | 95% LOWER | CI UPPER | |
|---|---|---|---|---|---|
| Age-adjusted | Females | 0.0152 | 0.003579 | 0.0082 | 0.0222 |
| Age-adjusted | Males | 0.0063 | 0.002929 | 0.0006 | 0.0121 |
| Age-adjusted | Total | 0.0107 | 0.002220 | 0.0063 | 0.0150 |
| Age- and sex- adjusted | Total | 0.011 | 0.002 | 0.006 | 0.015 |
CI, confidence interval.
Case Dataset = cana, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 6.
| INCIDENCE | INCIDENCE POPULATION | INCIDENCE RATES (×1000) | ADJUSTING POPULATION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | (B) | (C) | (D) | (E) | (F) | (G) | (H) | (I) | (J) | (K) | (L) | |
| AGE GROUP, YR | F | M | TOTAL | F | M | TOTAL | F | M | TOTAL | F | M | TOTAL |
| 5–14 | 0 | 0 | 0 | 199220 | 210415 | 409635 | 0.0000 | 0.0000 | 0.0000 | 13746 | 14521 | 28267 |
| 15–24 | 0 | 0 | 0 | 200700 | 181833 | 382533 | 0.0000 | 0.0000 | 0.0000 | 13267 | 13965 | 27232 |
| 25–34 | 1 | 0 | 1 | 234948 | 222912 | 457860 | 0.0043 | 0.0000 | 0.0022 | 13983 | 14338 | 28321 |
| 35–44 | 0 | 0 | 0 | 197182 | 190156 | 387338 | 0.0000 | 0.0000 | 0.0000 | 17121 | 17176 | 34297 |
| 45–54 | 1 | 0 | 1 | 140977 | 137115 | 278092 | 0.0071 | 0.0000 | 0.0036 | 15146 | 14880 | 30026 |
| 55–64 | 1 | 0 | 1 | 99994 | 93979 | 193973 | 0.0100 | 0.0000 | 0.0052 | 10344 | 9708 | 20052 |
| 65–74 | 5 | 0 | 5 | 76862 | 59525 | 136387 | 0.0651 | 0.0000 | 0.0367 | 8528 | 7162 | 15690 |
| 75–84 | 3 | 2 | 5 | 56261 | 30919 | 87180 | 0.0533 | 0.0647 | 0.0574 | 6598 | 4341 | 10939 |
| 85–105 | 0 | 1 | 1 | 26564 | 8628 | 35192 | 0.0000 | 0.1159 | 0.0284 | 2689 | 1089 | 3778 |
| TOTAL | 11 | 3 | 14 | 1232708 | 1135482 | 2368190 | 0.009 | 0.003 | 0.006 | 101422 | 97180 | 198602 |
Case Dataset = comcana, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 7.
SUMMARY AGE- AND GENDER-ADJUSTED ANNUAL INCIDENCE RATES FOR COMMON CANALICULAR STENOSIS, 1976–2000*†
| SUMMARY RATES | INCIDENCE RATE PER 1000 | SE (POISSON) | 95% LOWER | CI UPPER | |
|---|---|---|---|---|---|
| Age-adjusted | Females | 0.0108 | 0.003270 | 0.0044 | 0.0172 |
| Age-adjusted | Males | 0.0058 | 0.003348 | 0.0000 | 0.0123 |
| Age-adjusted | Total | 0.0080 | 0.002152 | 0.0038 | 0.0122 |
| Age- and sex-adjusted | Total | 0.0080 | 0.002 | 0.004 | 0.012 |
CI, confidence interval.
