How did the study come out?
Électricité de France-Gaz de France (EDF-GDF) is the only utility firm in France involved in production, transmission and distribution of energy. For several reasons, EDF-GDF is a unique setting for epidemiology. The company employs about 150,000 workers in all regions of France, from large cities to small villages; there is a wide socioeconomic range of occupational positions, including white and blue-collars workers. The workforce is very stable due to their civil servant-like status, employees almost never leave the company and are not lost to follow-up even after retirement, since retirement benefits are paid by the company itself. An extensive human resources system allows for a complete follow-up of the workers, even when they retire. EDF-GDF has its own Occupational Health and Social Security system; about 300 physicians work for the company and are responsible for the health surveillance of the workers.
During the seventies the medical department of EDF-GDF decided to build a comprehensive data base on the health of the workforce. The data base was designed in close collaboration with researchers at INSERM - the French National Institute for Health and Medical Research - Research Unit 88, directed at that time by one of us who was also a Scientific advisor for the medical department of the company (MG). The data base contained demographic, socioeconomic and professional data on each worker. An exhaustive register of sick leave, accidents, permanent disabilities, compensated diseases, causes of death, cancer and coronary heart disease incidence among active workers was created. Further, a job-exposure matrix was established for 30 potentially carcinogenic agents1,2. Using these data bases several epidemiological studies on working accidents, sick leave, cancer and mortality were carried out3–8. However the absence of individual level data on lifestyle, self-reported health conditions and the social environment limited the ability to study numerous research questions in depth. With the aim of overcoming some of these shortcomings, researchers at INSERM designed a new project to develop a longitudinal cohort made of a sample of volunteer EDF-GDF workers: the GAZEL Cohort Study (GAZEL stands for GAZ and ELectricité).
The management, the unions and the medical department of EDF-GDF gave their consent to the project, and the company accepted to provide regular access to all personal and health data files. EDF-GDF and the worker’s social activities organization decided to fund INSERM Unit 88 for the major part of the GAZEL Cohort Study costs on a regular basis; regular funding came also from INSERM Unit 88’s own budget, and specific funding for the setting up of a biobank came from private foundations (Fondation de France and Association pour la recherche sur le cancer). These resources allow only for the basic functioning of the cohort and all specific research projects must find their own additional funding.
The GAZEL Cohort Study was launched in January 1989. INSERM Unit 88 (now Unit 687: Public Health and Epidemiology of Occupational and Social Determinants of Health) manages the project and has had full responsibility for it since the beginning, without any interference from the company in relation to the scientific work or publication of results.
What does it cover, and how has this changed?
Designed as a research tool, the GAZEL Cohort Study was intended to facilitate epidemiological research on various diseases and multiple health-related factors. The GAZEL cohort is an “open and general-purpose epidemiological laboratory” and was not designed to study a specific issue. The project relies on a long-term follow-up of the cohort, which includes systematic and prospective collection of various data from different sources. These data are available to investigators conducting research on the cohort and they also have the possibility of collecting additional data to suit their research needs.
Over the years, the GAZEL Cohort Study has evolved to include many sub-studies which aim to examine a specific research question. These projects are focused on various physical and mental health outcomes and on many different determinants, especially occupational factors. As the cohort is ageing (mean age in 2006: 63 and 60 for men and women respectively), and as most of the subjects are retired, new research projects are increasingly on various determinants of health in early old age, taking advantage of the large amount of data collected prospectively from baseline. This almost unique feature of GAZEL allows an examination of the determinants of various physical and functional aspects of ageing earlier in life than in most of the ageing cohorts.
Who is in the sample?
In January 1989, after an information campaign in the company and union newsletters, an invitation to participate in the cohort on a voluntary basis was sent to all male employees then aged 40 to 50 years and all women then between 35 and 50 years old. The invitation did not mention diseases or specific risk factors, but simply proposed participation in a long-term health study to help medical research.
At baseline, the GAZEL cohort comprised 20,624 individuals: 15,010 men aged 40– 50 years in 1989, and 5,614 women aged 35–50 years. Table 1 presents the main socioeconomic characteristics of the sample and the distribution of some lifestyle and health-related variables at baseline, and shows that this cohort experienced a high upward occupational mobility over time. As they have aged, the vast majority of the workers of the cohort have retired, 91.7% men and 66.7% women by the end of 2005. Less than 5% of the cohort has died, 861 men and 155 women by the end of 2005.
Table 1.
