Abstract
Global climate change is inevitable — the combustion of fossil fuels has resulted in a buildup of greenhouse gases within the atmosphere, causing unprecedented changes to the earth's climate. The Fourth Assessment Report of the Intergovernmental Panel on Climate Change suggests that North America will experience marked changes in weather patterns in coming decades, including warmer temperatures and increased rainfall, summertime droughts and extreme weather events (e.g., tornadoes and hurricanes). Although these events may have direct consequences for health (e.g., injuries and displacement of populations due to thermal stress), they are also likely to cause important changes in the incidence and distribution of infectious diseases, including vector-borne and zoonotic diseases, water-and food-borne diseases and diseases with environmental reservoirs (e.g., endemic fungal diseases). Changes in weather patterns and ecosystems, and health consequences of climate change will probably be most severe in far northern regions (e.g., the Arctic). We provide an overview of the expected nature and direction of such changes, which pose current and future challenges to health care providers and public health agencies.
Human activities have caused a sharp increase in greenhouse gases, including carbon dioxide, nitrous oxide and methane, in the atmosphere, which has led to unprecedented changes in the earth's climate. The Intergovernmental Panel on Climate Change was established by the United Nations Environment Program and the World Meteorological Organization in 1988 to provide objective analysis of data related to climate change. The panel comprises scientists from around the globe and aims to present the scientific, technical and socioeconomic issues arising from the data to government decision-makers in a policy-neutral context.
In April 2007, the panel issued a report on the impact of global climate change on human and animal populations.1 This report was based on about 30 000 observations of changes in physical and biological systems worldwide. More than 90% of these changes are attributable to human activities such as the combustion of fossil fuels.1,2 The panel's fourth assessment report includes projections for regions including North America. These projections include warmer temperatures (Figure 1), more rainfall because of an increased fraction of precipitation falling as rain rather than snow, and more frequent droughts, wildfires and extreme weather events such as hurricanes and tornados.1 Warming is predicted to be most severe in the northernmost latitudes.
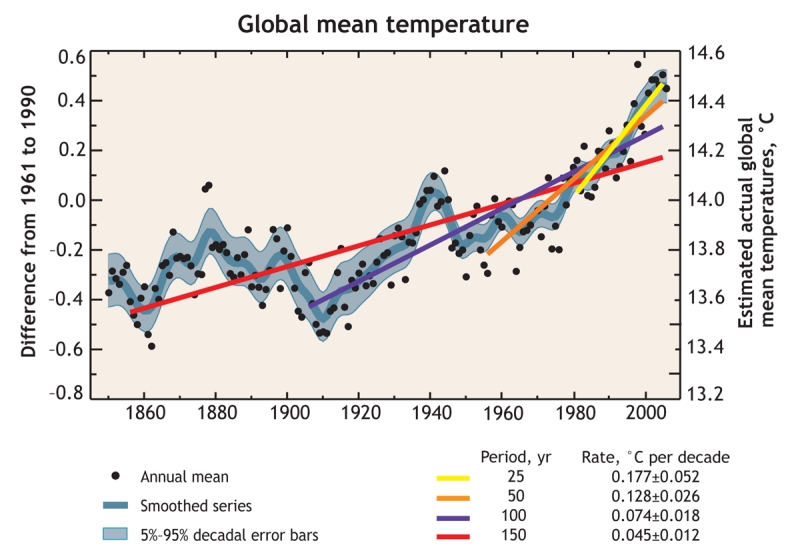
Figure 1: Trends in mean global temperatures since the mid-19th century. Coloured lines represent the linear trends over various time periods. Shorter (more recent time periods) lines have steeper slopes, indicating an accelerating warming trend for the planet. Reproduced, with permission, from reference 2. Copyright 2007 Cambridge University Press.
Some of the health effects attributable to climate change are directly related to changing environmental conditions. The Public Health Agency of Canada anticipates increased burden of disease as a result of thermal stress and more frequent extreme weather events,3 and some projected direct effects of climate change on human health, such as heat-related morbidity and injuries, have been previously reviewed.4 However, climate and weather patterns are important physical components of complex ecosystems5 and any major change in the nonliving component of an ecosystem will affect living components, including microbes, insect vectors, animal reservoirs and susceptible humans, and change the incidence and distribution of infectious diseases.