Case Dataset = comcana, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 8.
| INCIDENCE | INCIDENCE POPULATION | INCIDENCE RATES (×1000) | ADJUSTING POPULATION | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) | (B) | (C) | (D) | (E) | (F) | (G) | (H) | (I) | (J) | (K) | (L) | |
| AGE GROUP, YR | F | M | TOTAL | F | M | TOTAL | F | M | TOTAL | F | M | TOTAL |
| 5–14 | 5 | 5 | 10 | 199220 | 210415 | 409635 | 0.0251 | 0.0238 | 0.0244 | 13746 | 14521 | 28267 |
| 15–24 | 18 | 4 | 22 | 200700 | 181833 | 382533 | 0.0987 | 0.0220 | 0.0575 | 13267 | 13965 | 27232 |
| 25–34 | 35 | 13 | 48 | 234948 | 222912 | 457860 | 0.1490 | 0.0583 | 0.1048 | 13983 | 14338 | 28321 |
| 35–44 | 25 | 9 | 34 | 197182 | 190156 | 387338 | 0.1268 | 0.0473 | 0.0878 | 17121 | 17176 | 34297 |
| 45–54 | 27 | 8 | 35 | 140977 | 137115 | 278092 | 0.1915 | 0.0583 | 0.1259 | 15146 | 14880 | 30026 |
| 55–64 | 26 | 17 | 43 | 99994 | 93979 | 193973 | 0.2600 | 0.1809 | 0.2217 | 10344 | 9708 | 20052 |
| 65–74 | 54 | 24 | 78 | 76862 | 59525 | 136387 | 0.7026 | 0.4032 | 0.5719 | 8528 | 7162 | 15690 |
| 75–84 | 75 | 20 | 95 | 56261 | 30919 | 87180 | 1.3331 | 0.6469 | 1.0897 | 6598 | 4341 | 10939 |
| 85–105 | 25 | 7 | 32 | 26564 | 8628 | 35192 | 0.9411 | 0.8113 | 0.9093 | 2689 | 1089 | 3778 |
| TOTAL | 290 | 107 | 397 | 1232708 | 1135482 | 2368190 | 0.235 | 0.094 | 0.168 | 101422 | 97180 | 198602 |
Case Dataset = naso, Incidence Population = “. . . .” _COR, SUM (of P1976–P2000).
Adjusting population = USW2000 (US populations are in 1000’s).
TABLE 12.
FREQUENCY OF SELECTED OCULAR TREATMENTS PRECEDING OR NOTED AT TIME OF DIAGNOSIS OF LACRIMAL OBSTRUCTION IN 587 PATIENTS
| CONDITION | NO. (%) |
|---|---|
| Pilocarpine hydrochloride | 19 (3.24) |
| Echothiophate iodide | 1 (0.17) |
| Epinephrine hydrochloride | 3 (0.51) |
| Dipivefrin | 0 |
| Timolol maleate | 29 (4.94) |
| Latanoprost | 0 |
| Dorzolamide | 0 |
| Idoxuridine | 1 (0.17) |
| Trifluorothymidine | 2 (0.34) |
| Previous punctal plug placement | 3 (0.51) |
| Previous thermal punctal occlusion | 2 (0.34) |
Acknowledgments
Funding/Support: None. Financial Disclosures: None.
Other Acknowledgments: Robert Kennedy, MD, PhD, MBA, and George Bartley, MD, provided valuable advice regarding study design and reviewed a near-final draft of the manuscript. James Garrity, MD, and Elizabeth Bradley, MD, provided helpful suggestions regarding study design. Won Chan Park, MD, assisted in data collection. David Hodge and Gabriela Rosales performed statistical analyses.
