Abstract
Research into the nature and occurrence of medical errors has shown that these often result from a combination of factors that lead to the breakdown of workflow. Nowhere is this more critical than in the emergency department (ED), where the focus of clinical decision is on the timely evaluation and stabilization of patients. This paper reports on the nature of errors and their implications for patient safety in an adult ED, using methods of ethnographic observation, interviews, and think-aloud protocols. Data were analyzed using modified “grounded theory,” which refers to a theory developed inductively from a body of data. Analysis revealed four classes of errors, relating to errors of misidentification, ranging from multiple medical record numbers, wrong patient identification or address, and in one case, switching of one patient’s identification information with those of another. Further analysis traced the root of the errors to ED registration.
These results indicate that the nature of errors in the emergency department are complex, multi-layered and result from an intertwined web of activity, in which stress of the work environment, high patient volume and the tendency to adopt shortcuts play a significant role. The need for information technology (IT) solutions to these problems as well as the impact of alternative policies is discussed.
Keywords: ED registration, medical errors, misidentification, workarounds, shortcuts, distributed cognition, emergency care
Introduction
The emergency department (ED) of today has been described as a “natural laboratory for the study of error” [1]. It constitutes a complex and dynamic environment in which a team, consisting of attending and resident physicians, nurses, students, technicians and support staff, as well as subspecialty consultants, is charged with managing a varying, often overwhelming volume of patients with a wide range of clinical illnesses [2]. Such environments, where decisions are made under pressure and with incomplete information, have been considered more conducive to error [3].
A major theme that has arisen within the context of these errors is the frequency and potential risk of misidentification in the ED – misidentification of patients, study requisitions and patient laboratory specimens [4]. Factors such as the number of patients, the urgency of individual cases, the ability of patients to communicate (e.g. impaired consciousness), language barriers, low staff to patient ratios, and time pressures can all contribute to the risk [4]. In this type of setting, personnel are often prone to “workarounds”, defined as strategies or work patterns that bypass procedural codes in an effort to improve efficiency or productivity, but often with increased risk of error.
To understand the functioning of the healthcare system and to successfully address medical errors, it is necessary to study those components whose complex relationships constitute the system - humans, technologies and their interactions [5–9]. The study of human factors is an integral part of current safety research [10]. Human error in medicine can range from diagnostic errors to medication errors and has a spectrum of associated cognitive mechanisms [11, 12]. Zhang and colleagues describe a hierarchy of the healthcare system that elucidates the role of the individual in the causation of error [13]. Although most errors can be traced to actions (or inactions) of an individual, the root causes of errors go beyond a single individual [11, 14]. Patient safety research has expanded to study team interaction and collaborative decision-making [15, 16], the interaction of humans and technology [17–19], organizational issues [5, 18], institutional functions and national regulations [20]. Even though medical error is rarely due to only one of these factors, traditional patient safety research has not used an integrated approach to study error. As illustrated by Reason’s “Swiss cheese” model, medical error is more likely due to a combination of various miscues [11] (like holes in Swiss cheese) that must all line up to allow an error to occur. Perhaps even more alarming is the recognition that near-misses might be more prevalent than previously supposed, because they remain unreported when events do not end in any significant harm [17]. These events are corrected by “filters” in the system, in the form of human operators that act to rectify the results of previous events [17]. The question of whether such filters benefit patient safety needs to be considered in terms of immediate and long-term consequences. In the short term, filters can be effective in avoiding error but do not address larger, system-wide problems that promote error. They do not rectify the root causes of unsafe practices and may even mask the true extent of the problem and allow situations to repeat.
One aspect of medical errors where such filters play a significant role is that of misidentification. Incidents of misidentification or mislabeling are often caught prior to an adverse event and are often not reported. The failure to report misidentifications probably owes to the fact that the personnel fail to note the significance of these errors when caught prior to an adverse event. Some may feel that, if not identified by them, other fail-safes would have prevented an adverse event down the line. Unfortunately, adverse events usually occur as a result of a confluence of several errors – failure of fail-safes or lack of fail-safes [10, 18]. The presence of filters and the failure to report misidentification does not allow for the development or installation of systems or processes that would prevent future occurrences.
Despite increased recognition of the problem of misidentification of patients and samples [21], few researchers have looked at the dynamics of errors at the point of patient registration, where such misidentification usually occurs. At the time of initial registration, the information about the patient presenting to the ED is often far from complete or reliable. In the ED, some patients are unresponsive, unconscious or otherwise incapable of communication [4, 22]. Some are too ill or unstable to allow collection of this information in a timely fashion. Others communicate inaccurate information for a variety of personal and other reasons. Finally, some registration personnel noting existing patient demographic data in the database do not reconfirm this information, in order to save time.
