Abstract
Peptides based on heptad repeat (HR) domains of class I viral fusion proteins are considered promising antiviral drugs targeting virus cell entry. We have analyzed the evolution of the mouse hepatitis coronavirus during multiple passaging in the presence of an HR2-based fusion inhibitor. Drug-resistant variants emerged as a result of multiple substitutions in the spike fusion protein, notably within a 19-residue segment of the HR1 region. Strikingly, one mutation, an A1006V substitution, which consistently appeared first in four independently passaged viruses, was the main determinant of the resistance phenotype, suggesting that only limited options exist for escape from the inhibitory effect of the HR2 peptide.
Coronaviruses are important pathogens for humans and animals, as illustrated by the severe acute respiratory syndrome (SARS) coronavirus, which caused the global SARS epidemic in 2002-2003. Hence, there is a need for effective vaccines and antiviral therapeutics. While some progress has been made with the development of coronavirus vaccines (13), little success has been achieved in the search for antiviral therapies. For human immunodeficiency virus (HIV), the entry stage of the infection cycle has proven to be an attractive drug target (8). Entry of the enveloped coronaviruses is mediated by the viral spike (S) protein. The coronavirus S protein belongs to the class I viral fusion proteins (2), together with the fusion proteins of viruses of the orthomyxo-, retro-, paramyxo-, filo-, arena-, and baculoviridae. Class I fusion proteins mediate membrane fusion through extensive post-receptor-binding structural rearrangements in which two heptad repeat (HR) regions play a key role: HR1, positioned C-terminal of a hydrophobic fusion peptide, and HR2, located N-terminal of the transmembrane domain. It is hypothesized that upon anchoring of the fusion peptide in the target membrane, HR2 binds to the HR1 region in an antiparallel manner to form a stable six-helix bundle, with three HR1 fragments forming a central coiled coil surrounded by three coiled HR2 segments. The formation of this six-helix bundle is thought to mediate the juxtaposition of viral and cellular membranes, thereby facilitating the fusion process (for two recent reviews, see references 7 and 12). Peptides corresponding to the HR1 and HR2 regions were first shown for HIV to be potent virus inhibitors in vitro (6, 16, 17) and in vivo (8), most likely as a result of antagonistic binding to the HR regions within the fusion protein, thereby preventing hairpin formation and consequently membrane fusion. Similarly, we and others have shown that coronavirus entry can be effectively targeted by HR-derived peptides (1, 2, 9, 10, 18, 19, 21). Despite their effectiveness in vitro, the applicability of these HR homologues as therapeutics for treatment of coronavirus infections might be hampered by the emergence of drug-resistant viruses, as was illustrated by the development of clinical resistance of HIV against enfuvirtide, an HR2 peptide homologue (14).
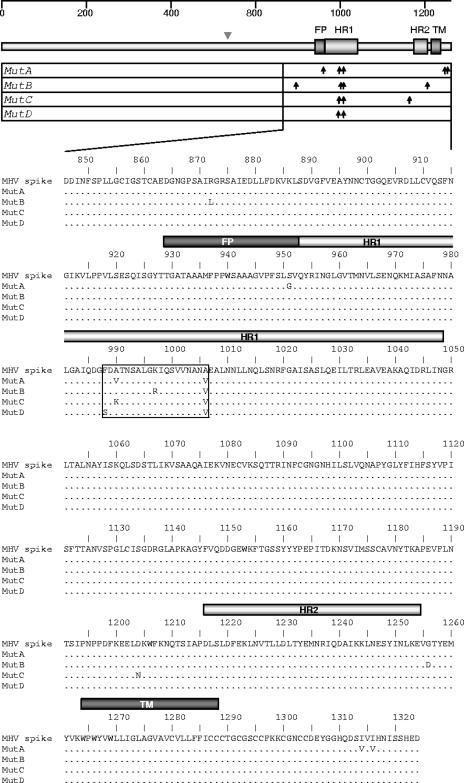
To analyze how a coronavirus would deal with the continuous presence of an HR2 peptide entry inhibitor, we passaged a recombinant mouse hepatitis virus (MHV; strain A59) expressing a Renilla luciferase reporter gene (MHV-ERLM) (3) in quadruplicate on LR7 cells at a high multiplicity of infection (∼10) for 10 rounds in the presence of 10 μM of the HR2 peptide (residues 1216 to 1254), which is known to inhibit the infection by ∼99% (2). Using the Renilla luciferase expression in infected cells as a readout (data not shown), we observed the gradual development of resistance toward the inhibitor. To identify mutations that might be responsible for this resistance, the