The GAZEL cohort: main socioeconomic, lifestyle and health-related characteristics at baseline
| Men | Women | ||||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Birth year | 1939–1943 | 6356 | 42.3 | 1379 | 24.6 |
| 1944–1948 | 8654 | 57.7 | 2037 | 36.3 | |
| 1949–1953 | --- | --- | 2198 | 39.2 | |
| Gender | Men | 15010 | 100.0 | ||
| Women | 5614 | 100.0 | |||
| SES at hiring | Executive | 1412 | 9.4 | 231 | 4.1 |
| Middle | 1329 | 8.9 | 357 | 6.4 | |
| Non manual | 3203 | 21.4 | 4961 | 88.5 | |
| Manual | 9052 | 60.4 | 55 | 1.0 | |
| SES at 35 | Executive | 2341 | 16.1 | 307 | 5.8 |
| Middle | 8149 | 56.2 | 2763 | 52.6 | |
| Non manual | 920 | 6.3 | 2143 | 40.8 | |
| Manual | 3095 | 21.3 | 37 | 0.7 | |
| SES at baseline | Executive | 4285 | 28.6 | 432 | 7.7 |
| Middle | 8277 | 55.2 | 3510 | 62.6 | |
| Non manual | 633 | 4.2 | 1625 | 29.0 | |
| Manual | 1799 | 12.0 | 36 | 0.6 | |
| Tobacco at baseline | Smoker | 4632 | 31.0 | 1200 | 24.6 |
| Non smoker | 5087 | 34.1 | 3672 | 75.4 | |
| Ex smoker | 5204 | 34.9 | 654 | 11.8 | |
| Alcohol at baseline | Abstinent | 293 | 2.0 | 258 | 4.6 |
| Occasional | 7370 | 49.1 | 4205 | 74.9 | |
| Light | 2444 | 16.3 | 443 | 7.9 | |
| Moderate | 2754 | 18.3 | 441 | 7.9 | |
| Heavy | 1848 | 12.3 | 132 | 2.4 | |
| Other | 301 | 2.0 | 135 | 2.4 | |
| BMI at baselinea | Low | 2709 | 19.1 | 1760 | 33.6 |
| Average | 8034 | 56.6 | 2932 | 56.0 | |
| High | 3443 | 24.3 | 540 | 10.3 | |
| Self-rated health at baselineb | 1–3 | 10433 | 70.1 | 3671 | 66.4 |
| 4–5 | 3755 | 25.2 | 1582 | 28.6 | |
| 6–8 | 691 | 4.6 | 272 | 4.9 | |
| Self reported diseases at baselinec | 0 | 3219 | 21.4 | 943 | 16.8 |
| 1–2 | 7730 | 51.5 | 2556 | 45.5 | |
| 3–5 | 3662 | 24.4 | 1693 | 30.2 | |
| 6–10 | 399 | 2.7 | 422 | 7.5 | |
Low: <20; Average: 20–25; High: >25
On a 1–8 scale
Among a predefined list
We have analyzed factors associated with participation for the entire target population.9 Higher participation was associated with being male, married, having children, managerial status, and residence in particular regions. Among men, lower participation was associated with sick leave in the year before recruitment into the cohort. During follow-up, participation was negatively associated with several diseases, especially those associated with alcohol consumption. The risk of upper respiratory and digestive tract and lung cancer during follow-up was higher among non-participants. The same occurred among women, but less markedly, for cancers of the breast and genital organs. During follow-up, mortality among men was higher among non-participants, especially for alcohol-related diseases. The association among women was less strong. Among men but not women, diseases related to alcohol, smoking, or risky behaviours were the primary cause of health differences observed between participants and non-participants9.
How often have they been followed-up?
Follow-up is continuous and includes data collection on health status, lifestyle, and socioeconomic and occupational factors from various sources. A postal questionnaire is sent to the participants each year, and data are extracted regularly from the files of the personnel and medical departments of EDF-GDF and from national registers. Participants were invited in 1999–2000 to a health clinic where medical and biological data were collected; we plan to invite them again in 2008 and 2011.
What has been measured?
Socio-demographic, lifestyle and psychosocial_data
Socio-demographics
Occupational position is known from two sources: company records and self-reports. Other measures include education, personal and household income, marital status, subjective socioeconomic status (SES), spouse’s SES, father’s SES, composition of the household, and type of housing.
Health behaviours assessed are alcohol consumption using a validated questionnaire on drinking habits10, the Cage alcoholism screening questionnaire11, smoking, dietary habits using a diet diary, and physical activity. The measures of smoking include age when started smoking, age when stopped for those who have stopped, and the number of cigarettes (or pipes, cigarillos, cigars) smoked every day, allowing the calculation of pack years of smoking.
Psychosocial data include measures of life events, social support and network12, relationship with partner, social and leisure activities, early life events, and socially productive activities assessed using measures of frequencies and motivations behind socially productive activities in early old age (SHARE questionnaire).
Personality profile
Type A Behavior13, self-esteem14, and the Buss and Durkee Hostility Inventory15 were introduced in 1993. The French versions of these scales have been validated16.
Major occupational exposures
Job history: a complete job history for each subject including a detailed characterization of each position (precise specific codes for occupation and activity sector, dates of beginning and end) were extracted from company files.
Job strain was assessed using the Karasek ‘job strain’17 and the Siegrist ‘effort-reward imbalance’ (ERI) measures18. The French versions were validated19,20 and introduced to the study in 1995 and repeated in 1997 and 1999 (Karasek) and in 1998 (ERI).
Other working conditions: self-reported data on various working conditions were collected through questionnaires over the years of follow-up: exposure to noise, extreme temperatures, and various constraints (working hours, computer work, and risky situations).
Ergonomic strain was assessed through questionnaire at different waves of follow-up for a subsample and is planned for the whole cohort in 2007. Ten specific aspects were considered: handling of heavy loads, bending and twisting, driving, kneeling, climbing stairs, climbing on ladders, working arms above the shoulders, handling loads on the shoulder, use of vibrating tools, heavy physical work. We also plan to develop a job exposure matrix for these factors.