The current study was conducted in the naturalistic environment of the ED in order to characterize the factors that compromise patient safety at the point of patient registration. Using ethnographic techniques of observation and interviews, data were gathered in the adult ED of a large academic tertiary care hospital in New York City.
Background
The true extent and seriousness of the impact of medical errors came to the forefront of the healthcare debate with the publication of the Institute of Medicine report in 1999 [5]. In this report, it was estimated that as many as 98,000 deaths per year result from various errors in hospitals. Critical care environments were identified as particularly vulnerable to errors due to their dynamic and complex systems. In addition, the Harvard Medical Practice Study reported that approximately 1.5–3% of observed adverse events occurred in the emergency department [23].
A major issue of concern has arisen in the form of misidentification of patients at various stages of care. It has formed the basis of many analyses of errors and has been one of the main goals of patient safety movement in the past several years [20, 24]. A recent analysis of voluntary near-miss reporting showed that 11% of the near-misses at 54 neonatal intensive care units in the United States involved patient misidentification [25]. In addition, during a three-year study, the Veterans Affairs National Center for Patient Safety received more than 100 reports of patient misidentification. Of these, 22% involved cases of medication administration (See [25]). Unfortunately, the root causes of these errors, such as the failure to read the chart or wristband and failure to obtain patient information correctly, have not been adequately studied. It is important to note that some of these errors occur despite complete adherence to the policies and procedures for proper identification of patients. A national sample of 712 hospitals reported 5.5% error rates for mislabeling and misidentification of patient’s wristbands. Of these, approximately half the cases involved missing wristbands, while the other half included more than one wristband with conflicting information (18.3%), wristbands with incomplete information (17.5%), erroneous information (8.6%), or illegible data (5.7%). Less than one percent of cases involved patients wearing wristbands with another patient’s data [26].
Of note, cases of patient misidentification are highly under-reported, rarely appearing in incident reports. This may be partly due to the fact that these errors are often caught before turning into adverse events and are therefore not considered important for reporting [4]. Furthermore, this lack of reporting may be caused by the fear of reproach or embarrassment [27, 28].
Theoretical Framework
The theoretical framework that guided this research is the theory of distributed cognition. Distributed cognition is a scientific discipline in cognitive science that is concerned with how cognitive activity is distributed across internal (human cognitive processes) and external cognitive artifacts (computers, telephones, charts), members of groups, and space and time [29–33]. Distributed cognition provides a unique framework to describe the interactions, processes, and knowledge structures critical to cognitive tasks in the healthcare environment. It allows researchers to focus on complex informational, social, organizational, and cognitive issues involved in team interactions with information technologies within a distributed, collaborative environment. The core unit of analysis is the functional system composed of human and artificial agents and their relations, which are distributed across time and space [32–34]. Distributed cognition can lead to discoveries concerning how interactions between agents are coordinated, how artifacts and tools are really used, and how errors occur as a result of interactions among the components of the system.
The ED is a prototypical distributed cognitive system. ED personnel have to manage many patients at the same time, constantly prioritizing tasks and dividing their attention between all their patients. They must interact with paper and electronic artifacts, other ED personnel and consultants while also managing interruptions, dealing with time pressure and stress, and communicating information to personnel at the next shift. Human errors in a distributed, dynamic environment such as the ED are viewed as products of cognitive activities in people’s adaptation to their complex physical, social, and cultural environments.
As mentioned earlier, little attention has been paid to the first step in the process of patient identification, namely, registration [27]. As the data indicate, these errors occur more often than one expects and certainly more often than are reported. Therefore, the aim of this study is to analyze a similar set of errors and look more closely at the underlying causes from the perspective of distributed cognition. In our previous work, we developed a model for the role of interruptions, multitasking and handoffs as critical factors contributing to medical errors [10]. The focus of the current study is on specific cases of errors that occurred as a result of multiple factors in the distributed cognitive system. The goal is to determine the root causes of these errors and the processes in the distributed cognitive system, the procedures and the mitigating circumstances that led to these errors.