entire spike gene of plaque-purified viruses from each series (MutA to MutD) was sequenced. We observed 14 amino acid substitutions, of which 8 localized to a 19-residue-long segment within the HR1 region (residues 988 to 1006) (Fig. 1). This segment directly interacts with the HR2 domain in the postfusion structure (20). Strikingly, within this stretch all the viruses contained an alanine-to-valine mutation at position 1006 (A1006V), which was accompanied by at least one additional substitution. In both MutA and MutC, the alanine at position 990 was mutated, though differently. In MutA, the mutation resulted in a valine through a single nucleotide change (GCA→GTA). A two-nucleotide change (GCA→AAA) resulting in an alanine-to-lysine mutation was found in the A990 codon of virus C. MutB and MutD exhibited, in addition to A1006V, a K997R and an F988S substitution, respectively. Outside the HR1 region, MutA had three mutations, one of them located within the putative fusion peptide (S951G) and two within the cytoplasmic tail (I1314V and I1316V); MutB contained a mutation upstream of the HR1 region (R867L) and a substitution carboxy-terminal of the HR2 region (G1256D), whereas MutC had one mutation located amino-terminal of the HR2 region (D1204N).
FIG. 1.
Sequence analysis of MHV viruses cultured in quadruplicate for 10 passages in the continuous presence of the HR2 entry inhibitor. (Upper) Schematic representation of the MHV-A59 spike protein. The fusion peptide (FP), HR1 and HR2 regions, and transmembrane region (TM) are indicated by gray bars. The furin cleavage site is indicated by an arrowhead. The arrows indicate the positions of the observed mutations in the spike genes of the four viruses (MutA to -D), which were independently passaged in the presence of 10 μM HR2 peptide. (Lower) Sequences of the MHV-A59 spike protein (residues 840 to 1324) with the mutations. Sequences of clones are aligned to the wild-type spike sequence. Dots mark amino acids that are identical. The bars indicate the positions of the FP, HR1, HR2, and TM regions. The boxed sequence marks the 19-residue segment within the HR1 region (residues 988 to 1006) containing 8 out of 14 mutations.
In MutD, both mutations localized to the HR1 region, suggesting that changes within the HR1 region alone can confer HR2 resistance. We therefore verified first whether the mutations in this HR1 region accounted for the observed phenotype by introducing these mutations of each mutant virus into the parental virus MHV-ERLM. Mutations were transferred into the MHV genome by targeted RNA recombination as described previously (3), yielding Renilla luciferase-expressing MHVs carrying S proteins with the S951G-A990V-A1006V (RecA), the R867L-K997R-A1006V (RecB), the A990K-A1006V (RecC), or the F988S-A1006V (RecD) mutations. The presence of the mutations in recombinant viruses was confirmed by reverse transcription-PCR sequence analysis.
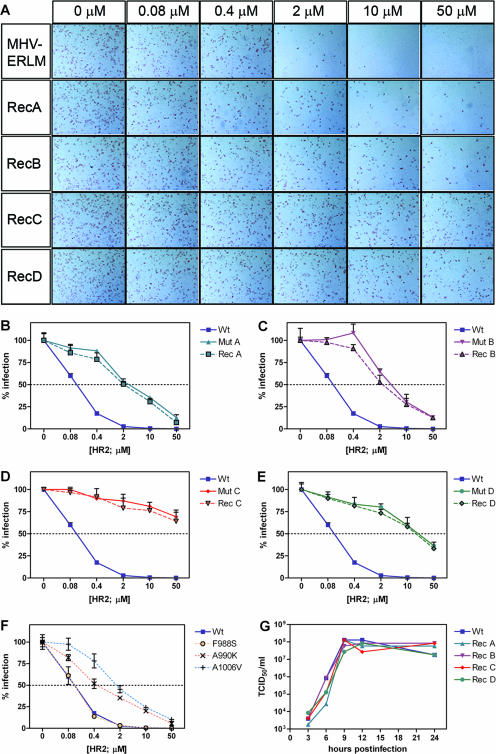
The possible effects of the introduced mutations on the growth characteristics of the recombinant viruses were checked by comparing the replication kinetics and yields of infectious virus with those of the parental virus. Murine LR7 cells were infected at a high multiplicity of infection (of 5) to obtain synchronous starting of the infection in all cells. Unabsorbed virus was washed away at 1 h postinoculation, and virus release into the medium was subsequently analyzed by performing a 50% tissue culture infectious dose assay with samples taken at different time points after infection. The recombinant viruses and parental virus MHV-ERLM showed comparable replication kinetics and yields (Fig. 2G), indicating that the introduced substitutions did not appreciably alter the viral growth properties.
