Abstract
Objective
The purpose of this study was to determine which spinal segment most closely corresponds to the level of the inferior angle of the scapula (IAS) using measurements taken on A-P full-spine radiographs.
Methods
Fifty sequentially selected radiographs were analyzed independently by two examiners. A straight edge was used to ascertain which spinal levels corresponded with the right and left IASs. For analysis, each spinal level was subdivided into three regions: upper vertebral body, lower vertebral body, and intervertebral space.
Results
he mean spinal level corresponding to the left IAS was midway between the T8–9 interspace and the upper T9 body (range, lower T7 to upper T10). The mean spinal level corresponding to the right IAS was slightly lower, but still within the upper T9 body (range, lower T7 to lower T10). These levels correspond to the T8 spinous process.
Conclusions
There is a considerable amount of variability in where the IASs are located, but most commonly, they correspond to the level of the upper body of T9.
Keywords: scapula, inferior angle, spinal segment, radiographs
Abstract
Objectif
L’objectif de la présente étude consistait à déterminer quel segment médullaire correspond le plus au niveau de l’angle inférieur de l’omoplate (IAS) en se servant des mesures relevées des radiogrammes A-P. du rachis intégral.
Méthodes
Cinquante radiogrammes sélectionnés d’une manière séquentielle ont été analysés indépendamment par deux examinateurs. Une règle à tracer a été utilisée pour établir quels niveaux rachidiens correspondaient aux IAS de la gauche et ceux de la droite. Aux fins d’analyse, chaque niveau rachidien a été subdivisé en trois régions : corps lombaire supérieur, corps lombaire inférieur et espace intervertébrale.
Résultats
Le niveau rachidien moyen correspondant à l’IAS de la gauche était mi-chemin entre l’inter-espace T8–9 et le corps T9 supérieur (plage, du T7 inférieur au T10 supérieur). Le niveau rachidien moyen correspondant à l’IAS de la droite était légèrement inférieur, cependant, toujours à l’intérieur du corps T9 supérieur (plage, du T7 inférieur au T10 inférieur). Ces niveaux correspondent à l’apophyse épineuse T8.
Conclusion
Il existe une variabilité significative là où se situent les IAS, mais plus couramment, ils correspondent au niveau du corps supérieur de T9.
Introduction
Musculoskeletal practitioners commonly use contiguous bony landmarks to locate spinal levels.1 One such landmark is the inferior angle of the scapula (IAS), which is said to correlate with the T7, T8, or T9 spinous process or spinal level, depending on the source.2–4 Gray’s Anatomy indicates that the IAS corresponds to the level of the ninth rib, which attaches to the spine at the T8–9 interspace.5 In another study on the location of the IAS, we provide a comprehensive list of citations, including many that suggest it lies at the level of the T7 spinous process.6 Some of this discrepancy is due to fact that some authors refer to the level of the spinous process, while others refer to the body of the vertebra. In spite of this inconsistency, no studies have attempted to determine as their primary goal which vertebral segment truly corresponds to the IAS.
Lewis et al.4 reported that manual palpation of surface landmarks is a valid method for determining the actual location of the scapula. Based on these findings, the authors opined that the location of thoracic landmarks could be accurately determined using surface palpation of scapular position as a reference point. On the other hand, several related studies have investigated the reliability of manual and physical therapists in locating spinal levels by palpation of spinous processes.7–10 Most found their procedures of low reliability. Thus, Lewis’ optimism notwithstanding, we are not confident that using the scapula position as a landmark would help in identifying segmental spinal levels by number.
Locating the precise spinal level by palpation is especially important to practitioners who intend to apply a specific therapy to a specific segment. However, anesthetists who attempted to identify a given lumbar interspace by palpation of spinous processes and iliac crests identified a level cephalad to their target in 33% to 68% of cases.11 Another study reported that the actual level, as determined by markers placed on patients’ backs prior to MRI, was from one space below to four spaces above the level identified by the anesthetist.12 Similar findings have been reported when physical therapists8 and spine surgeons13 were involved. Chiropractors, as well, are often interested in locating spinal levels by palpation and would benefit if a valid and reliable analytic method were available.
