Abstract
Although targeted inhibition of BCR-ABL with imatinib is an effective therapy for patients with chronic myeloid leukemia (CML), a minority of patients acquire mutations in the BCR-ABL kinase domain, resulting in imatinib resistance. The spectrum of kinase domain mutations discovered to date is quite heterogeneous, consisting almost exclusively of single nucleotide substitutions affecting key amino acids that regulate drug binding or BCR-ABL function. Here, we describe an alternative kinase domain insertion/truncation mutation in three CML patients undergoing kinase inhibitor therapy. In each of these patients, direct DNA sequencing of BCR-ABL RT-PCR products revealed that the same 35 nucleotides from ABL intron 8 had been inserted at the normal exon 8 to 9 splice junction. This 35-bp intronic sequence was flanked by excellent consensus splice donor and acceptor sequences, suggesting alternative splicing as the likely mutational mechanism. The insertion created a premature translational stop codon after 10 intron-encoded amino acids (amino acid 484). This resulted in truncation of 653 C-terminal amino acids, which included part of the kinase domain and the entire “last exon” region. These findings demonstrate that kinase domain insertions are an alternative (and not entirely uncommon) mutational mechanism in CML patients undergoing kinase inhibitor therapy.
Imatinib is the recommended first line therapy for patients with chronic myeloid leukemia (CML) [National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology: Chronic Myelogenous Leukemia. Version 1.2008; last accessed 07/02/07; available at http://www.nccn.org/professionals/physician_gls/PDF/cml.pdf; to view the most recent and complete version of the guideline, go online to http://www.nccn.org.]. While on imatinib therapy, more than 80% of patients will achieve a complete cytogenetic response (CCR).1,2 After CCR is achieved, molecular response, measured by RT-PCR quantification of BCR-ABL transcripts, is typically used to continue therapeutic monitoring and detect loss of response at an early stage, before overt relapse occurs. On standard imatinib therapy, most CCR patients will have residual disease detectable by RT-PCR quantification of BCR-ABL transcripts.3,4 The most common mechanism for a subsequent loss of response is acquired imatinib resistance due to the development of point mutations in the BCR-ABL kinase domain that interfere with optimal drug-target interactions.5 DNA sequencing of the BCR-ABL kinase domain can determine the presence or absence of such mutations, and since most of these variants are susceptible to alternative kinase inhibitors (dasatinib and/or nilotinib), alternative therapy can be initiated.6,7 Kinase domain mutations have been detected in the majority of patients with acquired imatinib resistance,8 and over 40 different mutations have been reported.9 Almost all of these mutations are single nucleotide point mutations, with insertions and deletions being rare in previous reports. In comparison, we now report three cases with an identical insertion/truncation mutation in which sequences from ABL intron 8 are aberrantly encoded into the truncated C terminus of the BCR-ABL kinase domain.
Cases
The first case was that of a 15-year-old adolescent initially diagnosed with a leukocyte count of 266,000 (with 4% blasts) and 100% Philadelphia (Ph) chromosome [t(9;22)]-positive metaphases in his bone marrow. The patient began imatinib therapy at a dose of 400 mg per day and rapidly achieved a complete hematological remission, followed by a CCR at 11 months, but with only a 1.3-log reduction in BCR-ABL RNA. After failing to achieve any improvement in his molecular response (1.3-log drop) after 14 months on imatinib (including a dose escalation to 800 mg), he was referred to our institution, where a 17-month sample revealed a significant molecular response (2.8-log drop), but also showed a novel insertion/truncation mutation in the C terminus of the BCR-ABL kinase domain. A 20-month follow-up sample showed a slight (or negligible) increase in disease burden (2.5-log drop), but confirmed a continuing good therapeutic response.