Chemical exposure was assessed through a job-exposure matrix (JEM) specific to EDF-GDF21. This matrix is based on the entire period of employment and takes into account the evolution over time in jobs. The chemicals included in the JEM are asbestos, coal tar, crystalline silica, cadmium compounds, chromium compounds coal gasification, man made mineral fibres, mechanical oils, non-refined or moderately-refined oils, herbicides-pesticides, hydrazine, creosotes, chlorinated solvents, polyester resins, PCB, polyurethane resins, epoxy resins, benzene and other aromatic solvents, petroleum solvents, toluylene diisocyanate. Additionally, a JEM specific to Extremely Low Frequency Electric and Magnetic Fields was also constructed22. Overall, there were a large number of subjects who experienced different types of occupational exposure during their career (Table 2).
Table 2.
Career-long exposure to occupational factors among the GAZEL Cohort participants
| Occupational exposure | Men | Women |
|---|---|---|
| Ever exposed to chemicals (JEM assessment, no missing data) | 9,237 | 77 |
| ≥ 2 postural constraints reported in 1989, 1990 or 1994 (estimates from individual data)a | 8,775–10,664 | 1,781–3,088 |
| Psychosocial constraints reported in 1995, 1997 or 1999 (estimates from individual data)a | 2,892–7,753 | 1,019–3,410 |
| All types of exposure | 1,257–4,016 | 6–37 |
| No exposure at all | 1,080–2,266 | 1,006–2,814 |
Postural and psychosocial constraints: estimation from self-reported conditions; for non response (retirees, non respondents of that year) we hypothesized that all were exposed (upper range) or that nobody was exposed (lower range).
Outcomes
Mortality
Vital status and cause of death has been obtained annually. Vital status data come from the EDF-GDF itself as it pays out retirement benefits. Cause of death, currently available up to 2003, is obtained from the French National Death Index. From 1989 to the end of 2003, 827 deaths have occurred among GAZEL participants. For 25 of them (3%), data on the cause of death were missing, due to death outside France; in the other 802 deaths, causes were available for 795 (99%).
Morbidity
Health data are collected through multiple sources: self-reports of diseases and standardized scales through the annual questionnaire, physician diagnoses, morbidity registers, health examinations, and linkages to national data bases (claims for medical benefits, hospitals discharge).
Self-reported specific diseases
Prevalent and incident diseases and those for which they are receiving medical treatment are reported by participants through a check-list of diseases included in the annual questionnaire. The validity of this method was examined by comparing it to data from medical sources and was found to be sound23.
Sickness absence
Episodes of sickness absence, available from 1978 onwards, are extracted from the data base of the EDF-GDF medical department. They include the date, the length, and the medical cause of the sick leave spells verified by a company physician and coded using the ICD classification (ICD-8 in 1978, ICD-9 from 1979 to 1999, ICD-10 since 2000).
Depression using the validated French version of the Center for Epidemiologic Studies –Depression scale (CES-D)24 and the Mini International Neuropsychiatric Interview (MINI) on a subsample25.
Health function using the French validated versions of the Nottingham Health Profile (NHP) 26, of the Short-Form 36 (SF-36)27, the CASP 1928 and the Activities of Daily Life (ADL) questionnaire29.
Musculoskeletal disorders were assessed using the French version of the Nordic questionnaire30.
Respiratory disease was assessed using the ECRHS (European Community Respiratory Health Survey), questionnaire in 200331.
Incidence of serious diseases
The EDF-GDF medical department runs registers for cancer and coronary heart disease during the period of employment of each employee. Both registers have been validated for accuracy and completeness32,33. When subjects retire they are no longer covered by these registers and other procedures are used to follow the incidence of these diseases and others serious medical conditions. Multiple sources of data are used: self-reports of subjects, exhaustive detailed data on health care extracted from social security files (visit to doctors and other health professional including their identification, drugs and other medical supplies used, including the name of the drugs), claims for serious diseases, and telephone calls to attending physicians for diagnosis validation.
Clinical screening
In 1999–2000 almost half of the cohort participants visited a health clinic where medical data were collected: blood pressure, waist hip ratio, height and weight and body mass index (BMI); for subjects aged 55 and more, some simple measures of cognitive and physical function were also taken and we plan to measure these in greater detail in new waves of data collection in 2008 and 2011 in order to provide a comprehensive assessment of functional status in early old age.
Biological measures
Stored serum and plasma are available from blood samples collected in 1999–2000. At that time, fasting blood samples were collected from 4,656 GAZEL participants. Venous blood samples (55 ml) were collected by venipuncture into Vacutainer tubes after an overnight fast. In the biobank archive, samples were stored at −196°C in liquid nitrogen. All the samples were divided into two replicates, each composed of 8 aliquots of serum; 4 aliquots of lithium heparin plasma; 4 aliquots of EDTA K3 plasma; 3 aliquots of natrium citrate plasma; and 5 aliquots of buffy coat. We plan to collect again blood samples data in 2008.
Overview of measures
Table 3 summarizes the main measures that are collected, with the source(s) and year(s) of data collection.
Table 3.