Methods
Study Setting
The study site is an adult urban ED in the Washington Heights section of northern Manhattan and has an annual census of approximately 70,000 patients. The population is 61% Hispanic, 18% African American, and 17% White. Twenty-five percent of patients arrive via ambulance. The admission rate for patients seen by a provider is 23%. The ED is staffed with attending emergency physicians and residents. The hospital’s Institutional Review Board approved the study and measures were taken to preserve the confidentiality of the data sources and patients.
Data Collection
Data were collected using ethnographic techniques of observations and interviews. Short-term observational studies focus on group behaviors and findings of a short-term qualitative study are presented based on the recorded observations [10]. Detailed, semi-structured interviews were also conducted to supplement the observation data [10].
Observation
The key aspect of qualitative research is the observation of phenomena in natural settings. During a period of three months, two researchers (one a physician) observed the activities unfolding in the emergency department and recorded their observations at different representative times of the day. In order to be as objective as possible, the physician researcher was not responsible for patient care and did not take part in the decision-making process. Observational data were collected in order to provide insight into the cognitive workflow, information transfer and decision-making processes in the ED [35, 36]. Each set of observations occurred for approximately three hours, usually in two separate shifts (morning and afternoon).
Interviews
Interviews were guided conversations where open-ended questions were asked. New questions were allowed to arise as a result of the discussion. The prepared questions focused on two broad themes including the general policies and procedures within ED registration, and the coping mechanism of the registration staff with regard to handling the large number of patients and timely processing of incoming cases.
Data Analysis
Observational and interview data were subsequently analyzed. First, a basic workflow model of ED registration was synthesized. Each error was analyzed individually in order to trace the origin of the errors and, more importantly, the point at which the ideal workflow of the registration broke down, resulting in the occurrence of the errors. This was achieved by thorough analysis of the observation data and the tape-recorded activities at the point of detection of the error and through the encounter with the patient. The observational data was subsequently supplemented with the interview data in order to form a comprehensive view of the course of events. Furthermore, the policies and procedures manual for ED registration was reviewed in order to fully understand the safeguards in place against such errors. Interviews with members of the ED registration staff were aimed at gaining an understanding of the workarounds and shortcuts taken by the staff in order to keep apace of the volume of patients.
Results
During the observations, four specific classes of problem were detected which are reflected in the four cases of errors reported in this paper. All of these errors were subsequently recognized and rectified by the filters within the system. As discussed in the following sections, these incidents of error constitute cases of near-misses that could have had potential adverse impact on the patients. All errors, except for case two, were discovered and subsequently corrected during one three-hour observation session on May 28, 2005 (case two was discovered in an earlier shift that day). It is important to note that the actual initiation and incremental proliferation of these errors were on-going processes that occurred up to about 24 hours before discovery.
Case 1
This case was brought to the attention of the physician by the ED nurse. On examining the patient’s record, the nurse realized that the patient had two medical record numbers. The ED chart, all tests and prescriptions for this ED visit were under one medical record number while the patient’s previous medical records were under another number. This error was caused by the failure of the initial registration clerk to obtain the required identification information. The patient was assumed to be new to the hospital and a new medical record number was generated. As a result, none of the prior medical information was available to the physician for this visit. Upon detecting the problem, the physician contacted the registration clerk and the two record numbers were combined.
Case 2
Ms. G was a 22-year-old pregnant woman who came to the ED for a fetal ultrasound. While being interviewed, it was discovered that the patient had been treated at the hospital two days earlier and had some tests done. However, none of this information was present on the hospital’s online medical information system under her name or medical record number. Upon further investigation, it was discovered that she had been given two medical record numbers, and that the test results were under the second number.
Case 3
A 20-year-old woman with sickle cell disease came to the ED with symptoms of bacterial pharyngitis. The patient was prescribed a five-day course of the antibiotic, azithromycin. The physician discussed the medication and the follow-up plan with the patient. He told her that a nurse would call her to check on the status of her illness. Upon inspecting her prescription, the patient noticed that the address recorded was incorrect. Investigation revealed that the patient was never given a registration form to complete upon arrival to the ED. Since the patient was found to have existing information in the hospital computer system, she was not asked for updated information. After being prompted by the physician, the registration clerk updated the patient’s demographic data.
Case 4
A young woman was brought into the emergency department after a motor-vehicle accident. The patient was fully conscious and communicative. While at the patient’s bedside, the attending and training physicians undertook a discussion of her case. During this period of discussion, the patient interrupted the attending-resident conversation to note that she was not the patient of whom they were speaking. The physicians referred to the patient’s chart and the wristband and discover that the name on both the chart and the wristband were incorrect. It was discovered that two patients were brought to the ED at approximately the same time with the result that the registration staff mismatched their identities. Corrections were made to the ED charts and wristbands of both patients. Fortunately, no adverse effects resulted from this error.
