Abstract
Outbreaks of highly pathogenic H5N1 influenza viruses in avian species began in Asia and have since spread to other continents. Concern regarding the pandemic potential of these viruses in humans is clearly warranted, and there is an urgent need to develop effective vaccines against them. Previously, we and others demonstrated that deletions of the M2 cytoplasmic tail caused a growth defect in A/WSN/33 (H1N1) influenza A virus in vitro (K. Iwatsuki-Horimoto, T. Horimoto, T. Noda, M. Kiso, J. Maeda, S. Watanabe, Y. Muramoto, K. Fujii, and Y. Kawaoka, J. Virol. 80:5233-5240, 2006; M. F. McCown and A. Pekosz, J. Virol. 79:3595-3605, 2005; M. F. McCown and A. Pekosz, J. Virol. 80:8178-8189, 2006). We therefore tested the feasibility of using M2 tail mutants as live attenuated vaccines against H5N1 virus. First we generated a series of highly pathogenic H5N1 (A/Vietnam/1203/04 [VN1203]) M2 cytoplasmic tail deletion mutants and examined their growth properties in vitro and in vivo. We found that one mutant, which contains an 11-amino-acid deletion from the C terminus (M2del11 virus), grew as well as the wild-type virus but replicated in mice less efficiently. We then generated a recombinant VN1203M2del11 virus whose hemagglutinin (HA) gene was modified by replacing sequences at the cleavage site with those of an avirulent type of HA (M2del11-HAavir virus). This M2del11-HAavir virus protected mice against challenge with lethal doses of homologous (VN1203; clade 1) and antigenically distinct heterologous (A/Indonesia/7/2005; clade 2) H5N1 viruses. Our results suggest that M2 cytoplasmic tail mutants have potential as live attenuated vaccines against H5N1 influenza viruses.
In 1997, a highly pathogenic avian influenza virus (H5N1 subtype) was transmitted from chickens to humans in Hong Kong, killing 6 of 18 people infected (7, 40). The recent H5N1 outbreaks in poultry, which began in late 2003, affected more than 10 Asian countries, and viruses have now been isolated from wild birds and poultry in Asia, Europe, and Africa (22, 47). The continued circulation of H5N1 viruses in birds provides ample opportunity for them to infect humans. Indeed, human cases of H5N1 infections have been observed in several countries since late 2003, with a total of 321 confirmed cases and 194 fatalities as of 16 August 2007, resulting in a fatality rate of approximately 60% (http://www.who.int/csr/disease/avian_influenza/country/cases_table_2007_08_16/en/index.html). Concern over the pandemic potential of H5N1 viruses is thus clearly warranted. Although antiviral drugs, such as matrix protein 2 (M2) (adamantanes) and neuraminidase (NA) (oseltamivir and zanamivir) inhibitors, are currently available for prophylaxis and treatment of influenza virus infection, some of the H5N1 viruses isolated from humans are resistant to the adamantanes (6, 15, 32). In addition, some H5N1 viruses are resistant to oseltamivir (9, 21). Therefore, there is an urgent need to develop effective vaccines against the H5N1 viruses.
For the existing seasonal human influenza, both inactivated virus vaccine and live attenuated virus vaccine are available. In April 2007, the U.S. Food and Drug Administration (FDA) announced the first approval of an inactivated vaccine for humans against the H5N1 virus. However, the available data indicate that inactivated H5 influenza vaccines are suboptimal in their immunogenicity, and a large amount of hemagglutinin (HA) glycoprotein or coadministration of an adjuvant is required to achieve an adequate immune response (4, 23, 28, 37, 46). To overcome the shortcomings of the current inactivated influenza vaccine, several approaches have been tried, including using live attenuated influenza viruses that can elicit both systemic and mucosal immunity at the primary portal of infection.
The influenza A virus M2 protein consists of three structural domains: a 24-amino-acid extracellular domain, a 19-amino-acid transmembrane domain, and a 54-amino-acid cytoplasmic tail domain (20, 50). The M2 transmembrane domain has ion channel activity, which functions at an early stage of the viral life cycle between the steps of virus penetration and uncoating (13, 31). Recently, we and others reported that the M2 cytoplasmic tail domain also has an important role in viral assembly and morphogenesis (16, 25, 26). Here, we demonstrate that an M2 cytoplasmic tail deletion mutant protects mice from lethal challenge with a highly pathogenic H5N1 virus, suggesting the potential of M2 tail mutants as live attenuated vaccines against H5N1 influenza virus infection.
MATERIALS AND METHODS
Cells.
293T human embryonic kidney cells and Madin-Darby canine kidney (MDCK) cells were maintained in Dulbecco's modified Eagle's medium supplemented with 10% fetal calf serum and in minimal essential medium (MEM) containing 5% newborn calf serum, respectively. MDCK cells stably expressing M2 from A/Puerto Rico/8/34 (H1N1) (M2CK cells) were cultured in MEM supplemented with 10% fetal calf serum and 0.15 mg/ml hygromycin (16). All cells were maintained at 37°C in 5% CO2.
Plasmid construction.
The cDNA of A/Vietnam/1203/04 (VN1203) virus was synthesized by reverse transcription of viral RNA with an oligonucleotide complementary to the conserved 3′ end of the viral RNA, as described by Katz et al. (17). The cDNA was amplified by PCR with M gene-specific oligonucleotide primers containing BsmBI sites, and PCR products were cloned into the pGEM vector. The resulting construct was designated pGEM-VN1203M. After digestion with BsmBI, the fragment was cloned into the BsmBI sites of the pHH21 vector, which contains the human RNA polymerase I promoter and the mouse RNA polymerase I terminator, separated by BsmBI sites, resulting in pPolIUdM. Plasmids derived from pHH21 for the expression of viral RNA are referred to as “PolI” constructs throughout this report.