GAZEL table of main variables
| Source† | 1988 | 1989 | 1990 | 1991 | 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sociodemographic data | |||||||||||||||||||||
| Education | SR&CR | x | x | x | x | x | x | x | x | x | x | x | x | ||||||||
| Number of people in household | SR&CR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Neighbourhood | SR | x | x | x | |||||||||||||||||
| Household income & assets | SR | x | x | ||||||||||||||||||
| Subjective socioeconomic status | SR | x | |||||||||||||||||||
| Health | |||||||||||||||||||||
| Death & cause of death | CR & CepiDc | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Self-reported specific diseases | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Sickness absence | CR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Cancer & CHD registers | CR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Self rated health | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| CES-D | SR | x | x | x | x | ||||||||||||||||
| Nottingham Health Profile (NHP) | SR | x | x | x | x | ||||||||||||||||
| SF-36 | SR | x | x | ||||||||||||||||||
| CASP 19 | SR | x | |||||||||||||||||||
| Activities of daily life | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||
| Health behaviours | |||||||||||||||||||||
| Nutrition | SR | x | x | x | |||||||||||||||||
| Alcohol consumption | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Physical activity | SR | x | x | x | x | x | |||||||||||||||
| Tobacco | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Occupational data | |||||||||||||||||||||
| Job history | CR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | |
| Psychosocial factors | SR | x | x | x | x | ||||||||||||||||
| Chemical exposure | CR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
| Ergonomic exposure | SR | x | x | x | x | x | x | x | x | ||||||||||||
| Psychosocial data | x | ||||||||||||||||||||
| Major life events | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | x | ||||
| Social support & network | SR | x | x | x | |||||||||||||||||
| Personality profile | SR | x | |||||||||||||||||||
| Social & leisure activities | SR | x | x | x | x | x | x | x | x | x | x | x | x | x | x |
SR: Self Reported, CR: Company Records, CepiDc: French national death index
What is attrition like?
Two principal types of attrition must be distinguished: (i) loss to follow-up, and (ii) dropping out, i.e., participants who no longer want to participate in the data collection.
The GAZEL cohort is characterized by a very low loss to follow-up. Members of the cohort are followed and data are collected from medical and non-medical sources even if they do not complete their annual self-administered questionnaire. Only 126 subjects (0.6%) were lost to follow-up during the first 17 years of follow-up (1989–2005).
Dropouts are participants who do not complete their annual questionnaire. After a fall during the first 5 years of follow-up, almost 75% of the questionnaires are now returned every year (Figure 1). As it is not always the same people who fail to respond each year, only 3.2% of the initial cohort never sent back any questionnaires during the 1989–2005 period.
Figure 1.
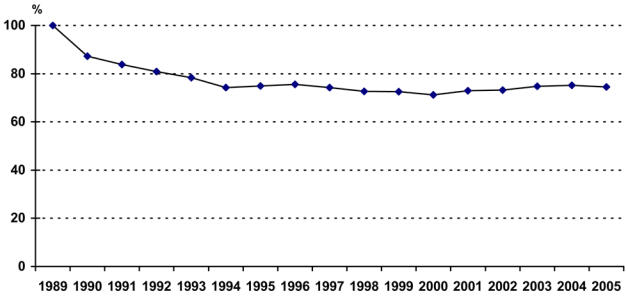
Annual response rate to mailed questionnaires
We examined socioeconomic, behavioural and health factors associated with response to annual questionnaires during an eleven year period of follow-up.34 Higher response rates were associated with gender (male), age (older), managerial status and retirement. Smoking and alcohol drinking at baseline was associated with lower participation. Subjects who had at least 3 sick-leaves during the two years preceding or following the questionnaire were less likely to respond, especially for absence for psychiatric and alcohol-related diseases among men. Those who had rated their health as poor at baseline were less prone to respond during follow-up. Attrition was associated with cancer and coronary heart disease for men. Finally, most variables that predicted initial participation were associated with continued participation. Health problems strongly predicted attrition, while socioeconomic factors played a weaker role34.
What has it found? Key findings and key publications
Findings from GAZEL are focused on various physical and mental health conditions and on many different determinants: effects of occupational psychosocial and ergonomic factors on various outcomes (mainly musculoskeletal disorders, psychiatric diseases and cardiovascular health), sickness absence, determinants of the social gradient of health, traffic accidents, women’s health, social determinants of alcohol drinking and of cardiovascular risk factors, treatments and health care. Cross national comparative studies of social gradients of health and of the prevalence of occupational psychosocial factors were also performed. Efforts have been made to analyse methodological problems related to the validity of the study: factors associated with selection of the cohort at inception and with attrition during the follow-up, validity of self-reported chronic conditions.
Work and health
Regarding ergonomic exposures, individual and occupational predictors of sciatica were investigated. Comparing the risk factors for sciatica and those for low back pain without sciatica, it appeared that height and driving were predictors only for sciatica, and bending forward and backward at work was a predictor only for low back pain without sciatica35. With regard to job strain, the relationship between psychosocial factors at work and changes in depressive symptoms was examined taking into account personality traits. In men, high decision latitude was predictive of a decrease in the CES-D scores. In both genders, high job demands and low social support at work were predictive of increased scores, regardless of personality traits and covariates36. Effort-Reward-Imbalance was a significant predictor of poor self-reported health for men and women. For both genders, effort did not predict self-reported health, but reward did. Over commitment was predictive of poor self-reported health for men only37. Looking at data on chemical exposures with the job matrix, we found that subjects whose cumulative exposure to solvents was above the 90th percentile had an elevated risk for cognitive impairment measured through MMSE and the Digit Symbol Substitution from the Wechsler Adult Intelligence Scale-Revised. The risk was increased in workers with the highest estimated cumulative exposure to chlorinated solvents and to the four types of chlorates studied, to petroleum solvents but also to benzene38.