Summary of Results
During the course of the observations, four separate types of errors were discovered. All four cases were determined to have originated during the registration process. In each case, the error was eventually caught and no adverse events occurred. Nevertheless, these results represent four cases of “near-miss” that may have resulted in negative outcomes for the patients, if not caught in time.
Discussion and Commentary
Errors in Distributed Cognition
The process of ED registration involves numerous agents and artifacts, including the registration clerks, the patients, the EMS personnel, computers, telephones, charts and wristbands. Like all other aspects of the ED, the artifacts in ED registration are involved in a highly intertwined and dynamically complex fabric of interactions. As a testament to the tremendous workload of ED registration, the registrars must collect several pieces of information on each patient while processing an average of 200 patients/day. In addition, the registration clerks have different avenues via which they can achieve their goal - retrieval of the patient’s demographic data (fig. 1). Most often the information is provided by the patient directly. On other occasions, when the patient cannot provide the information, it is obtained through a third party - a relative or caretaker, or, in some cases, the EMS personnel. Third party data collection creates a susceptibility to breakdown of communication and potential errors (Step 1). The retrieved patient information is subsequently entered into the registration computer system (Step 2). The information entered at this level consists of a set of data required for proper patient identification. It is important to note, however, that not all patients possess or are willing to share the required set of information necessary for registration. In such cases, the patient is admitted with little or no identifying information. This is one of the major factors in introduction of errors into the process of registration. Furthermore, the computer system is designed to run the patient information against the hospital database to find if the patient has any previous records in the hospital. If so, the patient is registered under the existing medical record number. However, if no matching information is found, then the patient is given a new record number and is registered as a new patient. Once registration data is entered, ED registration procedure dictates that the information is read back to the patient and the patient is asked to confirm the information. Finally, the registration clerk imprints the paper ED chart with the patient’s information and creates a patient wristband. The registration clerk must return to the patient, reconfirm his identity and apply the wristband to the patient (Step 3).
Figure 1.
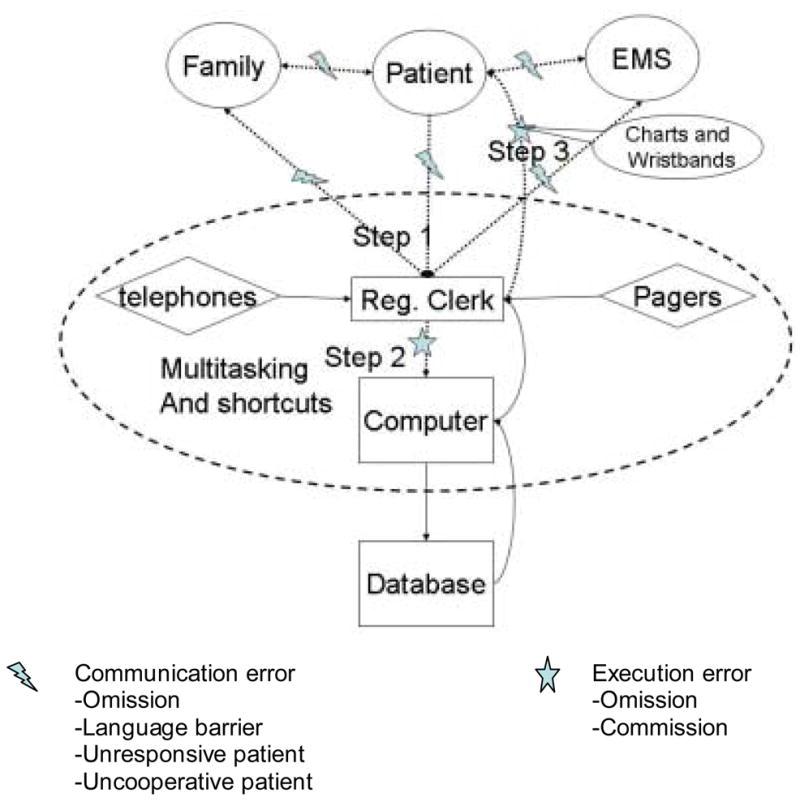
The dotted lines represent the points of communication that are prone to error.
