Abstract
Objective
African-American girls and women are at high risk of obesity and its associated morbidities. Few studies have tested obesity prevention strategies specifically designed for African-American girls. This report describes the design and baseline findings of the Stanford GEMS (Girls health Enrichment Multi-site Studies) trial to test the effect of a 2-year community- and family-based intervention to reduce weight gain in low-income, preadolescent African-American girls.
Design
Randomized controlled trial with measurements scheduled in girls’ homes at baseline, 6, 12, 18 and 24 months post randomization.
Setting
Low-income areas of Oakland, CA.
Participants
Eight, nine and ten year old African-American girls and their parents/caregivers.
Interventions
Girls are randomized to a culturally-tailored after school dance program and a home/family-based intervention to reduce screen media use versus an information-based community health education active-placebo comparison intervention. Interventions last for 2-years for each participant.
Main Outcome Measure
Change in body mass index over the two-year study.
Results
Recruitment and enrollment successfully produced a predominately low-socioeconomic status sample. 261 families were randomized. One girl per family is randomly chosen for the analysis sample. Randomization produced comparable experimental groups with only a few statistically significant differences. The sample had a mean body mass index (BMI) at the 74th percentile on the 2000 CDC BMI reference, and one-third of the analysis sample had a BMI at the 95th percentile or above. Average fasting total cholesterol and LDL-cholesterol were above NCEP thresholds for borderline high classifications. Girls averaged low levels of moderate to vigorous physical activity, more than 3 hours per day of screen media use, and diets high in energy from fat.
Conclusions
The Stanford GEMS trial is testing the benefits of culturally-tailored after-school dance and screen time reduction interventions for obesity prevention in low-income, preadolescent African-American girls.
Keywords: obesity prevention, children, diet, physical activity, television, sedentary behavior, health disparities, randomized controlled trial
INTRODUCTION
The United States has experienced dramatic increases in obesity among both children and adults.1, 2 Some of the greatest increases have occurred among African-American girls. National surveys from 1963 to 2002 demonstrate that the prevalences of child and adolescent obesity have more than tripled among African-American girls, with the majority of those increases occurring since 1980.3, 4 In the 1999-2002 NHANES, 23.2% and 40.1% of 6-19 year old non-Hispanic black girls had body mass index (BMI) ≥ 95th and 85th percentiles on the 2000 CDC growth references, respectively.4 BMI differences between white and black girls are already present prior to age six, significantly widen in older age groups, and are independent of socioeconomic status.5 Obesity in children and adolescents has been associated with hypertension, dyslipidemias, early atherosclerotic lesions, hyperinsulinemia, insulin resistance and type 2 diabetes mellitus, and other medical, psychological, and social complications.6
Reviews of cardiovascular disease and cancer risk reduction studies in children and adolescents suggest that body weight may be more difficult to change than other risk factors.7-9 Although many diet and physical activity interventions have increased knowledge or improved attitudes about healthful behaviors, very few successfully changed self-reported health behaviors, and most have not succeeded in reducing body fat or weight gain.7, 10 Few studies have tested intervention strategies specifically designed for African-American girls and their families.
GEMS (Girls’ health Enrichment Multi-site Studies) is a National, Heart, Lung, and Blood Institute (NHLBI)-sponsored collaborative effort to develop and test interventions to reduce weight gain in African-American preadolescent girls. Phase 1 was a development and pilot study phase, completed in May 2002.11-16 Phase 2 involves two field centers, Stanford University and University of Memphis, and the project office of the NHLBI, in full-scale clinical trials. Stanford and Memphis are each testing their own distinct interventions informed by the collaborative planning, experience and results from all centers in Phase 1, to enhance the quality of each trial in Phase 2.17 The two field centers are collaborating with a common primary outcome, eligibility criteria and a core set of measures and procedures. However, GEMS is not a “multi-center clinical trial” in the usual sense, because each field center is evaluating its own intervention. As a result, each study has high internal validity. This paper describes the design and baseline participant characteristics of the Stanford GEMS trial.
METHODS
General Design
Stanford GEMS is a 2-arm parallel group, randomized controlled trial to test the efficacy of a culturally-tailored after school dance program and a family-based intervention to reduce television, videotape and video game use to reduce body mass index gain among lower socioeconomic status African-American pre-adolescent girls. Participants are randomized to the dance and television reduction intervention versus an information-based community health education intervention for 2 years.
Recruitment and Screening
To enroll African-American families with lower socioeconomic status, we focused recruitment in neighborhoods in Oakland, CA, around elementary schools most likely to be disproportionately serving this population; ie.,those with high African-American enrollments, high rates of free or reduced price meals and poor standardized test score performance. We performed all assessments in participants’ homes, eliminating the need for families to come to a clinical research center. Recruitment strategies were based on the most successful methods from Phase 1,15, 18 making presentations and distributing fliers to girls and parents at existing after-school programs, schools, churches, and neighborhood and community events (e.g., street fairs, Juneteenth celebrations, African-American cultural events), and making individual presentations to parents and girls in commercial locations (e.g., food stores, new store openings). We also presented the project to school parent groups, church groups, and Parks and Recreation Department staff, to enhance the visibility of Stanford GEMS, especially among community opinion leaders, building upon relationships established during Phase 1. Interested families were given a description of the study and screened by telephone for inclusion and exclusion criteria. Potentially eligible families were scheduled for a home data collection visit to confirm eligibility, complete informed consent and assent, and conduct baseline assessments.
Eligibility criteria and exclusions
Girls were required to be African-American (identified as “African-American or Black” by her parent/guardian) and age 8, 9, or 10 years on the date of randomization. To focus on girls at higher risk of subsequent obesity, girls were required to have a BMI ≥ 25th percentile for age (2000 CDC growth charts) and/or at least one overweight parent/guardian (BMI ≥ 25 kg/m2).19 Girls were allowed to participate but excluded from the primary analysis sample if they had a BMI > 35 kg/m2 to prevent outliers and limit excessive variability to potentially enhance statistical power for the primary analysis. As a community-based prevention program, the eligibility criteria were designed to be liberal, to maximize the generalizability of the results of the trial. However, girls were excluded if they: had been diagnosed with a medical condition (e.g., Prader-Willi syndrome, type 1 diabetes, inflammatory bowel disease, cystic fibrosis, eating disorders) or were taking medications affecting growth; had a condition limiting their participation in the interventions or assessments; were unable to understand or complete informed consent; planned to move from the San Francisco Bay Area within the next 24 months; were homeless; or had no television.
Randomization
After completing baseline measures families/households were randomized by computer, stratified by baseline BMI of a randomly chosen eligible girl within each family/household (two strata defined by the mean BMI from the Phase 1 Stanford GEMS Pilot Study baseline sample; ≤21.4 kg/m2 vs. >21.4 kg/m2) using Efron’s biased coin randomization to produce similar sample sizes in each group.20
Interventions
The background, rationales and conceptual models for both the Treatment intervention and the Active-Placebo Comparison intervention were described previously,15 and were shaped by extensive formative research and the Phase 1 Stanford GEMS pilot study.15, 21 The interventions are designed to be implemented over the full two years in response to the limited success of short-term interventions in past research targeted at children.7, 10
The Treatment Intervention
Bandura’s social cognitive model22, 23 served as the foundation for intervention design. In order to incorporate African-American culture into our intervention, we emphasized elements to address both surface structure (e.g., culturally matched models, music, language) and deep structure (e.g., values, social and historical influences).24 Surface structure is addressed through culturally-matched staff, music chosen by the participants, and the selection of dance as physical activity.15 To address deep structure, we attempted to account for a number of elements associated with African-American culture (e.g., collectivism, importance of family, present orientation, importance of religiosity, sense of historical racism and prejudice, and use of social support as a coping mechanism).25-28 As part of our regard for deep structure, the Treatment intervention does not explicitly focus on obesity prevention. Instead, the results of formative research instructed us to emphasize a holistic concept of health that includes high self-esteem, spirituality and cultural awareness as well as physical health, a community atmosphere and social support, involving extended family members, and making explicit distinctions with racial majority and middle-class/upper-class value systems and norms. For example, choosing dance as an activity in which African-Americans are perceived to have superior skills compared to whites in the U.S., using dance styles with roots in African-American heritage and culture, acknowledging majority ownership and control of, and profiting from, mass media and marketing targeting African-Americans for consumption of unhealthful products and negative stereotypes, bringing attention to female African-American achievers who share a similar background to participants and/or maintained their independence from majority enterprises and interests, and identifying role models from within their own community.