The purpose of the current study was to determine which spinal segment corresponds to the level of the IAS by means of measurements taken on retrospectively analyzed A-P full-spine radiographs that were taken with patients in an upright neutral posture.
Methods
Fifty-three radiographs were sequentially selected from the educational radiographic archives of a chiropractic college, consisting of several hundred films. Once a sufficient number of female radiographs were located, we selected only males, passing over approximately 10 radiographs of females, in order to include enough males so that the gender distribution would be approximately equal. All radiographs were A-P full-spine views that were taken with the patient standing erect, feet together, arms at the side, and the back touching a radiographic bucky. No identifying information was collected from the radiographs; only the above-mentioned measurements and subjects’ gender, age, and height.
Radiographs were retrospectively analyzed by two chiropractic students, each of whom had completed their training in radiographic interpretation. The radiographs were evaluated independently by each examiner in a blinded fashion. Any discrepancies between examiners were resolved by one or both of the study chiropractors.
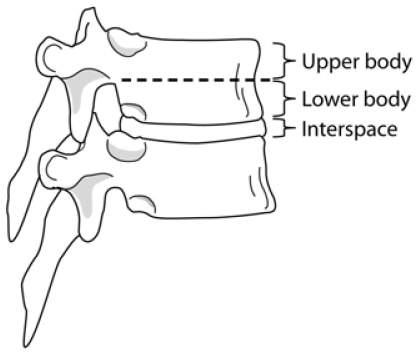
Each radiographic film was placed on a full-spine viewbox with the right edge evenly abutted to the right side of the viewbox cabinet. A T-square was positioned against the viewbox cabinet with the straight edge portion placed at the level of the lowest point of each subject’s IAS, first one side then the other. The examiners then ascertained which spinal level the straight edge passed through at the level of the right and left scapulae. For analysis, each evaluated spinal level was subdivided into three regions; upper vertebral body, lower vertebral body, and intersegmental region (e.g., between T7 and T8). When the demarcation between the upper and lower vertebral body was not obvious, the vertebral bodies were divided into upper and lower segments using a ruler to measure from the superior to inferior endplates to find the midpoint, which was marked with a small dot. (see Figure 1) Cobb angles14 were measured for subjects who appeared to have spinal curvature’s approaching 10 degrees. The data was entered into a Microsoft Excel spreadsheet and then exported to the Statistical Package for the Social Sciences (SPSS) for Windows (Version 12; SPSS, Inc, Chicago, Ill.). Data were analyzed using descriptive statistics including frequencies, percentages, mean/median, and standard deviation. Also, correlations were examined between age, height, gender, and the presence of scoliosis in relation to scapular position and vertebral level. Spinal levels were coded for easier statistical analysis with 1 representing the upper T6 body, 2 the lower T6 body, 3 the T6–7 interspace, and so on; continuing in sequence to 14 for the lower T10 body.
Figure 1.
Two thoracic vertebrae depicting the subdivisions that were used. Also, the typical degree of spinous process shingling in the mid-thoracic region.
This project was approved by the Institutional Review Board of the Palmer College of Chiropractic, Davenport, Iowa. Informed consent was not required from the included subjects because of the study’s retrospective nature, as well as the shared use of the radiographic library within the institution. Subjects’ names were protected and only de-identified information was gathered from the x-rays (e.g., age, gender, height, and weight).
Results
A total of 53 radiographs were selected, although 3 were ultimately excluded because of poor imaging technique precluding analysis. There were 25 males and 24 females, with gender information missing for 1 radiograph. The mean (SD) age was 47.5 (15.4) years and the mean height was 168.5 (12.0) cm. There were no disagreements between examiners as to the spinal level reported in association with the IAS.