The close relation between climate, environment and infectious disease in the developing world are well recognized. For example, the importance of rainfall and drought in the occurrence of malaria,6,7 the influence of the dry season on epidemic meningococcal disease in the sub-Saharan African “meningitis belt”8 and the importance of warm ocean waters in driving cholera occurrence in the Ganges River delta and elsewhere in Asia9 are well described. Indeed, there is widespread concern about the potential impact of global climate change on the distribution and burden of these and other infectious threats in the developing world.1,7
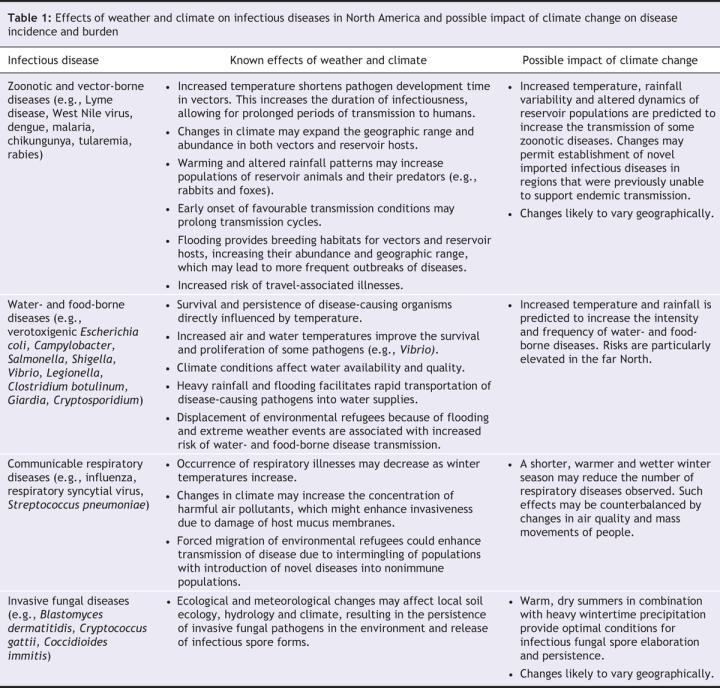
The relation between ecosystems, infectious diseases and global climate change are less intuitive in the context of more developed countries where clean drinking water, reduced exposure to insect vectors, higher-quality housing and other advantages partly mitigate such threats. However, climate changes projected to occur in the coming decades are likely to influence the burden and incidence of infectious diseases in more developed regions including North America. In this review, we describe the nature and direction of changes in infectious disease epidemiology that are likely to accompany global climate change and describe the challenges that these changes will pose to health care providers and public health agencies. We focus principally on Canada and the United States, including the Arctic regions of North America, where the effects of global climate change are likely to be most severe. We also include several illustrative examples from other highly developed regions such as the European Union and Australia. In particular, we review several zoonotic diseases of public health importance, the association between precipitation and water-borne diarrheal diseases, seasonal respiratory diseases with person-to-person transmission and endemic mycoses (Table 1).
Table 1
This review is not meant to obscure the likelihood that the brunt of the increased incidence of infectious diseases related to climate change will occur in the same less-developed, economically poor countries that are currently most affected by infectious diseases.1,10 For more information about the projected changes in infectious disease epidemiology in these diverse regions of the world, we encourage readers to consult the panel report and other reports and reviews devoted to this topic.1,7,11,12
Zoonotic and vector-borne diseases
Climate change may affect zoonoses (infectious diseases of animal origin that may be transmitted to humans) in 3 ways: it may increase the range or abundance of animal reservoirs or insect vectors, prolong transmission cycles, or increase the importation of vectors or animal reservoirs (e.g., by boat or air) to new regions, which may cause the establishment of diseases in those regions. For example, the burden of Lyme disease (a tick-borne borreliosis) is likely to change substantially in North America and Europe. Currently, endemic Lyme disease is uncommon in Canada, and established populations of competent vectors (vectors that are capable of allowing the pathogen to complete its lifecycle, such as Ixodes scapularis and Ixodes pacificus) are limited largely to southern Ontario, Nova Scotia and British Columbia.13 However, temperature determines the northernmost extent of tick populations. Mathematical models suggest that tick abundance may greatly increase in southern Canada, with a northern expansion of about 200 km by the year 2020. This rate of expansion would be sufficient to establish vector populations in Alberta and Saskatchewan (Figure 2).13
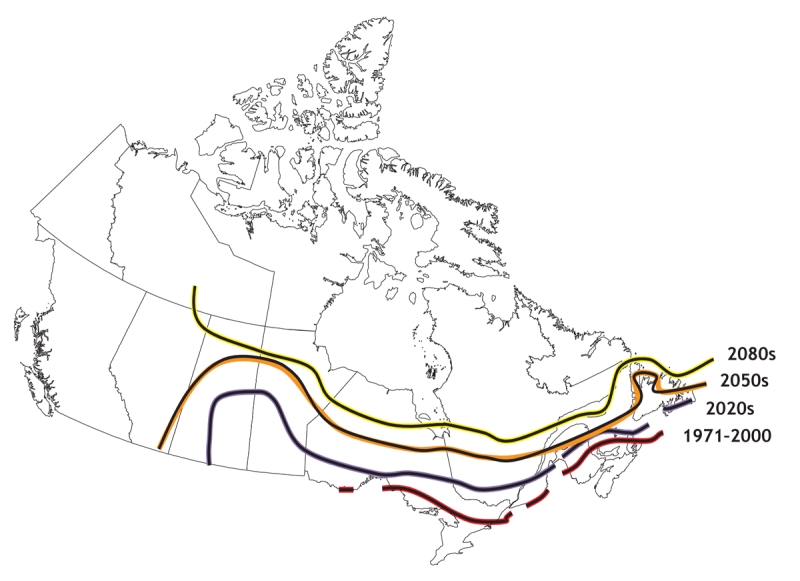
Figure 2: Upper temperature limits for Ixodes scapularis establishment in Canada, based on mathematical models. The graph shows the current upper geographic limits and projected limits for the 2020s, 2050s and 2080s, assuming continuous population growth, regionally oriented economic development and no reduction in greenhouse gas emissions. Upper and lower model-derived confidence limits are mapped as coloured lines around the black lines. Modified, with permission, from Elsevier (Int J Parasitol 2006;36: 63–70).13