The second case was a 60-year-old man initially diagnosed with a leukocyte count of over 200,000 and 100% Ph+ metaphases in his bone marrow. After six months of imatinib therapy (at 800 mg per day), he achieved a CCR and a 1.9-log reduction in BCR-ABL transcripts. After nine months, his molecular response improved to a 2.4-log drop. However, due to gastrointestinal side effects on the high imatinib dose, transient dose reductions to 400 or 600 mg were necessary. After one year of imatinib treatment, despite normal peripheral blood counts, normal bone marrow morphology, and continued CCR (with normal karyotype), his BCR-ABL RNA level increased to a 1.9-log drop. Because of this 0.5-log rise in BCR-ABL RNA, and the associated higher risk of early, evolving imatinib resistance,10,11 mutation analysis of the BCR-ABL kinase domain was requested and showed the intron 8 insertion/truncation. Despite continued high-dose imatinib treatment, a 14-month sample showed a slight (if any) increase in BCR-ABL transcripts (1.7-log drop), thus confirming a suboptimal molecular response.
The third case was that of a 50-year-old male diagnosed with a leukocyte count of 233,000, a platelet count of 733,000, and 100% Ph+ bone marrow metaphases. After imatinib therapy was initiated, he quickly achieved a hematological remission, but failed to attain an adequate cytogenetic response. After nine months of imatinib (at increasing doses), he relapsed with 100% Ph-positive bone marrow cells. Although BCR-ABL mutation analysis at that time failed to show any detectable kinase domain mutations, he was switched from imatinib to dasatinib. After nine additional months of dasatinib therapy (with an escalating dose), he finally achieved a major cytogenetic response (20% Ph-positive metaphases), but 3 months later, the cytogenetic response was not improved (25% Ph positivity; 0.7-log reduction in bcr-abl transcripts), and he was referred to our institution for a second opinion. When first seen at our institution (after 13 months of dasatinib), although his cytogenetic and molecular responses were essentially unchanged (25% Ph positivity and a 0.5-log drop in bcr-abl RNA), a new clonal cytogenetic alteration was detectable (trisomy 8 with an extra Y chromosome), suggesting possible disease progression. A bone marrow sample then sent to our laboratory for BCR-ABL kinase domain mutation analysis showed the intron 8 insertion/truncation mutation.
Materials and Methods
Therapeutic response monitoring by cytogenetics and BCR-ABL quantitative RT-PCR were performed as previously described.3 For screening the BCR-ABL kinase domain for mutations, 10 μl of RNA, extracted as previously described from 600,000 leukocytes,3 was reverse transcribed into cDNA (20-μl reaction volume) with SuperScript II (Invitrogen, Carlsbad, CA). BCR-ABL amplicons for direct DNA sequencing (1579 bp for b3a2, 1504 bp for b2a2) were then generated with forward primer BCRF and reverse primer ABLKinaseR as previously described.12 PCR products were run on a 1% agarose gel to confirm amplification and estimate amplicon quantity. Amplicons were purified using the UltraClean PCR Clean-up Kit (MO BIO Laboratories, Carlsbad, CA), and ∼80 ng of DNA was used for sequencing with the BigDye Terminator v1.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA). Five primers were used for sequencing: 2F (5′-CGCAACAAGCCCACTGTCT-3′), 1R (5′-CCACTTCGTCTGAGATACTGGAT-3′), MF (5′-ATCCACAGAGATCTTGCTGCC-3′), MR (5′-CCCCTACCAGGCAGTTTCG-3′), and HeinR (5′-AGAACTTGTTGTAGGCCA-3′). The amplicons and sequencing primers were thermocycled for 24 cycles at 96°C for 10 seconds, 50°C for 5 seconds, and 60°C for 4 minutes. Sequencing was carried out on an ABI 3100 capillary electrophoresis instrument using a 50 cm array, and results were analyzed using SeqScape software (Applied Biosystems). Our five sequencing primers encompass the entire BCR-ABL kinase domain (amino acids 234 to 496 of GenBank NM_005157) with redundant coverage.