APPENDIX A. CASE RETRIEVAL DIAGNOSTIC INDICES
DIAGNOSTIC CODES USED FOR RECORD RETRIEVAL
| TYPE OF CODE | CODE | DESCRIPTION |
|---|---|---|
| HICDA | 03680111 | DACRYOCYSTITIS, NOS |
| 03680112 | BOIL, LACRIMAL SAC | |
| 03680113 | INFLAMMATION, LACRIMAL SAC | |
| 03680114 | INFECTION, LACRIMAL SAC | |
| 03680120 | CANALICULITIS, ACUTE | |
| 03680130 | DACRYOCYSTITIS, ACUTE | |
| 03680140 | DACRYOCYSTITIS, PHLEGMON | |
| 03680170 | CANALICULITIS, CHRONIC | |
| 03680180 | DACRYOCYSTITIS, CHRONIC | |
| 03680210 | INFECTION, LACRIMAL | |
| 03680211 | INFLAMMATION, LACRIMAL GLAND OR DUCT | |
| 0368041 | STENOSIS, LACRIMAL DUCT | |
| 03680412 | OBSTRUCTION, NASOLACRIMAL DUCT | |
| 03680413 | OBSTRUCTION, LACRIMAL | |
| 03680414 | STRICTURE, LACRIMAL APPARATUS, DUCT | |
| 03680415 | OBSTRUCTION, TEAR DUCT | |
| 03680416 | OBSTRUCTION, CANALICULAR (LACRIMAL) | |
| 03680417 | STENOSIS, TEAR DUCT | |
| 03680418 | STRICTURE, PUNCTUM LACRIMALE | |
| 03680419 | DACRYOSTENOSIS | |
| ICD-9 | 375.3 | Acute & Unspecified inflammation Lacrimal passage |
| 375.41 | Chronic canaliculitis | |
| 375.42 | Chronic dacrocysitis | |
| 375.5 | STENOSIS AND INSUFFICIENCY OF LACRIMAL PASSAGES | |
| 375.2 | EPIPHORA |
APPENDIX B. CASE REVIEW DATASHEET
REFERENCES
- 1.Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 1. Bonn, Germany: JP Wayenborgh; 1982. p. 10. [Google Scholar]
- 2.Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 1. Bonn, Germany: JP Wayenborgh; 1982. p. 22. [Google Scholar]
- 3. [Accessed Dec 9, 2006]; Hypertext Webster Gateway: “epiphora.” http://www.bennetyee.org/http_webster.cgi?epiphora&method=exact.
- 4.Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 1. Bonn, Germany: JP Wayenborgh; 1982. p. 85. [Google Scholar]
- 5.Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 1. Bonn, Germany: JP Wayenborgh; 1982. p. 242. [Google Scholar]
- 6.Wafai MZ, Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 2. Bonn, Germany: JP Wayenborgh; 1985. p. 135. [Google Scholar]
- 7.Hirschberg J. In: The History of Ophthalmology. Blodi FC, translator. Vol. 4. Bonn, Germany: JP Wayenborgh; 1984. p. 83. [Google Scholar]
- 8.Duke-Elder S, MacFaul PA. In: System of Ophthalmology. Duke-Elder S, editor. Vol. 8. London: Henry Kimpton Publishers; 1974. p. 699. [Google Scholar]
- 9.Duke-Elder S, MacFaul PA. In: System of Ophthalmology. Duke-Elder S, editor. Vol. 8. London: Henry Kimpton Publishers; 1974. p. 675. [Google Scholar]
- 10.Caldwell GW. Two new operations for obstruction of the nasal duct with preservation of the canaliculi and an incidental description of a new lacrimal probe. N Y Med J. 1893;57:581. [Google Scholar]
- 11.Toti A. Nuovo metodo conservatore di cura radicale delle suppurazioni croniche del sacco lacrimale (Dacriocistorinostomia) Clin Mod Firenze. 1904;10:385. [Google Scholar]
- 12.Dupuy-Dutemps MM, Bourguet ET. Note preliminaire sur un prodede de dacryocystorhinostomie. Ann Ocul (Paris) 1920;157:445–447. [Google Scholar]
- 13.Rantakallio P, Krause U, Krause K. The use of the ophthalmological services during the preschool age: ocular findings and family background. J Pediatr Ophthalmol Strabismus. 1978;15:253–258. doi: 10.3928/0191-3913-19780701-16. [DOI] [PubMed] [Google Scholar]