The M mutants were constructed as follows. pGEM-VN1203M was first amplified by inverse PCR (29) using the back-to-back primers M987stopF (5′-gtgaATAGAATTGGAGTAAAAAACTACC-3′) and M987stopR (5′-tcaAAAATGACCATCGTCAACATCCAC-3′), M969stopF (5′-gtgaGATGGTCATTTTGTCAACATAGAA-3′) and M969stopR (5′-tcaATCCACAGCACTCTGCTGTTCCTG-3′), M936stopF (5′-gtgaCGGCAGGAACAGCAGAGTGCTG-3′) and M936stopR (5′-tcaTTCCCTCATAGACTCAGGTACC-3′), M903stopF (5′-gtgaGCAGGGGTACCTGAGTCTATG-3′) and M903stopR (5′-tcaAGGCCCTCTTTTCAAACCGTA-3′), M870stopF (5′-CTTAAATACGGTTTGAAAAGAGGGCCTGC-3′) and M870stopR (5′-tcactcaATAAATGCATTTGAAGAAAAGACGATC-3′), and M783stopF (5′-TTGTTGTTGCCGCAAATATCATTGGG-3′) and M783stopR (5′-TtcactcaACTTGAATCGCTGCATCTGC-3′). Nucleotide changes to introduce stop codons are indicated by lowercase letters. The PCR products were then phosphorylated, self-ligated, propagated in Escherichia coli strain DH5α, and then digested with BsmBI and cloned into the BsmBI sites of the pHH21 vector. The resulting constructs were designated pPolI-VN1203M2del5, pPolI-VN1203M2del11, pPolI-VN1203M2del22, pPolI-VN1203M2del33, pPolI-VN1203M2del44, and pPolI-VN1203delM2, each of which contained two stop codons at nucleotide positions 972 to 974, 939 to 941, 906 to 908, 873 to 875, and 786 to 788 of the M segment, which resulted in the deletion of 5, 11, 22, 33, 44, and 70 residues from the C terminus of the M2 protein, respectively (Fig. 1). All of the constructs were sequenced to ensure that unwanted mutations were not present.
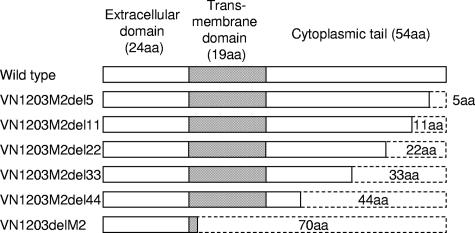
FIG. 1.
Schematic representation of the M2 mutants. The M gene was derived from a highly pathogenic H5N1 (VN1203) virus. The mutants del5, del11, del22, del33, and del44 contain a 5-, 11-, 22-, 33-, or 44-amino-acid (aa) deletion from the C terminus, respectively. The mutant delM2 was constructed by deletion of 70 C-terminal residues, including the entire transmembrane and cytoplasmic domains.
Plasmid-driven reverse genetics.
All of the viruses used in this study were generated by the introduction of plasmids expressing eight viral RNA segments and three polymerase proteins plus NP, as described by Neumann et al. (27). At 48 hours posttransfection, viruses were harvested and used to inoculate M2CK cells for the production of stock viruses. The M genes of transfectant viruses were sequenced to confirm the origin of the gene and the presence of the intended mutations and to ensure that no unwanted mutations were present. All experiments with live viruses and with transfectants generated by reverse genetics were performed in a biosafety level 3 containment laboratory approved for such use by the CDC and the U.S. Department of Agriculture.
Replicative properties of the transfectant viruses in cell culture.
MDCK cells were infected in duplicate wells of 24-well plates with the wild-type or mutant viruses at a multiplicity of infection (MOI) of 0.001, overlaid with MEM containing 0.5 μg of trypsin per ml, and incubated at 37°C. At select time points, supernatants were assayed for infectious virus in plaque assays on M2CK cells (16).
Experimental infection.
Five-week-old female BALB/c mice, anesthetized with isoflurane, were infected intranasally with 50 μl (100 PFU) of virus. Virus titers in organs were determined 3 days after infection by use of MDCK cells, as described previously (2).
Immunization and protection.
BALB/c mice (4-week-old females) were intranasally immunized with 100 or 1,000 PFU/50 μl of the M2del11-HAavir virus. Three weeks later, four mice were sacrificed to obtain sera, trachea-lung washes, and nasal washes. One month after vaccination, immunized mice were challenged intranasally, under anesthesia, with 3.8 × 102 PFU or 5 × 104 PFU of the wild-type VN1203 or A/Indonesia/7/05 virus, which was equivalent to 100 50% minimal lethal doses (MLD50) (dose required to kill 50% of infected mice), respectively. To determine virus titers in mice, organ samples were harvested at day 3 postchallenge and were homogenized and titrated on MDCK cells. The remaining animals were observed for clinical signs and symptoms of infection for 14 days postchallenge.
Virus-specific antibody detection.