In North America, other infectious diseases that may expand their ranges because of northern expansion of vector populations include such tick-borne threats as babesiosis, anaplasmoses and Powassan encephalitis in addition to mosquito-borne threats such as dengue. In Europe, the expansion of the range of ticks and other vectors (e.g., sandflies) may increase the incidence and distribution of Lyme disease,14 boutonneuse fever15 and leishmaniasis.16 In Australia, the southern expansion of mosquito ranges is expected to result in an increase in such endemic diseases as Ross River virus, Barmah Forest virus and Murray Valley encephalitis.17,18
The transmission of vector-borne zoonoses may also be enhanced by earlier onset of spring, resulting in a prolonged amplification cycle. West Nile virus, which appeared in Canada in 2002, has an amplification cycle that involves mosquitoes and birds. Human infections become more likely as the proportion of “bridge” vectors (mosquitoes that bite both birds and humans) increases. In temperate regions, virus amplification begins with the onset of mosquito activity in spring. Human risk peaks in late summer or early autumn, and risk decreases with the disappearance of mosquitoes in autumn. An earlier onset of spring would prolong the amplification cycle resulting in an increased incidence of human infection. The impact of increased precipitation on mosquito ecosystems is complicated. Transmission risk could increase because of increased mosquito breeding sites. Alternatively, increased numbers of mosquito predators and decreased geographic concentrations of amplifying hosts (i.e., birds) attributable to a rise in the distribution of water sources may lower the risk of transmission.11,19
Whether climate change will facilitate re-establishment of autochthonous (locally acquired) malaria in the United States and Canada, where it was once endemic,20 is unclear. However, prolonged amplification cycles and warmer winter temperatures may facilitate the establishment of imported mosquito-borne diseases in countries from which they have historically been absent. For example, in 2007 chikungunya fever, a mosquito-borne disease endemic in parts of Africa and Asia, caused a large outbreak of disease in northeastern Italy, presumably following importation of infected mosquitoes via boat or air.21 The onset of winter weather likely contributed to the control of this outbreak, but warming trends may make the control of future importation-related outbreaks more difficult.
Residents of temperate regions of North America may also be affected by increased incidence and distribution of vector-borne diseases in other countries because of high rates of travel to subtropical and tropical countries. For example, it is estimated that Canadians took over 2 million trips to Mexico, Cuba and the Dominican Republic in 2006 alone.22 As dengue and malaria activity are projected to increase in Latin America, the Caribbean, Asia and Africa, an increase in travel-related dengue fever and malaria in returning travellers is likely.1,9,23–25 Marked discrepancies in dengue incidence in contiguous geographical areas (e.g., along the US–Mexican border26) suggest that both vector abundance and economic factors, such as the availability of air conditioning, contribute to disease risk. Travellers who use more luxurious accommodations and insect repellents that contain diethyltoluamide (DEET) may be relatively protected.27 Nonetheless, the impact of such increases on local populations, combined with emerging resistance to antimalarial agents25 and the recent resurgence of malaria in a number of urban areas in Jamaica and India,28,29 are cause for substantial concern both for travel medicine practitioners and for those concerned about global health.
