Abstract
Background
Suicide is a leading cause of death world-wide; however, the prevalence and risk factors for the immediate precursors to suicide: suicidal ideation, plans and attempts, are not well-known, especially in developing countries.
Aims
To report on the prevalence and risk factors for suicidal behaviors across 17 countries.
Method
84,850 adults were interviewed regarding suicidal behaviors and socio-demographic and psychiatric risk factors.
Results
The cross-national lifetime prevalence (standard error) of suicidal ideation, plans, and attempts is 9.2% (0.1), 3.1% (0.1), and 2.7% (0.1). Across all countries, 60% of transitions from ideation to plan and attempt occur within the first year after ideation onset. Consistent cross-national risk factors included being: female, younger, less educated, unmarried, and having a mental disorder. Interestingly, the strongest diagnostic risk factors were mood disorders in developed countries but impulse-control disorders in developing countries.
Conclusion
Despite cross-national variability in prevalence, there is strong consistency in the characteristics of and risk factors for suicidal behaviors. These findings have significant implications for the prediction and prevention of suicidal behaviors.
Suicide is among the leading causes of death worldwide.1 Yet, basic data on the prevalence and risk factors for suicide and its immediate precursors: suicidal ideation, plans, and attempts, are unavailable in many countries around the world, particularly those that are less developed.2 Most studies of suicidal thoughts and behaviors (hereafter “suicidal behaviors”) have been conducted within individual, Western, developed countries3–6 and it is not known whether prevalence estimates and risk factors identified in such studies generalize beyond these countries. Recent studies in several developing countries such as China and India suggest the occurrence of suicidal behaviors may differ markedly from developed countries. For instance, this work suggests that gender and the presence of mental disorders play less of a role in the occurrence of suicidal behaviors in developing countries.7,8 Data on suicidal behaviors collected cross-nationally would provide a unique opportunity to evaluate the consistency of prevalence estimates and risk factors for these important outcomes, and would greatly inform research, policy, and treatment efforts more broadly aimed at understanding and preventing suicide around the world.1,9
The purpose of the current study was to estimate the cross-national prevalence of suicidal behaviors and to examine risk factors for these outcomes using data from the World Health Organization (WHO) World Mental Health (WMH) Survey Initiative.10 Several studies have provided valuable information about suicidal behaviors across several countries.5,11,12 The current study extends prior work by conducting a more thorough examination of suicidal behaviors, using more consistent assessment methods across sites, and represents the largest, most representative examination of suicidal behaviors ever conducted.
METHOD
Respondent Samples
The WMH surveys were carried out in 17 countries in: Africa (Nigeria; South Africa); the Americas (Colombia; Mexico; United States), Asia and the Pacific (Japan; New Zealand; Beijing and Shanghai in the Peoples Republic of China), Europe (Belgium; France; Germany; Italy; the Netherlands; Spain; Ukraine);13 and the Middle East (Israel; Lebanon). The World Bank14 classifies China, Colombia, Lebanon, Mexico, Nigeria, South Africa, and Ukraine as less developed or developing countries; and all other survey countries as developed. All surveys were conducted face-to-face by trained lay interviewers among multi-stage household probability samples (described in Table 1). The total sample size was 84,850, with individual country sample sizes ranging from 2,372 in the Netherlands to 12,992 in New Zealand. The weighted average response rate across all countries was 71.1%.
Table 1.
Sample Characteristics
| Country | Survey1 | Sample Characteristics2 | Field Dates | Age Range | Sample Size | Response Rate | ||
|---|---|---|---|---|---|---|---|---|
| Part I | Part II | Part II and Age ≤ 444 | ||||||
| Belgium | ESEMeD | Stratified multistage clustered probability sample of individuals residing in households from the national register of Belgium residents. NR | 2001–2 | 18+ | 2419 | 1043 | 486 | 50.6 |
| Colombia | NSMH | Stratified multistage clustered area probability sample of household residents in all urban areas of the country (approximately 73% of the total national population) | 2003 | 18–65 | 4426 | 2381 | 1731 | 87.7 |
| France | ESEMeD | Stratified multistage clustered sample of working telephone numbers merged with a reverse directory (for listed numbers). Initial recruitment was by telephone, with supplemental in-person recruitment in households with listed numbers. NR | 2001–2 | 18+ | 2894 | 1436 | 727 | 45.9 |
| Germany | ESEMeD | Stratified multistage clustered probability sample of individuals from community resident registries. NR | 2002–3 | 18+ | 3555 | 1323 | 621 | 57.8 |
| Italy | ESEMeD | Stratified multistage clustered probability sample of individuals from municipality resident registries. NR | 2001–2 | 18+ | 4712 | 1779 | 853 | 71.3 |
| Israel | NHS | Stratified multistage clustered area probability sample from national register of Israeli residents. NR | 2002–4 | 21+ | 4859 | -- | -- | 72.6 |
| Japan | WMHJ2002-2003 | Un-clustered two-stage probability sample of individuals residing in households in four metropolitan areas (Fukiage, Kushikino, Nagasaki, Okayama) | 2002–3 | 20+ | 2436 | 887 | 282 | 56.4 |
| Lebanon | LEBANON | Stratified multistage clustered area probability sample of household residents. NR | 2002–3 | 18+ | 2857 | 1031 | 595 | 70.0 |
| Mexico | M-NCS | Stratified multistage clustered area probability sample of household residents in all urban areas of the country (approximately 75% of the total national population). | 2001–2 | 18–65 | 5782 | 2362 | 1736 | 76.6 |
| Netherlands | ESEMeD | Stratified multistage clustered probability sample of individuals residing in households that are listed in municipal postal registries. NR | 2002–3 | 18+ | 2372 | 1094 | 516 | 56.4 |
| New Zealand | NZMHS | Stratified multistage clustered area probability sample of household residents. NR | 2004–5 | 16+ | 12992 | 7435 | 4242 | 73.3 |
| Nigeria | NSMHW | Stratified multistage clustered area probability sample of households in 21 of the36 states in the country, representing 57% of the national population. The surveys were conducted in Yoruba, Igbo, Hausa and Efik languages. | 2002–3 | 18+ | 6752 | 2143 | 1203 | 79.3 |
| PRC5 Beijing | B-WMH | Stratified multistage clustered area probability sample of household residents in the Beijing metropolitan area. | 2002–3 | 18+ | 2633 | 914 | 307 | 74.8 |
| PRC5 Shanghai | S-WMH | Stratified multistage clustered area probability sample of household residents in the Shanghai metropolitan area. | 2002–3 | 18+ | 2568 | 714 | 263 | 74.6 |
| South Africa | SASH | Stratified multistage clustered area probability sample of household residents. NR | 2003–4 | 18+ | 4315 | -- | -- | 87.1 |
| Spain | ESEMeD | Stratified multistage clustered area probability sample of household residents. NR | 2001–2 | 18+ | 5473 | 2121 | 960 | 78.6 |
| Ukraine | CMDPSD | Stratified multistage clustered area probability sample of household residents. NR | 2002 | 18+ | 4725 | 1720 | 541 | 78.3 |
| United States | NCS-R | Stratified multistage clustered area probability sample of household residents. NR | 2002–3 | 18+ | 9282 | 5692 | 3197 | 70.9 |
ESEMeD (The European Study Of The Epidemiology Of Mental Disorders); NSMH (The Colombian National Study of Mental Health); NHS (Israel National Health Survey); WMHJ2002-2003 (World Mental Health Japan Survey); LEBANON (Lebanese Evaluation of the Burden of Ailments and Needs of the Nation); M-NCS (The Mexico National Comorbidity Survey); NZMHS (New Zealand Mental Health Survey); NSMHW (The Nigerian Survey of Mental Health and Wellbeing); B-WMH (The Beijing World Mental Health survey); S-WMH (The Shanghai World Mental Health Survey); SASH (South Africa Health Survey); CMDPSD (Comorbid Mental Disorders during Periods of Social Disruption); NCS-R (The US National Comorbidity Survey Replication).
