Abstract
Positioning of the surgical patient is an important part of anesthesia care and attention to the physical and physiological consequences of positioning can help prevent serious adverse events and complications. The general principles of patient positioning of the anesthetized and awake neurosurgical patient are discussed in this chapter.
I. General Principles
Ideal patient positioning involves balancing surgical comfort, against the risks related to the patient position. Therefore, patient positioning during surgery should be considered during the preoperative evaluation. (1)
Patient positioning is typically attended to after induction of general anesthesia and placement of arterial and venous lines. Positioning is the joint responsibility of the surgeon and anesthesiologist. Positioning of the neurosurgical patient is challenging and requires adequate anesthetic depth, maintenance of hemodynamic stability, evidence of appropriate oxygenation, and preservation of invasive monitors. Disconnection of intravenous or arterial catheters and tracheal tube during body positioning and during rotation/movement of the operating table is often required, sometimes creating a complete “blackout” state, when the patient may not be monitored or oxygenated. (2) This is especially dangerous in trauma patients who are at risk of thromboembolism and in patients with hemo/pneumothoraces who are dependent on functioning chest tubes. Therefore, pulse oximetry and blood pressure should be monitored throughout positioning, whenever possible, and chest tubes should not be clamped. Specifically, positioning of the head and neck requires special attention. Positioning of the body should be based on general guidelines according to the Practice Advisory of American Society of Anesthesiologists. (1) (Table 1)
Table 1.
Summary of Specific Physiological Changes and Risks and Benefits with Positioning for Neurosurgical Procedures.
| Cardiovascular | Respiratory | Central nervous | Benefits | Risks | |
|---|---|---|---|---|---|
| Supine | Compared to upright, awake and anesthetized: | Compared to upright: FRC ↓, TLC ↓ atelectasis of the dependent lung zones; | Compared to upright: | The easiest position | Often needs head flexion/extention/rotation Ulnar and peroneal nerve injury |
| VR ↑, SV ↑, CO ↑ | Qs/Qt ↑ | JVF ↑ ↔ | |||
| HR ↓ | V/Q mismatch ↑ | JVR ↓ ↔ | |||
| SVR ↓ | CPP ↔ ↓ | ||||
| SBP ↔, MAP↓↔ | CSF drainage may be impaired | ||||