Climate change is also likely to impact the distribution and burden of zoonotic diseases that are not dependent on insect vectors for transmission. Pathogens such as the Sin Nombre virus, a cause of hantavirus pulmonary syndrome, are harboured by rodent species that are especially abundant in the southwestern United States and in western states and provinces.30–32 Rodent population density appears to be a key driver of disease in humans,32 who are often infected after exposure to dust contaminated by rodent urine (e.g., while sweeping out storage spaces). Recent surges in hantavirus infection have been attributed to the El Niño-type weather conditions, which may become predominant with future climate change,30 suggesting that hantavirus pulmonary syndrome incidence may increase in coming decades. Climate change may similarly increase the risk of plague in western states and provinces.33
Water-and food-borne diseases
Water-and food-borne diseases are a major cause of mortality worldwide and an important cause of morbidity in developed countries. Water-borne pathogens include viral, bacterial and protozoan agents of gastroenteritis and pneumonic pathogens such as Legionella species. Many of these pathogens (e.g., verotoxigenic Escherichia coli, Campylobacter species and viral pathogens) are also important causes of food-borne illness, as are bacterial pathogens such as Salmonella and Shigella species.
Water-borne diseases occur despite state-of-the-art water treatment technology. For example, a 1989 cryptosporidiosis outbreak tied to a municipal water supply in Milwaukee, Wisconsin, affected an estimated 400 000 people.34 The Walkerton, Ontario, disaster in 2000 underscored the vulnerability of populations to water-borne disease.35,36 The incidence of both water-and food-borne diseases is expected to increase as a result of climate change. Large water-borne disease outbreaks have been linked to extreme precipitation events, which are expected to increase in frequency in coming decades (Figure 3). In addition, most cases of water-and food-borne gastroenteritis, particularly illness related to Campylobacter and Salmonella, exhibit a distinct summertime pattern of occurrence.37 Although it is possible that seasonality is due to behavioural patterns (e.g., barbecuing or swimming in the summer), the association between warmer temperatures and disease suggests that rates of water-and food-borne illness are likely to increase with rising temperatures.
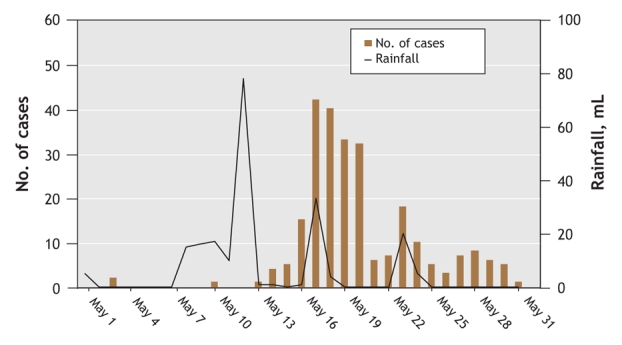
Figure 3: Association between precipitation and water-borne disease outbreaks. The graph shows the relation between unusually heavy rainfall and the number of confirmed cases of verotoxigenic Escherichia coli infection that occurred during a massive enteric disease outbreak in Walkerton, Ontario, in May 2000. The incubation period for verotoxigenic E. coli is usually 3–4 days, which is consistent with the lag between extreme precipitation events and surges in the number of cases. The figure is based on data published by Auld et al36 and data published in Report of the Walkerton Inquiry: the events of May 2000 and related issues. Part one.50
The incidence of pneumonic infections due to water-borne infectious agents, such as legionellosis (Legionnaire disease) and melioidosis, is also likely to be affected by climate change. Legionellosis incidence peaks during warmer months and risk appears to increase with rainy, humid weather.38 Melioidosis is an infectious disease caused by the bacterium Burkholderia pseudomallei and is endemic in southeast Asia and Australia. Cyclones appear to be associated with increased risk of severe melioidosis, perhaps because of aerosolization of the bacterium by stormy weather.39
Globally, the water-borne enteric disease most likely to increase in the face of global climate change is cholera, a diarrheal disease with a high case-fatality rate caused by infection with toxigenic strains of Vibrio cholerae, which remains an important cause of death in the developing world. Risk increases with warmer water temperatures, suggesting that global cholera activity may increase sharply in the face of climate change.40 Such increases pose a risk not only to developing countries, but also to developed countries via importation of disease. Nontoxigenic strains of V. cholerae and other noncholera Vibrio (e.g., Vibrio parahemolyticus and Vibrio vulnificus) may also become more frequent agents of disease as a result of increasing ocean temperatures and increasing frequency of extreme weather events. For example, cases of illness due to these micro-organisms occurred in association with Hurricane Katrina in 2005.41
Seasonality of communicable diseases
Many respiratory pathogens, including influenza, respiratory syncytial virus and Streptococcus pneumoniae, exhibit winter seasonality that is often attributed to seasonal changes in temperature or population behaviour (e.g., indoor crowding). In fact, these phenomena are poorly understood and causal mechanisms are difficult to establish owing to seasonal coincidence of multiple exposures.42 If cold temperatures are an important driver of respiratory disease, climate change might be expected to attenuate the impact of influenza epidemics. Data based on influenza activity during the El Niño Seasonal Oscillation (an intermittent inversion of Pacific Ocean thermal gradients) suggest that this may be the case.43,44 El Niño is associated with changes in weather patterns similar to those projected to occur in coming decades. In this sense, study of disease trends in the presence and absence of El Niño may provide insight into future disease patterns.