Immunoglobulin G (IgG) and IgA antibody titers were measured in sera, trachea-lung washes, and nasal washes of the immunized mice by use of an enzyme-linked immunosorbent assay (ELISA) (18). In this assay, the wells were coated with purified A/Vietnam/1194/05 virus after treatment with 0.05 M Tris-HCl (pH 7.8) containing 0.5% Triton X-100 and 0.6 M KCl at room temperature for 1 h and then diluted in phosphate-buffered saline (PBS). After incubation of virus-coated plates with test serum samples for 1 h, bound antibody was detected with a rabbit anti-mouse IgA (Kirkegaard & Perry Laboratories Inc., Gaithersburg, MD) and a goat anti-mouse IgG (Boehringer, Mannheim, Germany) conjugated to horseradish peroxidase. Neutralizing antibody titers in serum samples of the immunized mice were also evaluated. The sera were treated with receptor-destroying enzyme (Accurate Chemical and Scientific Corp.) to destroy inhibitors of influenza virus replication. After inactivation of the receptor-destroying enzyme by treatment at 56°C for 30 min, VN1203 and A/Indonesia/7/05 viruses were each incubated with twofold serial dilutions of serum (starting at a 1:10 dilution) at 37°C for 1 h. Viral infectivity was determined by titration of the samples in a plaque assay on MDCK cells. The neutralizing titer was defined as the reciprocal titer of serum required to neutralize at least 50% of each virus.
RESULTS
In vitro growth properties of VN1203 viruses possessing M2 cytoplasmic tail deletion mutations.
We first generated a series of M2 cytoplasmic tail deletion mutants of a highly pathogenic H5N1 (VN1203) virus by reverse genetics as described previously (27). Transfectant viruses were harvested at 48 h posttransfection and used to inoculate M2CK cells to propagate stock viruses. The stock virus titers were comparable to that of the wild-type virus: 6.2 × 108 PFU/ml for VN1203M2del44, 6.8 × 108 PFU/ml for VN1203M2del33, 6.3 × 108 PFU/ml for VN1203M2del22, 5.4 × 108 PFU/ml for VN1203M2dl11, 6.1 × 108 PFU/ml for VN1203M2del5, and 2.4 × 108 PFU/ml for the wild-type virus. The only exception was VN1203delM2 (6.0 × 106 PFU/ml).
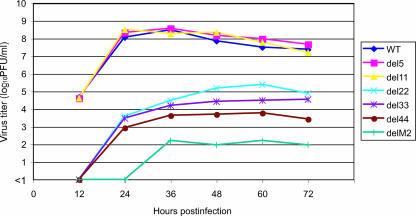
Next, we compared the growth properties of the VN1203 M2 tail mutant viruses with those of wild-type VN1203 virus in MDCK cells (Fig. 2). MDCK cells were infected with viruses at an MOI of 0.001, and their growth kinetics were monitored for 72 h. The VN1203M2del5 and -M2del11 viruses grew as well as the wild-type virus. By contrast, the VN1203M2del22, -M2del33, and -M2del44 viruses replicated less efficiently than the wild-type virus (1,000 to 10,000-fold-lower growth). In particular, the VN1203delM2 virus, which lacks both the transmembrane and cytoplasmic tail domains, was significantly growth restricted on MDCK cells (100,000-fold-lower growth than the wild-type virus). These results are consistent with previous findings that mutant viruses with deletions at the C terminus of the M2 tail grew less well in cell culture (16, 25, 26).
FIG. 2.
Growth kinetics of the M2 tail deletion mutant viruses in MDCK cells. MDCK cells were infected with the M2 tail deletion mutant viruses at an MOI of 0.001. At the indicated times after infection, the virus titer in the supernatant was determined with M2CK cells. The values presented are means from duplicate experiments. WT, wild type.
In vivo growth properties of VN1203 M2 tail deletion mutants.
To determine the virulence of our M2 tail mutants, we examined their growth properties in mice. Mice were infected with 100 PFU of M2 mutant or wild-type viruses. On day 3 postinfection, organs were taken from the infected mice for virus titration. As shown in Table 1, the wild-type VN1203 virus replicated well in all organs examined. Mutants possessing deletions of more than 22 amino acids were not recovered from any of the infected mice. Of interest, replication of the VN1203M2del5 and -M2del11 viruses was more than 1 log lower in the lungs, 2 logs lower in nasal turbinates, and 2 logs lower in the kidneys of infected mice than that of wild-type virus. Moreover, no virus was detected from the brain samples of mice infected with the VN1203M2del11 virus. These results indicate that the VN1203M2del11 virus was attenuated in mice, despite replicating as well as the wild-type virus in MDCK cells.
TABLE 1.
Replication of M2 mutant viruses in mice
| Virus | Virus titer (mean log10 PFU/g ± SD) ina:
|
||||
|---|---|---|---|---|---|
| Lungs | Nasal turbinates | Brains | Spleens | Kidneys | |
| Wild type | 8.41 ± 0.09 | 6.66 ± 0.85 | 5.02 ± 1.56 | 7.48 ± 0.48 | 6.23 ± 0.82 |
| VN1203M2del5 | 7.47 ± 0.29 | 4.70 ± 1.21 | 3.60, 3.51 | 5.54 ± 0.85 | 3.90, 4.03 |
| VN1203M2del11 | 7.30 ± 0.45 | 4.06, 4.74 | NDb | 3.97 ± 0.81 | 4.24 |
| VN1203M2del22 | ND | ND | ND | ND | ND |
| VN1203M2del33 | ND | ND | ND | ND | ND |
| VN1203M2del44 | ND | ND | ND | ND | ND |
| VN1203delM2 | ND | ND | ND | ND | ND |
Mice were infected with 100 PFU of M2 mutant or wild-type virus. Organ samples were taken from mice at day 3 postinfection. Virus titers were determined with M2CK cells. When virus was not recovered from all three mice, individual titers were recorded.
ND, not detected.
Generation of a recombinant VN1203 virus that possesses M2del11 and an avirulent HA.