| Modifications: a)lawn-chair b)reverse Trendelenbourg | Improvement of the VR from the lower extremities | Improvement of ventilation of the dependent lung zones | Improvement of the cerebral venous, lymphatic and CSF drainage. | ||
| Lateral | Compared to supine, anesthetized: | Compared to supine: | Compared to supine: | Optimal approach to the temporal lobe | Brachial plexus injury |
| VR ↓, SV ↓, CO↓ | FRC ↓, TLC ↓ | JVF↑↔ | Ear and eye injury | ||
| HR↑ ↔ | Qs/Qt ↑↑ | JVR↓↔ | Suprascapular nerve injury (of the dependent shoulder) | ||
| SVR↑, PVR↑ | V/Q mismatch ↑↑ atelectasis of the dependent lung | with neck flexion: | |||
| SBP↓, MAP↓ | JVF↓, JVR↑, ICP↑ | ||||
| Modification: park-bench | Stretch injuries (axillary trauma) Decreased perfusion to the dependent arm | ||||
| Prone | Compared to supine, awake: | Compared to supine: increase in upper airway resistance (Wilson frame and chest rolls) | Compared to supine: a) neutral to the heart | Optimal posterior approach to spine Less risk for VAE (compared to sitting) | The most difficult position Difficult access to airway Pressure sores of soft tissues Eye injury Blindness Bleeding (compared to sitting) |
| VR↓, SV↓ | |||||
| HR↑ ↔ | JVF ↑ ↔ | ||||
| SVR↑, PVR↑ | FRC↑ ↔, TLC↑ ↔ | JVR↓ ↔ | |||
| SBP↑↔, MAP↑↔ | V/Q mismatch ↓ | b) lower than heart | |||
| In anesthetized patient: | less atelectasis in lungs | JVF↑, JVR↓, venous congestion | |||
| VR↓, SV↓, CO↓↔ | ICP↑ | ||||
| HR↑, SVR↑, PVR↑ | |||||
| SBP↓↔, MAP↓↔ | |||||
| Modification: Concorde | Neck and head hyperflexion: venous congestion of the face, nose, and tongue, epystarchis, chin necrosis, cerebral venous obstruction, increase of ICP, quadriplegia | ||||
| Sitting | Compared to supine, awake: | Compared to supine: | Compared to supine: | Optimal approach to posterior fossa Low ICP | Venous air embolism (VAE) Paradoxical air embolism Arterial Hypotension |
| VR ↓, SV ↓, CO↓ | TLC ↑, FRC ↑ | JVF ↓, JVR ↑ | |||
| Qs/Qt↓ | ICP↓↓ | ||||
| HR↑, SVR↑, PVR↑ | V/Q mismatch ↓ | CPP ↔ | Minimal bleeding (compared to prone) Access to airway | Pneumocephalus Paraplegia, Quadriplegia Macroglossia | |
| SBP↑↔↓, MAP↓ ↔↑ | less atelectasis in lungs | Good cerebral venous and CSF drainage | |||
| In anesthetized patient: | |||||
| VR↓↓, SV↓, CO↓ | |||||
| HR↑, SVR↑, PVR↑ | |||||
| SBP↓, MAP↓ | |||||
| Three - quarters | different changes, resemble lateral or prone | changes, resemble lateral or prone | different changes, resemble lateral or prone | Less risk for VAE (compared to sitting) Better access to airway (compared to prone) | Difficult position Brachial plexus injury Pressure sores Compartment syndrome of the dependent upper extremity Pudendal nerve injury |
