Abstract
Introduction
Virtual reality (VR) simulators have been developed to train basic endoscopic surgical skills outside of the operating room. An important issue is how to create optimal conditions for integration of these types of simulators into the surgical training curriculum. The willingness of surgical residents to train these skills on a voluntary basis was surveyed.
Methods
Twenty-one surgical residents were given unrestricted access to a VR simulator for a period of four months. After this period, a competitive element was introduced to enhance individual training time spent on the simulator. The overall end-scores for individual residents were announced periodically to the full surgical department, and the winner was awarded a prize.
Results
In the first four months of study, only two of the 21 residents (10%) trained on the simulator, for a total time span of 163 minutes. After introducing the competitive element the number of trainees increased to seven residents (33%). The amount of training time spent on the simulator increased to 738 minutes.
Conclusions
Free unlimited access to a VR simulator for training basic endoscopic skills, without any form of obligation or assessment, did not motivate surgical residents to use the simulator. Introducing a competitive element for enhancing training time had only a marginal effect. The acquisition of expensive devices to train basic psychomotor skills for endoscopic surgery is probably only effective when it is an integrated and mandatory part of the surgical curriculum.
Keywords: Virtual reality simulation, Endoscopic Surgery, Surgical training, Curriculum design, Resident participation
Endoscopic surgery requires dedicated skills such as three-dimensional orientation in a two-dimensional representation of the operating field and complex instrument handling [8, 7, 5]. Training of these skills in the operating room (OR) is under pressure due to planning issues and ethical considerations. Virtual reality (VR) simulators have been developed to train basic endoscopic surgical skills outside of the OR. Several simulators have been validated and found adequate for the transfer of skills from the simulator to the OR [2, 6, 9, 13, 14]. However, discussion arises on how to integrate these simulation-based training modalities in the surgical training curriculum.
A questionnaire was distributed to 245 Dutch surgical residents to explore the perspective of the trainee on this issue. Approximately 75% of residents felt that endoscopic skills training outside the OR is useful [12]. In another study, sixty Dutch gynaecology residents responded positively (3.9 on a five-point Likert scale) with regard to training in laparoscopic skills before real surgery [10]. Fifty-five percent of these 60 residents did not have the opportunity to train laparoscopic skills. However, those that did appeared to train only once or twice a year and 33% did not use available skills trainers voluntarily at all. We hypothesized that insufficient simulator access might be the reason for this contradiction. Therefore, we investigated the willingness of surgical residents to train in endoscopic skills on a voluntary basis when VR simulators were indeed readily available. We also evaluated the effect of competitive incentives on the frequency and duration of simulator training.
Materials and methods
Equipment, tasks and scoring system
This study is performed with the LapSim virtual reality simulator, which uses the Virtual Laparoscopic Interface (VLI) hardware, (Immersion Inc., San Jose, CA, USA) The VLI has an interface with a 2600 MHz hyperthreading processor Pentium IV computer running Windows XP and is equipped with 256 random-access memory (RAM), a GeForce graphics card and an 18-inch thin-film transistor (TFT) monitor. The systems feature LapSim Basic Skills 3.0 software (Surgical Science Ltd, Göteburg, Sweden), from the LapSim Basic Skills package, consisting of nine tasks.
A training program was designed that included all nine tasks: camera navigation, instrument navigation, coordination, grasping, lifting and grasping, cutting, clipping and cutting, suturing and fine dissection [4].
The computer stores and displays between seven and eleven parameters of performance per task. These parameters are related to time, errors or efficiency of handling.
Tasks can be adjusted to different levels of difficulty. The training program for this study was set at an advanced level with thresholds that are based on the performance of 30 experienced endoscopic surgeons (more than 100 endoscopic procedures).
The scoring system is two-tiered. First, for any given parameter the system determines whether or not the participant passes or fails the test. Secondly, if a participant passes, a score of between 0% and 100% is attached to his or her performance on that particular parameter. The overall score per task is determined by the sum score of the parameters, divided by their number. Hence, an overall score of 100% can only be obtained by scoring 100% on each of the individual parameters measured during performance of the particular task. An outcome score of 100 points is given to those participants who score a 100% on the task performed. Logically, a score of 85% thus translates into 85 points. A maximum overall score of 900 could be obtained (i.e., 100 points on each of the nine tasks measured).
Participants
Twenty-one surgical residents, ranging from postgraduate year (PGY) -one level to PGY 6 level, with different endoscopic surgical experience, were given unlimited access to the simulator. Seven residents were at the beginning of their surgical educational program (PGY 1 and PGY 2) and therefore inexperienced in endoscopic surgery. Seven residents were in the middle (PGY 3 and PGY 4) and eight residents were at the end (PGY 5 and PGY 6) of their surgical educational program.