Since the VN1203M2del11 virus was attenuated in mice, we decided to test the feasibility of using it for an H5N1 vaccine. To improve the safety of an H5N1 virus vaccine, vaccine candidates should have multiple attenuating mutations in the viral genes. We therefore introduced mutations into the cleavage site of the VN1203M2del11 virus HA, a virulence determinant of influenza viruses in birds and mammals (11, 19, 36). In general, low-pathogenicity viruses do not contain a series of basic amino acids at the HA cleavage site (19, 35, 36), restricting cleavage and viral replication to a limited number of organs (i.e., these viruses cause localized infections). By contrast, the HAs of highly pathogenic H5N1 avian influenza viruses contain a series of basic amino acids at this site (3, 10, 35, 39), which allow HA to be cleaved not only by trypsin but also by ubiquitous cellular proteases (14, 38), thereby allowing viral replication in a variety of organs, including brain (i.e., these viruses cause systemic infections). To ensure the safety of our vaccine strains, we constructed a mutant HA in which the amino acid sequence at the HA cleavage site, PQRERRRKKR/G, was converted to the sequence in a typical avirulent avian virus, PQ—-RETR/G (dashes indicate deletions). We then generated a recombinant virus possessing this avirulent HA and M2del11 mutations (designated M2del11-HAavir). Stock virus was amplified on M2CK cells, and the virus titer was 2.0 × 106 PFU/ml.
Characterization of the recombinant M2del11-HAavir virus in vitro and in vivo.
To characterize the M2del11-HAavir virus, we first examined its trypsin dependency in vitro. Plaque assays were performed on M2CK cells in the presence or absence of trypsin. With the M2del11-HAavir virus, clear plaques were visible only in the presence of trypsin, whereas the M2del11 virus formed plaques in both the presence and absence of trypsin (data not shown).
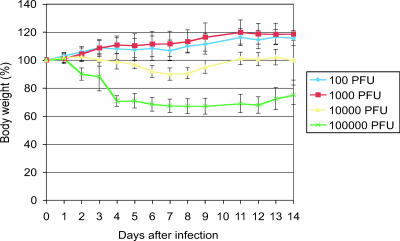
Next, to investigate the virulence of the M2del11-HAavir virus in vivo, mice were infected with various doses of the virus and monitored for 14 days (Fig. 3). Even at a high dose (1 × 105 PFU), the virus did not kill any mice (the MLD50 was >105 PFU, compared to 2.1 PFU for the wild-type VN1203 virus [data not shown]), although slight weight loss was observed (Fig. 3). Mice infected with 100 or 1,000 PFU of the M2del11-HAavir virus did not show any weight loss. We also examined organ tropisms for the M2del11-HAavir virus in mice. As shown in Table 2, the virus titers were 1 log lower in the lungs of mice infected with 100 PFU of the M2del11-HAavir virus than in those of mice infected with the wild-type virus. No virus was detected in the other organs of M2del11-HAavir-infected mice. Even in the mice infected with a high dose (1,000 PFU) of M2del11-HAaivr, the virus was recovered only from the lungs and nasal turbinates, indicating that virus replication was restricted to the respiratory tracts. These results suggest that the M2del11-HAavir virus was highly attenuated in mice.
FIG. 3.
Pathogenicity of a recombinant M2del11-HAavir virus. Mice were infected with 100, 1,000, 10,000, or 100,000 PFU of the M2del11-HAavir virus, and their body weights were monitored for 14 days. Data are reported as the mean changes in body weight ± standard deviation (n = 3).
TABLE 2.
Replication of M2del11-HAavir virus in mice
| Dose (PFU/mouse) | Virus titer (mean log10 PFU/g ± SD) ina:
|
||||
|---|---|---|---|---|---|
| Lungs | Nasal turbinates | Brains | Spleens | Kidneys | |
| 100 | 6.38 ± 1.28 | NDb | ND | ND | ND |
| 1,000 | 6.77 ± 0.17 | 3.67 ± 1.25 | ND | ND | ND |
Mice were infected with 100 or 1,000 PFU of M2 del11-HAair virus. Organ samples were taken from mice at day 3 postinfection. Virus titers were determined with M2CK cells.
ND, not detected.
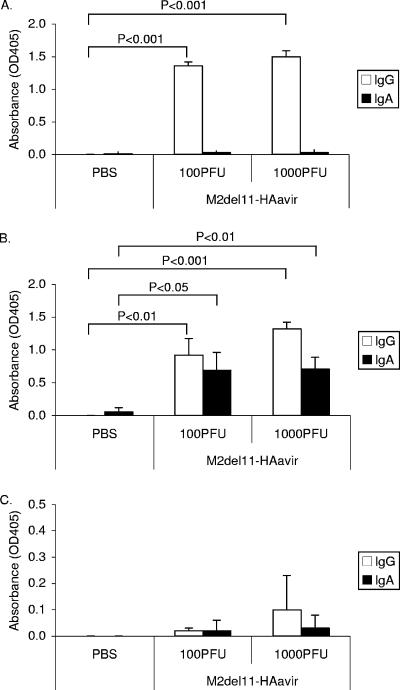
Antibody responses of mice immunized with the M2del11-HAavir virus.
To test the efficacy of the M2del11-HAavir virus as a vaccine, we intranasally immunized mice with 100 or 1,000 PFU of the M2del11-HAavir virus. Three weeks later, IgG and IgA levels in sera, trachea-lung washes, and nasal washes of immunized mice were measured by means of an ELISA (Fig. 4). Both IgG and IgA levels in trachea-lung washes were significantly higher in mice immunized with the M2del11-HAavir virus than in those treated with a PBS control, although there was no significant difference between the antibody titers in nasal washes from the vaccine group and the control group. The IgA response was negligible in serum, regardless of the dose of the mutant virus used for immunization, but IgG production was clearly higher in mice inoculated with the M2del11-HAavir virus. These data suggest that the M2del11-HAavir virus elicited a significant antibody response in the immunized mice.