Sickness Absence
There is an occupational gradient in sickness absence in GAZEL. The analysis of the respective contribution of stress-related and physical work factors to occupational class disparities in sickness absence shows that work characteristics account for 19% (women) and 21% (men) of all absences. Physical work conditions accounted for 42% and 13% of absences for musculoskeletal reasons, and work stress accounted for 48% and 40% of psychiatric absences39. Whether psychosocial work characteristics and social relations exert independent effects on the incidence of sickness absence was also studied. Among men and women, levels of decision latitude and personal social support below the median predicted 17% to 24% increases in absence rates. Low satisfaction with social relations and low social support at work lead to a 10% to 26% excess in sick leaves among men.40.
The social gradient of health: GAZEL and cross national comparative studies
We examined the association between occupational class, occupational mobility and cancer incidence. Male clerks and manual workers were at high risk, particularly from smoking and alcohol-related cancers. Adjusting for specific health behaviours and other cancer risk factors reduced this gradient41. Relative risk of dying during follow-up (1993–1999) for men who were the least socially integrated compared to the most socially integrated was 2.7. Isolated men and women had elevated risks of dying from cancer and from accidents and suicide42. A lack of social support and dissatisfaction with social relations was predictive of poor health status; low social support was an independent risk factor for poor health in men and women: for men the effect was strongest among individuals who held a high occupational status, for women among those in high and low occupational groups. This study suggested that social relations exert an independent effect on health, modified by gender and socio-economic factors43.
The social gradient in morbidity and risk factors that might explain it was compared to that in the Whitehall II study. Strong social gradients in long spells of sickness absence and self-reported health were observed in both cohorts. Health behaviours showed different relations with socioeconomic position in the two samples. Psychosocial work characteristics showed strong gradients in both cohorts. Cohort-specific significant risk factors explained between 12% and 56% of the gradient in sickness absence and self-reported health suggesting that some common susceptibility may underlie the social gradient in health and disease, which explains why inequalities occur in cultures with different patterns of morbidity and mortality44. The determinants of self rated health in the Whitehall II study and the GAZEL cohort study were investigated in men and women. Five determinants were identified (symptom score, sickness absence, longstanding illness, minor psychiatric morbidity, number of recurring health problems) in Whitehall II, explaining 34.7% of the variance in self rated health. In GAZEL, four measures (physical tiredness, number of health problems in the past year, physical mobility, number of prescription drugs used) explained 41.4% of the variance45.
Traffic accidents
The risk for serious road traffic accidents was found to be higher in individuals with type A behaviour pattern, but not in those with hostility personality traits46. Marital separation or divorce was associated with an increased risk of a serious accident47. Self assessed driving while sleepy was a powerful predictor of serious road traffic accidents, suggesting that drivers’ awareness of their sleepiness while driving is not sufficient to prevent them from having accidents48.
Determinants of alcohol consumption
Self-perception of bad health, consumption of sleeping pills and unmarried status were predictive of the cessation of alcohol consumption. Working under favourable conditions and being a non-smoker tended to be associated with reduced consumption. Increased consumption was associated with the number of reported diseases and the smoking status. Among abstainers or light daily drinkers, being exposed to more than one work constraint increased the risk of higher consumption. Among women divorcees and widows drank less than the married. Women in the oldest generation drank more than the younger women. Getting married was accompanied by an increased level of drinking, especially of wine, beginning a year before the wedding and lasting until 4 years after it. Consumption declined briefly during the year after a divorce49,50.
Women’s health
Studies on women’s health analyzed the relations between severity of urinary incontinence and quality of life, the association between social relations and the reporting of hot flushes and other common symptoms among non-menopausal women, the prevalence of severe stress urinary incontinence in relation to potential obstetric risk factors, and estimated the duration of hormone therapy use and factors associated with its discontinuation during the period before the publication of articles challenging their safety51–54.
What are the strengths and weaknesses?
We believe that the main strengths of the GAZEL Cohort Study are: (1) the diversity of the sample population in terms of social hierarchy; white and blue-collars; representation of all regions of France and various neighbourhoods from small villages to large cities; (2) the quality and length of follow-up: there is almost no loss to follow-up and subjects show a high participation level for additional data collection; (3) the prospective collection of data from different sources: self-reported, extracted from company and national registers, medical examinations, biology; (4) the large variety of health determinants (personal, lifestyle, social and occupational data), and outcomes (specific diseases, state of physical and mental health and quality of life); (5) repeated measures for most of the data, collected continuously (career, sickness absence, deaths) or through multiple waves.
The main weaknesses are (1): the limited size of the cohort for non frequent conditions (exposures and outcomes); (2) the restriction to EDF-GDF employees: security of employment, absence of certain categories of the population (agricultural workers, self-employed, foreigners…).
Can I get hold of the data? Where can I find out more?
Any research group, in France or elsewhere, can submit a research proposal to work on the GAZEL cohort. These projects are reviewed by a Scientific Committee, and those selected receive free access to the GAZEL data and subjects. More than 30 research projects have been conducted on this cohort by over 15 research groups from different countries (France, UK, Germany, Belgium, USA, Canada), many of them currently underway.
Submitting a research proposal involves filling an application form stating the objectives of the study, the description of sample, the methods, the data needed and a timetable. French legal requirements must also be met. The first step would be to contact one of the principal investigators of the GAZEL Cohort Study (MG or MZ). Refer to the GAZEL website: http://www.gazel.inserm.fr/ for further details on the study and the procedures for submitting a research proposal.