A Coherent Theme
The errors discussed above represent a unified theme and source of error, namely ED registration. Our observations and interview data revealed the nature of ED registration as one of high stress and high patient volume environment where individual patients must be processed quickly and efficiently [37]. As such, the registration staff is often interrupted and need to constantly reprioritize their set of tasks in order to meet the changing demands of their work environment [4]. This results in a considerable amount of multitasking, and a consequently high level of cognitive load on the staff. In addition, in order to process the patients in the shortest time possible, staff members tend to adopt a number of workaround protocols [22, 38]. It should be noted that study observations took place only during morning and afternoon shifts, although the types of errors described in this paper could occur during any shift. As we have pointed out, times of work overload and high patient volume promote increased error rates.
As is the case with all errors of this nature, the responsibility for the error cannot be entirely placed at any one point [11, 14]. Although it is ultimately the omission by one individual that results in the creation of the error [13], it is often a result of the overall system failure particularly that of the cognitive workload placed upon an individual care provider at a point in time [11, 22, 38]. Similarly, the discovery and subsequent correction of these errors result from the so-called “Swiss Cheese” model where, in most cases, the errors are finally caught and rectified by the system [11]. As such, these errors are called “near-miss” events because they are caught before resulting in an adverse event [39].
As figure 1 indicates, each error represents a breakdown in the overall distributed cognitive system that defines the registration desk and the emergency room. Cases 1 and 2 represent possible failures in communication and/or data entry into the computer (Step 1: figure. 1). The fact that the patients were given multiple record numbers suggests two possible scenarios: 1) it is possible that the registration clerk failed to get all the necessary information from the patients or their caretaker/EMS personnel. As a result, incorrect or incomplete information was entered into the computer, resulting in the failure of the system to recognize that the patient had visited the hospital on a prior occasion; 2) the other possibility is that while the information was correctly obtained from the patient, it was subsequently entered into the computer incorrectly. Interviews with the registration staff revealed that the system can only match records if the content is an exact match. Otherwise, the patient is given a new record number. In either scenario, when the computer compared the entered information with the hospital database, no matches were found and the patients were consequently assigned new record numbers.
On the other hand, the third case is a clear instance of the failure of the registration staff to update patient data, by failing to ask for any changes with regard to the patient’s information. As a result, the change in address was never noticed until the patient realized that the address on her file was an old one (Step 1).
In the first three cases of error (two cases with multiple medical record numbers and one case with wrong patient address), it can be inferred that the problem had arisen due to an incompatibility between the skills of the staff and the computer system used for registration [40]. This fact was reflected in the interviews with the registration staff, all of whom expressed their frustration with the system and the fact that “the system was too exact and not user-friendly”. In two cases (Cases 1 and 2), although the patients had already been to ED on prior occasions, ED registration had assigned them a new medical record number. As such, although all of their previous medical information including the laboratory and other test results were present within the system, the physicians were unaware of their existence. In the third case, although the patient had only one record number, the registration staff did not reconfirm the patient’s demographic information on the second visit and hence omitted to update the patient’s address and telephone number. It was stated during the interviews that when patients mention that they have previously visited the ED, their information is often not updated in order to save time. As evident in these cases, the process of shortcuts and workarounds, combined with the inherent difficulty in the functionality of the computer system, results in the occurrence of errors and potentially adverse events.
In these cases, it is possible that improvements in the computer system as well as better training of the staff to use the system can result in significant reduction of such errors. Indeed, if the computer systems used at ED registration are as difficult to work with as expressed by the registration staff, then the technology is actually facilitating the errors rather than preventing them [40].
The fourth case of registration error is of a different and conceivably more serious nature. In retrospect, it appears that this error resulted from the fact that two patients with similar physical and demographic characteristics and complaints arrived during the same, high volume time. The registration clerk generated the proper ED charts with correct information but, in the rush to process the charts through ED registration, incorrect name stamps were placed on the charts and the patients were incorrectly wrist-banded (Step 3). A failsafe exists to prevent this type of error. Any personnel applying a wristband to a patient is required to identify the patient by two means. In this scenario, this procedure was obviously not followed and it required another intervention (in this case, by the patient) to correct the error. This is clearly a cognitive error resulting from the high volume of patients, the constant distractions and, more importantly, the tendency of ED registration staff to work around the safety protocols established to avoid precisely this sort of error. It is also important to note that although in this particular case the error was identified by an attentive alert patient, this is not always the case. The patient may be unresponsive or uncooperative. On the other hand, at times, even confirmation with the patient may not be enough of a failsafe. Rosenthal reported the case of an anxious patient who mistakenly confirmed the wrong name, wrong diagnosis and wrong procedure, as the nurse read the information to her, hence creating a situation of “Uninformed Consent” [27, 41]. In such cases, additional steps must be taken to ensure patient safety.
