Sir,
We read with interest the article of Leung et al (2007) describing a reduced relapse rate after autologous HSCT in patients with an inhibitory KIR–HLA mismatch treated with autologous transplantation for non-Hodgkin's lymphoma or solid tumour. The analysis was performed after several recent publications indicated a reduced relapse rate in patients treated by allogeneic HSCT (by the same group (Leung et al, 2005) and others (Hsu et al, 2005)) in the presence of a mismatch between donor inhibitory KIR and patient HLA.
The manuscript prompted us to analyse the outcome after autologous transplantations carried out between 1997 and 2006 at our centre. Patients were included if HLA typing allowed unequivocal deduction of the KIR-ligand status, and were grouped according to the presence or absence of KIR ligands, without taking into account inhibitory KIR. This type of approach is generally chosen for retrospective studies (Miller et al, 2007), as population frequencies of KIR gene distribution indicate that virtually all Caucasians possess and express KIR2DL1 and KIR2DL2/3 and only a minority do not possess or express KIR3DL1. Therefore, grouping according to KIR ligands should correctly classify the vast majority of patients regarding an inhibitory KIR/HLA mismatch (in the publication by Leung, 1 out of 16 patients would have been misclassified using this approach).
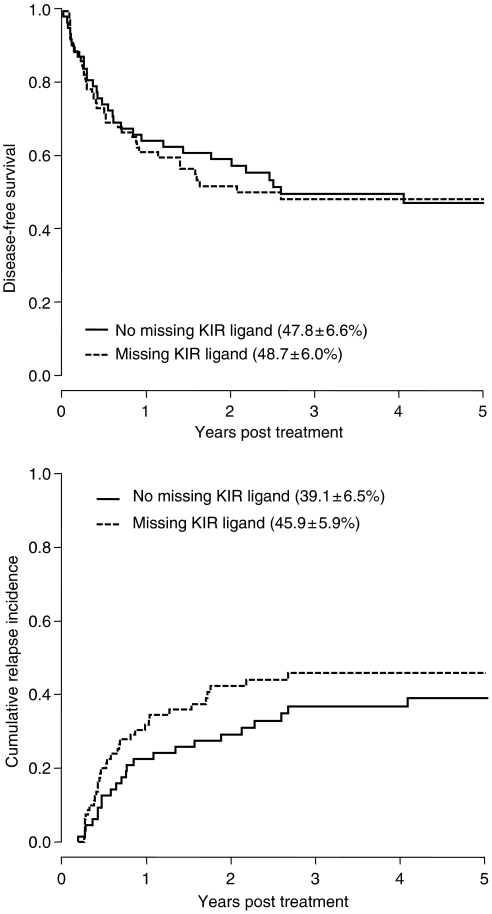
Outcome of 67 autologous transplants for solid tumour (N=23) or lymphoma (N=44) was analysed. In 21 patients, grafts were depleted from tumour cells and T cells by CD34 selection. Absence of KIR ligands had no effect on disease-free survival (DFS) (relative risk (RR) 1.03 vs patients with all KIR ligands, P=0.91) or disease relapse (RR 1.24, P=0.23; Figure 1). Similar results were seen when the analysis was restricted to patients receiving T-cell-depleted transplants (RR for DFS 1.08, P=0.88; RR for relapse 1.15, P=0.79). Excluding patients missing Bw4 (the ligand for KIR3DL1, the only inhibitory KIR absent in a significant proportion of Caucasians), the relative risks for DFS and relapse were 1.15 (P=0.59) and 1.36 (P=0.28) for missing ligand patients.
Figure 1.
Disease-free survival (upper panel) and cumulative incidence of relapse (lower panel) are not different between patients with or without a missing KIR ligand after high-dose chemotherapy and autologous haematopoietic stem cell transplantation.
In conclusion, we were not able to show a missing KIR-ligand effect in our population of autologous HSCT recipients. One caveat of our approach is that a missing KIR ligand does not imply an inhibitory KIR/HLA mismatch, however, restriction of analysis to the almost universally expressed KIR2D did not show significant differences. We therefore believe that while the data presented by Leung et al (2007) are intriguing, they should be confirmed in large studies.
References
- Hsu KC, Keever-Taylor CA, Wilton A, Pinto C, Heller G, Arkun K, O'Reilly RJ, Horowitz MM, Dupont B (2005) Improved outcome in HLA-identical sibling hematopoietic stem-cell transplantation for acute myelogenous leukemia predicted by KIR and HLA genotypes. Blood 105: 4878–4884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung W, Handgretinger R, Iyengar R, Turner V, Holladay MS, Hale GA (2007) Inhibitory KIR–HLA receptor–ligand mismatch in autologous haematopoietic stem cell transplantation for solid tumour and lymphoma. Br J Cancer 97: 539–542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung W, Iyengar R, Triplett B, Turner V, Behm FG, Holladay MS, Houston J, Handgretinger R (2005) Comparison of killer Ig-like receptor genotyping and phenotyping for selection of allogeneic blood stem cell donors. J Immunol 174: 6540–6545 [DOI] [PubMed] [Google Scholar]
- Miller JS, Cooley S, Parham P, Farag SS, Verneris MR, McQueen KL, Guethlein LA, Trachtenberg EA, Haagenson M, Horowitz MM, Klein JP, Weisdorf DJ (2007) Missing KIR ligands are associated with less relapse and increased graft-vs-host disease (GVHD) following unrelated donor allogeneic HCT. Blood 109: 5058–5061 [DOI] [PMC free article] [PubMed] [Google Scholar]