Changes of physiologic parameters in cardiovascular, respiratory and central nervous system are presented as observed in anesthetized subjects, changes in cardiovascular system presented in awake and anesthetized subjects: HR- heart rate, SV-stroke volume, VR – venous return, CO-cardiac output, SBP- systolic blood pressure, TLC- total lung capacity, FRC- functional residual capacity, Qs/Qt – intrapulmonary shunt, V/Q mismatch- ventilation/perfusion mismatch, ICP- intracranial pressure, JVF – jugular venous flow, JVR – jugular venous resistance, CPP- cerebral perfusion pressure; ↑- increase, ↓ - decrease, ↔ no change.
II. Head Positioning
Patient positioning for craniotomies and the majority of spine procedures begins with positioning of the head. Knowledge of the neurosurgical approach to head positioning is important for anesthesiologists since we should evaluate whether the patient can tolerate the desired intraoperative positioning, particularly during long procedures.
The ideal position of the head is the position that provides optimal surgical approach to the target brain area and is based on the two principles: 1) An imaginary trajectory from the highest point at the skull surface to the area of interest in the brain should be the shortest distance between the 2 points, and 2) Whenever possible, the exposed surface of the skull and an imaginary perimeter of craniotomy should be parallel to the floor.(3)
A. Types of Craniotomies
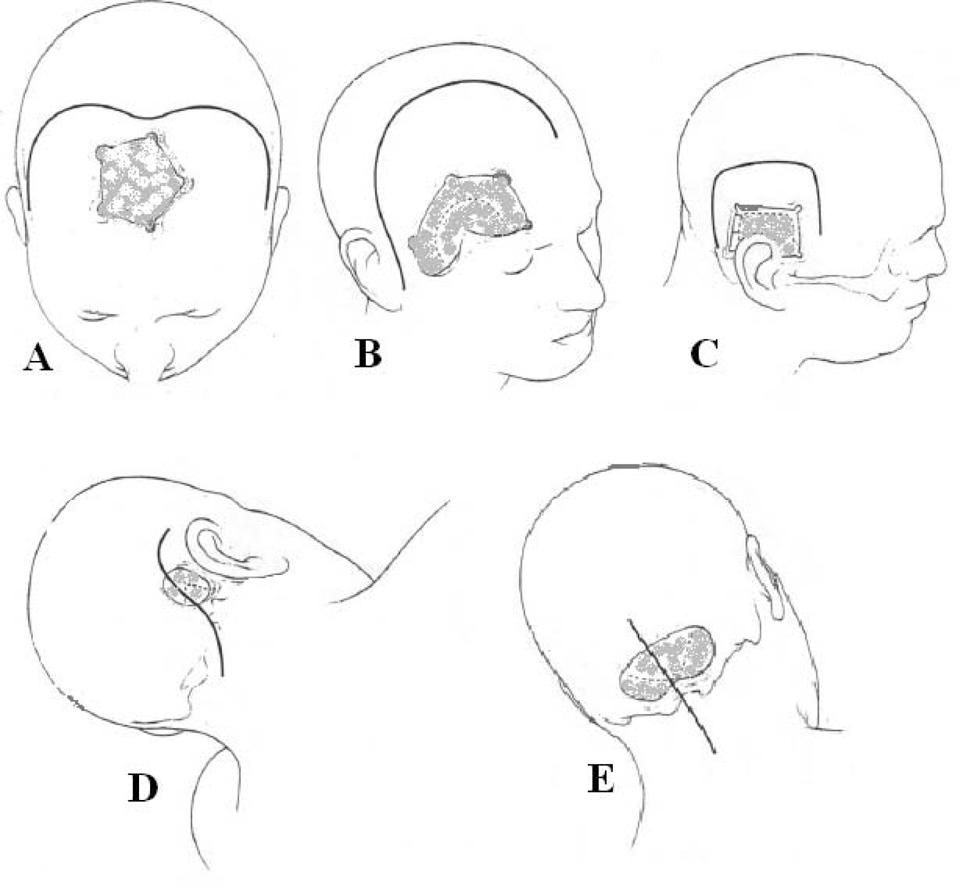
There are 5 classic surgical approaches for craniotomies: frontal, temporal, occipital, parietal, and posterior fossa. These approaches provide extensive “regional” exposure of the entire lobes and are currently used occasionally when exposure of large areas is required (e.g. decompressive craniectomy). In modern neurosurgery, 6 standard types of craniotomies, derived from the regional craniotomies by miniaturization of the area of exposure and/or combination of their different parts, are used: 1) anterior parasagittal, 2) frontosphenotemporal (pterional), 3) subtemporal 4) posterior parasagittal, 5) midline suboccipital, and 6) lateral suboccipital. (Figure 1) (3)
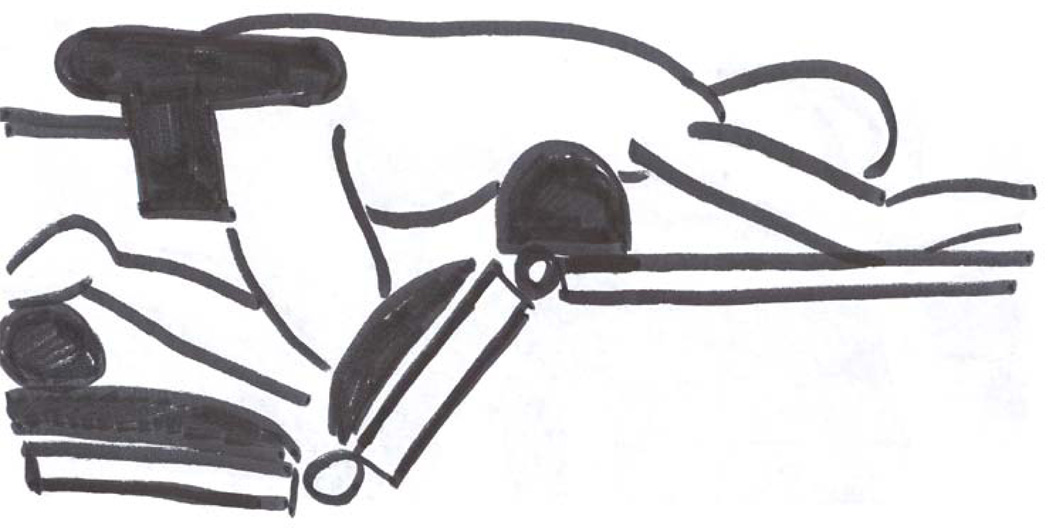
Figure 1.
Types of Standard Craniotomies. (Modified with permission from Youmans Neurological Surgery, Fifth Edition, pp 626–630 (1)).