Results and Discussion
Analysis of the BCR-ABL kinase domain cDNA sequence from all three patients revealed a 35-bp insertion mutation precisely at the exon 8 to 9 splice junction [after nucleotide 1423 (amino acid 475) of GenBank cDNA clone NM_005157]. The identical 35-bp insertion was evident on sequences obtained (in duplicate) using both forward (MF) and reverse (1R) sequencing primers (Figure 1). In all three cases, the mutation was co-expressed with wild-type BCR-ABL sequence, as a minority species compared to a predominating wild-type signal in patients 2 and 3, and as an approximate 50–50 mixture in patient 1. The ABL sequence in these three cases is not derived from the untranslocated chromosome 9 c-Abl gene, since the template for DNA sequencing was an RT-PCR product generated with a forward BCR primer together with a reverse ABL primer.
Figure 1.
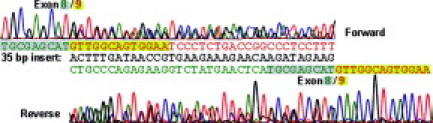
DNA sequencing traces of the 35-bp insertion mutation. Shown are sequencing electropherogram tracings from our first patient with a 35-bp insertion mutation (black text) at the junction between exon 8 sequences (green text) and exon 9 sequences (red text). For the forward primer tracing, the colors of the nuclotide peaks are T = red, A = green, G = black, and C = blue. The reverse primer tracing has been inverted so that the 5′ to 3′ extension of sequential nucleotides reads right to left, and the nucleotide peak colors are switched to their reverse complement so that A = red, T = green, C = black, and G = blue. The same nine nucleotides at the 3′ end of exon 8 (highlighted gray) and 13 nucleotides at the 5′ end of exon 9 (highlighted green) are included in both the forward and reverse tracings.
A BLAST (National Center for Biotechnology Information, Bethesda, MD) search of the inserted nucleotides revealed 100% identity with an ABL1 genomic DNA sequence, within intron 8 (GenBank accession number NC_000009, nucleotides 132,744,926 to 132,744,960), 1151 bp downstream from the normal splice donor site at the end of exon 8 (Figure 2). The mutational mechanism for this insertion is probably an aberrant RNA splicing event, since the inserted 35 nucleotides are flanked, at both ends, by sequences homologous to consensus splice acceptor and donor sequences. In particular, the CTTCAG sequence immediately upstream of the insert is a perfect match to the YYNCAG consensus splice acceptor sequence (with Y = C or T). In addition, the GTGAGC sequence immediately downstream of the insert has only a single nucleotide mismatch compared to the ideal GTRAGT consensus splice donor sequence (with R = G or A). The consensus splice donor and acceptor sequences are from Baralle et al.13 We found no nucleotide substitutions in the expressed BCR-ABL RNA, either in the exons or in the intron 8-derived insertion. The presence of other intronic sequence alterations that may affect the specificity or efficiency of splicing cannot, of course, be determined from the available RNA samples. Other alternatively spliced BCR-ABL transcript variants have recently been described as a minority species in most newly diagnosed CML patients,14 suggesting that mis-splicing may be a more common phenomenon in CML than has been previously appreciated.
Figure 2.

ABL1 genomic sequence showing the 35-bp intronic insertion. Exon 8 of the ABL1 gene is depicted in bold, capitalized text (nucleotides 1271 to 1423 of GenBank cDNA clone NM_005157). The first nucleotide of this exon is nucleotide 132743623 of the human chromosome 9 reference assembly sequence (GenBank NC_000009). Introns are denoted in lower case text, and exon 9 is depicted in bold, capitalized text (nucleotides 132745276 to 132745365 of GenBank NC_000009). The 35 bp of intron 8 that are inserted into the variant BCR-ABL transcript are depicted as bold, underlined text. Consensus splice donor and acceptor sequences flanking this 35-bp insert are also depicted (boxed text). Each row of sequence contains 50 nucleotides.