FIG. 4.
Virus-specific serum and mucosal antibody responses in mice immunized with the M2del11-HAavir virus. Samples from each group were obtained 3 weeks postimmunization. IgG and IgA levels in sera (A), lung washes (B), and nasal washes (C) from individual mice were detected by ELISA. Values are expressed as the mean absorbance ± standard deviation (n = 4) of undiluted samples (trachea-lung and nasal washes) or of samples diluted 1:10 (sera). Differences between responses to PBS and the M2del11-HA virus were tested for statistical significance by use of Student's t test.
To examine whether or not the antibodies detected by ELISA contribute to neutralization of the H5N1 virus infectivity, we tested the infectivity-neutralizing activity of the samples against VN1203 (homologous virus; clade 1) and A/Indonesia/7/2005 (Indonesia 7) (heterologous virus; clade 2), whose HA homology is 96.5% at the amino acid level. Immunization with 1,000 PFU of M2del11-HAavir virus did not elicit neutralizing antibody efficiently, and the reciprocal titers of serum required to neutralize 50% of VN1203 and Indonesia 7 were only 31 and 23, respectively (data not shown). Moreover, no neutralizing antibody was detectable in sera from mice immunized with 100 PFU of M2del11-HAavir virus (data not shown), indicating that only a limited level of neutralizing antibody was elicited upon immunization of mice with the M2del11-HAavir virus despite high levels of protection upon lethal challenge and high levels of IgG detected by ELISA.
Protective efficacy of the M2del1-HAavir virus in mice.
Mice immunized with the M2del11-HAavir virus were challenged 1 month after immunization with 100 MLD50 of the wild-type VN1203 virus (clade 1) or Indonesia 7 (clade 2). Unlike control mice, all M2del11-HAavir-immunized mice survived a lethal challenge with either of the highly pathogenic H5N1 viruses (data not shown) and did not show any symptoms, including weight loss, after the challenge. By contrast, all of the control mice died or had to be euthanized due to their symptoms by day 8 postchallenge (data not shown). We also determined the virus titers in several organs of the mice challenged with the VN1203 or Indonesia 7 virus (Table 3). High titers of viruses were recovered from all organs of the control group. No virus was detected from any of the organs in the M2del11-HA virus vaccine group challenged with VN1203, though a limited amount of virus was detected in the nasal turbinates of one of the immunized mice challenged with the Indonesia 7 virus (Table 3). Taking the results together, we conclude that the M2del11-HAavir virus can confer protective immunity to mice against lethal challenge with highly pathogenic H5N1 virus.
TABLE 3.
Replication of challenge viruses in immunized mice at day 3 postchallenge
| Challenge virus | Group | Virus titer (mean log10 PFU/g ± SD) ina:
|
||||
|---|---|---|---|---|---|---|
| Lungs | Nasal turbinates | Brains | Spleens | Kidneys | ||
| VN1203 | PBS | 7.83 ± 0.46 | 6.11, 4.19 | 3.04 | 4.96 ± 0.66 | 2.78, 4.27 |
| M2del11-HAavir | ||||||
| 100 PFU | NDb | ND | ND | ND | ND | |
| 1,000 PFU | ND | ND | ND | ND | ND | |
| Indonesia 7 | PBS | 9.06 ± 0.10 | 7.01 ± 0.21 | 3.32 ± 1.37 | 5.64 ± 0.12 | 4.27 ± 0.38 |
| M2del11-HAavir | ||||||
| 100 PFU | N D | ND | ND | ND | ND | |
| 1,000 PFU | ND | 1.96 | ND | ND | ND | |
Three mice from each group were sacrificed on day 3 postchallenge for virus titration. When virus was not recovered from all three mice, individual titers were recorded.
ND, not detected.
DISCUSSION
The influenza A virus M2 is a multifunctional protein. It has ion channel activity in its transmembrane domain (31), which is thought to function at an early stage of replication (acidification of the virion interior) (13, 24, 41) and at a late stage (protection of an acid-mediated conformational change of cleaved HA) (12, 30, 44). In addition, its cytoplasmic tail is important for viral assembly (16, 25, 26). In this study, we generated a series of M2 tail deletion mutants and examined their growth properties in vitro and in vivo. We found that deletions of 5 or 11 amino acids from the C terminus of M2 did not affect virus replication in cell culture but inhibited virus growth in mice. We previously showed that even one amino acid deletion from the M2 C terminus attenuated influenza virus in ferrets (5). Those findings indicate that the M2 cytoplasmic tail has a vital role(s) in virus replication in animals and that M2 tail mutants could be good vaccine candidates for influenza virus infection. Here, we demonstrated that H5N1 M2del11-HAavir virus, which has an 11-amino-acid deletion from the C terminus of its M2 protein and an avirulent HA, protected mice from a lethal challenge with H5N1 viruses, indicating its considerable potential as a live virus vaccine against highly pathogenic H5N1 viruses.