Most WMH surveys are based on stratified multistage clustered area probability household samples in which samples of areas equivalent to counties or municipalities in the US were selected in the first stage followed by one or more subsequent stages of geographic sampling (e.g., towns within counties, blocks within towns, households within blocks) to arrive at a sample of households, in each of which a listing of household members was created and one or two people were selected from this listing to be interviewed. No substitution was allowed when the originally sampled household resident could not be interviewed. These household samples were selected from Census area data in all countries other than France (where telephone directories were used to select households) and the Netherlands (where postal registries were used to select households). Several WMH surveys (Belgium, Germany, Italy) used municipal resident registries to select respondents without listing households. The Japanese sample is the only totally un-clustered sample, with households randomly selected in each of the four sample areas and one random respondent selected in each sample household. Nine of the 15 surveys are based on nationally representative (NR) household samples, while two others are based on nationally representative household samples in urbanized areas (Colombia, Mexico).
The response rate is calculated as the ratio of the number of households in which an interview was completed to the number of households originally sampled, excluding from the denominator households known not to be eligible either because of being vacant at the time of initial contact or because the residents were unable to speak the designated languages of the survey.
All countries, with the exception of Nigeria, PRC Beijing, PRC Shanghai, and Ukraine (which were age restricted to ≤ 39) were age restricted to ≤ 44.
People’s Republic of China
Procedures
All respondents completed a Part I interview that contained core diagnostic assessments, including the assessment of suicidal behaviors. All Part I respondents who met criteria for any disorder and a sub-sample of approximately 25% of the rest of the respondents were administered a Part II interview that assessed potential correlates and disorders of secondary interest (n=48,427). Data were weighted to adjust for this differential sampling of Part II respondents, differential probabilities of selection within households, and to match samples to population socio-demographic distributions.
Standardized interviewer training procedures, WHO translation protocols for all study materials, and quality control procedures for interviewer and data accuracy that have been consistently employed across all WMH countries are described in more detail elsewhere 10,15,16. Informed consent was obtained before beginning interviews in all countries. Procedures for obtaining informed consent and protecting human subjects were approved and monitored for compliance by the Institutional Review Boards of organizations coordinating surveys in each country.
Measures of suicidal behaviors
Suicidal ideation, plans, and attempts were assessed using Version 3.0 of the WHO Composite International Diagnostic Interview (CIDI).16 Based on evidence that reports of such potentially embarrassing behaviors are higher in self-administered than interviewer-administered surveys,17 these questions were printed in a self-administered booklet and referred to by letter (e.g., “Did experience C ever happen to you?” In booklet, “C=You attempted suicide”). In cases in which the respondent was unable to read, the interviewer read these items aloud (19.5% of all cases). Interviews assessed the lifetime presence and age-of-onset (AOO) of each outcome.
Risk factors for suicidal behaviors
Interviews also examined three sets of risk factors for suicidal behaviors: socio-demographics, characteristics of suicidal behaviors, and temporally prior DSM-IV mental disorders (i.e., those with an onset prior to the first onset of suicidal ideation). The socio-demographic factors included sex, age/cohort, education, employment history, and marital history. Characteristics of suicidal behaviors included AOO of ideation, time since onset of ideation, presence of a suicide plan, and time since onset of plan. Respondent disorders were assessed using the WHO CIDI.16 The assessment included DSM-IV mood, anxiety, impulse-control, and substance use disorders. Prior studies using clinical reappraisal interviews have found CIDI diagnoses to have good concordance with blinded diagnoses based on the Structured Clinical Interview for DSM-IV18 in probability sub-samples of respondents from the France, Italy, Spain, and US surveys.19,20
Statistical analysis
Cross-tabulations were used to estimate lifetime prevalence of suicidal ideation, plans, and attempts. Discrete-time survival analysis with person-year as the unit of analysis and including both stable (e.g., gender) and time-varying (e.g., marital history) covariates21 was used to study retrospectively assessed risk factors for the first onset of each suicidal behavior. Discrete-time survival analysis uses each year of life of each respondent as a separate observation, so that a sample of 100,000 respondents with an average age of 30 would be treated as 3 million separate records. Each record is coded for the respondent’s stable characteristics (e.g., gender), the respondent’s age at the time of the observational record (e.g., the 20th year of life of a respondent who was age 45 at the time of interview), values on the time-varying predictors as of that year of life (e.g., whether or not the respondent was still a student, had ever been married, and had ever been employed as of age 20), and values on the outcomes as of that year (e.g., whether or not the respondent had ever made a suicide attempt and, if so, if this was the year of the respondent’s first lifetime attempt). The data file was analyzed to compare person-years for all respondents that had never had the outcome of interest versus the year of first onset of the outcome using a logistic regression modelling approach and controlling for person-year (i.e., age at the time of the observational record) as well as for the predictors. Logistic regression coefficients were converted to odd-ratios (ORs) for ease of interpretation and 95% confidence intervals (CI’s) are also reported and have been adjusted for design effects. Continuous variables were divided into categories to minimize effects of extreme values. Standard errors (SE) and significance tests were estimated using the Taylor series method22 using SUDAAN software23 to adjust for the effects of weighting and clustering. Multivariate significance was evaluated using Wald χ2 tests based on design-corrected coefficient variance-covariance matrices. Statistical significance was evaluated using two-tailed .05-level tests.
RESULTS
Prevalence
The estimated lifetime prevalence (SE) of suicidal ideation, plan, and attempt in the overall cross-national sample is 9.2% (0.1), 3.1% (0.1), and 2.7% (0.1), respectively (Table 2a). Among suicide ideators, the conditional probability of ever making a suicide plan is 33.6% (0.7) and of ever making a suicide attempt is 29.0% (0.6). The probability of attempt among ideators with a plan is 56.0% (1.2) but only 15.4% (0.6) among those without a plan (Table 2b).
Table 2.