Whereas in the previous cases, the use of technology could result in significant improvements, in this case technology improvement could only provide a partial solution. The issue here is the work demand pressuring the registration personnel to cut corners. The primary solution is to address the intense work environment. The employment of more registration personnel would reduce the volume of work and promote adherence to policies and procedures with less need for workarounds. The implementation of wireless computers to do bedside registration would encourage the registration personnel to concentrate on one patient at a time and would likely reduce error.
Implications
The ED is a unique clinical environment and requires distinctive solutions to address the workflow issues that contribute to the occurrence of medical error. Although long-term solutions must be sought to reduce the root causes of error, the adaptive behavior of the human components of this system must also be bolstered. Although the adoption of technology may benefit the ED, the results of this study suggest that the existing generic electronic tools alone may be ill-suited for this environment. These tools must be tailored to support adaptive processes like multitasking and handoffs that occur in a time-constrained environment [10]. In study interviews, the registration staff expressed a consistent pattern of frustration with the existing technology. In every interview, the system was referred to as “too exact”, “not user friendly” and “difficult”. This suggests that steps must be taken to improve the usability of the computer system, coupled with proper training of the staff, in order to prevent errors of this nature. It is vital that usability studies be conducted in order to fully understand the nature and extent of this problem [42].
Other important issues arising from this study are the problem of ED over-crowding and the high patient/staff ratio. These issues are particularly significant at ED registration - a crucial component of ED functioning. Subsequently, any error created at this level would propagate for as long as it goes undiscovered. It is therefore vital that attention be paid to these problems and considerable effort must be made at the policy level to increase the number of staff in ED registration.
Conclusions
As the initial step of patient care in the ED, patient registration must be both efficient and accurate. Failure to meet both of these goals can lead to adverse outcomes. Slow registration can impede care by delaying the processing of orders of tests or delaying access to existing medical records and in the long run not providing adequate emergency care. Inaccuracy in gathering information can lead to a myriad of errors, including lack of access to existing medical records, inability to contact a patient after discharge and even implementation of an incorrect treatment regimen with dangerous consequences to the safety of the patient.
Errors often occur, not as a result of the failure of a single entity within the system, but as a result of the breakdown of the system [13]. These failures have many underlying causes, including but not limited to the heavy patient volume, the need to multitask and the inevitable tendency to work around the established procedural codes [10]. Whereas in some cases technological solutions can improve the situation, in others, they could very well lead to more errors or automate the errors that exist within the system.
Acknowledgments
This research was supported by grant R01 LM07894 from the National Library of Medicine to Vimla Patel. We thank the nurses, doctors and the administrative staff at the New York Presbyterian Hospital - Columbia University Medical Center Emergency Department for their participation and support of this study. Special thanks are extended to the subjects who participated in the interview portion of our project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Croskerry P, Shapiro M, Campbell S, LeBlanc C, Sinclair D, Wren P, Marcoux M. Profiles in Patient Safety: Medication Errors in the Emergency Department. Acad Emerg Med. 2004;11(3):289–99. doi: 10.1111/j.1553-2712.2004.tb02214.x. [DOI] [PubMed] [Google Scholar]
- 2.Kovacs G, Croskerry P. Clinical decision making: an emergency medicine perspective. Acad Emerg Med. 1999;6(9):947–952. doi: 10.1111/j.1553-2712.1999.tb01246.x. [DOI] [PubMed] [Google Scholar]
- 3.Brixey JJ, Robinson DJ, Johnson CW, Johnson TR, Turley JP, Patel VL, et al. Towards a hybrid method to categorize interruptions and activities in healthcare. Int J Med Inform. 00:000–00. doi: 10.1016/j.ijmedinf.2006.09.018. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaplan H. Transfusion “Slip”. AHRQ: Morbidity and Mortality Rounds on the Web. [Date Accessed: June. 5. 2006];2004 URL: http://webmm.ahrq.gov/case.aspx?caseID=50&searchStr=Transfusion+%22Slip%22.