FIG. 2.
Effects of HR1 mutations on HR2 peptide susceptibility and virus replication. (A) HR2 peptide susceptibilities of recombinant viruses (RecA to -D) and the parental virus MHV-ERLM (Wt). (B to F) HR2 peptide susceptibilities of mutant viruses (MutA to -D), recombinant viruses (RecA to -D), recombinant viruses containing single-amino-acid substitutions (F988S, A990K, or A1006V), and the parental virus (MHV-ERLM). (G) Single-step growth curve of the parental virus (MHV-ERLM) and recombinant viruses (RecA to -D).
The HR2 sensitivities of the recombinant viruses (RecA to -D) were subsequently compared with that of the parental virus MHV-ERLM in a single-round infection assay (Fig. 2A). Parallel cultures of LR7 cells were inoculated in the presence of increasing HR2 peptide concentrations, and infected cells were detected using an immunoperoxidase assay as described previously (1). As Fig. 2A illustrates, the introduced amino acid substitutions of all recombinants clearly conferred resistance toward the HR2 peptide entry inhibitor. Next, the recombinant viruses (RecA to -D) and the parental virus MHV-ERLM were analyzed together with the mutant viruses (MutA to -D) for their HR2 peptide sensitivities by using the assay described above, after which the number of infected cells was scored (Fig. 2B to E). The analyses were performed in triplicate in two independent experiments. For each virus, 50% inhibitory concentration (IC50) values were calculated and the results are combined in Table 1. All mutant viruses appeared to be less sensitive to the HR2 peptide than the parental virus (21- to 170-fold increases in IC50 values). Because the recombinant mutant viruses (RecA to -D) exhibited sensitivities almost identical to those of the corresponding mutant viruses (MutA to -D), the resistance phenotypes appear to be largely determined by the mutations in the HR1 region, with only a slight contribution of the additional substitutions in other regions. Of the recombinant viruses, RecC and RecD displayed the strongest reductions in susceptibility to the HR2 inhibitor, suggesting that the substitutions in RecC and RecD (F988S, A990K, and A1006V), all located in the HR1 region, play a key role. Therefore, we addressed the contributions of these individual mutations to HR2 peptide resistance. After introduction of these mutations into the parental transfer vector by site-directed mutagenesis, recombinant viruses carrying single HR1 mutations (F988S, A990K, or A1006V) were generated as described above and assayed for their abilities to contribute to HR2 peptide resistance (Fig. 2F). Clearly, the A1006V mutation had the strongest effect and was predominantly responsible for the resistance phenotypes of mutants A and B. The A990K substitution also significantly affected HR2 peptide sensitivity. The F988S substitution by itself did not confer HR2 peptide resistance. However, in combination with the A1006V substitution, both F988S and A990K further enhanced the resistance, as seen in RecD and RecC, respectively, indicating a synergistic effect of the mutations.
TABLE 1.