Climate change also has the potential to indirectly affect communicable disease transmission. The forced migration of people because of drought or flooding could increase the transmission of many communicable diseases because of enhanced intermingling of populations that have previously been isolated from one another. Large-scale migrations have been associated with surges in communicable diseases and emergence of novel infections throughout recorded history. Forced migration may ultimately be a more important driver of changes in infectious disease epidemiology than other effects described in this review.
Endemic mycoses
Several fungal pathogens of public health importance produce spores that rely on local soil ecology and climate for persistence in the environment. As ecosystems change, the burden of invasive fungal disease may increase. The dry summers and heavy wintertime precipitation projected for North America match the optimal conditions for spore dispersal by Blastomyces dermatitidis, a fungus that causes disease of the bones, lungs and skin. In Canada, B. dermatitidis occurs most commonly in northwestern Ontario.45 The incidence of disease due to Coccidioides imitis, which is endemic to the southwestern United States and causes pulmonary, central nervous system and bone disease, may also be altered by changing rainfall, drought and temperature patterns.33
Warmer, drier summers may have facilitated the establishment of Cryptococcus gattii in Canada.46 This fungus had previously been seen only in tropical and subtropical regions (particularly those in Australia), but emerged on Vancouver Island in 1999, where it has caused more than 100 cases of human illness in addition to illness in domestic animals.
Arctic regions
Arctic regions are uniquely vulnerable ecosystems that have experienced warming trends that are more substantial than those experienced elsewhere in North America.3 An increased incidence of water-and food-borne disease and zoonoses appears inevitable. The economic, social and environmental impact of disease emergence in Arctic regions will place a heavy burden on already underserved communities. Hunting and traditional means of food preparation may also increase the probability of contracting an infectious disease.
Increases in ocean temperatures have been linked to outbreaks of gastroenteritis as a result of infection by noncholera Vibrio species, which may have been acquired through consumption of contaminated seafood. Likewise, the risk of botulism from consumption of traditional fermented meats is enhanced by increased ambient air temperatures.
Changing ecosystems also disrupt the ecology of wildlife populations in ways that are likely to increase the risk of zoonotic disease. Climate-driven increases in rabbit and predator populations (e.g., fox) may augment the risk of tularemia and rabies.47 Warmer temperatures and longer summers increase the number of amplification cycles for parasites of food animals (e.g., Trichinella and Echinococcus species) and lead to longer summer hunting seasons. These parasites cause diseases that are largely concentrated in northern communities,48,49 and the burden of parasitic diseases in the North may increase with warming.
Conclusion
Climate change will increase the risk of infectious disease by expanding the ranges of species known to carry zoonotic diseases, changing pathogen dynamics in environmental reservoirs and altering pathogen transmission cycles. How should the medical and public health communities prepare for such threats? As a first step, agencies must have the ability to measure changes in disease burden. The fact that several diseases described above (e.g., Lyme disease, blastomycosis, echinococcosis and, since 1999, trichinosis) are not subject to national surveillance in Canada will make such reporting difficult. It may be helpful to reconsider the status of several of these important diseases.
At a more basic level in North America, the wide ranging and unpredictable health effects that are likely to result from climate change highlight the need for strengthening public health infrastructure related to disease surveillance, food and water safety, control of insect vectors and animal reservoirs of disease, and public health outbreak response. Although mitigation of greenhouse gas emissions cannot be regarded as the primary responsibility of the health care system or medical practitioners, physicians and other health care providers are highly credible opinion leaders and advocacy on environmental issues can be seen as a natural extension of the medical profession's interest in enhancing the health of the communities it serves.