- 14.Ffooks OO. Dacryocystitis in infancy. Br J Ophthalmol. 1962;46:422–434. doi: 10.1136/bjo.46.7.422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cassady JV. Dacryocystitis of infancy. Am J Ophthalmol. 1948;31:773–780. [PubMed] [Google Scholar]
- 16.Kendig EL, Jr, Guerry D., III The incidence of congenital impatency of the nasolacrimal duct. J Pediatr. 1950;36:212. doi: 10.1016/s0022-3476(50)80206-8. [DOI] [PubMed] [Google Scholar]
- 17.Noda S, Hayasaka S, Setogawa T. Congenital nasolacrimal duct obstruction in Japanese infants: its incidence and treatment with massage. J Pediatr Ophthalmol Strabismus. 1991;28:20–22. [PubMed] [Google Scholar]
- 18.Dalgleish R. Incidence of idiopathic acquired obstructions in the lacrimal drainage apparatus. Br J Ophthalmol. 1964;48:373–376. doi: 10.1136/bjo.48.7.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harley RD, Stefanyszyn MA, Apt L, Nelson LB. Herpetic canalicular obstruction. Ophthalmic Surg. 1987;18:367–370. [PubMed] [Google Scholar]
- 20.McNab AA. Lacrimal canalicular obstruction associated with topical ocular medication. Aust N Z J Ophthalmol. 1998;26:219–223. doi: 10.1111/j.1442-9071.1998.tb01315.x. [DOI] [PubMed] [Google Scholar]
- 21.Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 1. Ophthal Plast Reconstr Surg. 1992;8:237–242. [PubMed] [Google Scholar]
- 22.Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 2. Ophthal Plast Reconstr Surg. 1992;8:243–249. [PubMed] [Google Scholar]
- 23.Bartley GB. Acquired lacrimal drainage obstruction: an etiologic classification system, case reports, and a review of the literature. Part 3. Ophthal Plast Reconstr Surg. 1993;9:11–26. [PubMed] [Google Scholar]
- 24.Wojno TH. Allergic lacrimal obstruction. Am J Ophthalmol. 1988;106:48–52. doi: 10.1016/s0002-9394(14)76387-1. [DOI] [PubMed] [Google Scholar]
- 25.Chapman KL, Bartley GB, Garrity JA, Gonnering RS. Lacrimal bypass surgery in patients with sarcoidosis. Am J Ophthalmol. 1999;127:443–446. doi: 10.1016/s0002-9394(98)00420-6. [DOI] [PubMed] [Google Scholar]
- 26.Bullen CL, Liesegang TJ, McDonald TJ, DeRemee RA. Ocular complications of Wegener’s granulomatosis. Ophthalmology. 1983;90:279–290. doi: 10.1016/s0161-6420(83)34574-7. [DOI] [PubMed] [Google Scholar]
- 27.Benger RS, Frueh BR. Lacrimal drainage obstruction from lacrimal sac infiltration by lymphocytic neoplasia. Am J Ophthalmol. 1986;101:242–245. doi: 10.1016/0002-9394(86)90603-3. [DOI] [PubMed] [Google Scholar]
- 28.Schoff EO, Hattenhauer MG, Ing HH, et al. Estimated incidence of open-angle glaucoma in Olmsted County, Minnesota. Ophthalmology. 2001;108:882–886. doi: 10.1016/s0161-6420(01)00550-4. [DOI] [PubMed] [Google Scholar]
- 29.Baratz KH, Gray DT, Hodge DO, et al. Cataract extraction rates in Olmsted County, Minnesota, 1980 through 1994. Arch Ophthalmol. 1997;115:1441–1446. doi: 10.1001/archopht.1997.01100160611015. [DOI] [PubMed] [Google Scholar]
- 30.Duke-Elder S, MacFaul PA. In: System of Ophthalmology. Duke-Elder S, editor. Vol. 8. London: Henry Kimpton Publishers; 1974. p. 700. [Google Scholar]