HR2 susceptibilities of MHV viruses containing wild-type and mutated spikesa
| Virus | Substitution for indicated spike amino acid | IC50 (μM)b | Fold resistance | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MHV-ERLM | R867 | S951 | F988 | A990 | K997 | A1006 | D1204 | G1256 | I1314 | I1316 | 0.12 | 1.0 |
| MutA | G | V | V | V | V | 2.71 | 23.4 | |||||
| RecA | G | V | V | 2.03 | 17.5 | |||||||
| MutB | L | R | V | D | 3.95 | 34.1 | ||||||
| RecB | L | R | V | 2.45 | 21.1 | |||||||
| MutC | K | V | N | >50 | >416 | |||||||
| RecC | K | V | >50 | >416 | ||||||||
| MutD | S | V | 19.7 | 169.8 | ||||||||
| RecD | S | V | 16.5 | 142.2 | ||||||||
| F988S | S | 0.12 | 1,0 | |||||||||
| A990K | K | 0.48 | 4.1 | |||||||||
| A1006V | V | 1.6 | 13.6 | |||||||||
The spike protein amino acid substitutions are indicated with respect to the parental MHV-ERLM spike protein. Boldface marks the amino acids residing within the HR1 region.
Calculated from two replicate experiments performed in triplicate.
Further sequence analysis of viruses from earlier passages showed that the A1006V mutation was the first one appearing in the HR1 region, arising between passages 3 and 7. The other mutations were generally acquired later during passaging. The mutations were subsequently maintained, suggesting that they conferred an adaptive advantage to the virus. In addition, the mutations appeared to be stable in RecA to -D viruses for another 10 rounds of passaging, now in the absence of the HR2 peptide (data not shown). This observation indicates that the mutations conferred a stable phenotype to the virus, consistent with the unaltered growth kinetics (Fig. 2G). Sequence analysis of HR2-resistant MHV-A59 viruses which were generated in an independent experiment upon repeated in vitro passaging in the presence of gradually increasing HR2 concentrations (data not shown) revealed that the virus consistently acquired the A1006V substitution in the HR1 region. These data suggest that there are a limited number of options by which the virus can overcome the inhibitory effect of the HR2 peptide are limited.
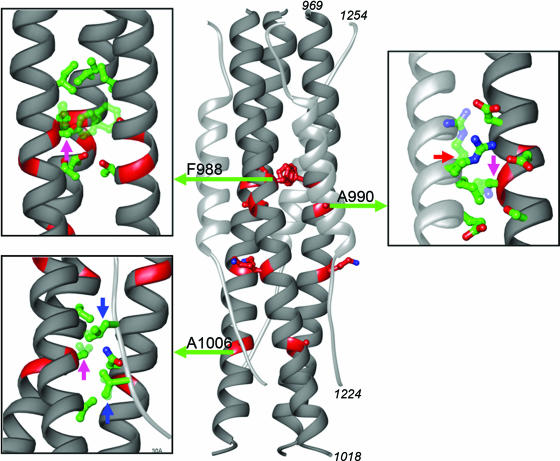
Central to the fusion process of class I viruses is the formation of the stable six-helix bundle in which HR2 regions assemble into the grooves formed by the trimeric HR1 coiled coil. Six-helix-bundle formation contributes critically to the energy needed for the membrane merger. Virus inhibition by the exogenous HR2 peptide can logically be explained by interference with six-helix-bundle formation through competitive binding to the HR1 region. It hence seems equally logical that viruses escape from the inhibitory pressure imposed by the HR2-derived peptides as a result of changes in these peptides' target site, the HR1 region. Paradoxically, these mutations have to preserve the effective, strong interaction with the HR2 region, which they appeared to do, in view of the wild-type-like infection properties of the escape mutant viruses. Consistent with this line of reasoning, the available HR1/HR2 postfusion structure of the MHV-A59 spike protein (20) reveals that none of the residues changed in the HR1 domain under the pressure of the HR2 peptide impose inevitable sterical hindrance to HR2 binding (Fig. 3). The A1006V and A990K substitutions lie at the interface of HR1 and HR2 but do not notably seem to destabilize HR1-HR2 interactions. Accommodation of the valine side chain of the A1006V substitution requires just a slight movement of the V1226 and L1228 side chains, whereas the lysine side chain of the A990K substitution can be accommodated relatively easily after slight movement of the arginine side chain (R1237) of the neighboring HR2 region, which can then interact with acidic residues. While this structural information explains why the mutant spikes are still fusion active, it does not provide insight into the mechanism of HR2 peptide inhibition.
FIG. 3.