The GEMS Jewels Dance Intervention
Based on our experiences in Phase 1,15 after school dance classes are offered five days per week, 12 months per year (excluding school holidays), at community centers near the selected neighborhoods. Each daily session lasts up to 2.5 hours (3:30-6:00 PM) and starts with a one-hour homework period. A small snack is then followed by 45-60 minutes of learning dance routines. Three styles of dance are taught: traditional African dance, Hip-Hop, and Step. The sessions include “GEMS talks” exploring the meaning of dance in girls’ lives, the importance of dance in the African-American community and culture, and costume and set preparation for performances. Additional activities to maintain motivation include: “GEMS Jamboree” dance performances approximately every 8 weeks for audiences of families and friends, including awards for each girl based on the seven Kwanzaa principles, Umoja (Unity), Kujichagulia (self-determination), Ujima (collective work and responsibility), Ujamaa (Cooperative Economics), Nia (purpose), Kuumba (Creativity), and Imani (faith); twice-monthly videotaped Kuumba classes to provide feedback; allowing girls to teach each other and choreograph routines; and performances at community events. Dance classes are led by female African-American college students and recent college or technical school graduates, from the local community where possible. These young women are intended to serve as role models for dance, the importance of maintaining cultural identity, and educational achievement, and are selected for these qualities. They are not selected based on their weight status and are generally expected to be a mix of normal weight and overweight women, but more fit than their peers in the local community. Although individual girls are the unit of study, the dance intervention can also be considered to be an “environmental” intervention, with girls attending as often as they wish. To eliminate the formidable transportation barrier that was discovered in Phase 1, we provide daily van transportation from girls’ schools to the participating community centers.
S.T.A.R.T. (Sisters Taking Action to Reduce Television) is a home-based screen-time reduction intervention designed specifically for African-American girls,15 including up to 24 lessons over two years. An African-American female “START mentor” schedules visits to meet with the family in their home to deliver each lesson. She acts as a behavior change partner and additional young adult female role model for the participating girl. The basic intervention model has been developed over several prior pilot studies.15, 29, 30 Activities within each lesson also focus on an element of African or African-American history or culture.
The Active-Placebo Comparison Intervention
Failing to consider and attend to negative attitudes towards science and “control groups” in the community can seriously jeopardize the conduct of a research trial. To address these, we chose an “active placebo” condition31, 32 consisting of state-of-the-art, culturally-tailored, information-based health education focused on nutrition, physical activity, and reducing cardiovascular and cancer risk, highlighting topics of particular relevance to African-American women, girls, and families, including ties to African history and heritage. It includes 24 monthly newsletters each for girls (Felicia’s Healthy News Flash) and their parents/guardians (Stanford GEMS Health Report), and quarterly community center health lectures (Family Fun Nights) led by professional health education staff from voluntary health organizations and our own research group, and African-American females where possible. The newsletters utilize standard educational materials from federal health agencies, voluntary health and professional organizations, and our own research team, with an emphasis on those designed for African-American audiences (e.g., soul food recipes). Where existing content was not available specifically for African-Americans, we added additional cultural tailoring to provide greater perceived relevance and individualization for our participants. In addition, the monitoring and incentive schedules employed for our experimental treatment procedures is also used to sustain participation of the active placebo control group. The two interventions were not matched in total intensity and frequency of contact, however, because the two approaches inherently differ in those domains. This active-placebo comparison intervention worked well in Phase 1, resulting in enthusiastic participation from parents and girls, without evidence of resentful demoralization or compensatory rivalry.33 Although this intervention contains ingredients that may produce effects on behaviors influencing weight gain, they are very different from the specific ingredients and intervention design principles operationalized in the Treatment intervention.
Assessments and measures
Data are collected in the participants’ homes by trained, female African-American research assistants, blinded to experimental assignment. By performing assessments in participants’ homes, we attempt to maximize generalizability by removing some potential barriers to participation and retention for the lowest income and highest risk African-American girls and families(e.g., ability to travel to a clinical research facility, taking time away from work and school). Therefore, we chose measures that can be feasibly, reliably and validly assessed in home settings, and excluded measures that cannot.
Assessments are performed every six-months over the course of the study to provide enough time points to satisfactorily model changes over time, and long enough intervals between assessments to try to minimize the potential for participant “fatigue” resulting in poor quality participation. A Manual of Procedures includes specific instructions for conducting all assessments, and measurement protocols, training, and data collector certification are standardized with Memphis GEMS for the assessments in common. Data collectors are trained by the investigators, and required to demonstrate high inter-and intra-rater reliability prior to starting data collection. All interview and physical data are entered directly into laptop computers using a database custom-designed for this project, including safeguards against illogical data entry and real-time data checking. A schedule of measures for both Stanford and Memphis GEMS is provided in Table 1.
Table 1.
Schedule of Measures for GEMS
| Baseline | 6-months | 12-months | 18-months | 24-months | |
|---|---|---|---|---|---|
| Physical/Objective Measures | |||||
| Height & Weight (BMI) | X | X | X | X | X |
| Waist Circumference | X | X | X | X | X |
| Triceps Skinfold Thickness | X | X | X | X | X |
| Resting Blood Pressure & Resting Heart Rate | X | X | X | ||
| Fasting Insulin, Glucose & Lipidsa | X | X | |||
| Physical Activity (accelerometery) | X | X | X | ||
| Self-Reported Measures | |||||
| Physical Activity Preferences | X | X | X | ||
| Television, videotape and video game usea | X | X | X | X | X |
| Eating meals with the televisiona | X | X | X | X | X |
| Dietary Intake (24-hour Recalls) | X | X | X | ||
| Activities and Social Context while Eating | X | X | X | ||
| Overconcern with weight and shape | X | X | X | ||
| Body size perception and dissatisfaction | X | X | X | ||
| Depressive Symptomsa | X | X | X | ||
| Global Self-esteem | X | X | X | ||
| School performancea | X | X | X | ||
| Demographics, Socioeconomic Status, Household membership | X | ||||
| Sexual maturation | X | X | X | X | X |
| African-American ethnic/cultural identity | X | X | |||
| Adverse events | X | X | X | X | X |
Stanford GEMS site-specific measures
Primary outcome measure
Body mass index (BMI, defined as the weight in kilograms divided by the square of the height in meters). On the basis of accessibility, reliability, measurement validity and clinical validity, BMI is preferable to other available indirect measures of body fatness in common use.34, 35 Height is measured without shoes with a portable stadiometer (Shorr Productions, Olney, MD). Weight is measured in indoor lightweight clothing without shoes using a direct reading electronic scale (Scaletronix Model 5602, White Plains, NY). Height is measured to the nearest 0.1 cm and weight to the nearest 0.1 kg. Two readings of each are taken, with a third reading taken if the difference between the first two is greater than 0.5 cm for height and 0.3 kg for weight. The mean of the closest two replicates taken is used analytically.