Acknowledgments
Many individuals at INSERM have contributed to the GAZEL Cohort Study. We wish to thank: Isabelle Bugel, Geneviève Carole, Mireille Coeuret-Pellicer, Sophie Launay, Marie-Hélène Martineau, Marie-José Marne, Jean-François Morcet, Anna Ozguler, Michèle Picciotti.
We are grateful to “Électricité de France-Gaz de France” and to the “Caisse centrale d’action sociale du personnel des industries électrique et gazière” for their cooperation and funding over so many years.
References
- 1.Goldberg M, Chevalier A, Imbernon E, Coing F, Pons H. The epidemiological information system of the French National Electricity and Gas Company: the SI-EPI Project. Med Lav. 1996;87:16–28. [PubMed] [Google Scholar]
- 2.Goldberg M, Blanc M, Chastang JF, Blanc C, Sommer M. The health data base of a nationwide company. Its use in epidemiological studies. J Occup Med. 1982;24:1, 47–52. [PubMed] [Google Scholar]
- 3.Blanc M, Lert F, Leclerc A, Chastang JF, Blanc C, Goldberg M. Épidémiologie des accidents graves du travail à Électricité et Gaz de France. Aspects démographiques, socioéconomiques, professionnels et géographiques. Arch Mai Prof. 1981:1, 42, 2, 69–84. [Google Scholar]
- 4.Chevalier A, Luce D, Blanc C, Goldberg M. Sickness absence at the French National Electric Gas Company. Br J Ind Med. 1987;44:2, 101–110. doi: 10.1136/oem.44.2.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chevalier A, Leclerc A, Blanc C, Goldberg M. Disparités sociales et professionnelles de la mortalité des travailleurs d’Électricité et Gaz de France. Population. 1987;6:863–880. [Google Scholar]
- 6.Thériault G, Goldberg M, Miller AB, Armstrong B, Guénel P, Deadman J, Imbernon E, To T, Chevalier A, Cyr D, et al. Cancer risks associated with occupational exposure to magnetic fields among electric utility workers in Ontario and Quebec, Canada, and France: 1970–1989. Am J Epidemiol. 1994;139(6):550–72. doi: 10.1093/oxfordjournals.aje.a117046. [DOI] [PubMed] [Google Scholar]
- 7.Armstrong B, Thériault G, Guénel P, Deadman J, Goldberg M, Heroux P. Association between exposure to pulsed electromagnetic fields and cancer in electric utility workers in Quebec, Canada, and France. Am J Epidemiol. 1994;140(9):805–20. doi: 10.1093/oxfordjournals.aje.a117329. [DOI] [PubMed] [Google Scholar]
- 8.Imbernon E, Goldberg M, Bonenfant S, Chevalier A, Guénel P, Vatré R, Dehaye J. Occupational respiratory cancer and exposure to asbestos: a case control study in a cohort of workers in the electricity and gas industry. Am J Ind Med. 1995;28:339–52. doi: 10.1002/ajim.4700280304. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg M, Chastang JF, Leclerc A, Zins, et al. Socioeconomic, demographic, occupational and health factors associated with participation in a long-term epidemiologic survey. A prospective study of the French GAZEL cohort and its target population. Am J Epidemiol. 2001;154(4):373–384. doi: 10.1093/aje/154.4.373. [DOI] [PubMed] [Google Scholar]
- 10.Corrao G, Lepore AR, Rapone C, Miccoli C, di Orio F. Reproducibility of an alcohol questionnaire for a case-control study on chronic liver diseases. Epidemiol Prev. 1991;13:45–9. [PubMed] [Google Scholar]
- 11.Mayfield D, McLeod G, Hall P. The CAGE questionnaire: validation of a new alcoholism screening instrument. Am J Psychiatry. 1974;131:1121–3. doi: 10.1176/ajp.131.10.1121. [DOI] [PubMed] [Google Scholar]
- 12.Berkman LF, Syme SL. Social networks, host resistance, and mortality: A nine-year follow-up of Alameda County residents. Am J Epidemiol. 1979;109:186–204. doi: 10.1093/oxfordjournals.aje.a112674. [DOI] [PubMed] [Google Scholar]
- 13.Bortner RW. A short rating scale as a potential measure of pattern A behavior. J Chronic Dis. 1969;22:87–91. doi: 10.1016/0021-9681(69)90061-7. [DOI] [PubMed] [Google Scholar]
- 14.Seeman TE, Berkman LF, Gulanski BI, Robbins RJ, Greenspan SL, Charpentier PA, Rowe JW. Self-esteem and neuroendocrine response to challenge: MacArthur studies of successful aging. J Psychosom Res. 1995;39:69–84. doi: 10.1016/0022-3999(94)00076-h. [DOI] [PubMed] [Google Scholar]
- 15.Buss AH, Durkee A. An inventory for assessing different kinds of hostility. J Consult Psychol. 1957;21:343–9. doi: 10.1037/h0046900. [DOI] [PubMed] [Google Scholar]
- 16.Consoli SM, Cordier S, Ducimetiere P. Validation of a personality questionnaire designed for defining sub-groups at risk for ischemic cardiopathy or cancer in the Gazel cohort. Rev Epidemiol Sante Publique. 1993;41:315–26. [PubMed] [Google Scholar]
- 17.Karasek RA. Job demands, job decision latitude, and mental strain: Implications for job redesign. Administrative Science Quarterly. 1979;24:285–308. [Google Scholar]