Table 2a. Lifetime Prevalence of Suicide-Related Outcomes in the WMH Surveys
Table 2b. Lifetime Prevalence of Suicide-Related Outcomes in the WMH Surveys
| Total Sample
|
||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | ||||||||||||||
| % | (se) | (sd) | (n) | % | (se) | (sd) | (n) | % | (se) | (sd) | (n) | |||||
| The Americas | ||||||||||||||||
| Colombia | 12.4** | (0.7) | (46.6) | (587) | 4.1** | (0.4) | (26.6) | (204) | 4.7** | (0.4) | (26.6) | (224) | ||||
| Mexico | 8.1* | (0.5) | (38.0) | (488) | 3.2 | (0.3) | (22.8) | (192) | 2.7 | (0.3) | (22.8) | (166) | ||||
| USA | 15.6** | (0.5) | (48.2) | (1462) | 5.4** | (0.3) | (28.9) | (507) | 5.0** | (0.2) | (19.3) | (469) | ||||
| Europe | ||||||||||||||||
| Belgium | 8.4 | (0.9) | (44.3) | (209) | 2.7 | (0.4) | (19.7) | (77) | 2.5 | (0.4) | (19.7) | (66) | ||||
| France | 12.4** | (0.7) | (37.7) | (391) | 4.4** | (0.4) | (21.5) | (143) | 3.4 | (0.4) | (21.5) | (115) | ||||
| Germany | 9.7 | (0.7) | (41.7) | (347) | 2.2* | (0.3) | (17.9) | (78) | 1.7* | (0.3) | (17.9) | (64) | ||||
| Italy | 3.0* | (0.3) | (20.6) | (144) | 0.7* | (0.1) | (6.9) | (33) | 0.5* | (0.1) | (6.9) | (26) | ||||
| Netherlands | 8.2 | (0.6) | (29.2) | (223) | 2.7 | (0.5) | (24.4) | (78) | 2.3 | (0.3) | (14.6) | (64) | ||||
| Spain | 4.4* | (0.3) | (22.2) | (272) | 1.4* | (0.2) | (14.8) | (84) | 1.5* | (0.2) | (14.8) | (80) | ||||
| Ukraine | 8.2* | (0.5) | (34.4) | (389) | 2.7 | (0.3) | (20.6) | (126) | 1.8* | (0.2) | (13.7) | (80) | ||||
| Africa & the Middle East | ||||||||||||||||
| Israel | 5.5* | (0.3) | (20.9) | (268) | 1.9* | (0.2) | (13.9) | (93) | 1.4* | (0.2) | (13.9) | (66) | ||||
| Lebanon | 4.3* | (0.6) | (32.1) | (117) | 1.7* | (0.4) | (21.4) | (39) | 2.0* | (0.3) | (16.0) | (54) | ||||
| Nigeria | 3.2* | (0.2) | (16.4) | (237) | 1.0* | (0.1) | (8.2) | (70) | 0.7* | (0.1) | (8.2) | (46) | ||||
| South Africa | 9.1 | (0.7) | (46.0) | (394) | 3.8 | (0.4) | (26.3) | (171) | 2.9 | (0.3) | (19.7) | (140) | ||||
| Asia and the Pacific | ||||||||||||||||
| China | 3.1* | (0.2) | (14.4) | (160) | 0.9* | (0.2) | (14.4) | (42) | 1.0* | (0.2) | (14.4) | (49) | ||||
| Japan | 10.9** | (0.5) | (24.7) | (264) | 2.1* | (0.3) | (14.8) | (50) | 1.9* | (0.3) | (14.8) | (48) | ||||
| New Zealand | 15.9** | (0.5) | (56.5) | (2212) | 5.6** | (0.3) | (33.9) | (814) | 4.6** | (0.3) | (33.9) | (688) | ||||
| Total | 9.2 | (0.1) | (29.1) | (8164) | 3.1 | (0.1) | (29.1) | (2801) | 2.7 | (0.1) | (29.1) | (2445) | ||||
|
| ||||||||||||||||
|
Among Ideators
|
||||||||||||||||
| Plan | Attempt | Attempt w/o a lifetime plan | Attempt with a lifetime plan | |||||||||||||
| % | (se) | (sd) | (n) | % | (se) | (sd) | (n) | % | (se) | (sd) | (n) | % | (se) | (sd) | (n) | |
|
|
||||||||||||||||
| The Americas | ||||||||||||||||
| Colombia | 33.2 | (2.6) | (63.0) | (204) | 37.8** | (2.6) | (63.0) | (224) | 22.7** | (3.2) | (62.6) | (77) | 68.3** | (3.5) | (50.0) | (147) |
| Mexico | 39.0** | (2.7) | (59.6) | (192) | 33.8 | (2.7) | (59.6) | (166) | 16.3 | (2.6) | (44.7) | (48) | 61.3 | (4.8) | (66.5) | (118) |
| USA | 34.5 | (1.6) | (61.2) | (507) | 31.8 | (1.4) | (53.5) | (469) | 19.9** | (1.4) | (43.3) | (185) | 54.4 | (3.1) | (69.8) | (284) |
| Europe | ||||||||||||||||
| Belgium | 32.2 | (3.4) | (49.2) | (77) | 29.4 | (4.3) | (62.2) | (66) | 12.2 | (3.4) | (39.1) | (16) | 65.7 | (7.0) | (61.4) | (50) |
| France | 35.9 | (3.1) | (61.3) | (143) | 27.2 | (2.9) | (57.3) | (115) | 14.2 | (3.1) | (48.8) | (40) | 50.4 | (4.6) | (55.0) | (75) |
| Germany | 22.1* | (2.5) | (46.6) | (78) | 17.4* | (2.2) | (41.0) | (64) | 4.0* | (1.3) | (21.3) | (14) | 64.7 | (5.8) | (51.2) | (50) |
| Italy | 24.6* | (4.0) | (48.0) | (33) | 18.2* | (4.5) | (54.0) | (26) | 8.2* | (3.0) | (31.6) | (10) | 48.8 | (11.2) | (64.3) | (16) |
| Netherlands | 33.4 | (4.6) | (68.7) | (78) | 27.6 | (3.5) | (52.3) | (64) | 12.0 | (3.2) | (38.5) | (18) | 58.6 | (7.4) | (65.4) | (46) |
| Spain | 33.1 | (3.8) | (62.7) | (84) | 33.9 | (3.1) | (51.1) | (80) | 14.4 | (3.4) | (46.6) | (23) | 73.3** | (5.8) | (53.2) | (57) |
| Ukraine | 32.9 | (2.5) | (49.3) | (126) | 21.5* | (2.7) | (53.3) | (80) | 13.4 | (2.3) | (37.3) | (32) | 38.2* | (5.0) | (56.1) | (48) |
| Africa & the Middle East | ||||||||||||||||
| Israel | 35.3 | (3.2) | (52.4) | (93) | 25.0 | (2.9) | (47.5) | (66) | 8.3* | (2.1) | (27.8) | (15) | 55.5 | (5.5) | (53.0) | (51) |
| Lebanon | 38.4 | (5.0) | (54.1) | (39) | 46.4** | (5.2) | (56.2) | (54) | 30.1** | (6.3) | (55.6) | (25) | 72.4** | (6.9) | (43.1) | (29) |
| Nigeria | 30.1 | (3.6) | (55.4) | (70) | 20.9* | (3.0) | (46.2) | (46) | 1.9* | (0.9) | (11.6) | (3) | 64.8 | (7.2) | (60.2) | (43) |
| South Africa | 41.7** | (2.3) | (45.7) | (171) | 31.7 | (2.6) | (51.6) | (140) | 11.2 | (2.3) | (34.3) | (33) | 60.5 | (4.5) | (58.8) | (107) |
| Asia and the Pacific | ||||||||||||||||
| China | 29.5 | (4.6) | (58.2) | (42) | 32.3 | (4.9) | (62.0) | (49) | 26.1** | (4.7) | (51.1) | (28) | 47.1 | (10.0) | (64.8) | (21) |
| Japan | 18.8* | (2.6) | (42.2) | (50) | 17.0* | (2.5) | (40.6) | (48) | 8.8* | (2.1) | (30.7) | (21) | 52.1 | (7.0) | (49.5) | (27) |
| New Zealand | 35.1 | (1.4) | (65.8) | (814) | 28.8 | (1.3) | (61.1) | (688) | 16.6 | (1.4) | (52.3) | (241) | 51.2 | (2.2) | (62.8) | (447) |
| Total | 33.6 | (0.7) | (63.2) | (2801) | 29.0 | (0.6) | (54.2) | (2445) | 15.4 | (0.6) | (43.9) | (829) | 56.0 | (1.2) | (63.5) | (1616) |
n = 84,850
The upper end of the 95% confidence interval of the estimate is below the prevalence estimate for the total sample.
The lower end of the 95% confidence interval of the estimate is above the prevalence estimate for the total sample.
Within-country prevalence estimates show substantial variability, with the cross-national estimate outside the 95% CI in 13 of the 17 countries for suicidal ideation, and 12 of the 17 for suicide plans and attempts. Prevalence estimates in developing countries are similar to those in developed countries for: suicidal ideation (3.1% to 12.4% versus 3.0% to 15.9%, respectively), suicide plan (0.9% to 4.1% vs. 0.7% to 5.6%, respectively), and suicide attempt (0.7% to 4.7% vs. 0.5% to 5.0%, respectively). Although prevalence estimates varied cross-nationally, the conditional probability of suicide plan and attempt among ideators is more consistent across countries, with the cross-national estimate outside the 95% CI in only 5 of the 17 countries for plans, 7 of 17 for attempts, 9 of 17 for unplanned attempts, and 4 of 17 for planned attempts.
Socio-demographic factors
In the cross-national sample, risk of each suicidal behavior is significantly related to being female, younger age, having fewer years of formal education, and before ever being married (Table 3a). The ORs of these predictors are fairly modest in magnitude (1.3–3.1) with the exception of age. Age is inversely related to risk of each suicidal behavior, with ORs increasing as age decreases across those 50–64 years (2.6–3.4), 35–49 years (4.2–5.6), and 18–34 years (9.5–12.4). Employment history is unrelated to suicidal behaviors. Notably, the relations between the socio-demographic risk factors and suicidal behaviors are attenuated when predicting suicide plans and attempts among ideators (Table 3b), suggesting the relations between these socio-demographic factors and suicide plans and attempts are due primarily to their association with suicidal ideation.