Secondary outcome measures
Waist Circumference measures are made at end-expiration parallel to the floor using the umbilicus as a landmark. Two measures are made to the nearest millimeter using a non-elastic metric tape. A third measure is taken if the difference between the first two is greater than 1.0 cm.
Triceps skinfold thickness is measured three times on the right arm to the nearest 0.1 mm and the mean used for analysis.36
Resting Blood Pressure and Resting Heart Rate are measured according to established protocols37 with an automated blood pressure monitor (Dinamap Pro 100, GE Medical Systems Information Technologies, Inc., Waukesha, Wisconsin). Participants are seated comfortably and quietly for 3 minutes before measurement. Measures are made three times at one-minute intervals on the right arm supported at heart level using an appropriately-sized cuff. The mean of the second and third measures is used.
Fasting Serum Insulin, Glucose, and Lipids are measured from blood samples taken after an overnight fast of at least 8 hours. Whole blood is collected into 10-ml serum separator tubes (BD Vacutainer Systems, Franklin Lakes, NJ). Serum is separated from cells by centrifugation 30 minutes after collection, aliquoted, and placed on ice for delivery to the Stanford University Hospital Clinical Laboratory, a participant in the Centers for Disease Control – NHLBI Lipid Standardization Program, for analysis within 24 hours. All assays have ≤5% intraassay precision and ≤6% interassay precision.
Additional secondary outcomes and potential moderators and/or mediators of intervention effects
Physical Activity is assessed on three consecutive days, including a weekend day, using the Actigraph accelerometer (Manufacturing Technologies Inc., MTI, formerly, Computer Sciences and Applications, CSA). Monitors are secured above the girl’s hip using an elastic belt. Girls are instructed to wear them continuously, except while bathing or swimming. The monitor is programmed to store data at 1-minute epochs. A detailed checking algorithm examines minute-by-minute data to distinguish “noise” from useful data. Published count thresholds from adolescent girls38 are used to estimate minutes of moderate to vigorous physical activity (≥ 3000 counts per minute). Self-report measures are not used in this trial because they were poorly correlated with activity monitoring results with evidence of treatment-related bias in Phase 1.39
Physical Activity Preferences are assessed with a questionnaire developed for prior studies at Stanford (T.N. Robinson, unpublished data) and used in Phase 1 of GEMS.15, 40
Television Viewing, Videotape Viewing, Video Game, and Computer Use are measured with a self-report instrument used in Phase 1 and prior studies of reducing screen media use.15, 29 These measures have proved sensitive to change. Parents report on overall household television viewing.29, 41
Eating Meals with the Television on is reported by children for breakfast and dinner during the past week using items previously validated with direct videotaped observations42 and is sensitive to change.15, 29
Dietary Intake is assessed by 24-hour recalls on three randomly selected nonconsecutive days, including one weekend day and two weekdays, using the Minnesota Nutrition Data System for Research (NDS-R) from the University of Minnesota Nutrition Coordinating Center (NCC). The first recall is collected face-to-face and the second and third by phone. All data collectors are trained in NCC protocols and certified.43 Primary variables of interest are average total daily energy intake and average percent of energy from fat.
Overconcern with Weight and Shape is assessed with the McKnight Risk Factor Survey.44, 45
Body size perception and dissatisfaction is assessed with African-American pre-adolescent female body figure silhouettes ranging from underweight to overweight and the questions, “Which picture looks most like you?” and “Which picture shows the way you would like to look?”45
Depressive symptoms are measured using the 10-item short form of the Children’s Depression Inventory (CDI), designed for use with preadolescents.46
Global Self-Esteem is assessed with the 10-item Rosenberg Self-esteem scale.47, 48
School Performance is self-reported as “most recent school grades” on a 9-point scale ranging from “mostly A’s (9) to mostly F’s (1).15
Additional Potential Moderators and/or Mediators of Intervention Effects
Demographics and Socioeconomic Status
Parents/caregivers report the girl’s race, ethnicity, date of birth, and household membership, and parent/caregiver education levels and total household income.
Sexual Maturation is assessed by self-report using drawings and descriptions of the pubertal stages.49 and age at menarche.
African-American Ethnic/Cultural Identity
Parents/caregivers complete measures of African-American family practices and values, preferences for things African-American, racial segregation, 50 and participation in African-American activities, 51 piloted in Phase 1.52
Participant Safety
Adverse Events are assessed systematically at each data collection visit with two separate queries, one for all injuries and one for all other medical problems requiring a visit to a medical care provider. Serious Adverse Events (SAEs) are specifically monitored.
Clinical Monitoring
As an additional safety feature, girls with a stature or BMI less than the 5th percentile for age on the 2000 CDC national growth references (http://www.cdc.gov/growthcharts/), growing less than 3.5 cm per year in stature, losing more than 10% of their weight per year, with a high fasting blood glucose, total cholesterol, LDL-cholesterol or triglyceride, or low HDL-cholesterol53 and/or high systolic or diastolic blood pressure37 are notified and referred for further evaluation by their primary care medical professional.
Data & Safety Monitoring Board
A six-member, independent Data & Safety Monitoring Board (DSMB) was appointed by NHLBI and meets 1-2 times per year.
Process measures
Intervention implementation is assessed throughout the entire two-year trial using similar measures to Phase 1.15
Methods to Limit Attrition
It is expected to be challenging to retain low socioeconomic status families for the full two years of the study. Specific strategies have been designed to limit attrition. First, participants are not randomized until they complete baseline assessments. Second, families are compensated for their participation in each assessment visit. Third, both the Treatment and Comparison interventions span the entire 2-year study period, and many of the intervention elements are designed to maintain interest and participation. Interventions also include non-monetary incentives such as T-shirts, gym bags, lunch bags, visors, GEMS collecting/trading cards, birthday cards, etc. to reinforce participation. Fourth, all measures are collected in participants’ homes and scheduled at the family’s convenience. Fifth, families intending to move away are not eligible, and we collect friend and/or relative contact information from each family to help find families who move; if within northern California, data collectors travel to their new residences.
Statistical Analysis
The primary objective of the proposed intervention is to reduce weight gain to a degree that has clinical and/or public health and policy significance. Success is judged by comparing changes in the Treatment and Comparison groups over the course of the two-year interventions, using an analytic strategy that takes full advantage of the prospective nature of the data collected. BMI is assessed at baseline and every six months over the duration of the trial (a total of five time points). These multiple BMI measures define individual trajectories of change for each subject, using all available data. Using Random Regression Models (RRM)54 trajectories of change in BMI are regressed on Treatment group assignment, with the baseline value of BMI (centered at its mean) and the Treatment × baseline BMI interaction as covariates. Analyses will follow intention-to-treat principles. RRM allow the use of multiple repeated measures (with associated power benefits as well as conceptual benefits) and have advantages over other repeated measures analysis methods for longitudinal data; they do not require linearity, can accommodate differential lengths of follow-up, irregular measurement intervals and missing data.54, 55 These methods produce valid inferences whether data are missing at random or related to treatment status.54 We use BMI instead of a standardized BMI (e.g., BMI z-score or BMI percentile) because randomization results in a random distribution of BMI relative to age across the two groups, within-subject changes in BMI already account for changes in age, and standardization may introduce error if the normative data are not representative of the study sample.