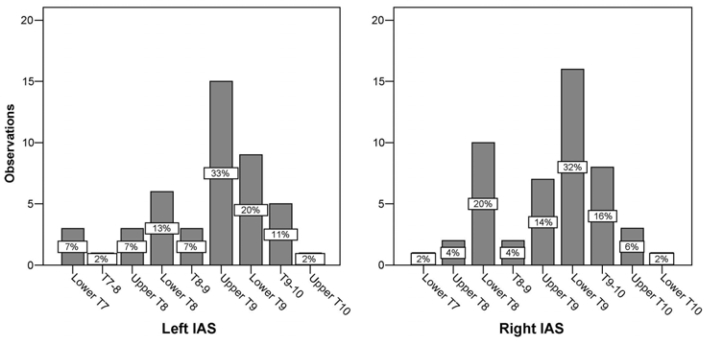
The mean spinal level corresponding to the left IAS was midway between the T8/9 interspace and the upper body of T9. This corresponded to the T8 spinous process. The range was from lower T7 to upper T10. The median value was upper T9, which was also the mode, the most common position of the IAS, accounting for 33% of the observations.
The mean spinal level corresponding to the right IAS was approximately at the level of the upper body of T9, and T8 spinous process. The range was from lower T7 to lower T10. The median and mode on the right both corresponded to lower T9, which comprised 32% of the observations for that side. Figure 2 shows the distribution of instances of vertebral levels corresponding to the left and right IASs.
Figure 2.
Frequencies of spinal levels associated with the left and right inferior angle of the scapula (IAS).
Slight differences were apparent between males and females that are presented in Table 1. Most notably, the IAS was positioned slightly lower bilaterally on males by approximately one-quarter of a vertebral body.
Table 1.
Spinal levels corresponding to the inferior angle of the scapula for the intact group, males, and females.
| n | Mean | Range | |
|---|---|---|---|
| Intact group | |||
| Left | 44 | Between T8/9 and Upper T9 | Lower T7-Upper T10 |
| Right | 48 | Lower T9 | Lower T7-Lower T10 |
| Males | |||
| Left | 22 | Upper T9 | Lower T7-Upper T10 |
| Right | 24 | Lower T9 | Lower T7-Upper T10 |
| Females | |||
| Left | 22 | T8/9 | Lower T7-T9/10 |
| Right | 24 | Upper T9 | Upper T8-Lower T10 |
Only 1 radiograph depicted thoracic scoliosis greater than 10 degrees, determined to be 15° by the Cobb method.14 The scapulae were positioned at the level of upper T9 on the left and lower T8 on the right in this case. The left scapulae were not observable on 4 of the radiographs because they were obscured by the superimposed heart shadow; as a result, the related data did not figure in the analysis.
Discussion
This study demonstrates that there is a considerable amount of variability in where the IASs are located. They are most commonly found at the level of the upper body of T9 on the left and the lower body of T9 on the right; corresponding most closely to the T8 spinous process. This finding, which was determined using a retrospective study design, is consistent with our earlier prospective study that utilized an entirely different methodology.6
The range for IAS position is rather wide, spanning T7 to T10, suggesting that patient variations in scapular position would refute any simplistic association of the scapular tip with a specific vertebral level. The right scapula was in a lower position more frequently, possibly due to handedness.15 According to Kendall et al,15 patients typically maintain a posture wherein the lower shoulder is on the side of the dominant hand.
The mid-thoracic spinous processes are nearly vertical, directed obliquely downward5 and extending to the interspace of the segment below. A cadaveric study of 12 thoracic spines from T5 through T8 reported that the length of spinous processes was variable, ranging from 2.6 to 4.5 cm, with a mean value of 3.5 cm.16 Thus, the spinous process completely spans an entire vertebral body; e.g., lower body of T8 corresponds to the T7 spinous process. (see Figure 1) Therefore, when the IAS is found parallel to the body of a given vertebra it is also parallel to the tip of the spinous process of the vertebra above.