Table 3.
Table 3a. Sociodemographic risk factors for 1st onset of suicide-related outcomes: Pooled Analysis1,2
Table 3b. Sociodemographic risk factors for 1st onset of suicide-related outcomes: Pooled Analysis1
| Total Sample (n=48427)
|
||||||||
|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | ||||||
| Socio-Demographic | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | ||
| Gender | ||||||||
| Female | 1.4* | (1.3 – 1.4) | 1.4* | (1.3 – 1.6) | 1.7* | (1.5 – 1.9) | ||
| X21 [p] | 83.0** | [0.000] | 41.8** | [0.000] | 75.7** | [0.000] | ||
| Age/Cohort3 | ||||||||
| 18–34 | 9.5* | (8.1 – 11.0) | 10.3* | (8.0 – 13.3) | 12.4* | (9.1 – 16.8) | ||
| 35–49 | 4.2* | (3.7 – 4.9) | 4.3* | (3.4 – 5.6) | 5.6* | (4.1 – 7.5) | ||
| 50–64 | 2.6* | (2.2 – 3.0) | 2.7* | (2.1 – 3.4) | 3.4* | (2.4 – 4.7) | ||
| X23 [p] | 1139.6** | [0.000] | 454.5** | [0.000] | 417.0** | [0.000] | ||
| Education4 | ||||||||
| Student | 2.6* | (2.2 – 3.0) | 2.5* | (1.9 – 3.3) | 2.6* | (2.0 – 3.4) | ||
| Low | 2.0* | (1.8 – 2.3) | 2.0* | (1.7 – 2.5) | 3.1* | (2.5 – 3.9) | ||
| Low/Medium | 1.3* | (1.2 – 1.5) | 1.4* | (1.2 – 1.7) | 1.8* | (1.4 – 2.3) | ||
| Medium | 1.4* | (1.2 – 1.6) | 1.5* | (1.2 – 1.8) | 1.7* | (1.4 – 2.1) | ||
| X24 [p] | 233.4** | [0.000] | 67.9** | [0.000] | 119.1** | [0.000] | ||
| Ever employed | ||||||||
| No | 0.9 | (0.8 – 1.0) | 0.9 | (0.7 – 1.1) | 0.9 | (0.7 – 1.1) | ||
| X21 [p] | 2.7 | [0.103] | 1.6 | [0.209] | 2.0 | [0.157] | ||
| Ever married | ||||||||
| No | 1.3* | (1.2 – 1.5) | 1.3* | (1.1 – 1.5) | 1.4* | (1.2 – 1.7) | ||
| X21 [p] | 40.0** | [0.000] | 14.2** | [0.000] | 17.9** | [0.000] | ||
|
| ||||||||
|
Among Ideators
|
||||||||
| Plan (n=6872)2 | Attempt (n=6872)2 | Attempt w/o a lifetime plan (n=4239)2 | Attempt w/a lifetime plan (n=2633)3 | |||||
| Socio-Demographic | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) |
|
|
||||||||
| Gender | ||||||||
| Female | 1.1 | (1.0 – 1.3) | 1.3* | (1.1 – 1.5) | 1.4* | (1.1 – 1.7) | 1.3* | (1.0 – 1.6) |
| X21 [p] | 2.1 | [0.143] | 12.6** | [0.000] | 8.0** | [0.005] | 5.3** | [0.021] |
| Age/Cohort4 | ||||||||
| 18–34 | 1.4* | (1.0 – 1.9) | 1.8* | (1.2 – 2.7) | 2.0* | (1.1 – 3.6) | 1.6 | (0.9 – 2.7) |
| 35–49 | 1.2 | (0.9 – 1.7) | 1.8* | (1.3 – 2.7) | 2.1* | (1.2 – 3.7) | 1.6 | (0.9 – 2.7) |
| 50–64 | 1.2 | (0.9 – 1.5) | 1.6* | (1.1 – 2.3) | 1.8* | (1.0 – 3.2) | 1.5 | (0.9 – 2.5) |
| X23 [p] | 4.5 | [0.214] | 11.3** | [0.010] | 7.6 | [0.056] | 3.1 | [0.380] |
| Education5 | ||||||||
| Student | 1.0 | (0.8 – 1.3) | 1.1 | (0.8 – 1.5) | 1.1 | (0.7 – 1.8) | 1.1 | (0.8 – 1.6) |
| Low | 1.0 | (0.8 – 1.3) | 1.9* | (1.4 – 2.5) | 2.2* | (1.4 – 3.5) | 1.6* | (1.1 – 2.4) |
| Low/Medium | 1.1 | (0.9 – 1.4) | 1.4* | (1.1 – 1.9) | 1.6* | (1.0 – 2.6) | 1.2 | (0.9 – 1.7) |
| Medium | 1.1 | (0.9 – 1.4) | 1.3 | (1.0 – 1.7) | 1.6 | (1.0 – 2.5) | 1.1 | (0.8 – 1.5) |
| X24 [p] | 1.9 | [0.753] | 29.5** | [0.000] | 24.5** | [0.000] | 10.8** | [0.028] |
| Ever employed | ||||||||
| No | 1.0 | (0.8 – 1.2) | 0.9 | (0.8 – 1.1) | 0.9 | (0.6 – 1.2) | 1.0 | (0.8 – 1.4) |
| X21 [p] | 0.2 | [0.696] | 0.6 | [0.437] | 1.0 | [0.325] | 0.1 | [0.733] |
| Ever married | ||||||||
| No | 1.0 | (0.9 – 1.2) | 1.2 | (1.0 – 1.5) | 1.0 | (0.7 – 1.3) | 1.2 | (0.9 – 1.6) |
| X21 [p] | 0.0 | [0.909] | 2.9 | [0.091] | 0.0 | [0.991] | 2.0 | [0.159] |
| Age of onset of ideation6 | ||||||||
| Early | 1.3* | (1.0 – 1.6) | 2.2* | (1.7 – 2.9) | 2.9* | (1.9 – 4.4) | 1.8* | (1.2 – 2.6) |
| Middle | 1.2* | (1.0 – 1.5) | 1.5* | (1.2 – 1.9) | 1.6* | (1.1 – 2.2) | 1.5* | (1.1 – 2.0) |
| X22 [p] | 5.0 | [0.083] | 32.2** | [0.000] | 27.3** | [0.000] | 10.4** | [0.005] |
| Years since onset of ideation7 | ||||||||
| 0 | 117.4* | (87.9 – 156.8) | 123.1* | (92.9 – 162.9) | 174.6* | (100.9 – 302.1) | -- | -- |
| 1–5 | 3.3* | (2.4 – 4.5) | 4.4* | (3.2 – 5.9) | 6.2* | (3.4 – 11.2) | -- | -- |
| 6–10 | 1.8* | (1.2 – 2.6) | 1.5 | (1.0 – 2.1) | 1.5 | (0.6 – 3.4) | -- | -- |
| X23 [p] | 2207.2** | [0.000] | 2521.0** | [0.000] | 873.6** | [0.000] | -- | -- |
| Have a plan | ||||||||
| Yes | -- | -- | 7.5* | (6.4 – 8.7) | -- | -- | -- | -- |
| X21 [p] | -- | -- | 650.2** | [0.000] | -- | -- | -- | -- |
| Years since onset of plan7 | ||||||||
| 0 | -- | -- | -- | -- | -- | -- | 168.4* | (106.6 – 266.1) |
| 1–5 | -- | -- | -- | -- | -- | -- | 5.0* | (3.1 – 8.0) |
| 6–10 | -- | -- | -- | -- | -- | -- | 1.6 | (0.9 – 3.0) |
| X23 [p] | -- | -- | -- | -- | -- | -- | 1126.1** | [0.000] |
Significant at the 0.05 level, 2-sided test
Results are based on multivariate discrete-time survival models with person-year as the unit of analysis; see the text for a description.