1-A. Anterior Parasagittal craniotomy is a miniaturization of the frontal regional craniotomy along the midline.
1-B. Frontosphenotemporal craniotomy is a combination of two regional craniotomies: anterior-inferior portion of the frontal regional craniotomy with the anterior portion of the temporal regional craniotomy.
1-C. Subtemporal craniotomy is a miniaturization of the temporal regional craniotomy along with the middle fossa floor.
1-D. Lateral Suboccipital craniotomy is a miniaturization of the posterior fossa regional craniotomy along with the midportion of cerebellum.
1-E. Midline Suboccipital craniotomy is a miniaturization of the frontal regional craniotomy along the midline.
B. Fixation of the Head
For craniotomies or burr holes, the head can be positioned on the horseshoe headrest (or doughnut), or skeletally fixed with the three or four-pins fixation device. The Mayfield frame is a three-pin device which is used for fixation during craniotomies, and a four-pin rigid frame is usually used for burr holes and functional neurosurgical procedures (e.g., implantation of deep brain stimulators). For prone positioning, the head may be positioned on a foam pillow, headrest, or fixed with the Mayfield frame.
Application of a skeletal fixation device and tightening of pins on the scalp has a profound stimulating effect, leading to tachycardia and hypertension. Since severe hypertension during pin fixation may cause rupture of untreated cerebral aneurysms, pins may be placed only after the anesthesia team has preempted the hemodynamic effects of fixation. Local infiltration of the skin should be used whenever possible in every awake as well as in the anesthetized patient, and the dose of local anesthetic should be recorded. In patients under general anesthesia, anesthesia should be deepened with either a bolus of intravenous anesthetic agent (e.g. propofol 0.5–1 mg/kg) or with deepening of the inhalational anesthetic. The dose of the anesthetic given should be titrated to the estimated depth of anesthesia and arterial blood pressure. Therefore, standard monitoring and invasive blood pressure monitoring should have commenced before application of pins. In cases when invasive blood pressure monitoring is unavailable (e.g. during an emergency such as head trauma), a bolus of an anesthetic agent should be given before application of pins, titrated to the noninvasive blood pressure value.
Benefits of the skeletal head holder consist of immobility of the head, and surgical comfort. Risks of the head holder include bleeding from the pins sites, air embolism (especially in sitting position, where placement of antibiotic ointment on pins is advocated for prevention of air embolism), and scalp and eye laceration. Pressure alopecia has been described after using a horseshoe headrest. (4)
C. Head and Neck positioning: Head Rotation, Hyperflexion, Hyperextension, and Lateral Flexion
Manipulation of the head and neck during positioning may have serious consequences, including quadriplegia and cerebral infarction. Even in healthy individuals, slight movement of the head and neck may lead to mechanical stress of arteries and veins supplying brain and cervical spinal cord. (5) Blood flow in the vertebral arteries, which are located in the narrow foramina in the transverse processes along the cervical spine, decreases on the side ipsilateral to the direction of head turning. Hyperflexion of the head and neck may decrease blood flow in vertebral and carotid arteries, leading to brain stem and cervical spine ischemia, resulting in quadriparesis and quadriplegia. Patients with osteophytes, arthritis, or vascular atherosclerosis also are at risk for cerebral ischemia secondary to inappropriate head and neck movement. (6) During positioning, the head can typically be safely rotated between 0 – 45 degrees away from the body. If more rotation is needed, a roll or pillow placement under the opposite shoulder is recommended. (4) Maintaining 2–3 finger-breadths thyromental distance is recommended during neck flexion. The patient’s preoperative ability to move the neck without neurological consequences such as paresthesias, pain, or dizziness may limit or dictate the extent of intraoperative head and neck positioning. Hyperflexion, hyperextension, lateral flexion or rotation should be avoided.