- 31.Groessl SA, Sires BS, Lemke BN. An anatomical basis for primary acquired nasolacrimal duct obstruction. Arch Ophthalmol. 1997;115:71–74. doi: 10.1001/archopht.1997.01100150073012. [DOI] [PubMed] [Google Scholar]
- 32.Minnesota Department of Health. Population estimates by region, county, cities over 100,000, age, and sex: Olmsted County. Minneapolis, MN: Minnesota Dept of Health; 1975. p. 8. [Google Scholar]
- 33.Minnesota Department of Health. Population estimates by region, county, cities over 100, 000, age, and sex: Olmsted County 2000. Minneapolis, MN: Minnesota Dept of Health; 2000. p. 121. [Google Scholar]
- 34.Marquis Who’s Who. The Official ABMS Directory of Board Certified Medical Specialists. 17. Vol. 2. Chicago: Marquis Who’s Who; 1976. [Google Scholar]
- 35.Marquis Who’s Who. The Official ABMS Directory of Board Certified Medical Specialists. 32. Vol. 2. New Providence, NJ: Marquis Who’s Who; 2000. [Google Scholar]
- 36.Coster DJ, Welham RA. Herpetic canalicular obstruction. Br J Ophthalmol. 1979;63:259–262. doi: 10.1136/bjo.63.4.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sanke RF, Welham RA. Lacrimal canalicular obstruction following chickenpox. Br J Ophthalmol. 1982;66:71–74. doi: 10.1136/bjo.66.1.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lass JH, Thoft RA, Dohlman CH. Idoxuridine-induced conjunctival cicatrization. Arch Ophthalmol. 1983;101:747–750. doi: 10.1001/archopht.1983.01040010747009. [DOI] [PubMed] [Google Scholar]
- 39.White WL, Bartley GB, Hawes MJ, Linberg JV, Leventer DB. Iatrogenic complications related to the use of Herrick lacrimal plugs. Ophthalmology. 2001;108:1835–1837. doi: 10.1016/s0161-6420(01)00718-7. [DOI] [PubMed] [Google Scholar]
- 40.Soparkar CN, Patrinely JR, Hunts J, et al. The perils of permanent punctal plugs. Am J Ophthalmol. 1997;123:120–121. doi: 10.1016/s0002-9394(14)71002-5. [DOI] [PubMed] [Google Scholar]
- 41.Annamalai S, Kumar NA, Madkour MB, Sivakumar S, Kubba H. An association between acquired epiphora and the signs and symptoms of chronic rhinosinusitis: a prospective case-control study. Am J Rhinol. 2003;17:111–114. [PubMed] [Google Scholar]
- 42.Bolger WE, Parsons DS, Mair EA, Kuhn FA. Lacrimal drainage system injury in functional endoscopic sinus surgery. Incidence, analysis, and prevention. Arch Otolaryngol Head Neck Surg. 1992;118:1179–1184. doi: 10.1001/archotol.1992.01880110047011. [DOI] [PubMed] [Google Scholar]
- 43.Gruss JS, Hurwitz JJ, Nik NA, Kassel EE. The pattern and incidence of nasolacrimal injury in naso-orbital-ethmoid fractures: the role of delayed assessment and dacryocystorhinostomy. Br J Plast Surg. 1985;38:116–121. doi: 10.1016/0007-1226(85)90098-0. [DOI] [PubMed] [Google Scholar]
- 44.Becelli R, Renzi G, Mannino G, Cerulli G, Iannetti G. Posttraumatic obstruction of lacrimal pathways: a retrospective analysis of 58 consecutive naso-orbitoethmoid fractures. J Craniofac Surg. 2004;15:29–33. doi: 10.1097/00001665-200401000-00011. [DOI] [PubMed] [Google Scholar]
- 45.Caravella LP, Jr, Burns JA, Zangmeister M. Punctal-canalicular stenosis related to systemic fluorouracil therapy. Arch Ophthalmol. 1981;99:284–286. doi: 10.1001/archopht.1981.03930010286013. [DOI] [PubMed] [Google Scholar]