Recently, Suguitan et al. tested the vaccine efficacy in mice and ferrets of live attenuated, cold-adapted virus vaccine candidates that possess the modified avirulent type of HA and the NA from H5N1 strains, together with the internal genes from cold-adapted A/Ann Arbor/6/60 (H2N2) (42). They demonstrated that a single dose of the vaccine protected animals from lethality but did not fully protected them from replication of the challenge H5N1 viruses, indicating limited efficacy for single-dose vaccination of these cold-adapted viruses. This incomplete protection may stem from unmatched antigenicity between the internal proteins of the cold-adapted virus (i.e., derived from H2N2 virus) and the challenge virus. Here, we showed that the M2del11-HAavir virus, whose eight genes are derived from an H5N1 virus, protects mice almost completely from replication of heterologous H5N1 virus as well as homologous virus (Table 3). Despite its complete protection, the M2del11-HAavir virus did not elicit neutralizing antibody against either homologous or heterologous viruses efficiently, whereas it elicited high levels of antibodies detected by ELISA (Fig. 4). Therefore, cytotoxic T-lymphocyte responses specific to viral internal proteins that contain common cytotoxic T-lymphocyte epitopes among influenza A viruses (i.e., NP and M proteins) and mucosal immune responses may be responsible for the cross-protection observed in this study, as suggested in a previous report (43). If a vaccine against pandemic influenza is introduced only once a pandemic is imminent, all of the eight genes of the vaccine candidates could be derived from the pandemic strain to offer optimal protection to humans from virus infection. To reduce the risk of the emergence of the revertants, live attenuated virus vaccines should have multiple attenuating mutations in the genes that encode their internal proteins. NS1 mutant viruses are highly attenuated in mice because they lack interferon antagonist activity while retaining the ability to induce protective immunity against influenza virus challenge (45). Hence, by combining a mutant NS1 protein with the M2 tail deletion mutants identified in this study, an improved “master” influenza virus could be produced as a first step in the production of safe live influenza vaccines. Continued progress in understanding the functions of these influenza virus proteins should allow the introduction of multiple mutations in live vaccine strains, in addition to those in the HA, NS, and M genes, thereby reducing the likelihood of the emergence of pathogenic revertant viruses.
For live attenuated H5N1 virus vaccines to be clinically useful, the binding specificity of H5 HA for α-2,3-linked sialic acid (SA) receptors, which are preferentially recognized by avian influenza virus and rarely present in the upper respiratory tract of humans (8, 33, 34), must be considered. To address this problem, one could modify the H5 HA to alter its specificity for SA receptors. Recently, we (48) and others (1, 49) have determined specific amino acids in the avian H5 HA that alter its receptor-binding specificity toward α-2,6-SA (human-type receptor) recognition. This strategy may allow the generation of a recombinant H5N1-based vaccine that recognizes human-type α-2,6-SA receptors and efficiently replicates in the upper respiratory tract in humans.
Acknowledgments
We thank Susan Watson for editing the manuscript. We also thank Krisna Wells and Martha McGregor for excellent technical assistance.
Support for this work was provided by NIAID Public Health Service research grants and by the Japan Health Science Foundation and the Ministry of Education and Culture of Japan.
Footnotes
Published ahead of print on 26 December 2007.
REFERENCES
- 1.Auewarakul, P., O. Suptawiwat, A. Kongchanagul, C. Sangma, Y. Suzuki, K. Ungchusak, S. Louisirirotchanakul, H. Lerdsamran, P. Pooruk, A. Thitithanyanont, C. Pittayawonganon, C. T. Guo, H. Hiramatsu, W. Jampangern, S. Chunsutthiwat, and P. Puthavathana. 2007. An avian influenza H5N1 virus that binds to a human-type receptor. J. Virol. 819950-9955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bilsel, P., M. R. Castrucci, and Y. Kawaoka. 1993. Mutations in the cytoplasmic tail of influenza A virus neuraminidase affect incorporation into virions. J. Virol. 676762-6767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosch, F. X., W. Garten, H. D. Klenk, and R. Rott. 1981. Proteolytic cleavage of influenza virus hemagglutinins: primary structure of the connecting peptide between HA1 and HA2 determines proteolytic cleavability and pathogenicity of avian influenza viruses. Virology 113725-735. [DOI] [PubMed] [Google Scholar]
- 4.Bresson, J. L., C. Perronne, O. Launay, C. Gerdil, M. Saville, J. Wood, K. Hoschler, and M. C. Zambon. 2006. Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: phase I randomised trial. Lancet 3671657-1664. [DOI] [PubMed] [Google Scholar]
- 5.Castrucci, M. R., and Y. Kawaoka. 1995. Reverse genetics system for generation of an influenza A virus mutant containing a deletion of the carboxyl-terminal residue of M2 protein. J. Virol. 692725-2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cheung, C. L., J. M. Rayner, G. J. Smith, P. Wang, T. S. Naipospos, J. Zhang, K. Y. Yuen, R. G. Webster, J. S. Peiris, Y. Guan, and H. Chen. 2006. Distribution of amantadine-resistant H5N1 avian influenza variants in Asia. J. Infect. Dis. 1931626-1629. [DOI] [PubMed] [Google Scholar]