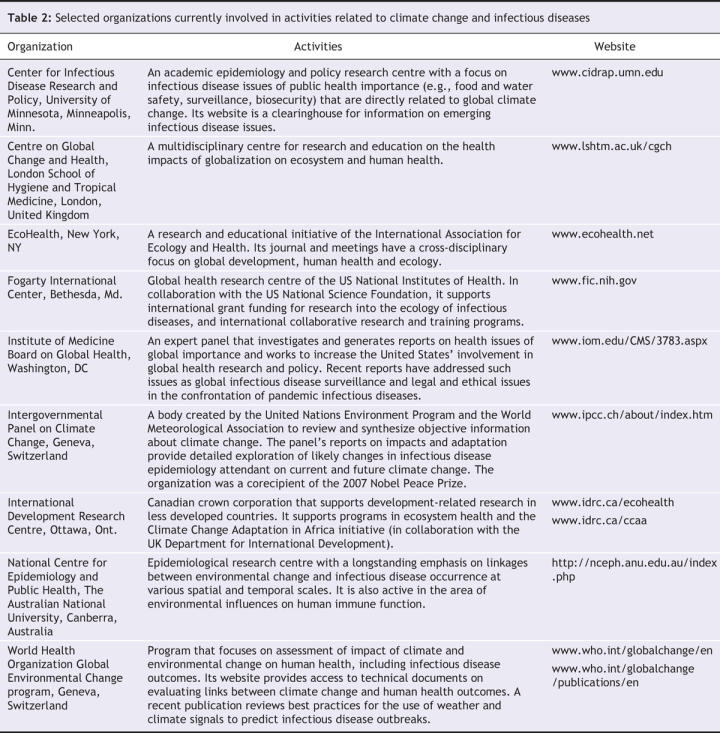
In less developed countries, changes in infectious disease burden due to climate change will be greater than those seen in the developed world, and enhancement of public health infrastructure (particularly related to surveillance and outbreak forecasting,7 provision of safe food and water, and vector control) will be the key to mitigating the effects of climate change. The global scope of these challenges and the fact that infectious diseases do not respect national borders highlight the need for multinational and collaborative scientific efforts to control disease. There are currently many national and international initiatives underway that are directly or indirectly related to climate change, infectious diseases and global health (Table 2).
Table 2
Finally, the importance of animal and environmental reservoirs of disease suggests that interdisciplinary communication between health professionals, veterinarians, environmental scientists, ecologists, geographers and economists seeking to understand climate change will be key to protecting people in North America and worldwide against these threats. Rigorous cross-disciplinary studies using a variety of methodologic tools will enable us to predict the transmission dynamics of diseases under different climate scenarios and estimate the cost-effectiveness of mitigation strategies. The performance of such high-quality research will depend on the extent to which such endeavours are embraced by decision-makers, the research community and funding agencies.
Key points of the article
• Global climate change is occurring as a result of greenhouse gases created by human activities. Changes in climate and associated changes in weather and other environmental exposures will have important consequences for human health.
• Climate change will alter the relations between microbes, insect vectors, animal reservoirs of infectious diseases and humans, and will alter the burden and distribution of infectious diseases of public health importance.
• Warmer temperatures and altered rainfall patterns are likely to increase the range and burden of vector-borne infectious diseases in North America and elsewhere.
• Altered patterns of rainfall and increased frequency of extreme weather events are likely to influence the incidence of water-borne gastrointestinal and respiratory diseases in North America and elsewhere.
• The best defence against increases in infectious disease burden related to climate change lies in strengthening existing public health infrastructure. Physicians, as opinion leaders, can also influence public policy related to greenhouse gas emissions.
Acknowledgments
All of the authors receive financial support from the US National Institute of Allergy and Infectious Diseases (R21AI065826-01A1) and from the Early Researcher Award program of the Ontario Ministry of Research and Innovation.
Footnotes
Une version française de ce résumé est disponible à l'adresse www.cmaj.ca/cgi/content/full/178/6/715/DC1
Contributors: All of the authors contributed to the conception of this article, the acquisition of data, and drafting and revision of the manuscript. All of the authors provided final approval of the version to be published.
Competing interests: None declared.
Correspondence to: Dr. David N. Fisman, The Hospital for Sick Children Research Institute, Rm. 428, 123 Edward St., Toronto ON M5G 1E6; fax 416 813-5979; david.fisman@sickkids.ca
REFERENCES
- 1.Intergovernmental Panel on Climate Change. Climate change 2007: impacts, adaptation and vulnerability. Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge (UK): Cambridge University Press; 2007.
- 2.Intergovernmental Panel on Climate Change. Climate change 2007: the physical science basis. Contribution of Working Group I to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge (UK): Cambridge University Press; 2007.
- 3.Health Canada. Canada's health concerns from climate change and variability. Ottawa, Ont.: Health Canada; 2007. Available: www.hc-sc.gc.ca/ewh-semt/alt_formats/hecs-sesc/pdf/climat/health_table-tableau_sante_e.pdf (accessed 2008 Jan 16).
- 4.Haines A, McMichael AJ, Epstein PR. Environment and health: 2. Global climate change and health. CMAJ 2000;163:729-34. [PMC free article] [PubMed]
- 5.Allaby M. A dictionary of ecology. 3rd ed. New York: Oxford University Press; 2005.
- 6.Teklehaimanot HD, Schwatrz J, Teklehaimanot A, et al. Alert threshold algorithms and malaria epidemic detection. Emerg Infect Dis 2004;10:1220-6. [DOI] [PMC free article] [PubMed]
- 7.Kuhn K, Campbell-Lendrum D, Haines A, et al. Using climate to predict infectious disease epidemics. Geneva: World Health Organization; 2005. Available: www.who.int/globalchange/publications/infectdiseases/en/index.html (accessed 2008 Jan 16).