- 46.Eiseman AS, Flanagan JC, Brooks AB, Mitchell EP, Pemberton CH. Ocular surface, ocular adnexal, and lacrimal complications associated with the use of systemic 5-fluorouracil. Ophthal Plast Reconstr Surg. 2003;19:216–224. doi: 10.1097/01.iop.0000066648.33513.3d. [DOI] [PubMed] [Google Scholar]
- 47.Linberg JV, McCormick SA. Primary acquired nasolacrimal duct obstruction. A clinicopathologic report and biopsy technique. Ophthalmology. 1986;93:1055–1063. doi: 10.1016/s0161-6420(86)33620-0. [DOI] [PubMed] [Google Scholar]
- 48.Kashkouli MB, Parvaresh M, Modarreszadeh M, Hashemi M, Beigi B. Factors affecting the success of external dacryocystorhinostomy. Orbit. 2003;22:247–255. doi: 10.1076/orbi.22.4.247.17255. [DOI] [PubMed] [Google Scholar]
- 49.Tsirbas A, Davis G, Wormald PJ. Mechanical endonasal dacryocystorhinostomy versus external dacryocystorhinostomy. Ophthal Plast Reconstr Surg. 2004;20:50–56. doi: 10.1097/01.IOP.0000103006.49679.23. [DOI] [PubMed] [Google Scholar]
- 50.Dolman PJ. Comparison of external dacryocystorhinostomy with nonlaser endonasal dacryocystorhinostomy. Ophthalmology. 2003;110:78–84. doi: 10.1016/s0161-6420(02)01452-5. [DOI] [PubMed] [Google Scholar]
- 51.Duffy MT. Advances in lacrimal surgery. Curr Opin Ophthalmol. 2000;11:352–356. doi: 10.1097/00055735-200010000-00011. [DOI] [PubMed] [Google Scholar]
- 52. [Accessed Dec 15, 2004];Publications of the Rochester Epidemiology Project. Available at: http://hsrwww.mayo.edu/epi/rep/REPbib.doc.
- 53.Melton LJ. History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–274. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 54. [Accessed Dec 5, 2004];Rochester Census: Profile of general demographic characteristics. Available at: http://govpubs.lib.umn.edu/census/profiles/390276820.pdf.
- 55.US Census Bureau. [Accessed Dec 17, 2004];People: race and ethnicity. http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=tp9_race_ethnicity.
- 56.US Census Bureau. [Accessed Dec 17, 2004];People: income and employment. Available at: http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=tp6_income_employment.
- 57.US Census Bureau: People: educationAvailable at: http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=tp5_educationAccessed Dec 17, 2004
- 58.US Census Bureau. People: aging. [Accessed Dec 17, 2004]; http://factfinder.census.gov/jsp/saff/SAFFInfo.jsp?_pageId=tp2_aging.
- 59.Esmaeli B, Hidaji L, Adinin RB, et al. Blockage of the lacrimal drainage apparatus as a side effect of docetaxel therapy. Cancer. 2003;98:504–507. doi: 10.1002/cncr.11527. [DOI] [PubMed] [Google Scholar]
- 60.Woog JJ, Kennedy RH, Custer PL, et al. Endonasal dacryocystorhinostomy: a report by the American Academy of Ophthalmology. Ophthalmology. 2001;108:2369–2377. doi: 10.1016/s0161-6420(01)00945-9. [DOI] [PubMed] [Google Scholar]
- 61.Couch SM, White WL. Endoscopically assisted balloon dacryoplasty treatment of incomplete nasolacrimal duct obstruction. Ophthalmology. 2004;111:585–589. doi: 10.1016/j.ophtha.2003.06.013. [DOI] [PubMed] [Google Scholar]