We include the Treatment × baseline BMI interaction term in our primary analysis of treatment effects because we previously found evidence of greater effects of behavioral interventions among participants with greater BMI at baseline in some prevention studies,29 including the Phase 1 Pilot Study.15 Baseline BMI and a Treatment × baseline BMI interaction term are included as covariates in the analysis of the primary treatment effects to obtain the most valid and unbiased estimate of the main effect of treatment.56-59 To ignore a meaningful interaction in the model could produce a biased estimate of the main effect of treatment, reduce power and attenuate the estimated effect size of treatment.60 If our expectation is wrong, and there is no non-zero Treatment × baseline interaction, then this analysis still results in an unbiased estimate of the main effect of Treatment, and we only lose one degree of freedom. Thus the risks of ignoring a meaningful interaction generally far outweigh the risks of including an unnecessary interaction.
We use a similar analysis approach to examine the effects of the intervention on secondary outcome measures. We follow the methods of Kraemer and colleagues61-63 to examine potential moderators and mediators of Treatment effects. Additional analyses examine hypothesized correlates/risk factors for BMI and secondary outcome measures.
Sample Size and Power
Based on judgment and experience, we estimate a standardized effect size (Cohen’s d) = 0.4 to be a minimum acceptable difference between groups to be considered of clinical or public health significance. Based on the observed Stanford GEMS Phase 1 Pilot Study BMI SD = 5.5 kg/m2 and an estimated 0.90 correlation between baseline and 24-month follow-up BMI, a Cohen’s d = 0.4 is equivalent to a follow-up BMI difference between groups of about 1 kg/m2 (~5 pounds difference for a girl at the CDC 75th percentile for height for age (and about 3 times the BMI difference observed in 12-weeks in the Stanford GEMS Phase 1 Pilot Study). For a two-sided 5% alpha level test, the planned sample size of 130 girls per group provides approximately 90% power to detect intervention effects of that magnitude or greater.64, 65 These sample size estimates do not account for potentially increased power from using serial measures and RRM.66
RESULTS
We recruited and enrolled 100% of our planned analysis sample of 261 families (total sample of 294 girls in 271 families, including 10 girls with BMI > 35 kg/m2) during the period from October 2002 thru February 2004. Only data from the analysis sample are included in this report. Participant recruitment and enrollment flow are displayed in Figure 1. 83 percent of eligible families completed baseline assessments and were randomized, 127 to Group 1 and 134 to Group 2. The two groups are labeled Group 1 and Group 2 throughout this report to maintain blinding until the trial is complete. Demographic characteristics of the study sample are presented in Table 2, and key baseline measures are presented in Table 3.
Figure 1.
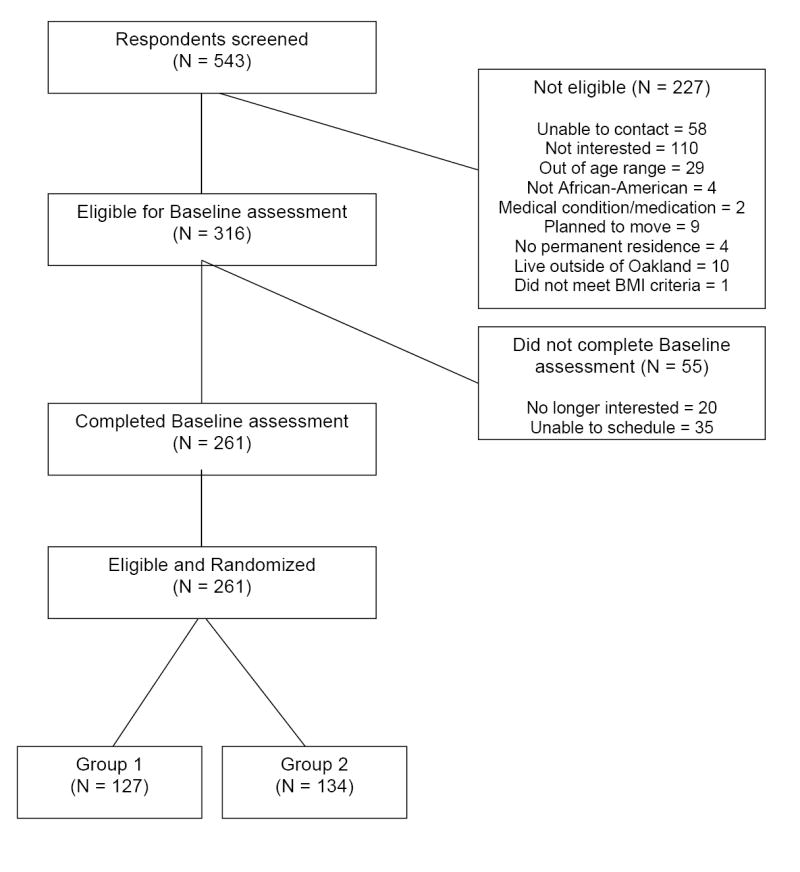
Participant Recruitment and Enrollment Flow Chart.
Table 2.
Baseline demographic characteristics of the Stanford GEMS sample.
| Group 1 | Group 2 | P | All | |
|---|---|---|---|---|
| N | 127 | 134 | 261 | |
| Age in years, mean (sd) | 9.4 (0.8) | 9.5 (0.9) | .34 | 9.4 (0.9) |
| Number of adults living in the household, mean (sd) | 1.9 (0.8) | 1.9 (1.0) | .75 | 1.9 (0.9) |
| Number of children living in the household, mean (sd) | 2.9 (1.4) | 2.9 (1.6) | .54 | 2.9 (1.5) |
| Families who own their own home, n (%) | 32 (25%) | 29 (22%) | .50 | 61(23%) |
| Parent/Caregiver marital status, n (%) | .96 | |||
| Single-Never Married | 58 (46%) | 64 (48%) | 122 (47%) | |
| Divorced/Separated or Widowed | 32 (25%) | 30 (22%) | 62 (23%) | |
| Married | 36 (28%) | 38 (28%) | 74 (28%) | |
| Maximum household education level, n (%) | .38 | |||
| High School graduate or less | 33 (26%) | 38 (28%) | 71 (27%) | |
| Some College/Technical School | 56 (44%) | 66 (49%) | 122 (47%) | |
| College graduate | 38 (30%) | 30 (22%) | 68 (26%) | |
| Annual total household income, n (%) | .71 | |||
| Refusal to respond | 2 (2%) | 2 (1%) | 4 (2%) | |
| Less than $20,000 | 57 (45%) | 50 (37%) | 107 (41%) | |
| $20,000-39,999 | 35 (28%) | 38 (28%) | 73 (28%) | |
| $40,000-$59,999 | 20 (16%) | 28 (21%) | 48 (18%) | |
| $60,000-$79,999 | 5 (4%) | 7 (5%) | 12 (5%) | |
| $80,000 or more | 8 (6%) | 9 (7%) | 17 (7%) |
Table 3.