- 7.Claas, E. C., A. D. Osterhaus, R. van Beek, J. C. De Jong, G. F. Rimmelzwaan, D. A. Senne, S. Krauss, K. F. Shortridge, and R. G. Webster. 1998. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351472-477. [DOI] [PubMed] [Google Scholar]
- 8.Connor, R. J., Y. Kawaoka, R. G. Webster, and J. C. Paulson. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 20517-23. [DOI] [PubMed] [Google Scholar]
- 9.de Jong, M. D., T. T. Tran, H. K. Truong, M. H. Vo, G. J. Smith, V. C. Nguyen, V. C. Bach, T. Q. Phan, Q. H. Do, Y. Guan, J. S. Peiris, T. H. Tran, and J. Farrar. 2005. Oseltamivir resistance during treatment of influenza A (H5N1) infection. N. Engl. J. Med. 3532667-2672. [DOI] [PubMed] [Google Scholar]
- 10.Garten, W., F. X. Bosch, D. Linder, R. Rott, and H. D. Klenk. 1981. Proteolytic activation of the influenza virus hemagglutinin: the structure of the cleavage site and the enzymes involved in cleavage. Virology 115361-374. [DOI] [PubMed] [Google Scholar]
- 11.Hatta, M., P. Gao, P. Halfmann, and Y. Kawaoka. 2001. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 2931840-1842. [DOI] [PubMed] [Google Scholar]
- 12.Hay, A. J., A. J. Wolstenholme, J. J. Skehel, and M. H. Smith. 1985. The molecular basis of the specific anti-influenza action of amantadine. EMBO J. 43021-3024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helenius, A. 1992. Unpacking the incoming influenza virus. Cell 69577-578. [DOI] [PubMed] [Google Scholar]
- 14.Horimoto, T., K. Nakayama, S. P. Smeekens, and Y. Kawaoka. 1994. Proprotein-processing endoproteases PC6 and furin both activate hemagglutinin of virulent avian influenza viruses. J. Virol. 686074-6078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ilyushina, N. A., E. A. Govorkova, and R. G. Webster. 2005. Detection of amantadine-resistant variants among avian influenza viruses isolated in North America and Asia. Virology 341102-106. [DOI] [PubMed] [Google Scholar]
- 16.Iwatsuki-Horimoto, K., T. Horimoto, T. Noda, M. Kiso, J. Maeda, S. Watanabe, Y. Muramoto, K. Fujii, and Y. Kawaoka. 2006. The cytoplasmic tail of the influenza A virus M2 protein plays a role in viral assembly. J. Virol. 805233-5240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz, J. M., M. Wang, and R. G. Webster. 1990. Direct sequencing of the HA gene of influenza (H3N2) virus in original clinical samples reveals sequence identity with mammalian cell-grown virus. J. Virol. 641808-1811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kida, H., L. E. Brown, and R. G. Webster. 1982. Biological activity of monoclonal antibodies to operationally defined antigenic regions on the hemagglutinin molecule of A/Seal/Massachusetts/1/80 (H7N7) influenza virus. Virology 12238-47. [DOI] [PubMed] [Google Scholar]
- 19.Klenk, H. D., and W. Garten. 1994. Host cell proteases controlling virus pathogenicity. Trends Microbiol. 239-43. [DOI] [PubMed] [Google Scholar]
- 20.Lamb, R. A., S. L. Zebedee, and C. D. Richardson. 1985. Influenza virus M2 protein is an integral membrane protein expressed on the infected-cell surface. Cell 40627-633. [DOI] [PubMed] [Google Scholar]
- 21.Le, Q. M., M. Kiso, K. Someya, Y. T. Sakai, T. H. Nguyen, K. H. Nguyen, N. D. Pham, H. H. Ngyen, S. Yamada, Y. Muramoto, T. Horimoto, A. Takada, H. Goto, T. Suzuki, Y. Suzuki, and Y. Kawaoka. 2005. Avian flu: isolation of drug-resistant H5N1 virus. Nature 4371108. [DOI] [PubMed] [Google Scholar]
- 22.Li, K. S., Y. Guan, J. Wang, G. J. Smith, K. M. Xu, L. Duan, A. P. Rahardjo, P. Puthavathana, C. Buranathai, T. D. Nguyen, A. T. Estoepangestie, A. Chaisingh, P. Auewarakul, H. T. Long, N. T. Hanh, R. J. Webby, L. L. Poon, H. Chen, K. F. Shortridge, K. Y. Yuen, R. G. Webster, and J. S. Peiris. 2004. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature 430209-213. [DOI] [PubMed] [Google Scholar]
- 23.Lin, J., J. Zhang, X. Dong, H. Fang, J. Chen, N. Su, Q. Gao, Z. Zhang, Y. Liu, Z. Wang, M. Yang, R. Sun, C. Li, S. Lin, M. Ji, Y. Liu, X. Wang, J. Wood, Z. Feng, Y. Wang, and W. Yin. 2006. Safety and immunogenicity of an inactivated adjuvanted whole-virion influenza A (H5N1) vaccine: a phase I randomised controlled trial. Lancet 368991-997. [DOI] [PubMed] [Google Scholar]
- 24.Martin, K., and A. Helenius. 1991. Nuclear transport of influenza virus ribonucleoproteins: the viral matrix protein (M1) promotes export and inhibits import. Cell 67117-130. [DOI] [PubMed] [Google Scholar]
- 25.McCown, M. F., and A. Pekosz. 2006. Distinct domains of the influenza a virus M2 protein cytoplasmic tail mediate binding to the M1 protein and facilitate infectious virus production. J. Virol. 808178-8189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.McCown, M. F., and A. Pekosz. 2005. The influenza A virus M2 cytoplasmic tail is required for infectious virus production and efficient genome packaging. J. Virol. 793595-3605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neumann, G., T. Watanabe, H. Ito, S. Watanabe, H. Goto, P. Gao, M. Hughes, D. R. Perez, R. Donis, E. Hoffmann, G. Hobom, and Y. Kawaoka. 1999. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl. Acad. Sci. USA 969345-9350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nicholson, K. G., A. E. Colegate, A. Podda, I. Stephenson, J. Wood, E. Ypma, and M. C. Zambon. 2001. Safety and antigenicity of non-adjuvanted and MF59-adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 3571937-1943. [DOI] [PubMed] [Google Scholar]