The interexaminer reliability of identifying spinous processes has been reported to be poor, with errors ranging up to 177.1 mm in the thoracic spine. Therefore, in addition to the problem posed by the IAS lying in a somewhat wide range, it is likely that examiner error further compounds the difficulty a musculoskeletal practitioner would have in accurately locating a particular spinal segment using the IAS as a landmark
Our findings should be of interest to clinicians who use the scapula as a landmark for locating other anatomical structures, such as vertebral levels. Such clinicians include chiropractors, osteopaths, physical therapists, orthopedists, neurologists, anesthetists, surgeons, nurses, discographers, and others.
Although this study did not investigate the validity of attempting to identify subluxations or other aspects of spinal dysfunction radiographically, it is common practice among chiropractors to take radiographs to identify potential segments or areas deemed worthy of adjustive care. The present study suggests it may be very challenging to situate areas of radiographic interest on the actual patient, at least in the thoracic spine, if the scapula is to be used as a landmark for identifying spinal levels.
The following factors may have an influence on the accuracy of locating a spinal level seen on a radiograph on an actual patient:
The scapular tip varies in location from patient to patient, exhibiting a rather wide range.
The scapular tip tends to be lower on the side of the dominant upper extremity.
The scapular tip may line up with different levels in the standing patient as compared with the prone patient, so that spinal levels identified in relation to the scapula in an upright radiograph may change relative to the scapula if the patient is placed prone or supine for the purposes of an adjustive procedure.
There may be examiner error.
Since the rule of thumb most used in chiropractic and elsewhere has been that the inferior scapular tip lies at the spinous process of T7, whereas it is actually closer to T8, then any spinal landmark located starting from this apparently erroneous landmark is likely to be phase-shifted on average by about one vertebral level, winding up one level below what was intended. Moreover, patient anatomical variation is such that even “correcting” the rule of thumb would at best direct the chiropractor to a 3 level spinal region that probably contains the level seen on the radiograph, not the point location that is generally desired.
To the extent chiropractors have been using the standing T7 spinous process = scapular tip benchmark, and the prone T6 spinous process = scapular tip benchmark rules for finding thoracic locations, they have not been introducing forces where they thought they were. Consistently being one vertebra below the target suggested by radiography results in systematic bias, while not taking into account that the scapular tip lies within an anatomical range rather than a single place introduces random error. Accordingly, clinicians who believe segmental specificity remains clinically important and thus take radiographs to identify adjustable segments will have to explain their claimed good results in some other way, since they have been treating the putatively wrong level much of the time.
The sources of error we highlight are not entirely insuperable. We believe a clinician could improve his or her accuracy by simply revising the traditional spinal landmark rule of thumb, and look for the scapular tip to be on average one level lower than previously thought. Even more importantly, provided the scapula tip may be visualized on the radiograph (collimation may prevent this), the clinician need not presume what spinal level corresponds to the scapular tip. That information may be directly visualized. Even at that, the chiropractor would still have to determine how that landmark changes going from the standing to the prone position or seated position.
Since the radiographic beam in a full spine radiograph penetrates the IAS in an inferior to superior direction, we calculated the extent to which radiographic distortion may have influenced our findings, which is illustrated in Figure 3. Using these figures, we calculated that the IAS lies approximately one-half cm lower than reported herein, which corresponds to approximately one-quarter of a typical T9 vertebral body.17
Figure 3.
Because of radiographic image distortion, the actual vertebral level corresponding to the IAS is approximately one-half cm lower than reported herein. The illustration is not to scale.
Footnotes
Funding sources and conflicts of interest
None.