Baseline measures of the Stanford GEMS sample
| Group 1 | Group 2 | P | All | |
|---|---|---|---|---|
| Height (cm), mean (sd) | 139.3 (9.4) | 139.6 (8.8) | .49 | 139.5 (9.1) |
| Weight (kg), mean (sd) | 40.7 (12.7) | 41.1 (13.5) | .95 | 40.9 (13.1) |
| Body mass index (kg/m2), mean (sd) | 20.7 (4.8) | 20.7 (4.9) | .88 | 20.7 (4.9) |
| Body mass index percentile distributiona, n (%) | .67 | |||
| 0-24th percentile | 10 (8%) | 8 (6%) | 18 (7%) | |
| 25-49th percentile | 13 (10%) | 21 (16%) | 34 (13%) | |
| 50-74th percentile | 23 (18%) | 27 (20%) | 50 (19%) | |
| 75-84th percentile | 13 (10%) | 12 (9%) | 25 (10%) | |
| 85-94th percentile | 25 (20%) | 22 (16%) | 47 (18%) | |
| ≥ 95th percentile | 43 (34%) | 44 (33%) | 87 (33%) | |
| Waist circumference (cm), mean (sd) | 68.8 (12.3) | 69.3 (13.2) | .95 | 69.1 (12.7) |
| Triceps skinfold thickness (mm), mean (sd) | 17.7 (8.1) | 17.2 (8.4) | .50 | 17.5 (8.2) |
| Systolic blood pressure (mmHg), mean (sd) | 98.3 (10.6) | 98.1 (9.3) | .65 | 98.2 (9.9) |
| Diastolic blood pressure (mmHg), mean (sd) | 56.2 (7.1) | 56.0 (6.0) | .94 | 56.1 (6.5) |
| Resting heart rate (beats/min), mean (sd) | 82.5 (9.8) | 79.8 (10.0) | .02 | 81.1 (10.0) |
| Fasting total cholesterol (mg/dL)b , mean (sd) | 175.9 (31.2) | 171.5 (30.5) | .22 | 173.6 (30.8) |
| Fasting HDL cholesterol (mg/dL)b, mean (sd) | 57.0 (13.6) | 54.1 (11.7) | .09 | 55.6 (12.7) |
| Fasting LDL cholesterol (mg/dL)b, mean (sd) | 106.4 (28.4) | 103.9 (26.2) | .33 | 105.1 (27.3) |
| Fasting triglycerides (mg/dL)b, mean (sd) | 61.8 (25.4) | 66.9 (37.1) | .97 | 64.4 (32.0) |
| Fasting glucose (mg/dL)b , mean (sd) | 84.9 (6.6) | 85.0 (7.4) | .99 | 84.9 (7.0) |
| Fasting insulin (uIU/mL)b , mean (sd) | 9.8 (6.9) | 11.0 (11.2) | .69 | 10.4 (9.4) |
| Physical activity (average daily accelerometer counts per minute), mean (sd) | 632.0(184.5) | 662.5(197.9) | .34 | 647.6 (191.8) |
| Minutes per day of moderate-to-vigorous physical activity (average minutes per day of ≥3000 counts per minute), mean (sd) | 29.9 (17.9) | 34.9 (20.5) | .04 | 32.5 (19.4) |
| Screen Media UseWeekly hours of television viewing, mean (sd) | 16.8 (12.4) | 13.1 (10.3) | .02 | 14.9 (11.5) |
| Weekly hours of VCR/DVD viewing, mean (sd) | 4.8 (6.8) | 4.7 (6.4) | .86 | 4.8 (6.6) |
| Weekly hours of video game playing, mean (sd) | 1.0 (3.1) | 1.0 (2.8) | .20 | 1.0 (3.0) |
| Weekly hours of computer use, mean (sd) | 0.8 (2.1) | 0.9 (2.5) | .59 | 0.8 (2.3) |
| Days per week ate breakfast with the TV on,c mean (sd) | 2.2 (2.7) | 1.5 (2.3) | .04 | 1.8 (2.5) |
| Days per week ate dinner with the TV on, mean (sd) | 3.2 (2.9) | 2.7 (2.8) | .12 | 2.9 (2.9) |
| TV in the girl’s bedroom, n (%) | 101 (80%) | 101 (75%) | .42 | 202 (77%) |
| Total household TV use (0-4), mean (sd) | 2.5 (1.2) | 2.5 (1.0) | .98 | 2.5 (1.1) |
| Dietary Intake by 24-hour recallAverage total daily energy intake (kcal), mean (sd) | 1360.1 (432.3) | 1353.7 (460.0) | .97 | 1356.8 (445.9) |
| Average percent of dietary energy from fat, mean (sd) | 35.4 (5.6) | 35.4 (5.3) | .74 | 35.4 (5.5) |
| Overconcern with weight and shape (0-100)d, mean (sd) | 29.2 (27.8) | 29.9 (27.4) | .77 | 29.6 (27.6) |
| Body size dissatisfaction,e mean (sd) | 1.1 (1.8) | 1.2 (1.9) | .38 | 1.2 (1.8) |
| Depressive symptoms (0-20)f, mean (sd) | 2.1 (2.7) | 2.0 (2.7) | .82 | 2.0 (2.7) |
| Global Self-esteem (high=10 – low=40)g, mean (sd) | 19.3 (4.0) | 19.2 (3.9) | .71 | 19.2 (3.9) |
| School performance (9=mostly A’s to 1=mostly F’s)h, mean (sd) | 7.6 (1.5) | 7.7 (1.3) | .67 | 7.6 (1.4) |
| Self-assessed breast maturation, n (%) | .37 | |||
| Refused | 1 (1%) | 2 (1%) | 3 (1%) | |
| Stage 1 | 39 (31%) | 43 (32%) | 82 (31%) | |
| Stage 2 | 43 (34%) | 43 (32%) | 86 (33%) | |
| Stage 3 | 41 (32%) | 37 (28%) | 78 (30%) | |
| Stage 4 | 3 (2%) | 6 (4%) | 9 (3%) | |
| Stage 5 | . | 3 (2%) | 3 (1%) | |
| Self-assessed pubic hair maturation, n (%) | .88 | |||
| Refused | . | 2 (1%) | 2 (1%) | |
| Stage 1 | 52 (41%) | 59 (44%) | 111 (43%) | |
| Stage 2 | 39 (31%) | 41 (31%) | 80 (31%) | |
| Stage 3 | 22 (17%) | 18 (13%) | 40 (15%) | |
| Stage 4 | 13 (10% | 12 (9%) | 25 (10%) | |
| Stage 5 | 1 (1%) | 2 (1%) | 3 (1%) | |
| Entered puberty (stage 2 or greater for breast and/or pubic hair), n (%) | 100 (79%) | 101 (75%) | .67 | 201 (77%) |
| Achieved menarche, n (%) | 4 (3%) | 4 (3%) | .94 | 8 (3%) |
| Preferences for things African-American (1-7), mean (sd) | 4.2 (1.4) | 4.1 (1.3) | .45 | 4.2 (1.4) |
| African-American family practices and values (1-7), mean (sd) | 5.6 (1.3) | 5.6 (1.3) | .64 | 5.6 (1.3) |
| Racial segregation (1-7), mean (sd) | 4.7 (1.7) | 4.7 (1.6) | .77 | 4.7 (1.7) |
| African-American ethnic identity (1-7), mean (sd) | 4.7 (1.5) | 4.7 (1.4) | .59 | 4.7 (1.4) |
Percentiles based on 2000 CDC BMI charts (http://www.cdc.gov/growthcharts/)
n for blood measures = 101 for Group 1, 107 for Group 2, 208 for All.
1 Group 1 girl did not respond
1 Group 1 girl and 5 Group 2 girls did not respond
1 Group 1 girl and 1 Group 2 girl did not respond
8 Group 1 girls and 7 Group 2 girls did not complete the measure
3 Group 1 girls and 4 Group 2 girls did not complete the measure
1 Group 2 girl did not respond
The results demonstrate success enrolling low socioeconomic status participants with nearly complete data. Baseline fasting blood results were acquired from 80% of the analysis sample. Statistical significance of group contrasts are made with non-parametric Wilcoxon Rank Sum tests for scaled variables and Chi-Square tests for categorical variables, with a two-sided alpha = .05. Girls in Group 1 had a statistically significantly greater average resting heart rate, fewer average daily minutes of accelerometer counts ≥3000, and greater reported hours per week of television viewing, compared to girls in Group 2. There were no other significant differences between the two groups.