Ribbon diagram of the fusion core structure of MHV (PDB 1WDF) (20), with the HR1 (residues 969 to 1018) and HR2 (residues 1224 to 1254) peptides in dark and light gray, respectively, and the mutated residues (F988, A990, K997, and A1006) indicated. The insets show modeling of the F988S, A990K, and A1006V substitutions. The magenta arrows point at the green-colored side chains, with faded green representing the substituted side chain (A990K and A1006V) and solid green the original side chain (F988S). The blue arrows indicate the V1226 (lower arrow) and L1228 (upper arrow) side chains, and the red arrow points to the R1237 side chain, with faded green representing the movements of the side chains required to accommodate the V1006-and-K990 side chain.
Another possibility is that the acquired HR1 mutations influence the prefusion and intermediate structures of the spike protein. Intriguingly, the F988S, A990V, and A990K substitutions reside within the stretch of residues lining the central cavity, which is reported to have a destabilizing effect on the HR1 trimeric coiled coil of the SARS coronavirus spike protein (4). Mutations in a paramyxovirus fusion protein that destabilize the HR1 coiled coil result in stimulation of membrane fusion (15). The mutations in the HR1 domain might therefore influence the kinetics of spike protein refolding by affecting the stability of the spike protein, which in the case of HIV has been shown to be a critical determinant for enfuvirtide sensitivity (5, 11). However, further studies will be required to fully understand how these amino acid substitutions in the HR1 region contribute to the resistance of coronavirus toward the HR2 peptide fusion inhibitor.
Acknowledgments
B.J.B. is supported by VENI grant 016.062.027 from The Netherlands Organization for Scientific Research (NWO).
Footnotes
Published ahead of print on 12 December 2007.
REFERENCES
- 1.Bosch, B. J., B. E. Martina, R. Van Der Zee, J. Lepault, B. J. Haijema, C. Versluis, A. J. Heck, R. De Groot, A. D. Osterhaus, and P. J. Rottier. 2004. Severe acute respiratory syndrome coronavirus (SARS-CoV) infection inhibition using spike protein heptad repeat-derived peptides. Proc. Natl. Acad. Sci. USA 1018455-8460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bosch, B. J., R. van der Zee, C. A. de Haan, and P. J. Rottier. 2003. The coronavirus spike protein is a class I virus fusion protein: structural and functional characterization of the fusion core complex. J. Virol. 778801-8811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Haan, C. A., L. van Genne, J. N. Stoop, H. Volders, and P. J. Rottier. 2003. Coronaviruses as vectors: position dependence of foreign gene expression. J. Virol. 7711312-11323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duquerroy, S., A. Vigouroux, P. J. Rottier, F. A. Rey, and B. J. Bosch. 2005. Central ions and lateral asparagine/glutamine zippers stabilize the post-fusion hairpin conformation of the SARS coronavirus spike glycoprotein. Virology 335276-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gallo, S. A., K. Sackett, S. S. Rawat, Y. Shai, and R. Blumenthal. 2004. The stability of the intact envelope glycoproteins is a major determinant of sensitivity of HIV/SIV to peptidic fusion inhibitors. J. Mol. Biol. 3409-14. [DOI] [PubMed] [Google Scholar]
- 6.Jiang, S., K. Lin, N. Strick, and A. R. Neurath. 1993. HIV-1 inhibition by a peptide. Nature 365113. [DOI] [PubMed] [Google Scholar]
- 7.Kielian, M., and F. A. Rey. 2006. Virus membrane-fusion proteins: more than one way to make a hairpin. Nat. Rev. Microbiol. 467-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kilby, J. M., S. Hopkins, T. M. Venetta, B. DiMassimo, G. A. Cloud, J. Y. Lee, L. Alldredge, E. Hunter, D. Lambert, D. Bolognesi, T. Matthews, M. R. Johnson, M. A. Nowak, G. M. Shaw, and M. S. Saag. 1998. Potent suppression of HIV-1 replication in humans by T-20, a peptide inhibitor of gp41-mediated virus entry. Nat. Med. 41302-1307. [DOI] [PubMed] [Google Scholar]