Each model controls for person-year
Referent category: 65+
Referent category: High education
Significant at the 0.05 level, 2-sided test
-- indicates that the variable is not used as a predictor in the model
Results are based on multivariate discrete-time survival models with person-year as the unit of analysis; see the text for a description.
model controls for years since onset of ideation
model controls for years since onset of plan
Referent category: 65+
Referent category: High education
Referent category: Late
Referent category: 11+ years
Within-country findings are very similar to those in the pooled sample. For example, a dominant sign pattern exists for female gender and risk of the three main outcomes of suicidal ideation, plan, and attempt (i.e., 47 of the 51 ORs across the 17 separate countries are 1.0 or greater) and 57% of the within-country ORs for gender are significant at the .05 level. ORs for female gender are always 1.0 or greater for suicidal ideation, and are less than 1.0 in only two instances for suicide plan (Japan=0.9, Nigeria=0.9), and two for attempt (Colombia=0.9, Nigeria=0.8), none being statistically significant. Similarly, the strong relation between age and risk of suicidal behaviors is consistent across 16 of the 17 countries (in Japan the highest risk of each outcome is in the 35–49 cohort), with 88% of the within-country ORs for the youngest cohort significant at the .05 level. Results are similar but less consistently significant in within-country analyses for education, employment, and marital history given the relatively small effect sizes for these relations.
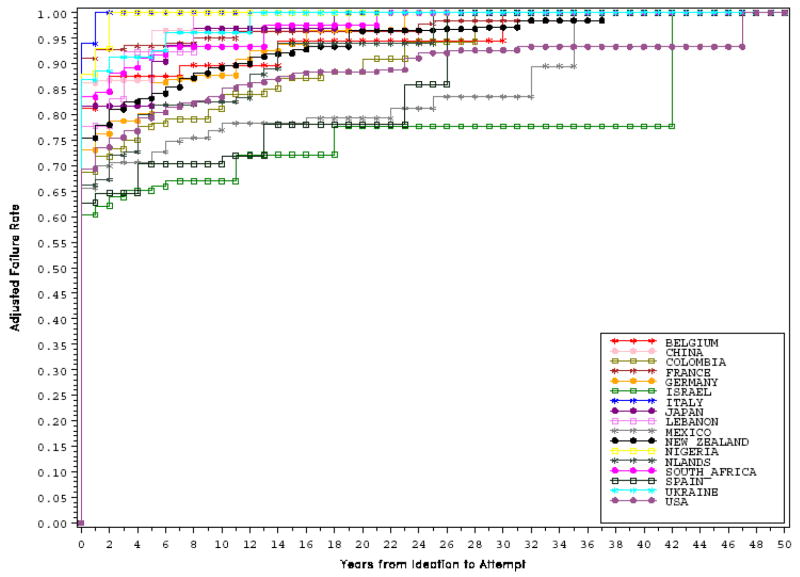
Characteristics of suicidal behaviors as risk factors
Suicide ideators within each country were classified into terciles based on age-of-onset (AOO) of suicidal ideation to examine the relation between AOO and risk of transition from ideation to plans and attempts. Analyses revealed that earlier AOO is significantly associated with greater risk of suicide plan and attempt among those with ideation (Table 3b). Importantly, the transition from suicidal ideation to first onset of plan or attempt is extremely elevated within the first year of onset of ideation (OR=117.4–123.1), and decreases substantially thereafter (OR=1.5–4.4). Among ideators, having a suicide plan is associated with a significantly higher risk of making an attempt (OR=7.5), although the odds of making an unplanned attempt within the first year after onset of ideation are just as high (OR=174.6) as the odds of making an attempt within the first year after onset of a plan (OR=168.4). Thus, whether a plan is present or not, the highest risk of suicide attempt is in the first year after onset of ideation.
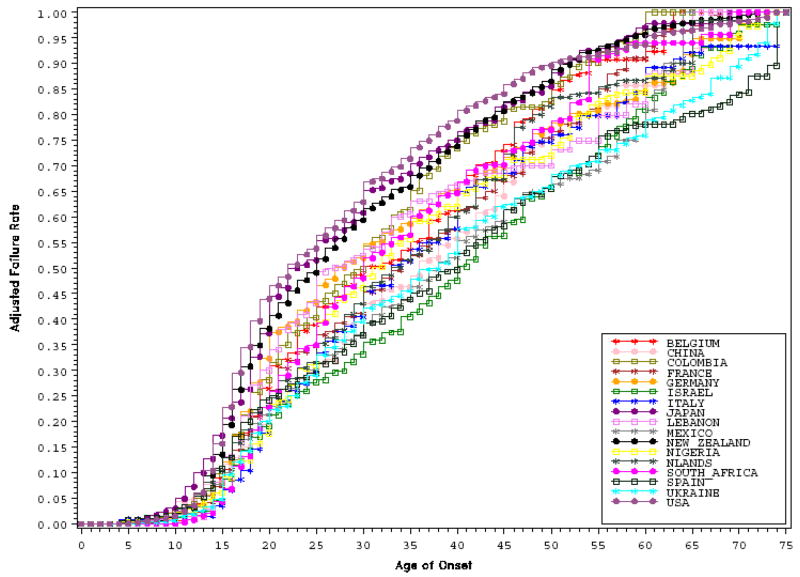
Examination of AOO curves reveals that across all 17 countries the risk of first onset of suicidal ideation increases sharply during adolescence and young adulthood (Figure 1). These curves separate in the mid-teens to early-20’s, with several countries (Japan, New Zealand, US) showing an earlier increase in risk of suicidal ideation, while other countries have a sharp increase in risk later in life (Israel, Mexico, Spain, Ukraine). Conditional AOO curves show that the rapid transitions from ideation to attempt (Figure 2) occur within the first year of onset of ideation more than 60% of the time across all 17 countries. The same pattern was observed for the transitions from ideation to plan and plan to attempt across all countries.
Figure 1.
Cumulative Age-of-Onset Distribution for Suicide Ideation in each Country
Figure 2.
Conditional, Cumulative Speed of Transition from Ideation to Attempt in each Country
Mental disorders as risk factors
In the cross-national sample, the presence of a prior mental disorder is associated with significantly increased risk of suicidal behaviors, even after controlling for socio-demographic factors, characteristics of suicidal behaviors, and country of residence (see Tables 4a & 4b). Relations are strongest across both developed and developing countries for mood disorders (OR=3.4–5.9) and impulse-control disorders (3.3–6.5), followed by anxiety disorders (2.8–4.8), and substance use disorders (2.8–4.6). Importantly, associations between mental disorders and suicidal behaviors are attenuated when predicting plans and attempts among ideators, with ORs decreasing to 1.0–2.1 across all categories. Among ideators, the risk of making an attempt is highest for those with substance use and impulse-control disorders, suggesting these disorders are most strongly associated with acting on suicidal thoughts when they are present. Results also show a strong dose-response relation between the number of mental disorders present and the risk of suicidal behaviors.
Table 4.