Setting and incentives
In the period May 2005 to January 2006 a simulator was placed in the general room for surgical residents at the surgical ward of the University Medical Centre in Utrecht. Before the study, residents were instructed on how to operate the simulator, and allocated a personal login number for the simulator. By placing the simulator in the general residents’ room, it was readily and easily accessible 24 hours a day. The room is secured by a code-locked door and accessible by residents only.
During the first four months, there were no additional incentives other than the permanent (24-hour) accessibility to the residents for training on the simulator. After these four months, a competitive element was introduced in which the frequency of training was also rewarded (bi-weekly). The overall end-score was calculated every other week by adding this frequency bonus to the highest scores for each task. These overall end-scores for each resident were publicly announced to the complete department of surgery and the winner (the resident with the highest score) was awarded a prize.
Questionnaire
After eight months all residents were requested to fill out a questionnaire.
Ten questions were presented on a five-point Likert scale, concerning their perception of their own experience level in endoscopic procedures, their opinion of the possibility to develop and train endoscopic skills within the current surgical curriculum, and their opinion about the application of virtual reality as a means to training endoscopic skills. Value 1 was assigned to “totally agree”, value 5 to “totally disagree”. In addition, the residents were asked about their frequency of usage of the simulator. If a participant indicated little usage, he or she was questioned why, and what could motivate increased usage.
Results
In the first four months only two of the 21 residents (10%) trained on the simulator, for a total of 163 minutes. One resident was a PGY 2, the other one a PGY 5. In the second period of four months the number of trainees increased to seven residents (33%, two PGY 2, two PGY 3, one PGY 5 and two PGY 6). The duration of training increased to 738 minutes, thereby constituting an average increase of 23.9 minutes per subject. Fifty-eight percent of training was performed during night shifts.
All 22 residents (100%) replied to the questionnaire. The total training time, as an accumulation of estimation on individual training time, was 4140 minutes. The actual cumulated training time for all residents was 901 minutes (22%). Thirteen out of 15 residents who did not train at all (86%) stated that this was due to a lack of time during the day. One resident (7%) stated he had been not interested enough to train and indicated that he had alternative priorities. Another resident (7%) stated that she was fully occupied due to an intensive-care traineeship and maternity leave.
Residents suggested that the use of the VR trainers could be enhanced by incorporating a mandatory VR training into the surgical curriculum (9x = people agreeing), to oblige certain skills level on VR simulator before starting endoscopic surgery in the OR (3x), to implement competitive training with coaching (2x), to diminish working pressure (2x), to have more-advanced exercises available on the simulator (3x), to place the VR simulator in a location other than in the residents’ room (1x). Only two stated that more initiative of residents was required to improve outcome.
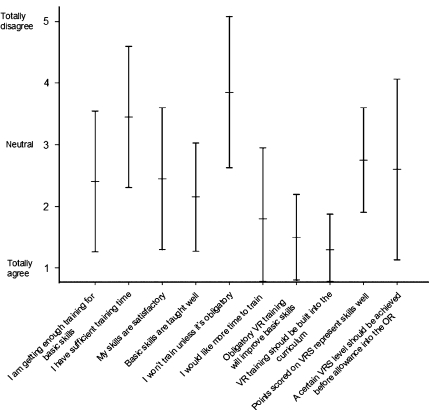
Figure 1 refers to the perception of residents’ own experience level in endoscopic procedures, their opinion of the possibility to develop and train endoscopic skills within the current surgical curriculum and their opinion about the application of virtual reality as a means to training endoscopic skills.
Fig. 1.
Results of questionnaire
In general, the opinion of the residents on their own experience level, on the possibility to develop and train endoscopic skills during their training and on the role of virtual reality varies considerably [standard deviation (SD) 0.44 to 1.39]. Their opinion on obligation of VR training to improve endoscopic skills and having VR training as a mandatory part of the basic skills training is most uniform. Residents do not have a marked positive, nor a marked negative opinion on the presented statements on receiving enough training for acquiring basic skills (mean 2.63, SD 1.19), on receiving sufficient training time in the OR to train in endoscopic skills (mean 3.47 SD 1.17) and on acquiring a satisfactory level of basic psychomotor skills (mean 2.42, SD 1.16). The same applies to their opinion on the representation of their training results on the simulator (mean 2.98, SD 0.83); as well as on the statement that thresholds should be reached before training in the OR is allowed (mean 2.47, SD 1.39). There is one statement they do not agree with; I will not train unless it is obligatory (mean 4.26, SD 1.10).
Discussion
Virtual reality training has the potential to improve and professionalize the training in endoscopic basic psychomotor skills [2, 6, 9, 13, 14]. Training results can be shown instantly to demonstrate objective performance and progress of performance assessment. However, one of the main concerns in acquisition of expensive equipment for educational purposes is its effectiveness. While initial enthusiasm about new innovative equipment is usually high among the surgical community, actual usage tends to be disappointing [3]. This study was undertaken to evaluate the aptitude for training on a voluntary basis when a VR simulator was readily available. Free unlimited access to a VR simulator without obligation or assessment in our setting did not seem to motivate surgical residents to use the simulator for improvement of their psychomotor endoscopic skills level. The addition of a competitive element and a desirable prize had only a marginal effect on the frequency and duration of training. We believe that the effort required to provide this incentive is disproportionate to its marginal effect.