- 9.Liu, S., G. Xiao, Y. Chen, Y. He, J. Niu, C. R. Escalante, H. Xiong, J. Farmar, A. K. Debnath, P. Tien, and S. Jiang. 2004. Interaction between heptad repeat 1 and 2 regions in spike protein of SARS-associated coronavirus: implications for virus fusogenic mechanism and identification of fusion inhibitors. Lancet 363938-947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pyrc, K., B. J. Bosch, B. Berkhout, M. F. Jebbink, R. Dijkman, P. Rottier, and L. van der Hoek. 2006. Inhibition of human coronavirus NL63 infection at early stages of the replication cycle. Antimicrob. Agents Chemother. 502000-2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reeves, J. D., S. A. Gallo, N. Ahmad, J. L. Miamidian, P. E. Harvey, M. Sharron, S. Pohlmann, J. N. Sfakianos, C. A. Derdeyn, R. Blumenthal, E. Hunter, and R. W. Doms. 2002. Sensitivity of HIV-1 to entry inhibitors correlates with envelope/coreceptor affinity, receptor density, and fusion kinetics. Proc. Natl. Acad. Sci. USA 9916249-16254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schibli, D. J., and W. Weissenhorn. 2004. Class I and class II viral fusion protein structures reveal similar principles in membrane fusion. Mol. Membr. Biol. 21361-371. [DOI] [PubMed] [Google Scholar]
- 13.Stadler, K., and R. Rappuoli. 2005. SARS: understanding the virus and development of rational therapy. Curr. Mol. Med. 5677-697. [DOI] [PubMed] [Google Scholar]
- 14.Wei, X., J. M. Decker, H. Liu, Z. Zhang, R. B. Arani, J. M. Kilby, M. S. Saag, X. Wu, G. M. Shaw, and J. C. Kappes. 2002. Emergence of resistant human immunodeficiency virus type 1 in patients receiving fusion inhibitor (T-20) monotherapy. Antimicrob. Agents Chemother. 461896-1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.West, D. S., M. S. Sheehan, P. K. Segeleon, and R. E. Dutch. 2005. Role of the simian virus 5 fusion protein N-terminal coiled-coil domain in folding and promotion of membrane fusion. J. Virol. 791543-1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wild, C., T. Greenwell, and T. Matthews. 1993. A synthetic peptide from HIV-1 gp41 is a potent inhibitor of virus-mediated cell-cell fusion. AIDS Res. Hum. Retrovir. 91051-1053. [DOI] [PubMed] [Google Scholar]
- 17.Wild, C. T., D. C. Shugars, T. K. Greenwell, C. B. McDanal, and T. J. Matthews. 1994. Peptides corresponding to a predictive alpha-helical domain of human immunodeficiency virus type 1 gp41 are potent inhibitors of virus infection. Proc. Natl. Acad. Sci. USA 919770-9774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Würdinger, T., M. H. Verheije, K. Broen, B. J. Bosch, B. J. Haijema, C. A. de Haan, V. W. van Beusechem, W. R. Gerritsen, and P. J. Rottier. 2005. Soluble receptor-mediated targeting of mouse hepatitis coronavirus to the human epidermal growth factor receptor. J. Virol. 7915314-15322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wurdinger, T., M. H. Verheije, M. Raaben, B. J. Bosch, C. A. de Haan, V. W. van Beusechem, P. J. Rottier, and W. R. Gerritsen. 2005. Targeting non-human coronaviruses to human cancer cells using a bispecific single-chain antibody. Gene. Ther. 121394-1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu, Y., Y. Liu, Z. Lou, L. Qin, X. Li, Z. Bai, H. Pang, P. Tien, G. F. Gao, and Z. Rao. 2004. Structural basis for coronavirus-mediated membrane fusion. Crystal structure of mouse hepatitis virus spike protein fusion core. J. Biol. Chem. 27930514-30522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuan, K., L. Yi, J. Chen, X. Qu, T. Qing, X. Rao, P. Jiang, J. Hu, Z. Xiong, Y. Nie, X. Shi, W. Wang, C. Ling, X. Yin, K. Fan, L. Lai, M. Ding, and H. Deng. 2004. Suppression of SARS-CoV entry by peptides corresponding to heptad regions on spike glycoprotein. Biochem. Biophys. Res. Commun. 319746-752. [DOI] [PMC free article] [PubMed] [Google Scholar]