Abstract
We investigated the in vitro activity of AR-709, a novel diaminopyrimidine antibiotic currently in development for treatment of community-acquired upper and lower respiratory tract infections, against 151 Streptococcus pneumoniae strains from various European countries. AR-709 showed excellent activity against both drug-susceptible and multidrug-resistant pneumococci.
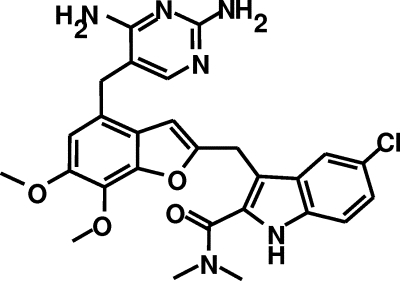
Diaminopyrimidine antibiotics block bacterial DNA, RNA, and protein synthesis by inhibiting bacterial dihydrofolate reductase (2). AR-709 (Fig. 1) is a low-molecular-weight, synthetic, novel diaminopyrimidine antibiotic under development by Arpida (Muenchenstein, Switzerland) for the treatment of community-acquired respiratory infection. AR-709 recently entered human clinical trials. We investigated the in vitro activity against Streptococcus pneumoniae isolates from various European countries.
FIG. 1.
Schematic structure of the diaminopyrimidine antibiotic AR-709.
A total of 151 clinical S. pneumoniae strains were tested, including 63 penicillin-susceptible isolates and 88 penicillin-intermediate or -resistant strains. Isolates were derived from patients with respiratory tract infections from 16 different European countries. Only one isolate per patient was included. Microtiter plates containing frozen serial dilutions of the antibiotics were prepared by Trek Diagnostics. Susceptibility testing was performed by the microdilution method according to CLSI guidelines (1). MICs were recorded as the lowest antibiotic concentration that inhibits visible growth. MICs of AR-709, trimethoprim, and trimethoprim-sulfamethoxazole (cotrimoxazole) were read as the concentration at which there was an 80% or greater reduction of growth compared to the control. S. pneumoniae ATCC 49619 was used as the quality control.
Based on concentrations at which 50% of bacteria were inhibited (MIC50s), telithromycin and AR-709 were the most active compounds. Telithromycin had a lower MIC50 than AR-709 (≤0.015 versus 0.03, respectively), whereas its concentration at which 90% of bacteria were inhibited (MIC90) was slightly higher (0.5 versus 0.25, respectively). AR-709 was 128 times more active than trimethoprim (MIC90 of >32 mg/liter) and 16 times more active than cotrimoxazole (MIC90 of 8 mg/liter) and showed a superior MIC distribution range (≤0.015 to 0.5) (Table 1).
TABLE 1.
Susceptibilities of S. pneumoniae (n = 151 isolates) to AR-709 and comparators
| Antibiotica | Susceptibility of isolatesb
|
MIC of antibiotic (mg/liter)
|
||||
|---|---|---|---|---|---|---|
| % S | % I | % R | Range | 50% | 90% | |
| AR-709 | ≤0.015-0.5 | 0.03 | 0.25 | |||
| Trimethoprim | 1->32 | 4 | >32 | |||
| Cotrimoxazole | 50.3 | 10.6 | 39.1 | 0.06-16 | 0.5 | 8 |
| Penicillin | 41.7 | 19.9 | 38.4 | ≤0.06-4 | 0.25 | 2 |
| Amoxicillin | 55.0 | 5.3 | 39.7 | ≤0.015-16 | 0.25 | 4 |
| Amox/clav | 55.0 | 6.0 | 39.1 | 0.03-16 | 0.25 | 4 |
| Azithromycin | 62.3 | 0.0 | 37.7 | ≤0.015->8 | 0.12 | >8 |
| Telithromycin | 98.0 | 1.3 | 0.7 | ≤0.015-4 | 0.5 | |
| Gatifloxacin | 98.7 | 0.7 | 0.7 | 0.12-4 | 0.25 | 0.25 |
Amox/clav, amoxicillin-clavulanic acid.
S, I, and R, susceptible, intermediate, and resistant, respectively. For ATCC 49619 (quality control), the MIC of AR-709 was ≤0.015 mg/liter.