Benefits include surgical comfort and optimal access to the target area. Risks and complications of head positioning include: cervical strain leading to postoperative discomfort and pain, necrosis of the chin, brachial plexus injury, obstruction of the cerebral lymphatic and venous outflow, leading to face, neck, and airway swelling, macroglossia leading to the airway obstruction, obstruction of cerebro-spinal fluid flow, and obstruction of vertebral or carotid arteries leading to the brain stem ischemia and quadriplegia. Impairment of cerebral venous outflow, especially during prolonged surgery, can potentially cause intraoperative brain swelling, increased intracranial pressure (ICP), ischemia and cerebral infarction. (7) Jugular veins and vertebral venous plexuses are the major venous pathways from the brain. Because jugular veins tend to collapse with change of the body position (e.g. in sitting position), (8) vertebral venous drainage may predominate. (9) Collapse or obstruction of jugular veins, and stretching or obstruction of the vertebral venous plexus should be avoided during head and neck positioning.
D. Monitoring during head positioning
First, since increase in ICP can reflect impaired venous drainage, measuring intracranial pressure (ICP) can be helpful during head positioning. In patients with in-situ ICP monitoring, we recommend monitoring ICP, with the goal of maintaining normal ICP < 20 mmHg. Repositioning to achieve a normal ICP may be needed. Second, jugular bulb pressure (JBP) monitoring is an alternative to direct ICP monitoring. Jugular bulb pressure and jugular venous saturations can both be measured using a retrograde jugular bulb catheter. Monitoring JBP allows the anesthesiologist to continuously measure and record intracranial venous pressure and compare it to central venous pressure (CVP). When CVP and JBP are measured and monitored continuously, obstruction of jugular vein can be quickly recognized (JBP exceeds CVP). If the patient is supine, and pressure transducers are placed at the level of the heart, JBP and CVP are usually equal, or JBP may be higher by 1–2 cmH2O. During head up tilt, placement of the pressure transducers should be considered. If both transducers are placed at the same level (usually at the ear tragus to reflect middle cerebral artery pressure), JBP will be higher than CVP; with head-down tilt, JBP is lower than CVP. If each transducer is placed near its reference level (CVP at the level of the right atrium, and JBP at the level of tragus), there should be no change in pressures compared to baseline. The most important sign of proper head positioning is that JBP remains the same. Any elevation of JBP requires evaluation. Once technical errors are excluded (check for kinking of the catheter, flush the catheter), partial obstruction of venous outflow, and repositioning of the head should be considered.
III. Body Positioning
There are six basic body positions utilized in neurological surgery: supine, lateral, prone, concorde, sitting, and three-quarters. Additionally, there are significant circulatory and respiratory changes with changes in body position in both awake and anesthetized patients. These changes may affect blood-gas exchange and cerebral hemodynamics. The most significant physiologic changes and benefits and risks with different body positions utilized in neurosurgery are summarized in Box 2.
A. Supine Position (Dorsal Decubitus Position)
The supine position is the most frequently utilized position in neurosurgery and is used for cranial procedures, carotid endarterectomies, and for anterior approaches to the cervical and lumbar spine. (Figures 2A–C) Benefits: This is the simplest position because it does not require special instrumentation, is easily achievable, and usually does not require disconnection of the tracheal tube and invasive monitors. Risks: Head rotation or flexion is often required for in order to create optimal surgical conditions.