Translation of the insertion mutant would produce a BCR-ABL protein with 10 novel amino acids inserted after amino acid 474 (with numbering as per GenBank cDNA clone NM_005157) (Figure 3). These novel amino acids would form the protein's C terminus, because the insertion would create a premature translation stop codon at nucleotide 30 of the intron-derived sequence (Figure 3). The truncated BCR-ABL variant would thus lack 653 C-terminal amino acids including 22 amino acids of the kinase domain, along with the entire C-terminal region downstream of the kinase domain. This region includes the entire “last exon” region, which contains a proline-rich domain (for interactions with proteins containing SH3 domains), three nuclear localization signals, a DNA-binding domain, an actin-binding domain, and a nuclear export signal.15 The tyrosine kinase and other functional activities of this truncated insertion variant—including possible resistance to imatinib—could be different from wild-type BCR-ABL. For example, a c-Abl variant lacking the entire C-terminal region downstream of the kinase domain retains its kinase activity (for some substrates), but lacks the associated cellular transforming activity.15 To directly assess these functions in our truncation mutant, expression of this variant clone in cultured hematopoietic cells is in progress.
Figure 3.
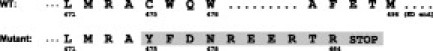
Amino acid sequence of the C terminus of the BCR-ABL kinase domain for the wild-type and insertion/truncation variant. Amino acid numbering (single letter codes) is per GenBank cDNA clone NM_005157. The intron 8-derived insertion begins within codon 475, changing a C to a Y. Mutant, insertion-derived amino acids (shaded) extend for 10 codons before a TAG stop codon. The wild-type BCR-ABL extends for another 631 amino acids beyond the end of the kinase domain (at amino acid 496).
To indirectly assess this mutation's pathological function, we determined its continued presence in serial follow-up samples drawn after its initial detection. In each of the two patients (1 and 2) with available follow-up samples, the intron 8 insertion was not detectable in a sample drawn two to three months after its initial discovery. In both cases, despite continued imatinib therapy, the follow-up sample had a 1.6- to 2.4-fold increased BCR-ABL transcript burden compared to the immediately prior sample with the insertion mutation. Because a BCR-ABL mutation conferring high-level imatinib resistance would be expected to persist (and expand) under the continued selective pressure of the drug, the transient appearance (and then disappearance) of the intron 8 insertion clone likely suggests a low-level (or absent) “resistance” phenotype for this mutation, perhaps because the insertion impairs the tyrosine kinase activity. Other transiently appearing BCR-ABL mutant clones have been previously described, even in patients with a stable complete cytogenetic response,16,17 and, rather than being directly pathogenic, may be the indirect consequence of the intrinsic genomic instability of CML. Consistent with the hypothesis that the intron 8 insertion may be transiently acquired during CML disease progression, in our one patient with an available pretherapy diagnostic sample (patient 2), the intron 8 insertion was not detectable at baseline.
In summary, we describe three CML patients undergoing tyrosine kinase inhibitor therapy, all of whom express the same unique BCR-ABL insertion/truncation mutation: the insertion of 35 bp from intron 8 into the C terminus of the kinase domain. Although aberrant RNA splicing is likely responsible for creating this variant, no specific nucleotide sequence substitutions were detected in the expressed cDNA sequences. These three insertion mutation cases were detected in our diagnostic clinical molecular pathology laboratory after sequencing 174 cases referred to us for suspected imatinib resistance, 78 of which (45%) contained a detectable mutation. The estimated prevalence of the exon 8/9 insertion/truncation mutation is then approximately 1.7% among patients with suspected drug resistance, and this mutation constitutes approximately 3.8% of all mutations. In comparison, previously described acquired mutations in BCR-ABL conferring putative imatinib resistance, have virtually always been point mutations.9 Although we do not yet know whether this insertion/truncation mutation is associated with imatinib resistance (or other specific functional alterations), laboratories that routinely screen the BCR-ABL kinase domain for possible drug resistance mutations should be aware that point mutations are not the only sequence variants to be found.