- 8.Sultan B, Labadi K, Guegan JF, et al. Climate drives the meningitis epidemics onset in west Africa. PLoS Med 2005;2:e6. [DOI] [PMC free article] [PubMed]
- 9.Pascual M, Bouma MJ, Dobson AP. Cholera and climate: revisiting the quantitative evidence. Microbes Infect 2002;4:237-45. [DOI] [PubMed]
- 10.Lopez AD, Mathers CD, Ezzati M, et al. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. Lancet 2006;367:1747-57. [DOI] [PubMed]
- 11.Sutherst RW. Global change and human vulnerability to vector-borne diseases. Clin Microbiol Rev 2004;17:136-73. [DOI] [PMC free article] [PubMed]
- 12.Altizer S, Dobson A, Hosseini P, et al. Seasonality and the dynamics of infectious diseases. Ecol Lett 2006;9:467-84. [DOI] [PubMed]
- 13.Ogden NH, Maarouf A, Barker IK, et al. Climate change and the potential for range expansion of the Lyme disease vector Ixodes scapularis in Canada. Int J Parasitol 2006;36:63-70. [DOI] [PubMed]
- 14.Randolph SE. The shifting landscape of tick-borne zoonoses: tick-borne encephalitis and Lyme borreliosis in Europe. Philos Trans R Soc Lond B Biol Sci 2001;356:1045-56. [DOI] [PMC free article] [PubMed]
- 15.de Sousa R, Luz T, Parreira P, et al. Boutonneuse fever and climate variability. Ann N Y Acad Sci 2006;1078:162-9. [DOI] [PubMed]
- 16.Casimiro E, Calheiros J, Santos FD, et al. National assessment of human health effects of climate change in Portugal: approach and key findings. Environ Health Perspect 2006;114:1950-6. [DOI] [PMC free article] [PubMed]
- 17.Russell RC. Mosquito-borne arboviruses in Australia: the current scene and implications of climate change for human health. Int J Parasitol 1998;28:955-69. [DOI] [PubMed]
- 18.Woodruff RE, McMichael T, Butler C, et al. Action on climate change: the health risks of procrastinating. Aust N Z J Public Health 2006;30:567-71. [DOI] [PubMed]
- 19.Epstein PR West Nile virus and the climate. J Urban Health 2001;78:367-71. [DOI] [PMC free article] [PubMed]
- 20.Zucker JR. Changing patterns of autochthonous malaria transmission in the United States: a review of recent outbreaks. Emerg Infect Dis 1996;2:37-43. [DOI] [PMC free article] [PubMed]
- 21.Angelini R, Finarelli AC, Angelini P, et al. Chikungunya in north-eastern Italy: a summing up of the outbreak. Euro Surveill 2007;12:E071122. 2. Available: www.eurosurveillance.org/ew/2007/071122.asp#2 (accesed 2008 Jan 15). [DOI] [PubMed]
- 22.Travel by Canadians to foreign countries, top 15 countries visited (2006). Ottawa: Statistics Canada; 2007. Available: www40.statcan.ca/l01/cst01/arts37a.htm (accessed 2008 Jan 16).
- 23.Freedman DO, Weld LH, Kozarsky PE, et al. Spectrum of disease and relation to place of exposure among ill returned travelers. N Engl J Med 2006;354:119-30. [DOI] [PubMed]
- 24.Patz JA, Olson SH. Malaria risk and temperature: influences from global climate change and local land use practices. Proc Natl Acad Sci U S A 2006;103:5635-6. [DOI] [PMC free article] [PubMed]
- 25.Suh KN, Kain KC, Keystone JS. Malaria. CMAJ 2004;170:1693-702. [DOI] [PMC free article] [PubMed]
- 26.Reiter P, Lathrop S, Bunning M, et al. Texas lifestyle limits transmission of dengue virus. Emerg Infect Dis 2003;9:86-9. [DOI] [PMC free article] [PubMed]
- 27.US Centers for Disease Control and Prevention. Mosquito-transmitted malaria — Michigan, 1995. MMWR Morb Mortal Wkly Rep 1996;45:398-400. [PubMed]
- 28.Outbreak news. Malaria, Jamaica. Wkly Epidemiol Rec 2007;82:49. [PubMed]
- 29.Kamat V. Resurgence of malaria in Bombay (Mumbai) in the 1990s: a historical perspective. Parassitologia 2000;42:135-48. [PubMed]
- 30.Hjelle B, Glass GE. Outbreak of hantavirus infection in the Four Corners region of the United States in the wake of the 1997–1998 El Niño-southern oscillation. J Infect Dis 2000;181:1569-73. [DOI] [PubMed]
- 31.Verity R, Prasad E, Grimsrud K, et al. Hantavirus pulmonary syndrome in northern Alberta, Canada: clinical and laboratory findings for 19 cases. Clin Infect Dis 2000;31:942-6. [DOI] [PubMed]
- 32.Engelthaler DM, Mosley DG, Cheek JE, et al. Climatic and environmental patterns associated with hantavirus pulmonary syndrome, Four Corners region, United States. Emerg Infect Dis 1999;5:87-94. [DOI] [PMC free article] [PubMed]
- 33.Kolivras K, Comrie A. Climate and infectious disease in the southwestern United States. Prog Phys Geogr 2004;28:387-98.