The majority of residents (86%) stated that ‘lack of time due to high working pressure’ is the most important reason for not using the simulator. Following a recent European guideline, as set by the European Commission, a working week for a resident in training is being reduced from 70 to 48 hours [1, 11]. This may have led to an increase in pressure during working hours, with little time available for voluntary training. However, spare time has increased vastly compared to the former curriculum. Residents did not use personal free time for VR simulator training to improve their skills.
The perception of their own experience level in endoscopic procedures and the possibility of developing and training in endoscopic skills within the current surgical curriculum was in general neutral. Therefore no conclusions can be drawn from this. There is favorable, uniform opinion on the desirability of integration of skills training into the curriculum. In addition, residents believe skills training ought to be mandatory for marked improvement of their psychomotor skills. Interestingly, the disagreement on the statement of not training unless it is obligatory (mean 4.26, SD 1.10) appears to have no bearing in reality, because our study shows very limited use of the simulator. This incongruence might be caused by political correctness or by a discrepancy between intentions and actions.
It must be said that our result reflects the quantity of training on a voluntary basis of 22 residents in a single institute only, and might therefore not represent the attitude of national or international surgical residents.
In conclusion, the acquisition of expensive devices to train basic psychomotor skills for endoscopic surgery is probably only effective when it is a mandatory part of the curriculum.
References
- 1.European Community. Directive 2000/34/EC of the European Parliament and of the Council of 22 June 2000 amending Council Directive 93/104/EC concerning certain aspects of the organisation of working time to cover sectors and activities excluded from that Directive. Official Journal of the European Communities, No. L 195, 1 August 2000, pp 41–45
- 2.Carter FJ, Schijven MP, Aggarwal R, Grantcharov T, Francis NK, Hanna GB, Jakimowicz JJ (2005) Consensus guidelines for validation of virtual reality surgical simulators. Surg Endosc 19:1523–1532 [DOI] [PubMed]
- 3.Chang L, Petros J, Hess DT, Rotondi C, Babineau TJ (16-12-2006) Integrating simulation into a surgical residency program: Is voluntary participation effective? Surg Endosc (in press) [DOI] [PubMed]
- 4.Eriksen JR, Grantcharov T (2005) Objective assessment of laparoscopic skills using a virtual reality stimulator. Surg Endosc 19:1216–1219 [DOI] [PubMed]
- 5.Gallagher AG, McClure N, McGuigan J, Ritchie K, Sheehy NP (1998) An ergonomic analysis of the fulcrum effect in the acquisition of endoscopic skills. Endoscopy 30:617–620 [DOI] [PubMed]
- 6.Grantcharov TP, Kristiansen VB, Bendix J, Bardram L, Rosenberg J, Funch-Jensen P (2004) Randomized clinical trial of virtual reality simulation for laparoscopic skills training. Br J Surg 91:146–150 [DOI] [PubMed]
- 7.Hanna GB, Cuschieri A (1999) Influence of the optical axis-to-target view angle on endoscopic task performance. Surg Endosc 13:371–375 [DOI] [PubMed]
- 8.Hanna GB, Shimi SM, Cuschieri A (1998) Randomised study of influence of two-dimensional versus three-dimensional imaging on performance of laparoscopic cholecystectomy. Lancet 351:248–251 [DOI] [PubMed]
- 9.Hyltander A, Liljegren E, Rhodin PH, Lonroth H (2002) The transfer of basic skills learned in a laparoscopic simulator to the operating room. Surg Endosc 16:1324–1328 [DOI] [PubMed]
- 10.Kolkman W, Wolterbeek R, Jansen FW (2005) Gynecological laparoscopy in residency training program: Dutch perspectives. Surg Endosc 19:1498–1502 [DOI] [PubMed]
- 11.Sakorafas GH, Tsiotos GG (2004) New legislative regulations, problems, and future perspectives, with a particular emphasis on surgical education. J Postgrad Med 50:274–277 [PubMed]
- 12.Schijven MP, Berlage JT, Jakimowicz JJ (2004) Minimal-access surgery training in the Netherlands: a survey among residents-in-training for general surgery. Surg Endosc 18:1805–1814 [DOI] [PubMed]
- 13.Schijven MP, Jakimowicz JJ, Broeders IA, Tseng LN (2005) The Eindhoven laparoscopic cholecystectomy training course—improving operating room performance using virtual reality training: results from the first E.A.E.S. accredited virtual reality trainings curriculum. Surg Endosc 19:1220–1226 [DOI] [PubMed]
- 14.Seymour NE, Gallagher AG, Roman SA, O’Brien MK, Bansal VK, Andersen DK, Satava RM (2002) Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg 236:458–463 [DOI] [PMC free article] [PubMed]