References
- 1.Najm WI, Seffinger MA, Mishra SI, et al. Content validity of manual spinal palpatory exams – A systematic review. BMC Complement Altern Med. 2003;3:1. doi: 10.1186/1472-6882-3-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellis H. Clinical anatomy: a revision and applied anatomy for clinical students. 10. Oxford, UK; Malden, MA: Blackwell Science; 2002. [Google Scholar]
- 3.Oatis CA. Kinesiology: the mechanics and pathomechanics of human movement. 1. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 4.Lewis J, Green A, Reichard Z, Wright C. Scapular position: the validity of skin surface palpation. Man Ther. 2002;7:26–30. doi: 10.1054/math.2001.0405. [DOI] [PubMed] [Google Scholar]
- 5.Gray H. Anatomy of the Human Body. Philadelphia: Lea & Febiger; 1918. Bartleby.com, 2000. [Google Scholar]
- 6.Cooperstein R, Haneline M. Identification of thoracic spinal levels by palpation versus an x-ray gold standard. Journal of Chiropractic Medicine In press. [Google Scholar]
- 7.Binkley J, Stratford PW, Gill C. Interrater reliability of lumbar accessory motion mobility testing. Phys Ther. 1995;75:786–792. 793–795. doi: 10.1093/ptj/75.9.786. [DOI] [PubMed] [Google Scholar]
- 8.Downey BJ, Taylor NF, Niere KR. Manipulative physiotherapists can reliably palpate nominated lumbar spinal levels. Man Ther. 1999;4:151–156. doi: 10.1054/math.1999.0196. [DOI] [PubMed] [Google Scholar]
- 9.McKenzie AM, Taylor NF. Can physiotherapists locate lumbar spinal levels. Physiotherapy. 1997;83:235–239. [Google Scholar]
- 10.Billis EV, Foster NE, Wright CC. Reproducibility and repeatability: errors of three groups of physiotherapists in locating spinal levels by palpation. Man Ther. 2003;8:223–232. doi: 10.1016/s1356-689x(03)00017-1. [DOI] [PubMed] [Google Scholar]
- 11.Lirk P, Messner H, Deibl M, et al. Accuracy in estimating the correct intervertebral space level during lumbar, thoracic and cervical epidural anaesthesia. Acta Anaesthesiologica Scandinavica. 2004;48:347–349. doi: 10.1111/j.0001-5172.2004.0315.x. [DOI] [PubMed] [Google Scholar]
- 12.Broadbent CR, Maxwell WB, Ferrie R, Wilson DJ, Gawne-Cain M, Russell R. Ability of anaesthetists to identify a marked lumbar interspace. Anaesthesia. 2000;55:1122–1126. doi: 10.1046/j.1365-2044.2000.01547-4.x. [DOI] [PubMed] [Google Scholar]
- 13.Ebraheim NA, Inzerillo C, Xu R. Are anatomic landmarks reliable in determination of fusion level in posterolateral lumbar fusion? Spine. 1999;24:973–974. doi: 10.1097/00007632-199905150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg MS, Poitras B, Mayo NE, Labelle H, Bourassa R, Cloutier R. Observer variation in assessing spinal curvature and skeletal development in adolescent idiopathic scoliosis. Spine. 1988;13:1371–1377. doi: 10.1097/00007632-198812000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Sobush DC, Simoneau GG, Dietz KE, Levene JA, Grossman RE, Smith WB. The lennie test for measuring scapular position in healthy young adult females: a reliability and validity study. J Orthop Sports Phys Ther. 1996;23:39–50. doi: 10.2519/jospt.1996.23.1.39. [DOI] [PubMed] [Google Scholar]
- 16.Sran MM, Khan KM, Zhu Q, McKay HA, Oxland TR. Failure characteristics of the thoracic spine with a posteroanterior load: investigating the safety of spinal mobilization. Spine. 2004;29:2382–2388. doi: 10.1097/01.brs.0000143110.59837.f2. [DOI] [PubMed] [Google Scholar]
- 17.Panjabi MM, Takata K, Goel V, et al. Thoracic human vertebrae. Quantitative three-dimensional anatomy. Spine. 1991;16:888–901. doi: 10.1097/00007632-199108000-00006. [DOI] [PubMed] [Google Scholar]