Footnotes
Supported, in part, by National Institutes of Health grants R21 CA095203 (to R.D.P.) and HL082978-01 (to M.W.D.), the Doris Duke Charitable Foundation (to B.J.D.), and the Leukemia and Lymphoma Society (to B.J.D. and M.W.D.).
References
- 1.Druker BJ, Guilhot F, O'Brien SG, Gathmann I, Kantarjian H, Gattermann N, Deininger MWN, Silver RT, Goldman JM. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355:2408–2417. doi: 10.1056/NEJMoa062867. [DOI] [PubMed] [Google Scholar]
- 2.Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA, O'Brien SG, So C, Massimini G, Guilhot F. Survival advantage from imatinib compared to the combination interferon-{alpha} plus cytarabine in chronic phase CML: historical comparison between two phase III trials. Blood. 2006;108:1478–1484. doi: 10.1182/blood-2006-02-001495. [DOI] [PubMed] [Google Scholar]
- 3.Press RD, Love Z, Tronnes AA, Yang R, Tran T, Mongoue-Tchokote S, Mori M, Mauro MJ, Deininger MW, Druker BJ. BCR-ABL mRNA levels at and after the time of a complete cytogenetic response (CCR) predict the duration of CCR in imatinib-treated patients with CML. Blood. 2006;107:4250–4256. doi: 10.1182/blood-2005-11-4406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hughes TP, Kaeda J, Branford S, Rudzki Z, Hochhaus A, Hensley ML, Gathmann I, Bolton AE, van Hoomissen IC, Goldman JM, Radich JP. Frequency of major molecular responses to imatinib or interferon alfa plus cytarabine in newly diagnosed chronic myeloid leukemia. N Engl J Med. 2003;349:1423–1432. doi: 10.1056/NEJMoa030513. [DOI] [PubMed] [Google Scholar]
- 5.Shah N, Nicoll J, Nagar B, Gorre M, Paquette R, Kuriyan J, Sawyers C. Multiple BCR-ABL kinase domain mutations confer polyclonal resistance to the tyrosine kinase inhibitor imatinib (STI571) in chronic phase and blast crisis chronic myeloid leukemia. Cancer Cell. 2002;2:117–125. doi: 10.1016/s1535-6108(02)00096-x. [DOI] [PubMed] [Google Scholar]
- 6.Kantarjian H, Giles F, Wunderle L, Bhalla K, O'Brien S, Wassmann B, Tanaka C, Manley P, Rae P, Mietlowski W, Bochinski K, Hochhaus A, Griffin JD, Hoelzer D, Albitar M, Dugan M, Cortes J, Alland L, Ottmann OG. Nilotinib in imatinib-resistant CML and Philadelphia chromosome-positive ALL. N Engl J Med. 2006;354:2542–2551. doi: 10.1056/NEJMoa055104. [DOI] [PubMed] [Google Scholar]
- 7.Talpaz M, Shah NP, Kantarjian H, Donato N, Nicoll J, Paquette R, Cortes J, O'Brien S, Nicaise C, Bleickardt E, Blackwood-Chirchir MA, Iyer V, Chen TT, Huang F, Decillis AP, Sawyers CL. Dasatinib in imatinib-resistant Philadelphia chromosome-positive leukemias. N Engl J Med. 2006;354:2531–2541. doi: 10.1056/NEJMoa055229. [DOI] [PubMed] [Google Scholar]
- 8.Deininger M, Buchdunger E, Druker BJ. The development of imatinib as a therapeutic agent for chronic myeloid leukemia. Blood. 2005;105:2640–2653. doi: 10.1182/blood-2004-08-3097. [DOI] [PubMed] [Google Scholar]