Table 4a. DSM-IV Disorders as risk factors for 1st onset of suicide-related outcomes in the developed countries: Pooled Analysis
Table 4b. DSM-IV Disorders as risk factors for 1st onset of suicide-related outcomes in the developing countries: Pooled Analysis
|
Total Sample (n=32,921) |
Among Ideators |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ideation | Plan | Attempt | Plan (n=5,017) | Attempt (n=5,017) | Attempt w/o a lifetime plan (n=3,189) | Attempt w/a lifetime plan (n=1,828) | ||||||||
| Disorder category | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) |
|
|
|
|||||||||||||
| Any anxiety disorders1 | 3.4* | (3.2 – 3.7) | 4.5* | (3.9 – 5.1) | 4.8* | (4.1 – 5.5) | 1.6* | (1.3 – 1.8) | 1.5* | (1.3 – 1.8) | 1.3* | (1.0 – 1.7) | 1.6* | (1.2 – 2.0) |
| Any mood disorders1,3 | 4.7* | (4.2 – 5.2) | 5.8* | (4.9 – 6.9) | 5.9* | (5.0 – 7.1) | 1.5* | (1.3 – 1.8) | 1.3* | (1.1 – 1.6) | 1.3 | (0.9 – 1.7) | 1.2 | (0.9 – 1.5) |
| Any impulse-control disorders2 | 3.3* | (2.8 – 3.8) | 3.6* | (2.8 – 4.6) | 4.2* | (3.3 – 5.4) | 1.4* | (1.0 – 1.9) | 1.5* | (1.1 – 2.1) | 1.5* | (1.0 – 2.3) | 1.5* | (1.0 – 2.2) |
| Any substance use disorders1,3 | 2.8* | (2.5 – 3.2) | 4.1* | (3.4 – 4.9) | 4.2* | (3.5 – 5.1) | 1.9* | (1.6 – 2.4) | 1.6* | (1.2 – 2.1) | 1.9* | (1.3 – 2.7) | 1.4 | (1.0 – 1.9) |
| Any disorders1 | 4.1* | (3.8 – 4.5) | 5.8* | (5.0 – 6.8) | 6.4* | (5.4 – 7.6) | 1.6* | (1.4 – 1.9) | 1.6* | (1.3 – 1.9) | 1.5* | (1.1 – 1.9) | 1.6* | (1.2 – 2.1) |
| Exactly 1 disorder1 | 1.0 | (0.9 – 1.1) | 0.9 | (0.7 – 1.1) | 0.8 | (0.7 – 1.1) | 0.8 | (0.6 – 1.0) | 0.8 | (0.6 – 1.1) | 0.7 | (0.4 – 1.1) | 0.9 | (0.6 – 1.3) |
| Exactly 2 disorders1 | 2.1* | (1.9 – 2.4) | 1.9* | (1.5 – 2.2) | 1.9* | (1.5 – 2.3) | 0.9 | (0.7 – 1.1) | 1.0 | (0.7 – 1.3) | 1.2 | (0.8 – 1.8) | 0.8 | (0.6 – 1.2) |
| 3+ disorders1 | 6.1* | (5.6 – 6.6) | 8.6* | (7.4 – 10.0) | 8.9* | (7.7 – 10.3) | 2.0* | (1.7 – 2.4) | 1.8* | (1.5 – 2.1) | 1.7* | (1.3 – 2.1) | 1.8* | (1.4 – 2.3) |
|
Total Sample (n=15,506)
|
Among Ideators
|
|||||||||||||
| Ideation | Plan | Attempt | Plan (n=1,855) | Attempt (n=1,855) | Attempt w/o a lifetime plan (n=1,050) | Attempt w/a lifetime plan (n=805) | ||||||||
| Disorder category | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) |
|
|
|
|||||||||||||
| Any anxiety disorders1 | 2.8* | (2.4 – 3.2) | 3.6* | (2.8 – 4.5) | 3.5* | (2.8 – 4.3) | 1.5* | (1.2 – 1.9) | 1.2 | (0.9 – 1.5) | 1.1 | (0.7 – 1.6) | 1.3 | (0.9 – 1.8) |
| Any mood disorders1 | 3.4* | (2.8 – 4.1) | 5.5* | (4.4 – 6.9) | 4.7* | (3.6 – 6.0) | 2.1* | (1.6 – 2.9) | 1.0 | (0.8 – 1.4) | 0.8 | (0.5 – 1.3) | 1.2 | (0.8 – 1.9) |
| Any impulse-control disorders2 | 4.4* | (3.5 – 5.5) | 6.5* | (4.8 – 8.8) | 6.3* | (4.6 – 8.5) | 2.1* | (1.5 – 2.9) | 1.6* | (1.1 – 2.4) | 1.4 | (0.8 – 2.6) | 2.3* | (1.3 – 4.2) |
| Any substance use disorders1 | 2.9* | (2.3 – 3.7) | 4.2* | (3.0 – 5.9) | 4.6* | (3.5 – 6.3) | 1.8* | (1.1 – 2.8) | 1.4* | (1.0 – 2.0) | 1.2 | (0.6 – 2.5) | 1.6 | (1.0 – 2.5) |
| Any disorders1 | 3.6* | (3.1 – 4.1) | 5.4* | (4.4 – 6.7) | 5.3* | (4.2 – 6.6) | 1.8* | (1.4 – 2.4) | 1.4* | (1.1 – 1.7) | 1.2 | (0.8 – 1.7) | 1.6* | (1.1 – 2.3) |
| Exactly 1 disorder1 | 1.4* | (1.1 – 1.7) | 1.0 | (0.8 – 1.3) | 1.2 | (0.9 – 1.6) | 0.7* | (0.5 – 1.0) | 0.9 | (0.7 – 1.3) | 0.9 | (0.5 – 1.6) | 1.0 | (0.6 – 1.6) |
| Exactly 2 disorders1 | 2.8* | (2.3 – 3.5) | 3.7* | (2.9 – 4.7) | 3.1* | (2.4 – 4.1) | 1.5* | (1.1 – 2.1) | 1.1 | (0.8 – 1.6) | 0.9 | (0.5 – 1.5) | 1.0 | (0.6 – 1.7) |
| 3+ disorders1 | 5.9* | (4.9 – 7.2) | 10.0* | (7.7 – 12.9) | 9.2* | (7.4 – 11.6) | 2.5* | (1.9 – 3.3) | 1.5* | (1.1 – 2.1) | 1.6* | (1.0 – 2.6) | 1.8* | (1.2 – 2.7) |
OR significant at the 0.05 level, 2-sided test
Assessed in the Part II sample
Assessed only in the Part II sample with age range 18–44
New Zealand assessed in the Part I sample
Results are based on multivariate discrete-time survival model
Each model controls for person-year, countries and the sociodemographic variables from the table 2
Developed countries include: United States, Belgium, France, Germany, Italy, Netherlands, Spain, Israel, Japan and New Zealand
Developing countries include: Colombia, Mexico, Ukraine, Lebanon, Nigeria, South Africa and People's Republic of China
Any mood disorder = major depressive, dysthymic, and bipolar disorders; Any impulse-control disorder = intermittent explosive, attention-deficit/hyperactivity, conduct, and oppositional defiant disorders; Any anxiety disorder = panic, agoraphobia, generalized anxiety, specific phobia, social phobia, post-traumatic stress, and adult separation anxiety disorders; Any substance use disorder = alcohol abuse or dependence and illicit drug abuse or dependence.
In within-country analyses, the presence of any mental disorder is associated with significantly increased risk in each of the 17 countries. The ORs for these analyses are quite stable, with only three countries differing significantly from the cross-national estimate for any outcome. Specifically, Israel is above the cross-national estimate for ideation, plan, and attempt, Italy is above the estimate for attempt, and Germany is below the estimate for ideation. The strong dose-response relation between number of disorders and risk of suicidal behaviors also is consistent across all 17 countries.
Within-country analyses examining the relation between each of the four disorder categories and the three primary suicidal behaviors also are largely consistent with those in the pooled cross-national sample, with only three of 204 (1.5%) ORs less than 1.0, and 92.5% of ORs significant at the .05 level. The greatest variability among countries is in the relation between mood disorder and suicidal behaviors. Seven countries have ORs significantly higher than the cross-national estimate (Belgium, China, Germany, Israel, Italy, Japan, and Nigeria) and two below (Colombia, France).
Analyses revealed an interesting pattern regarding developing versus developed countries. In developed countries the presence of a mood disorder is the strongest predictor of suicidal ideation, plan, and attempt (see Table 4a; 9 of 10 countries show this pattern). However, in developing countries the presence of an impulse-control disorder is a stronger predictor than mood disorder (see Table 4b; 5 of the 6 countries in which impulse-control disorders were examined). Thus, although the presence of mental disorders in general, and comorbidity in particular, are consistently strong predictors of suicidal behaviors cross-nationally, there are notable differences in the type of disorder most strongly predictive of suicidal behaviors.