The sample also is at high risk for obesity and obesity-related risk factors. Girls’ weights averaged the 75th percentile, heights averaged the 67th percentile and BMIs averaged the 74th percentile on the sex-and age-specific 2000 CDC growth references. More than half the analysis sample had a baseline BMI ≥ the 85th percentile for their age and sex, and a third have a BMI ≥ the 95th percentile, even after excluding girls with BMI > 35 kg/m2 from the analysis sample.
At baseline, the clinical monitoring procedures identified 6 girls (2%) in the analysis sample with BMI less than the 5th percentile, 5 (2%) with height less than the 5th percentile on the 2000 CDC growth references. Five girls (2%) had systolic blood pressure ≥95th percentile for age, sex and height but no girls had diastolic blood pressure ≥95th percentile. Of the 208 girls with fasting blood tests, 41 (20%) had total cholesterol ≥200 mg/dL or greater and 71 (34%) had total cholesterol of 177-199 mg/dL. Thirty-eight girls (18%) had an LDL-cholesterol ≥130 mg/dL, and 46 girls had an LDL-cholesterol of 110-129 mg/dL. Only 5 girls (2%) had an HDL-cholesterol less than 35 mg/dL and 10 (5%) had triglycerides ≥135 mg/dL. One girl had a fasting glucose >110 mg/dL but none ≥126 mg/dL.
DISCUSSION
Stanford GEMS is a 2-arm parallel group, randomized controlled trial to test the efficacy of a theory-based, culturally-tailored after school dance program and a home/family-based intervention to reduce television, videotape and video game use to reduce body mass index gain over 2 years, among lower socioeconomic status African-American pre-adolescent girls. Study design and implementation plans have benefited from extensive formative research and a 12-week randomized controlled pilot trial during Phase 1, including sharing knowledge and experience among four different field centers, a coordinating center and the NHLBI project office. The design and rationale for this study, and our experiences in recruitment and enrollment, therefore serve to summarize the lessons learned to assist others in the design of future studies. For the Phase 2 full-scale trial, Stanford GEMS benefits from ongoing collaboration with the Memphis GEMS trial investigators and the NHLBI project office.
To enroll lower socioeconomic status families in Oakland, CA, we used available elementary school data to identify neighborhoods for recruitment, and performed all assessments in participants’ homes, avoiding the barrier of requiring families to come to a clinical research center. These methods resulted in the successful recruitment and enrollment/randomization of 261 families over 17 months, with a high yield of eligible families completing baseline assessments and randomization (83%). Demographic characteristics of the resulting study sample demonstrate success in enrolling a sample with low household incomes, low maximum household education levels, and a large proportion of single parents/caregivers. Despite the multiple strategies we used to reduce barriers to enrollment and to have as few eligibility criteria as possible, our sample is still composed of volunteers and, as with all studies, this may limit the generalizability of the results.
By scheduling early morning visits at girls’ homes, fasting blood samples were successfully collected from 80% of the analysis sample. This demonstrates the feasibility of acquiring blood measures from low-income samples of African-American children if strategies are thoughtfully designed and tested to be culturally sensitive and acceptable. Consistent with the otherwise high risk status of the sample, fasting total cholesterol and LDL-cholesterol measures both averaged above National Cholesterol Education Program cut-offs for borderline high classifications.53
Accelerometer measurements found that girls averaged a total of only slightly more than one half-hour per day of moderate to vigorous physical activity. In contrast, they reported an average of more than 3 hours per day of screen media use, mostly television and VCR/DVDs with only small amounts of average video game playing and computer use, and nearly 4 out of 5 girls reported having a television in her bedroom, exceeding the national average for girls this age.67 Girls were eating a relatively high fat diet, averaging more than 35% of their daily energy from fat. These baseline results suggest there is significant room for improvement in response to effective obesity prevention interventions, even among a relatively unselected, community-based sample of low-income African-American girls.
Randomization successfully produced comparable experimental groups, with only a few statistically significant differences at baseline, about as many as one would expect by chance. The absolute differences for these measures were small, however, and they should not threaten the internal validity of the study. These variables will be given special attention in secondary analyses.
The Treatment intervention applies Bandura’s social cognitive model 22, 23 to a community-based setting with low-income, urban African-American girls and their families. This foundation in theory and prior experience in Phase 1 allowed the development of protocols intended to maximize motivation and self-efficacy for each girl’s participation in the intervention activities for the full two years of the study. Phase 1 provided an important opportunity to pre-test most elements of the proposed interventions, including specific cultural tailoring for participants living in the focus neighborhoods in Oakland.15 It is unknown, however, what new challenges will be faced in maintaining participation in the interventions for an entire two-year period. Emphasizing applied theoretical principles combined with involving the community in implementation is an anticipated strength of the intervention, and is intended to maximize long-term participation and potential generalizability to other similar communities. Our active-placebo comparison intervention is not matched on attention but it is intended to allow comparison with what we would consider a state-of-the-art version of usual practice (health and nutrition education) and to reduce potential threats to internal validity that might be introduced by less attractive or acceptable comparison groups.33
It is expected to be a challenge to retain such low socioeconomic status families for the full two years of the study. A number of specific strategies have been designed to limit attrition and this is one of the highest priorities of the trial. Measures were selected for their reliability and validity as well as their feasibility for home-based assessments. Phase 1 provided the opportunity to test many of the measures and to be more selective in Phase 2.
The analysis plan uses random regression models to estimate individual changes over the two-year study period, and derives the greatest benefit from the multiple serial measures. It also offers potential advantages for accommodating irregular measurement intervals, differential lengths of follow-up and missing data, problems that may be more common when following a socioeconomically-stressed sample. The study design will allow us to compare the effects of the two-year interventions. Without first knowing the 2-year efficacy of the Treatment intervention, no post-intervention long-term follow-up is yet planned.
Stanford GEMS is powered to detect what we consider a clinically meaningful average difference between groups, about 1 kg/m2 in BMI. As a community-based primary prevention trial, the intervention is designed to act along the entire distribution of BMI in the population, though not necessarily equally at all points. Our expectation is for greater quantitative effects among girls who are starting at the upper end of the BMI distribution. The baseline data show that a large proportion of this community-based sample can be considered at risk, occupying the upper parts of the 2000 CDC reference distribution. The population-based primary prevention approach is considered to be particularly suited for a widespread problem like obesity and for obesity prevention in children.9, 68 A population-wide prevention approach also is expected to produce the greatest effects on population morbidity and mortality.69, 70
Very few past diet and physical activity interventions have succeeded in reducing body fat and weight gain.7, 10 There have also been few studies that have tested obesity prevention interventions specifically designed to meet the needs of pre-adolescent African-American girls and their families, despite their increased rates of obesity and associated morbidities. Stanford GEMS was designed with particular attention to applying theory and experience to help address the paucity of research in this area. Designed according to a “solution-oriented” research paradigm,71 Stanford GEMS combines community-involvement to produce maximum generalizability with a rigorous randomized controlled design and implementation methods to maintain high internal validity. As a result, it may have a greater chance to directly inform public health practice and policy, as well as prevention science.