- 5.Kohn LT, Corrigan JM, Donaldson MS, editors. To err is human: Building a safer health system. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 6.Alvarez G, Coiera E. Interruptive communication patterns in the intensive care unit ward round. Int J Med Inform. 2005;74:791–6. doi: 10.1016/j.ijmedinf.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 7.Anderson JG, Ramanujam R, Hensel D, Anderson MM, Sirio CA. The need for organizational change in patient safety initiatives. Int J Med Inform. 2006;75(12):809–817. doi: 10.1016/j.ijmedinf.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 8.Ash JS, Sittig DF, Dykstra RH, Guappone K, Carpenter JD, Seshadri V. Categorizing the unintended sociotechnical consequences of computerized provider order entry. Int J Med Inform. 00:000–000. doi: 10.1016/j.ijmedinf.2006.05.017. in press. [DOI] [PubMed] [Google Scholar]
- 9.Balka E, Doyle-Waters M, Lecznarowicz D, FitzGerald JM. Technology, governance and patient safety: Systems issues in technology and patient safety. Int J Med Inform. 00:000–000. doi: 10.1016/j.ijmedinf.2006.05.046. in press. [DOI] [PubMed] [Google Scholar]
- 10.Laxmisan A, Hakimzada F, Sayan O, Green R, Zhang J, Patel V. The multitasking clinician: Decision-making and cognitive demand during and after team handoffs in emergency care. Int J Med Inform. 00:000–000. doi: 10.1016/j.ijmedinf.2006.09.019. in press. [DOI] [PubMed] [Google Scholar]
- 11.Reason JT. Human error. Cambridge, England: Cambridge University Press; 1990. [Google Scholar]
- 12.Beuscart-Zéphir M-C, Pelayo S, Anceaux F, Maxwell D, Guerlinger S. Cognitive analysis of physicians and nurses cooperation in the medication ordering and administration process. Int J Med Inform. 00:000–000. doi: 10.1016/j.ijmedinf.2006.05.022. in press. [DOI] [PubMed] [Google Scholar]
- 13.Zhang J, Patel VL, Johnson TR, Shortliffe EH. A cognitive taxonomy of medical errors. Journal of Biomedical Informatics. 2004 Jun;37(3):193–204. doi: 10.1016/j.jbi.2004.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Woods DD, Cook RI. National Patient Safety Foundation (U.S.) From Counting Failures to Anticipating Risks: Possible Futures for Patient Safety. In: Zipperer LA, Cushman S, editors. Lessons in patient safety. Chicago, IL: National Patient Safety Foundation; 2001. p. xiv.p. 134. [Google Scholar]
- 15.Patterson ES, Roth EM, Woods DD, Chow R, Orlando J. Handoff strategies in settings with high consequences for failure: lessons for health care operations. International Journal for Quality in Health Care. 2004;16(2):125–32. doi: 10.1093/intqhc/mzh026. [DOI] [PubMed] [Google Scholar]
- 16.Patel VL, Cytryn KN, Shortliffe EH, Safran C. The Collaborative Health Care Team: The Role of Individual and Group Expertise. Teaching and Learning in Medicine. 2000;12(3):117–32. doi: 10.1207/S15328015TLM1203_2. [DOI] [PubMed] [Google Scholar]
- 17.Laxmisan A, Malhotra S, Keselman A, Johnson TR, Patel VL. Decisions about critical events in device-related scenarios as a function of expertise. J Biomed Inform. 2005;38(3):200–12. doi: 10.1016/j.jbi.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 18.Bates DW, Cohen M, Leape LL, Overhage JM, Shabot MM, Sheridan T. Reducing the frequency of errors in medicine using information technology. J Am Med Inform Assoc. 2001;8(4):299–308. doi: 10.1136/jamia.2001.0080299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McAlearney AS, Chisolm DJ, Schweikhart S, Medow MA, Kelleher K. The story behind the story: Physician skepticism about relying on clinical information technologies to reduce medical errors. Int J Med Inform. 00:000–000. doi: 10.1016/j.ijmedinf.2006.09.021. in press. [DOI] [PubMed] [Google Scholar]
- 20.National Patient Safety Goals for 2006: Joint Commission on Accreditation of Healthcare Organizations; 2006. URL: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/06_npsgs.htm
- 21.National patient safety goals: Joint Commission on Accreditation of Healthcare Organizations Web site; 2004. URL: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/2004_npsgs.htm?