DISCUSSION
The results of this study provide valuable and previously unavailable information about the prevalence and risk factors of suicidal behaviors around the world. Our results show that although there is substantial variability in the prevalence of suicidal behaviors cross-nationally, there are important cross-national consistencies in the prevalence and risk factors for suicidal behaviors. Most notably, across all countries examined, 60% of the transitions from suicidal ideation to first suicide attempt occurred within the first year of ideation onset. Moreover, consistent cross-national risk factors included: female sex, younger age, fewer years of education, unmarried status, and the presence of a mental disorder, with psychiatric comorbidity significantly increasing risk. Interestingly, the strongest diagnostic risk factors were mood disorders in developed countries, but impulse-control disorders in developing countries.
Several important limitations should be borne in mind when interpreting these results. First, although the overall response rate was at an acceptable level, response rates varied across countries and in some cases were below commonly accepted standards. We controlled for differential response using post-stratification adjustments, but it is possible that response rates were related to the presence of suicidal behaviors or mental disorders, which could have biased cross-national comparisons. Also, although surveys in most countries included nationally representative samples, several surveys (e.g., China, Japan) focused on specific urban areas and so findings from those surveys may not generalize to all regions of those countries. A related limitation is that although we examined suicidal behaviors across 17 countries, several countries/regions with high rates of suicide were not included such as India and South East Asia.24 The inclusion of data from additional countries/regions in future work will significantly enhance our understanding of the factors influencing suicidal behaviors more broadly.
Second, data were based on retrospective self-report of the occurrence and timing of suicidal behaviors, and thus may be subject to under-reporting and biased recall. We also did not collect information from third-party informants to validate respondent reports. On balance, several systematic reviews have demonstrated that adults can recall past experiences with sufficient accuracy to provide valuable information,25,26 and such data are especially useful when prospective data are not available,27 as in the current case. Another limitation is that there may be cultural differences in the willingness to report on suicidal behaviors and in the interpretation of questions about DSM-IV mental disorders. Our results must be viewed with these limitations in mind.
Third, several mental disorders were not adequately assessed in the WMH surveys for various reasons. A few DSM-IV disorders were not assessed in some surveys because they were believed to have low relevance or they were excluded from analyses due to an insufficient number of cases, such as impulse-control disorders in Nigeria; and in some cases disorders were not adequately assessed due to skip logic errors, such as bipolar disorder and substance use disorders in the ESEMeD Surveys.10 Schizophrenia and other nonaffective psychoses were not included in any WMH survey because previous validation studies showed they are overestimated in lay-administered interviews like the CIDI.28 These exclusions are unfortunate because prior research clearly indicates that bipolar and substance use disorders are strongly associated with suicidal behaviors3,6 and suggests that schizophrenia and suicidal behaviors share unique prevalence patterns and are strongly related in developing countries,29 thus the current study might have provided important information in this regard. The measurement of these disorders and the explanation of their relation to suicidal behaviors in both developed and developing countries is one of the most important tasks for future work on this topic.
Fourth, this initial study included only a limited range of risk factors for suicidal behavior. Factors such as individual axis I and axis II disorders and traumatic life events were not examined in this study. Also excluded were potential protective factors such as treatment utilization and social support. The investigation of these and other factors remain important directions for future research.
These limitations notwithstanding, several important findings from this study warrant more detailed comment. Perhaps the most important finding of this study is that there is strong cross-national consistency for several key risk factors for suicidal behaviors. Female gender, young age, and low educational attainment have been identified as risk factors for suicidal behaviors in prior studies,3,6 and the current findings suggest these risk factors may be universal. Future research is needed to determine whether risk of suicidal behaviors is occurring at higher rates among young people, or whether people simply become less likely to report on earlier suicidal behavior with age, due to forgetting or re-interpretation of these earlier events.
Risk of suicide plans and attempts also was highest when suicidal ideation had an earlier AOO and within the first year of ideation. Remarkably, 60% of the transitions from ideation to attempt—as well as from ideation to plan and plan to attempt—occur within the first year of onset of ideation and this result is consistent across all 17 countries. Few studies have examined the probability and speed of transition from ideation to plans and attempts, and this information can be especially useful to health care providers. Another important finding is that the strong relation observed between mental disorders and suicide plans and attempts diminishes when controlling for ideation. Thus, although mental disorders are strong risk factors of suicidal behaviors, factors beyond the mere presence of mental disorders explain the transition from ideation to plans and attempts.
Several recent studies have suggested that mental disorders are less important in the occurrence of suicidal behaviors in developing countries relative to developed countries. Whereas studies in developed countries suggest >90% of those who die by suicide have a diagnosable mental disorder and >60% have a mood disorder in particular,30 rates in developing countries have been suggested to be as low as 60% and 35%, respectively.7 Our results indicate that when the same assessment methods are used cross-nationally, mental disorders are as predictive of suicidal behaviors in developing countries as they are in developed countries, and that comorbidity is an important predictor across all countries. Notably though, impulse-control disorders were stronger predictors than mood disorders in most developing countries. The fact that mood and impulse control disorders have the strongest associations with suicidal behaviors is consistent with prior work highlighting the importance of depressed mood and impulsiveness in the suicidal process,31 and extends these findings cross-nationally. The reason for the difference in the importance of impulse-control disorders between developed and developing countries is unclear and awaits further examination.
Future research must examine factors that might explain the variability in prevalence and also must develop more complex risk and protective models that take into account both common and specific factors for each country/region. From a practical perspective, the similarities observed between developing and developed countries suggest equivalent resources should be devoted to studying and preventing suicidal behaviors in these countries. Currently, however, resources devoted to the treatment of mental disorders in general, and to suicide prevention in particular,9 are lacking in many developing (and developed) countries.7,10 It is important to note, however, that more treatment alone is not the answer. Several recent studies have highlighted that despite significant increases in service utilization among suicidal individuals, the rates of suicidal ideation, plans, and attempts have remained virtually unchanged.4 Moreover, although several different forms of treatment have proven effective at decreasing the likelihood of making suicide attempts, psychosocial treatments have proven less effective at decreasing the likelihood of suicide death.32 Improvements in our ability to predict and prevent suicidal behaviors and suicide deaths are clearly needed and require that we continue to identify the risk and protective factors that influence such behaviors and also that we develop more sophisticated methods for synthesizing and using the information obtained about such factors.