- 9.Hughes TP, Deininger MW, Hochhaus A, Branford S, Radich JP, Kaeda J, Baccarani M, Cortes J, Cross NC, Druker BJ, Gabert J, Grimwade D, Hehlmann R, Kamel-Reid S, Lipton JH, Longtine J, Martinelli G, Saglio G, Soverini S, Stock W, Goldman JM. Monitoring CML patients responding to treatment with tyrosine kinase inhibitors—review and recommendations for ‘harmonizing’ current methodology for detecting BCR-ABL transcripts and kinase domain mutations and for expressing results. Blood. 2006;108:28–37. doi: 10.1182/blood-2006-01-0092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Press RD, Galderisi C, Yang R, Rempfer C, Willis SG, Mauro MJ, Druker BJ, Deininger MWN. A half-log increase in BCR-ABL RNA predicts a higher risk of relapse in patients with CML with an imatinib-induced complete cytogenetic response (CCR) Clin Cancer Res. 2007;13:6136–6143. doi: 10.1158/1078-0432.CCR-07-1112. [DOI] [PubMed] [Google Scholar]
- 11.Branford S, Rudzki Z, Parkinson I, Grigg A, Taylor K, Seymour JF, Durrant S, Browett P, Schwarer AP, Arthur C, Catalano J, Leahy MF, Filshie R, Bradstock K, Herrmann R, Joske D, Lynch K, Hughes T. Real-time quantitative PCR analysis can be used as a primary screen to identify patients with CML treated with imatinib who have BCR-ABL kinase domain mutations. Blood. 2004;104:2926–2932. doi: 10.1182/blood-2004-03-1134. [DOI] [PubMed] [Google Scholar]
- 12.Branford S, Rudzki Z, Walsh S, Grigg A, Arthur C, Taylor K, Herrmann R, Lynch KP, Hughes TP. High frequency of point mutations clustered within the adenosine triphosphate-binding region of BCR/ABL in patients with chronic myeloid leukemia or Ph-positive acute lymphoblastic leukemia who develop imatinib (STI571) resistance. Blood. 2002;99:3472–3475. doi: 10.1182/blood.v99.9.3472. [DOI] [PubMed] [Google Scholar]
- 13.Baralle D, Baralle M. Splicing in action: assessing disease causing sequence changes. J Med Genet. 2005;42:737–748. doi: 10.1136/jmg.2004.029538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Volpe G, Cignetti A, Panuzzo C, Kuka M, Vitaggio K, Brancaccio M, Perrone G, Rinaldi M, Prato G, Fava M, Geuna M, Pautasso M, Casnici C, Signori E, Tonon G, Tarone G, Marelli O, Fazio V, Saglio G. Alternative BCR-ABL splice variants in Philadelphia chromosome-positive leukemias result in novel tumor-specific fusion proteins that may represent potential targets for immunotherapy approaches. Cancer Res. 2007;67:5300–5307. doi: 10.1158/0008-5472.CAN-06-3737. [DOI] [PubMed] [Google Scholar]
- 15.Hantschel O, Superti-Furga G. Regulation of the c-Abl and Bcr-Abl tyrosine kinases. Nat Rev Mol Cell Biol. 2004;5:33–44. doi: 10.1038/nrm1280. [DOI] [PubMed] [Google Scholar]
- 16.Sherbenou DW, Wong MJ, Humayun A, McGreevey LS, Harrell P, Yang R, Mauro M, Heinrich MC, Press RD, Druker BJ, Deininger MW. Mutations of the BCR-ABL-kinase domain occur in a minority of patients with stable complete cytogenetic response to imatinib. Leukemia. 2007;21:489–493. doi: 10.1038/sj.leu.2404554. [DOI] [PubMed] [Google Scholar]
- 17.Khorashad JS, Anand M, Marin D, Saunders S, Al-Jabary T, Iqbal A, Margerison S, Melo JV, Goldman JM, Apperley JF, Kaeda J. The presence of a BCR-ABL mutant allele in CML does not always explain clinical resistance to imatinib. Leukemia. 2006;20:658–663. doi: 10.1038/sj.leu.2404137. [DOI] [PubMed] [Google Scholar]