- 29.Ochman, H., A. S. Gerber, and D. L. Hartl. 1988. Genetic applications of an inverse polymerase chain reaction. Genetics 120621-623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ohuchi, M., A. Cramer, M. Vey, R. Ohuchi, W. Garten, and H. D. Klenk. 1994. Rescue of vector-expressed fowl plague virus hemagglutinin in biologically active form by acidotropic agents and coexpressed M2 protein. J. Virol. 68920-926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pinto, L. H., L. J. Holsinger, and R. A. Lamb. 1992. Influenza virus M2 protein has ion channel activity. Cell 69517-528. [DOI] [PubMed] [Google Scholar]
- 32.Puthavathana, P., P. Auewarakul, P. C. Charoenying, K. Sangsiriwut, P. Pooruk, K. Boonnak, R. Khanyok, P. Thawachsupa, R. Kijphati, and P. Sawanpanyalert. 2005. Molecular characterization of the complete genome of human influenza H5N1 virus isolates from Thailand. J. Gen. Virol. 86423-433. [DOI] [PubMed] [Google Scholar]
- 33.Rogers, G. N., and B. L. D'Souza. 1989. Receptor binding properties of human and animal H1 influenza virus isolates. Virology 173317-322. [DOI] [PubMed] [Google Scholar]
- 34.Rogers, G. N., and J. C. Paulson. 1983. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglutinin based on species of origin. Virology 127361-373. [DOI] [PubMed] [Google Scholar]
- 35.Senne, D. A., B. Panigrahy, Y. Kawaoka, J. E. Pearson, J. Suss, M. Lipkind, H. Kida, and R. G. Webster. 1996. Survey of the hemagglutinin (HA) cleavage site sequence of H5 and H7 avian influenza viruses: amino acid sequence at the HA cleavage site as a marker of pathogenicity potential. Avian Dis. 40425-437. [PubMed] [Google Scholar]
- 36.Steinhauer, D. A. 1999. Role of hemagglutinin cleavage for the pathogenicity of influenza virus. Virology 2581-20. [DOI] [PubMed] [Google Scholar]
- 37.Stephenson, I., K. G. Nicholson, A. Colegate, A. Podda, J. Wood, E. Ypma, and M. Zambon. 2003. Boosting immunity to influenza H5N1 with MF59-adjuvanted H5N3 A/Duck/Singapore/97 vaccine in a primed human population. Vaccine 211687-1693. [DOI] [PubMed] [Google Scholar]
- 38.Stieneke-Grober, A., M. Vey, H. Angliker, E. Shaw, G. Thomas, C. Roberts, H. D. Klenk, and W. Garten. 1992. Influenza virus hemagglutinin with multibasic cleavage site is activated by furin, a subtilisin-like endoprotease. EMBO J. 112407-2414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Suarez, D. L., M. L. Perdue, N. Cox, T. Rowe, C. Bender, J. Huang, and D. E. Swayne. 1998. Comparisons of highly virulent H5N1 influenza A viruses isolated from humans and chickens from Hong Kong. J. Virol. 726678-6688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subbarao, K., A. Klimov, J. Katz, H. Regnery, W. Lim, H. Hall, M. Perdue, D. Swayne, C. Bender, J. Huang, M. Hemphill, T. Rowe, M. Shaw, X. Xu, K. Fukuda, and N. Cox. 1998. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279393-396. [DOI] [PubMed] [Google Scholar]
- 41.Sugrue, R. J., and A. J. Hay. 1991. Structural characteristics of the M2 protein of influenza A viruses: evidence that it forms a tetrameric channel. Virology 180617-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Suguitan, A. L., Jr., J. McAuliffe, K. L. Mills, H. Jin, G. Duke, B. Lu, C. J. Luke, B. Murphy, D. E. Swayne, G. Kemble, and K. Subbarao. 2006. Live, attenuated influenza A H5N1 candidate vaccines provide broad cross-protection in mice and ferrets. PLoS Med. 3e360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Takada, A., S. Matsushita, A. Ninomiya, Y. Kawaoka, and H. Kida. 2003. Intranasal immunization with formalin-inactivated virus vaccine induces a broad spectrum of heterosubtypic immunity against influenza A virus infection in mice. Vaccine 213212-3218. [DOI] [PubMed] [Google Scholar]
- 44.Takeuchi, K., and R. A. Lamb. 1994. Influenza virus M2 protein ion channel activity stabilizes the native form of fowl plague virus hemagglutinin during intracellular transport. J. Virol. 68911-919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Talon, J., M. Salvatore, R. E. O'Neill, Y. Nakaya, H. Zheng, T. Muster, A. Garcia-Sastre, and P. Palese. 2000. Influenza A and B viruses expressing altered NS1 proteins: a vaccine approach. Proc. Natl. Acad. Sci. USA 974309-4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Treanor, J. J., J. D. Campbell, K. M. Zangwill, T. Rowe, and M. Wolff. 2006. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. N. Engl. J. Med. 3541343-1351. [DOI] [PubMed] [Google Scholar]
- 47.World Health Organization. 2006. Avian influenza A (H5N1). Wkly. Epidemiol. Rec. 81249-260.16812929 [Google Scholar]
- 48.Yamada, S., Y. Suzuki, T. Suzuki, M. Q. Le, C. A. Nidom, Y. Sakai-Tagawa, Y. Muramoto, M. Ito, M. Kiso, T. Horimoto, K. Shinya, T. Sawada, M. Kiso, T. Usui, T. Murata, Y. Lin, A. Hay, L. F. Haire, D. J. Stevens, R. J. Russell, S. J. Gamblin, J. J. Skehel, and Y. Kawaoka. 2006. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature 444378-382. [DOI] [PubMed] [Google Scholar]
- 49.Yang, Z. Y., C. J. Wei, W. P. Kong, L. Wu, L. Xu, D. F. Smith, and G. J. Nabel. 2007. Immunization by avian H5 influenza hemagglutinin mutants with altered receptor binding specificity. Science 317825-828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zebedee, S. L., C. D. Richardson, and R. A. Lamb. 1985. Characterization of the influenza virus M2 integral membrane protein and expression at the infected-cell surface from cloned cDNA. J. Virol. 56502-511. [DOI] [PMC free article] [PubMed] [Google Scholar]