- 18.Siegrist J, Peter R. Measuring effort-reward imbalance at work: Guidelines. Düsseldorf. 1996 [Google Scholar]
- 19.Niedhammer I. Psychometric properties of the French version of the Karasek Job Content Questionnaire: a study of the scales of decision latitude, psychological demands, social support, and physical demands in the GAZEL cohort. Int Arch Occup Environ Health. 2002;75:129–44. doi: 10.1007/s004200100270. [DOI] [PubMed] [Google Scholar]
- 20.Niedhammer I, Tek ML, Starke D, Siegrist J. Effort-reward imbalance model and self-reported health: cross-sectional and prospective findings from the GAZEL cohort. Soc Sci Med. 2004;58:8, 1531–1541. doi: 10.1016/S0277-9536(03)00346-0. [DOI] [PubMed] [Google Scholar]
- 21.Imbernon E, Goldberg M, Guénel P, Bitouze F, Brèment F, Casal A, Creux S, Folliot D, Huez D, Lagorio S, et al. MATEX: une matrice emplois-expositions destineé á la surveillance épidémiologique des travailleurs d’une grande entreprise (EDF-GDF) Arch Mal Prof. 1991;52:559–66. [Google Scholar]
- 22.Guénel P, Nicolau Molina J, Imbernon E, Warret G, Goldberg M. Design of a job-exposure matrix on electric and magnetic fields: selection of an efficient job classification for workers in thermoelectric power production plants. Int J Epidemiol. 1993;22(suppl 2):S16–S21. doi: 10.1093/ije/22.supplement_2.s16. [DOI] [PubMed] [Google Scholar]
- 23.Metzger MH, Goldberg M, Chastang JF, Leclerc A, Zins M. Factors associated with self-reporting of chronic health problems in the French GAZEL cohort. J Clin Epidemiol. 2002 Jan;:55, 48–59. doi: 10.1016/s0895-4356(01)00409-7. [DOI] [PubMed] [Google Scholar]
- 24.Fuhrer R, Rouillon F. La version française de I’échelle CES-D: description et tracuction de I’échelle d’auto-évaluation. Psychiatry and Psychobiology. 1989;4:163–6. [Google Scholar]
- 25.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 26.Bucquet D, Condon S, Ritchie K. The French version of the Nottingham Health Profile. A comparison of items weights with those of the source version. Soc Sci Med. 1990;30:829–35. doi: 10.1016/0277-9536(90)90207-9. [DOI] [PubMed] [Google Scholar]
- 27.Leplege A, Mesbah M, Marquis P. Preliminary analysis of the psychometric properties of the French version of an international questionnaire measuring the quality of life: the MOS SF-36 (version 1.1) Rev Epidemiol Sante Publique. 1995;43(4):371–9. [PubMed] [Google Scholar]
- 28.Wiggins RD, Higgs PFD, Hyde M, Blane DB. Quality of life in the third age: key predictors of the CASP-19 measure. Ageing Soc. 2004;24:693–708. [Google Scholar]
- 29.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963 September 21;:185, 914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 30.Kuorinka I, Jonsson B, Kilbom A, et al. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987 Sep;18(3):233–7. doi: 10.1016/0003-6870(87)90010-x. [DOI] [PubMed] [Google Scholar]
- 31.Chaudemanche H, Monnet E, Westeel V, et al. Respiratory status in dairy farmers in France; cross sectional and longitudinal analyses. Occup Environ Med. 2003 Nov;60(11):858–63. doi: 10.1136/oem.60.11.858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chevalier A, Goldberg M, Godard C, et al. Cancer incidence among active male workers at Electricite de France-Gaz de France. Rev Epidemiol Sante Publique. 1996;44:25–36. [PubMed] [Google Scholar]
- 33.Chevalier A, Zins M, Godard C, et al. A registry of ischaemic cardiopathies among active workers at Electricite de France-Gaz de France. Program development and first results Rev Epidemiol Sante Publique. 2001;49:51–60. [PubMed] [Google Scholar]
- 34.Goldberg M, Chastang JF, Zins M, Niedhammer I, Leclerc A. Health problems were the strongest predictors of attrition during follow up of the GAZEL cohort. J Clin Epid. 2006 doi: 10.1016/j.jclinepi.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 35.Leclerc A, Tubach F, Landre MF, Ozguler A. Personal and occupational predictors of sciatica in the GAZEL cohort. Occup Med. 2003;53:384–91. doi: 10.1093/occmed/kqg072. [DOI] [PubMed] [Google Scholar]
- 36.Paterniti S, Niedhammer I, Lang T, Consoli SM. Psychosocial factors at work, personality traits and depressive symptoms. Longitudinal results from the GAZEL Study Br J Psychiatry. 2002;181:111–7. [PubMed] [Google Scholar]
- 37.Niedhammer I, Tek ML, Starke D, Siegrist J. Effort-reward imbalance model and self-reported health: cross-sectional and prospective findings from the GAZEL cohort. Soc Sci Med. 2004;58:1531–41. doi: 10.1016/S0277-9536(03)00346-0. [DOI] [PubMed] [Google Scholar]
- 38.Berr C, Bonenfant S, Vercambre MN, Zins M. Long term occupational exposure and risk of cognitive impairment: preliminary results from the GAZEL Cohort. Neurology. 2005;64(Suppl 1):A364. [Google Scholar]