Pneumococcal strains susceptible to penicillin had slightly lower AR-709 MICs (MIC50/MIC90 of ≤0.015/≤0.015 mg/ liter) than penicillin-nonsusceptible strains (for penicillin- intermediate strains, the MIC50/MIC90 was 0.03/0.12 mg/liter, versus penicillin-resistant strains, for which the MIC50/MIC90 was 0.06/0.25 mg/liter). Similarly, cotrimoxazole-susceptible pneumococci showed a lower AR-709 MIC50/MIC90 than cotrimoxazole-resistant strains (≤0.015/0.03 mg/liter versus 0.12/0.25 mg/liter, respectively). A total of 26 pneumococcal isolates were multidrug resistant, exhibiting resistance to penicillin, cotrimoxazole, azithromycin, and amoxicillin- clavulanic acid. AR-709 was also highly active against these multidrug-resistant S. pneumoniae strains, with a MIC50/MIC90 of 0.12/0.25 mg/liter (Table 2).
TABLE 2.
In vitro activities of AR-709 against S. pneumoniae strains with various resistance patterns
| Resistance patterna | No. of strains | In vitro activity of AR-709 (mg/liter)
|
||
|---|---|---|---|---|
| MIC50 | MIC90 | MIC range | ||
| Penicillin S | 63 | ≤0.015 | ≤0.015 | ≤0.015-0.25 |
| Penicillin I | 30 | 0.03 | 0.12 | ≤0.015-0.25 |
| Penicillin R | 58 | 0.06 | 0.25 | ≤0.015-0.5 |
| Cotrimoxazole S | 76 | ≤0.015 | 0.03 | ≤0.015-0.06 |
| Cotrimoxazole I | 16 | ≤0.015 | 0.06 | ≤0.015-0.25 |
| Cotrimoxazole R | 59 | 0.12 | 0.25 | 0.03-0.5 |
| Azithromycin S | 94 | ≤0.015 | 0.12 | ≤0.015-0.25 |
| Azithromycin R | 57 | 0.06 | 0.25 | ≤0.015-0.5 |
| Amox/clav S | 92 | ≤0.015 | 0.06 | ≤0.015-0.25 |
| Amox/clav R | 59 | 0.06 | 0.25 | 0.03-0.5 |
| Multidrug resistant | 26 | 0.12 | 0.25 | 0.03-0.5 |
S, I, and R, susceptible, intermediate, and resistant; amox/clav, amoxicillin-clavulanic acid; multidrug resistant, resistant to penicillin, cotrimoxazole, azithromycin, and amoxicillin-clavulanic acid.
The potent in vitro activity of AR-709 against S. pneumoniae is in agreement with findings of Smith et al. (3), although MIC50s/MIC90s reported in our study are two- to fourfold lower for penicillin-susceptible, -intermediate, and -resistant S. pneumoniae. This may be due to differences in the origins of the strains, since the strains from the study conducted by Smith et al. were from the United States, Europe, Russia, and Greece.
The fact that MICs of AR-709 were low against all strains tested in this study, independent of their resistance phenotypes and including strains resistant to one or two, as well as three or more, drugs (i.e., multidrug-resistant strains), makes this new agent a promising therapeutic alternative for treatment of infections caused by drug-susceptible and -resistant pneumococci.
Acknowledgments
This study was supported by Arpida.
Isolates were kindly provided by the following: M. Struelens, Belgium; J. K. Moller and K. Fuursted, Denmark; M. Vaara, Finland; J. Acar, F. Goldstein, J. Mgyen and J. Etienne, France; F. J. Schmitz, Germany; N. Legakis, Greece; F. Schneider and P. Kirpach, Luxembourg; A. R. Janz, H. van de Boogards, E. Ijzerman, and R. Muiser, The Netherlands; W. Hryniewicz, Poland; G. Ribeiro, Portugal; R. Martin, Spain; H. Miorner, Sweden; J. Bille and F. Praplan, Switzerland; D. Gür, Turkey; and J. Andrews, United Kingdom.
Footnotes
Published ahead of print on 7 January 2008.
REFERENCES
- 1.Clinical and Laboratory Standards Institute. 2005. Performance standards for antimicrobial susceptibility testing. Document M100-S15. CLSI, Wayne, PA.
- 2.Hawser, S., S. Lociuro, and K. Islam. 2006. Dihydrofolate reductase inhibitors as antibacterial agents. Biochem. Pharmacol. 71:941-948. [DOI] [PubMed] [Google Scholar]
- 3.Smith, K., L. M. Ednie, and P. C. Appelbaum. 2006. Comparative activity of AR-709, an investigational diaminopyrimidine, against 165 drug-susceptible and -resistant pneumococci. Abstr. Intersci. Conf. Antimicrob. Agents Chemother., abstr. F1-1958.