Acknowledgments
We thank the Stanford GEMS participants and their families, our Stanford GEMS field staff, the many community members and community centers that make this study possible. We also thank the Memphis GEMS investigators and the GEMS Data and Safety Monitoring Board for their valuable input and collaboration.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Update: prevalence of overweight among children, adolescents, and adults-United States, 1988-1994. MMWR. 1997;46:199–202. [PubMed] [Google Scholar]
- 2.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286(10):1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 3.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 4.Hedley A, Ogden CL, Johnson CL, Carrol MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among U.S. Children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 5.Winkleby MA, Robinson TN, Sundquist J, Kraemer HC. Ethnic variation in cardiovascular disease risk factors among children and young adults: Findings from the Third National Health and Nutrition Examination Survey, 1988-1994. JAMA. 1999;281(11):1006–1013. doi: 10.1001/jama.281.11.1006. [DOI] [PubMed] [Google Scholar]
- 6.Dietz WH, Robinson TN. Overweight Children and Adolescents. New England Journal of Medicine. 2005;352:2100–2109. doi: 10.1056/NEJMcp043052. [DOI] [PubMed] [Google Scholar]
- 7.Resnicow K, Robinson TN. School-based cardiovascular disease prevention studies: review and synthesis. Annals of Epidemiology. 1997;S7:S14–S31. [Google Scholar]
- 8.Robinson TN, Killen JD. Obesity prevention for children and adolescents. In: Thompson JK, Smolak L, editors. Body Image, Eating Disorders, and Obesity in Children and Adolescents: Assessment, Prevention, and Treatment. Washington, DC: American Psychological Association; 2001. pp. 261–292. [Google Scholar]
- 9.Robinson TN. Population-based obesity prevention for children and adolescents. In: Johnston FE, Foster GD, editors. Obesity, Growth and Development. Vol. 3. London, UK: Smith-Gordon and Company Limited; 2001. pp. 129–141. [Google Scholar]
- 10.Summerbell C, Waters E, Edmunds L, Kelly S, Brown T, Campbell K. Interventions forpreventing obesity in children. The Cochrane Database of Systematic Reviews. 2005;3 doi: 10.1002/14651858.CD001871.pub2. Art No.: CD001871.pub001872. DOI: 001810.001002/14651858.pub14651852. [DOI] [PubMed] [Google Scholar]
- 11.Obarzanek E, Pratt C. Girls health Enrichment Multi-site Studies (GEMS): new approaches to obesity prevention among young African-American girls. Ethnicity and Disease. 2003;13(suppl 1):S1–S5. [PubMed] [Google Scholar]
- 12.Baranowski T, Baranowski JC, Cullen KW, et al. The Fun, Food and Fitness Project (FFFP): The Baylor GEMS pilot study. Ethnicity and Disease. 2003;13(suppl 1):S30–S39. [PubMed] [Google Scholar]
- 13.Beech BM, Klesges RC, Kumanyika SK, et al. Child- and parent-targeted interventions:The Memphis GEMS pilot study. Ethnicity and Disease. 2003;13(suppl 1):S40–S53. [PubMed] [Google Scholar]
- 14.Story M, Sherwood NE, Himes JH, et al. An after-school obesity prevention program for African-American girls: the Minnesota GEMS pilot study. Ethnicity and Disease. 2003;13(suppl 1):S54–S64. [PubMed] [Google Scholar]
- 15.Robinson TN, Killen JD, Kraemer HC, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: The Stanford GEMS pilot study. Ethnicity and Disease. 2003;13(S1):s65–s77. [PubMed] [Google Scholar]
- 16.Kumanyika S, Obarzanek E, Robinson TN, Beech BM. Phase 1 of the Girls health Enrichment Multi-Site Studies (GEMS): Conclusion. Ethnicity and Disease. 2003;13:S1-88–S81-99. [PubMed] [Google Scholar]
- 17.Kraemer HC, Robinson TN. Are certain multicenter randomized clinical trial structures misleading clinical and policy decisions? Controlled Clinical Trials. 2005;26:518–529. doi: 10.1016/j.cct.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 18.Story M, Sherwood NE, Obarzanek E, et al. Recruitment of African-American preadolescent girls in an obesity prevention trial: The GEMS pilot studies. Ethnicity and Disease. 2003;13(Suppl 1):S88–S91. [PubMed] [Google Scholar]
- 19.NIH Expert Panel on the Identification Evaluation and Treatment of Overweight and Obesity in Adults. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Publication no. 98-4083. Bethesda, MD: Obesity Education Initiative, National Heart, Lung, and Blood Institute, National Institutes of Health; 1998. [Google Scholar]
- 20.Efron B. Forcing a sequential experiment to be balanced. Biometrika. 1971;58:403–417. [Google Scholar]
- 21.Kumanyika S, Story M, Beech BM, et al. Collaborative planning process for formative assessment and cultural appropriateness in the Girls health Enrichment Multi-site Studies (GEMS): a retrospection. Ethnicity and Disease. 2003;13(Suppl 1):S15–S29. [PubMed] [Google Scholar]
- 22.Bandura A. Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 23.Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H; Freeman and Company: 1997. [Google Scholar]
- 24.Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural sensitivity in public health: defined and demystified. Ethnicity and Disease. 1999;9(1):10–21. [PubMed] [Google Scholar]
- 25.Anderson LP. Acculturative stress: a theory of relevance to black Americans. Clin Psychol Rev. 1991;11:685–702. [Google Scholar]
- 26.Gaines SO, Marelich WD, Bledsoe KL, et al. Links between race/ethnicity and cultural values as mediated by race/ethnicity identity and moderated by gender. JPers Soc Psychol. 1997;72:1460–1476. doi: 10.1037//0022-3514.72.6.1460. [DOI] [PubMed] [Google Scholar]
- 27.Harrison AO, Wilson MN, Pine CJ, Chan SQ, Buriel R. Family ecologies of ethnic minority children. Child Dev. 1990;61:347–362. [Google Scholar]
- 28.Resnicow K, Braithwaite RL, Kuo J. Interpersonal interventions for minority adolescents. In: Wilson DK, Rodrigue JR, Taylor WC, editors. Health Promoting and Health Compromising Behaviors Among Minority Adolescents. Washington, DC: American Psychological Association; 1997. [Google Scholar]
- 29.Robinson TN. Reducing children’s television viewing to prevent obesity. JAMA. 1999;282:1561–1567. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- 30.Ford BS, McDonald TE, Owens AS, Robinson TN. Primary care interventions to reduce television viewing in African-American children. American Journal of Preventive Medicine. 2002;22(2):106–109. doi: 10.1016/s0749-3797(01)00410-x. [DOI] [PubMed] [Google Scholar]
- 31.Kazdin AE, Wicoxon LA. Systematic desensitization and non-specific treatment effects: a methodological evaluation. Psychol Bull. 1976;83:729–758. [PubMed] [Google Scholar]
- 32.Shapiro AK, Morris LA. The placebo effect in medical and psychological therapies. In: Garfield SL, Bergin AE, editors. Handbook of Psychotherapy and Behavior Change. New York: John Wiley & Sons; 1978. pp. 369–410. [Google Scholar]
- 33.Cook TD, Campbell DT. Quasi-Experimentation. Design & Analysis Issues for Field Settings. Boston: Houghton Mifflin Company; 1979. [Google Scholar]
- 34.Dietz WH, Robinson TN. Use of the body mass index (BMI) as a measure of overweight in children and adolescents. J Pediatr. 1998;132:191–193. doi: 10.1016/s0022-3476(98)70426-3. [DOI] [PubMed] [Google Scholar]