- 39.Melchior M, Krieger N, Kawachi I, Berkman LF, Niedhammer I, Goldberg M. Work factors and occupational class disparities in sickness absence: findings from the GAZEL cohort study. Am J Public Health. 2005;95:1206–12. doi: 10.2105/AJPH.2004.048835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Melchior M, Niedhammer I, Berkman LF, Goldberg M. Do psychosocial work factors and social relations exert independent effects on sickness absence? A six year prospective study of the GAZEL cohort J Epidemiol Community Health. 2003;57:285–93. doi: 10.1136/jech.57.4.285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Melchior M, Goldberg M, Krieger N, Kawachi I, Menvielle G, Zins M, Berkman L. Occupational class, occupational mobility and cancer incidence among middle-aged men and women: a prospective study of the French GAZEL cohort. Cancer Causes and Control. 2005;16:515–524. doi: 10.1007/s10552-004-7116-0. [DOI] [PubMed] [Google Scholar]
- 42.Berkman L, Melchior M, Chastang JF. Social Integration and Mortality: A prospective study of French employees of Electricity of France Gas of France, the GAZEL Cohort. Am J Epid. 2004;159:167–174. doi: 10.1093/aje/kwh020. [DOI] [PubMed] [Google Scholar]
- 43.Melchior M, Berkman L, Niedhammer I, Chea M, Goldberg M. Social relations and self-reported health: a prospective analysis of the French GAZEL cohort. Social Science & Medicine. 2003;56:1817–1830. doi: 10.1016/s0277-9536(02)00181-8. [DOI] [PubMed] [Google Scholar]
- 44.Fuhrer R, Shipley MJ, Chastang JF, et al. Socioeconomic position, health, and possible explanations: a tale of two cohorts. Am J Public Health. 2002;92:1290–4. doi: 10.2105/ajph.92.8.1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Singh-Manoux A, Martikainen P, Ferrie J, Zins M, Marmot M, Goldberg M. What does self rated health measure? Results from the British Whitehall II and French Gazel cohort studies J Epidemiol Community Health. 2006;60:364–72. doi: 10.1136/jech.2005.039883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nabi H, Consoli SM, Chastang JF, Chiron M, Lafont S, Lagarde E. Type A Behavior Pattern, Risky Driving Behaviors, and Serious Road Traffic Accidents: A Prospective Study of the GAZEL Cohort. American Journal Of Epidemiology. 2005;161:9, 864–870. doi: 10.1093/aje/kwi110. [DOI] [PubMed] [Google Scholar]
- 47.Lagarde E, Chastang Jf, Gueguen A, Coeuret-Pellicer M, Chiron M, Lafont S. Emotional stress and traffic accidents: the impact of separation and divorce. Epidemiology. 2004;15:6, 762–766. doi: 10.1097/01.ede.0000142140.77194.ad. [DOI] [PubMed] [Google Scholar]
- 48.Nabi H, Guéguen A, Chiron M, Lafont S, Zins M, Lagarde E. Awareness of driving while sleepy and road traffic accidents: prospective study in GAZEL cohort. BMJ. 2006;333(7558):75. doi: 10.1136/bmj.38863.638194.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zins M, Carle F, Bugel I, Leclerc A, Di Orio F, Goldberg M. Predictors of change in alcohol consumption among Frenchmen of the GAZEL study cohort. Addiction. 1999;94(3):385–395. doi: 10.1046/j.1360-0443.1999.9433858.x. [DOI] [PubMed] [Google Scholar]
- 50.Zins M, Guéguen A, Leclerc A, Goldberg M. Alcohol consumption and marital status of French women in the GAZEL cohort: a longitudinal analysis between 1992 and 1996. J Stud Alcohol. 2003;64:784–789. doi: 10.15288/jsa.2003.64.784. [DOI] [PubMed] [Google Scholar]
- 51.Saadoun K, Ringa V, Fritel X, Varnoux N, Zins M, Breart G. Negative impact of urinary incontinence on quality of life, a cross-sectional study among women aged 49–61 years enrolled in the GAZEL cohort. Neurourol Urodyn. 2006 Aug 17; doi: 10.1002/nau.20245. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 52.Duche L, Ringa V, Melchior M, Varnoux N, Piault S, Zins M, Breart G. Hot flushes, common symptoms, and social relations among middle-aged nonmenopausal French women in the GAZEL cohort. Menopause. 2006;13:592–9. doi: 10.1097/01.gme.0000227329.41458.86. [DOI] [PubMed] [Google Scholar]
- 53.Fritel X, Ringa V, Varnoux N, Fauconnier A, Piault S, Breart G. Mode of delivery and severe stress incontinence, a cross-sectional study among 2,625 perimenopausal women. BJOG. 2005112:1646–51. doi: 10.1111/j.1471-0528.2005.00763.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ringa V, Varnoux N, Piault S, Breart G. Hormone therapy use among postmenopausal French women before the publication of the Women’s Health Initiative study: duration of use and factors associated with discontinuation. Fertil Steril. 2005;83:1771–9. doi: 10.1016/j.fertnstert.2004.12.040. [DOI] [PubMed] [Google Scholar]