- 34.MacKenzie WR, Schell WL, Blair KA, et al. Massive outbreak of waterborne cryptosporidium infection in Milwaukee, Wisconsin: recurrence of illness and risk of secondary transmission. Clin Infect Dis 1995;21:57-62. [DOI] [PubMed]
- 35.Charron D, Thomas M, Waltner-Toews D, et al. Vulnerability of waterborne diseases to climate change in Canada: a review. J Toxicol Environ Health A 2004;67:1667-77. [DOI] [PubMed]
- 36.Auld H, MacIver D, Klaassen J. Heavy rainfall and waterborne disease outbreaks: the Walkerton example. J Toxicol Environ Health A 2004;67:1879-87. [DOI] [PubMed]
- 37.Bowman C, Flint J, Pollari F. Canadian integrated surveillance report: Salmonella, Campylobacter, pathogenic E. coli and Shigella, from 1996 to 1999. Can Commun Dis Rep 2003;29(Suppl 1):i-vi, 1-32. [PubMed]
- 38.Fisman DN, Lim S, Wellenius GA, et al. It's not the heat, it's the humidity: wet weather increases legionellosis risk in the greater Philadelphia metropolitan area. J Infect Dis 2005;192:2066-73. [DOI] [PubMed]
- 39.Currie BJ, Jacups SP. Intensity of rainfall and severity of melioidosis, Australia. Emerg Infect Dis 2003;9:1538-42. [DOI] [PMC free article] [PubMed]
- 40.Rodo X, Pascual M, Fuchs G, et al. ENSO and cholera: a nonstationary link related to climate change? Proc Natl Acad Sci USA 2002;99:12901-6. [DOI] [PMC free article] [PubMed]
- 41.US Centers for Disease Control and Prevention. Vibrio illnesses after Hurricane Katrina—multiple states, August–September 2005. MMWR Morb Mortal Wkly Rep 2005;54:928-31. [PubMed]
- 42.Fisman DN. Seasonality of infectious diseases. Annu Rev Public Health 2007;28:127-43. [DOI] [PubMed]
- 43.Choi KM, Christakos G, Wilson ML. El Niño effects on influenza mortality risks in the state of California. Public Health 2006;120:505-16. [DOI] [PubMed]
- 44.Viboud C, Pakdaman K, Boelle P. et al. Association of influenza epidemics with global climate variability. Eur J Epidemiol 2004;19:1055-9. [DOI] [PubMed]
- 45.Morris SK, Brophy J, Richardson SE, et al. Blastomycosis in Ontario, 1994–2003. Emerg Infect Dis 2006;12:274-9. [DOI] [PMC free article] [PubMed]
- 46.Kidd SE, Chow Y, Mak S, et al. Characterization of environmental sources of the human and animal pathogen Cryptococcus gattii in British Columbia, Canada and the Pacific Northwest of the United States. Appl Environ Microbiol 2007;73:1433-43. [DOI] [PMC free article] [PubMed]
- 47.Parkinson AJ, Butler JC. Potential impacts of climate change on infectious diseases in the Arctic. Int J Circumpolar Health 2005;64:478-86. [DOI] [PubMed]
- 48.Schellenberg RS, Tan BJ, Irvine JD, et al. An outbreak of trichinellosis due to consumption of bear meat infected with Trichinella nativa, in 2 northern Saskatchewan communities. J Infect Dis 2003;188:835-43. [DOI] [PubMed]
- 49.Somily A, Robinson JL, Miedzinski LJ, et al. Echinococcal disease in Alberta, Canada: more than a calcified opacity. BMC Infect Dis 2005;5:34. [DOI] [PMC free article] [PubMed]
- 50.O'Connor DR. The physical causes of the contamination. Report of the Walkerton Inquiry, Part One: The Events of May 2000 and Related Issues. Toronto, Ontario, Canada: Queens Printer for Ontario for the Ontario Ministry of the Attorney General., 2002:103–179. Available: www.attorneygeneral.jus.gov.on.ca/english/about/pubs/walkerton/part1/WI_Chapter_04.pdf (accessed 2008 Feb 5).