- 22.Pape T. Applying airline safety practices to medication administration. Medsurg Nurs. 2003;12:77–93. [PubMed] [Google Scholar]
- 23.Leape LL, Brennan TA, Laird NM, Lawthers AG, Localio AR, Barnes BA, et al. The nature of adverse events in hospitalized patients. Results of the Harvard Medical Practice Study II. N Engl J Med. 1991;324(6):377–84. doi: 10.1056/NEJM199102073240605. [DOI] [PubMed] [Google Scholar]
- 24.National patient safety goals: Joint Commission on Accreditation of Healthcare Organizations Web site; 2005. URL: http://www.jointcommission.org/PatientSafety/NationalPatientSafetyGoals/05_npsgs.htm
- 25.Suresh G, Horbar J, P P, et al. Voluntary anonymous reporting of medical errors for neonatal intensive care. Pediatrics. 2004;113:1609–18. doi: 10.1542/peds.113.6.1609. [DOI] [PubMed] [Google Scholar]
- 26.Renner SW, Howanitz PJ, P B. Wristband identification error reporting in 712 hospitals. A College of American Pathologists’ Q-Probes study of quality issues in transfusion practice. Arch Pathol Lab Med. 1993;117:573–7. [PubMed] [Google Scholar]
- 27.Rosenthal M. Check the Wristband. AHRQ: Morbidity and Mortality Rounds on the Web. [Date Accessed: June 5 2006];2003 URL: http://www.webmm.ahrq.gov/case.aspx?caseID=22&searchStr=misidentification#ref2.
- 28.Osborne J, Blais K, JS H. Nurses’ perceptions: when is it a medication error? J Nurs Adm. 1999;29:33–8. doi: 10.1097/00005110-199904000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Hutchins E. How a cockpit remembers its speed. Cognitive Science. 1995;19:265–88. [Google Scholar]
- 30.Norman DA. Cognitive Artifacts. In: Carroll JM, editor. Designing interaction: Psychology at the human-computer interface. New York: Cambridge University Press; 1991. [Google Scholar]
- 31.Zhang J. A distributed representation approach to group problem solving. J Am Society Inform Sci. 1998;49(9):801–9. [Google Scholar]
- 32.Zhang J, Norman DA. Representations in distributed cognitive tasks. Cog Sci. 1994;18(1):87–122. [Google Scholar]
- 33.Cohen T, Blatter B, Almeida C, Shortliffe EH, Patel VL. Distributed cognition in the psychiatric emergency department: A cognitive blueprint of collaboration in context. Artif Intell Med. 2006;37(2):73–83. doi: 10.1016/j.artmed.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Hutchins E. Cognition in the wild. Cambridge, MA: MIT Press; 1995. [Google Scholar]
- 35.Patel VL, Kaufman D, Magder SA. The Road To Excellence: The Acquisition Of Expert Performance In The Arts And Sciences Sports And Games. Hillsdale, NJ: Lawrence Erlbaum publishers; 1996. The acquisition of medical expertise in complex dynamic medical environments; pp. 127–65. [Google Scholar]
- 36.Strauss A, Corbin J. Basics of qualitative research: Techniques and procedures for developing grounded theory. 2. Thousand Oaks, CA, US: Sage Publications, Inc; 1998. [Google Scholar]
- 37.Morrissey J. Quality vs. quantity. IOM report: Hopsitals must cut back workload and hours of nurses to maintain patient safety. Mod Healthc. 2003;33:8–11. [PubMed] [Google Scholar]
- 38.Pape T. Workaround Error. AHRQ: Morbidity and Mortality Rounds on the Web. [Date Accessed: June. 5.2006];2006 URL: http://www.webmm.ahrq.gov/case.aspx?caseID=118&searchStr=workaround.
- 39.Shojania K. Patient Mix-Up. AHRQ: Morbidity and Mortality Rounds on the Web. [Date Accessed: June. 15. 2006];2003 URL: http://www.webmm.ahrq.gov/case.aspx?caseID=1&searchStr=patient+mix-up.
- 40.Coiera E. Interaction design theory. Int J Med Inform. 2003;69:205–22. doi: 10.1016/s1386-5056(02)00106-5. [DOI] [PubMed] [Google Scholar]
- 41.Chassin M, Becher E. The wrong patient. Ann Intern Med. 2002;136:826–33. doi: 10.7326/0003-4819-136-11-200206040-00012. [DOI] [PubMed] [Google Scholar]
- 42.Kushniruk AW, Patel VL. Cognitive and usability engineering methods for the evaluation of clinical information systems. J Biomed Inform. 2004;37(1):56–76. doi: 10.1016/j.jbi.2004.01.003. [DOI] [PubMed] [Google Scholar]