- 35.Kraemer HC, Berkowitz RI, Hammer LD. Methodological difficulties in studies of obesity. I. measurement issues. Ann Behav Med. 1990;12:112–118. [Google Scholar]
- 36.Lohman TG, Roche AF, Martorell R. Anthropometric Standardization Reference Manual. Champaign, IL: Human Kinetics Publishers; 1988. [Google Scholar]
- 37.National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. Update on the Task Force Report (1987) on High Blood Pressure in Children and Adolescents: A Working Group Report from the National High Blood Pressure Education Program. NIH Publication No. 96-3790. Bethesda, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 1996. [Google Scholar]
- 38.Treuth MS, Schmitz K, Catellier DJ, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Medicine and Science in Sports and Exercise. 2004;36:1259–1266. [PMC free article] [PubMed] [Google Scholar]
- 39.Treuth MS, Sherwood NE, Baranowski T, et al. Physical activity self-report and accelerometry measures from the Girls health Enrichment Multi-site Studies. Preventive Medicine. 2003;38:s43–s49. doi: 10.1016/j.ypmed.2003.01.001. [DOI] [PubMed] [Google Scholar]
- 40.Sherwood NE, Taylor WC, Treuth M, et al. Measurement characteristics of activity-related psychosocial measures in 8-10-year-old African-American girls in the Girls health Enrichment Multisite Study (GEMS) Preventive Medicine. 2004;38:s60–s68. doi: 10.1016/j.ypmed.2003.12.030. [DOI] [PubMed] [Google Scholar]
- 41.Medrich EA. Constant television: A background to daily life. J Communication. 1979;29:171–176. [Google Scholar]
- 42.Borzekowski DLG, Robinson TN. Viewing the viewers: 10 video case studies of children’s television viewing behaviors. J Broadcasting Electronic Media. 1999;43:506–528. [Google Scholar]
- 43.Cullen KW, Watson M, Himes JH, et al. Evaluation and quality control procedures for 24-hour dietary recalls: results from the Girls health Enrichment Multisite Studies. Preventive Medicine. 2004;38:s14–s23. doi: 10.1016/j.ypmed.2003.10.014. [DOI] [PubMed] [Google Scholar]
- 44.Shisslak CM, Rneger R, Sharpe T, et al. Development and evaluation of the McKnight Risk Factor Survey for assessing potential risk factors for disordered eating in preadolescent girls. International Journal of Eating Disorders. 1999;25:195–214. doi: 10.1002/(sici)1098-108x(199903)25:2<195::aid-eat9>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 45.Sherwood NE, Beech BM, Klesges LM, et al. Measurement characteristics of weight concern and dieting measures in 8-10 year old African American girls in the Girl’s health Enrichment Multisite Studies (GEMS) Preventive Medicine. 2004;38(Suppl 1):50–59. doi: 10.1016/j.ypmed.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 46.Kovacs M. The Children’s Depression Inventory (CDI) Manual. Toronto, Ontario: Multi-Health Systems, Inc; 1992. [Google Scholar]
- 47.Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- 48.Rosenberg M. Conceiving the Self. New York: Basic Books; 1979. [Google Scholar]
- 49.Morris NM, Udry JR. Validation of a self-administered instrument to assess stage of adolescent development. J Youth Adolesc. 1980;9:271–280. doi: 10.1007/BF02088471. [DOI] [PubMed] [Google Scholar]
- 50.Klonoff EA, Landrine H. Revising and improving the African American acculturation scale. J Black Psychol. 2000;26:235–261. [Google Scholar]
- 51.Phinney JS. The multigroup ethnic identity measure: a new scale for use with diverse groups. J Adolesc Res. 1992;7:156–176. [Google Scholar]
- 52.Beech BM, Kumanyika SK, Baranowski T, et al. Parental cultural perspectives in relation to weight-related behaviors and concerns of African-American girls. Obesity Research. 2003;12:7S–19S. doi: 10.1038/oby.2004.264. [DOI] [PubMed] [Google Scholar]
- 53.National Cholesterol Education Program. Report of the Expert Panel on Blood Cholesterol Levels in Children and Adolescents. NIH Publication No. 91-2732. Bethesda, MD: U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Heart, Lung, and Blood Institute; 1991. [Google Scholar]
- 54.Gibbons RD, Hedeker D, Elkin I, et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- 55.Hedeker D, Rose JS. The natural history of smoking: A pattern-mixture random-effects regression model. In: Rose JS, Chassin L, Presson CC, editors. Multivariate Applications in Substance Use Research: New Methods for New Questions. Mahweh, NJ: Lawrence Erlbaum Associates; 2000. pp. 79–112. [Google Scholar]
- 56.Cronbach LJ, Snow RE. Aptitudes and Instructional Methods: A Handbook for Research on Interactions. New York: Irvington; 1977. [Google Scholar]
- 57.Finney JW, Mitchell RE. Methodological issues in estimating main and interactive effects. Journal of Health and Social Behavior. 1984;25:85–98. [PubMed] [Google Scholar]
- 58.Overall JE, Lee DM, Hornick CW. Comparisons of two strategies for analysis of variance in nonorthogonal designs. Psychological Bulletin. 1981;90:367–375. [Google Scholar]
- 59.Rogosa D. Comparing nonparallel regression lines. Psychological Bulletin. 1980;88:307–321. [Google Scholar]
- 60.Kraemer HC, Blasey CM. Centring in regression analyses: a strategy to prevent errors in statistical inference. International Journal of Methods in Psychiatric Research. 2004;13:141–151. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kraemer HC, Frank E, Kupfer DJ. Moderators of treatment outcomes: clinical, research, and policy importance. JAMA. 2006;296:1286–1289. doi: 10.1001/jama.296.10.1286. [DOI] [PubMed] [Google Scholar]
- 62.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 63.Kraemer HC, Stice E, Kazdin A, Offord D, Kupfer D. How do risk factors work together? Mediators, moderators, and independent, overlapping, and proxy risk factors. American Journal of Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 64.Cohen J. Statistical Power Analysis for the Behavioral Sciences. Second. Hillsdale, NJ: Lawrence Erlbaum Associated, Publishers; 1988. [Google Scholar]
- 65.Kraemer HC, Thiemann S. How many subjects? Statistical Power Analysis in Research. Newberry Park, CA: Sage Publications; 1987. [Google Scholar]
- 66.Kraemer HC. To increase power in randomized clinical trials without increasing sample size. Psychopharmacol Bull. 1991;27:217–224. [PubMed] [Google Scholar]
- 67.Roberts DF, Foehr UG, Rideout VJ, Brodie M. Kids and Media in America. Cambridge, UK: Cambridge University Press; 2003. [Google Scholar]
- 68.Institute of Medicine Committee on Prevention of Obesity in Children and Youth. Preventing Childhood Obesity: Health in the Balance. Washington, DC: The National Academies Press; 2005. [PubMed] [Google Scholar]
- 69.Rose G. Strategy of prevention: lessons from cardiovascular disease. Br Med J. 1981;282:1847–1851. doi: 10.1136/bmj.282.6279.1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rose G. Strategies of prevention: the individual and the population. In: Marmot M, Elliott P, editors. Coronary Heart Disease Epidemiology: From Aetiology to Public Health. Oxford: Oxford University Press; 1992. [Google Scholar]
- 71.Robinson TN, Sirard JR. Preventing childhood obesity: A solution-oriented research paradigm. American Journal of Preventive Medicine. 2005;28:194–201. doi: 10.1016/j.amepre.2004.10.030. [DOI] [PubMed] [Google Scholar]