Acknowledgments
The surveys included in this report were carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. We thank the WMH staff for assistance with instrumentation, fieldwork, and data analysis. These activities were supported by the United States National Institute of Mental Health (R01MH077883; R01MH070884), the John D. and Catherine T. MacArthur Foundation, the Pfizer Foundation, the US Public Health Service (R13-MH066849, R01-MH069864, and R01 DA016558), the Fogarty International Center (FIRCA R03-TW006481), the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical, Inc., GlaxoSmithKline, and Bristol-Myers Squibb. A complete list of WMH publications can be found at http://www.hcp.med.harvard.edu/wmh/. The Chinese World Mental Health Survey Initiative is supported by the Pfizer Foundation. The Colombian National Study of Mental Health (NSMH) is supported by the Ministry of Social Protection, with supplemental support from the Saldarriaga Concha Foundation. The ESEMeD project is funded by the European Commission (Contracts QLG5-1999-01042; SANCO 2004123), the Piedmont Region (Italy), Fondo de Investigación Sanitaria, Instituto de Salud Carlos III, Spain (FIS 00/0028), Ministerio de Ciencia y Tecnología, Spain (SAF 2000-158-CE), Departament de Salut, Generalitat de Catalunya, Spain, RETICS RD06/0011 REM-TAP, and other local agencies and by an unrestricted educational grant from GlaxoSmithKline. The Israel National Health Survey is funded by the Ministry of Health with support from the Israel National Institute for Health Policy and Health Services Research and the National Insurance Institute of Israel. The World Mental Health Japan (WMHJ) Survey is supported by the Grant for Research on Psychiatric and Neurological Diseases and Mental Health (H13-SHOGAI-023, H14-TOKUBETSU-026, H16-KOKORO-013) from the Japan Ministry of Health, Labour and Welfare. The Lebanese National Mental Health Survey (LNMHS) is supported by the Lebanese Ministry of Public Health, the WHO (Lebanon), the Fogarty International Center and anonymous private donations to IDRAAC, Lebanon, and unrestricted grants from Janssen Cilag, Eli Lilly, GlaxoSmithKline, Roche, and Novartis. The Mexican National Comorbidity Survey (MNCS) is supported by The National Institute of Psychiatry Ramon de la Fuente (INPRFMDIES 4280) and by the National Council on Science and Technology (CONACyT-G30544- H), with supplemental support from the PanAmerican Health Organization (PAHO). Te Rau Hinengaro: The New Zealand Mental Health Survey (NZMHS) is supported by the New Zealand Ministry of Health, Alcohol Advisory Council, and the Health Research Council. The Nigerian Survey of Mental Health and Wellbeing (NSMHW) is supported by the WHO (Geneva), the WHO (Nigeria), and the Federal Ministry of Health, Abuja, Nigeria. The South Africa Stress and Health Study (SASH) is supported by the US National Institute of Mental Health (R01-MH059575) and National Institute of Drug Abuse with supplemental funding from the South African Department of Health and the University of Michigan. The Ukraine Comorbid Mental Disorders during Periods of Social Disruption (CMDPSD) study is funded by the US National Institute of Mental Health (R01-MH61905). The US National Comorbidity Survey Replication (NCS-R) is supported by the National Institute of Mental Health (NIMH; U01-MH60220) with supplemental support from the National Institute of Drug Abuse (NIDA), the Substance Abuse and Mental Health Services Administration (SAMHSA), the Robert Wood Johnson Foundation (RWJF; Grant 044780), and the John W. Alden Trust. Dr. Kessler, as principal investigator, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Declaration of interests: None. Funding sources are detailed in Acknowledgements.
References
- 1.WHO. Prevention of suicide: guidelines for the formulation and implementation of national strategies. Geneva: World Health Organization; 1996. [Google Scholar]
- 2.Vijayakumar L, Nagaraj K, Pirkis J, Whiteford H. Suicide in developing countries (1): frequency, distribution, and association with socioeconomic indicators. Crisis. 2005;26(3):104–11. doi: 10.1027/0227-5910.26.3.104. [DOI] [PubMed] [Google Scholar]
- 3.Moscicki EK. Epidemiology of suicide. In: Jacobs DG, editor. The Harvard Medical School guide to suicide assessment and intervention. San Francisco, CA: Jossey-Bass; 1999. pp. 40–51. [Google Scholar]
- 4.Kessler RC, Berglund P, Borges G, Nock MK, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. Journal of the American Medical Association. 2005;293(20):2487–95. doi: 10.1001/jama.293.20.2487. [DOI] [PubMed] [Google Scholar]
- 5.Weissman MM, Bland RC, Canino GJ, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychological Medicine. 1999;29(1):9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- 6.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry. 1999;56(7):617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]
- 7.Vijayakumar L. Suicide prevention: the urgent need in developing countries. World Psychiatry. 2004;3(3):158–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips MR, Yang G, Zhang Y, Wang L, Ji H, Zhou M. Risk factors for suicide in China: a national case-control psychological autopsy study. Lancet. 2002;360(9347):1728–36. doi: 10.1016/S0140-6736(02)11681-3. [DOI] [PubMed] [Google Scholar]
- 9.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. Journal of the American Medical Association. 2005;294(16):2064–74. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 10.Demyttenaere K, Bruffaerts R, Posada-Villa J, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. Jama. 2004;291(21):2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 11.Platt S, Bille-Brahe U, Kerkhof A, et al. Parasuicide in Europe: the WHO/EURO multicentre study on parasuicide. I. Introduction and preliminary analysis for 1989. Acta Psychiatrica Scandanavica. 1992;85(2):97–104. doi: 10.1111/j.1600-0447.1992.tb01451.x. [DOI] [PubMed] [Google Scholar]
- 12.Bertolote JM, Fleischmann A, De Leo D, et al. Suicide attempts, plans, and ideation in culturally diverse sites: the WHO SUPRE-MISS community survey. Psychol Med. 2005;35(10):1457–65. doi: 10.1017/S0033291705005404. [DOI] [PubMed] [Google Scholar]
- 13.Alonso J, Angermeyer MC, Bernert S, et al. Sampling and methods of the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatrica Scandanavica Supplement. 2004;(420):8–20. doi: 10.1111/j.1600-0047.2004.00326. [DOI] [PubMed] [Google Scholar]
- 14.World Bank. World Development Indicators 2003. Washington, DC: The World Bank; 2003. [Google Scholar]
- 15.Kessler RC, Merikangas KR. The National Comorbidity Survey Replication (NCS-R): background and aims. International Journal of Methods in Psychiatric Research. 2004;13(2):60–8. doi: 10.1002/mpr.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13(2):93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Turner CF, Ku L, Rogers SM, Lindberg LD, Pleck JH, Sonenstein FL. Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science. 1998;280(5365):867–873. doi: 10.1126/science.280.5365.867. [DOI] [PubMed] [Google Scholar]
- 18.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP) New York, NY: Biometrics Research, New York State Psychiatric Institute; 2002. [Google Scholar]
- 19.Kessler RC, Berglund P, Demler O, Jin R, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 20.Haro JM, Arbabzadeh-Bouchez S, Brugha TS, et al. Concordance of the Composite International Diagnostic Interview Version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health Surveys. International Journal of Methods in Psychiatric Research. 2006;15(4):167–180. doi: 10.1002/mpr.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Efron B. Logistic regression, survival analysis, and the Kaplan Meier curve. J Am Sociol Assoc. 1988;83:414–425. [Google Scholar]
- 22.Wolter K. Introduction to Variance Estimation. New York, NY: Springer-Verlag; 1985. [Google Scholar]
- 23.SUDAAN. Professional Software for Survey Data Analysis [program]. 8.01 version. Research Triangle Park, NC: Research Triangle Institute; 2002. [Google Scholar]
- 24.Eddleston M, Konradsen F. Commentary: Time for a re-assessment of the incidence of intentional and unintentional injury in India and South East Asia. International Journal of Epidemiology. 2007;36(1):208–11. doi: 10.1093/ije/dyl240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Brewin CR, Andrews B, Gotlib IH. Psychopathology and early experience: a reappraisal of retrospective reports. Psychological Bulletin. 1993;113(1):82–98. doi: 10.1037/0033-2909.113.1.82. [DOI] [PubMed] [Google Scholar]
- 26.Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45(2):260–73. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- 27.Schlesselman JJ. Case-control studies: Design, conduct, and analysis. New York, NY: Oxford University Press; 1982. [Google Scholar]
- 28.Kendler KS, Gallagher TJ, Abelson JM, Kessler RC. Lifetime prevalence, demographic risk factors, and diagnostic validity of nonaffective psychosis as assessed in a US community sample. The National Comorbidity Survey. Archives of General Psychiatry. 1996;53(11):1022–31. doi: 10.1001/archpsyc.1996.01830110060007. [DOI] [PubMed] [Google Scholar]
- 29.Phillips MR, Yang G, Li S, Li Y. Suicide and the unique prevalence pattern of schizophrenia in mainland China: a retrospective observational study. Lancet. 2004;364(9439):1062–8. doi: 10.1016/S0140-6736(04)17061-X. [DOI] [PubMed] [Google Scholar]
- 30.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychological Medicine. 2003;33(3):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 31.Mann JJ, Waternaux C, Haas GL, Malone KM. Toward a clinical model of suicidal behavior in psychiatric patients. American Journal of Psychiatry. 1999;156(2):181–9. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 32.Crawford MJ, Thomas O, Khan N, Kulinskaya E. Psychosocial interventions following self-harm: systematic review of their efficacy in preventing suicide. British Journal of Psychiatry. 2007;190:11–7. doi: 10.1192/bjp.bp.106.025437. [DOI] [PubMed] [Google Scholar]