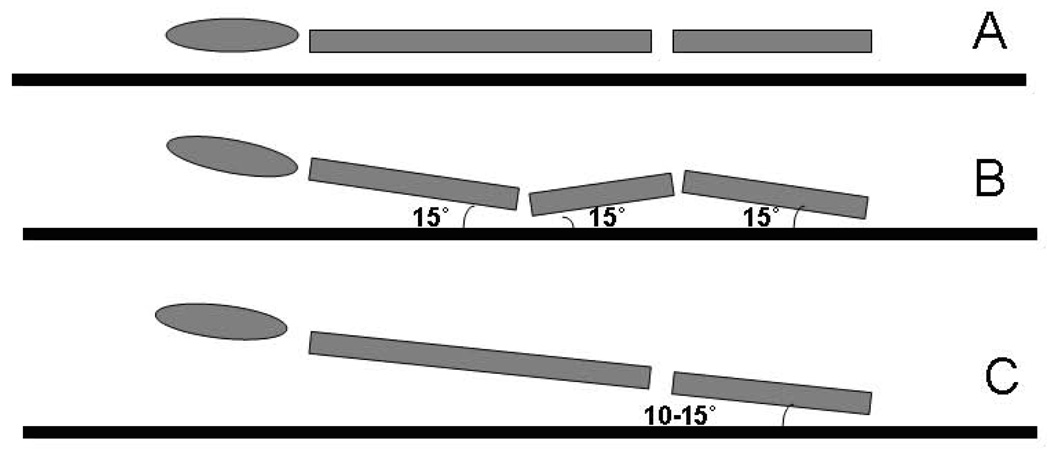
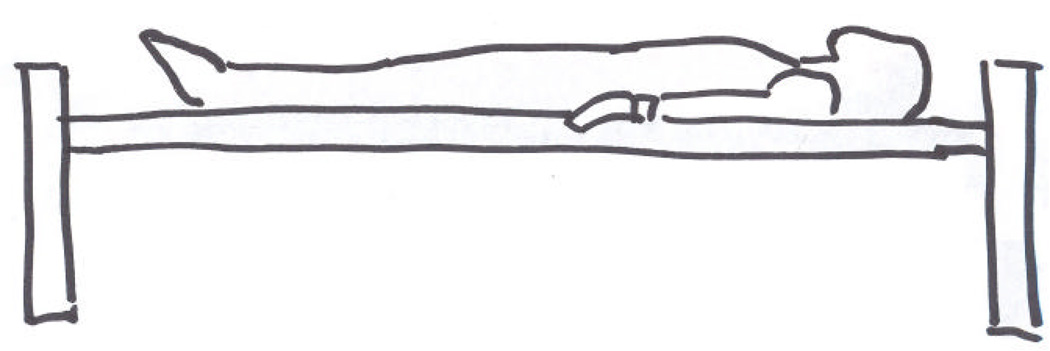
Figure 2.
Types of supine_positioning. A- horizontal position, B - lawn chair (contoured) position, C - reverse Trendelenbourg position.
There are 3 types of supine positioning utilized in neurosurgery. The horizontal position (Figure 2-A) is achieved when patient is lying on his/her back on a straight table. This position does not provide optimal positioning of the hip and knee joint and is poorly tolerated even for a short time by awake patients. Skin to metal contact should prevented and arms must be padded or restrained along the body or positioned on arm boards. Bony contact points at elbows and heels should be padded. The lawn chair (contoured) position (Figure 2-B) is a modification of the horizontal position with 15 degree angulation and flexion at the trunk-thigh-knee and provides more physiological positioning of the lumbar spine, hips and knees. A blanket, soft (gel) cushion or pillow can be placed under the knees to keep them flexed. The other advantage of lawn chair position includes a slight head elevation with improvement of venous drainage from the brain and a slight elevation of legs, which can improve venous return to the heart. The head-up tilt or reverse Trendelenbourg position (Figure 2-C) usually involves a 10–15 degree repositioning from the horizontal axis to provide optimal venous drainage from the brain.
Hemodynamics and Ventilation. Since each 2.5 cm change of vertical height from the reference point at the level of the heart leads to a change of mean arterial pressure by 2 mmHg in the opposite direction (10), and since the venous compartment is a low pressure compartment, venous return to the heart depends on body position. Head-down tilt increases venous return from the lower extremities, but increases venous congestion in the upper part of the body. If the head is tilted below the level of the heart, venous pressure in the cerebral veins increases in proportion to the hydrostatic pressure gradient. Even after short procedures, postoperative headache, congestion of the conjunctivae and nasal mucosa may be observed. Therefore, to improve venous drainage from the brain, the head should be positioned above the level of the heart using reverse Trendelenbourg positioning or with flexion of the table. The head can typically be safely rotated to 45 degrees relative to the body, but if more rotation is needed, a roll or pillow should be placed under the contralateral shoulder.
In awake subjects, change in body position does not usually cause profound changes in blood pressure because of the baroreceptor (from aortic arch and carotid sinus) reflexes and renin-angiotensin-aldosterone system. During anesthesia, hemodynamic instability may develop due to impaired compensatory mechanisms and effect of anesthetic agents. (11) Adverse hemodynamic changes are not common in supine positioning.
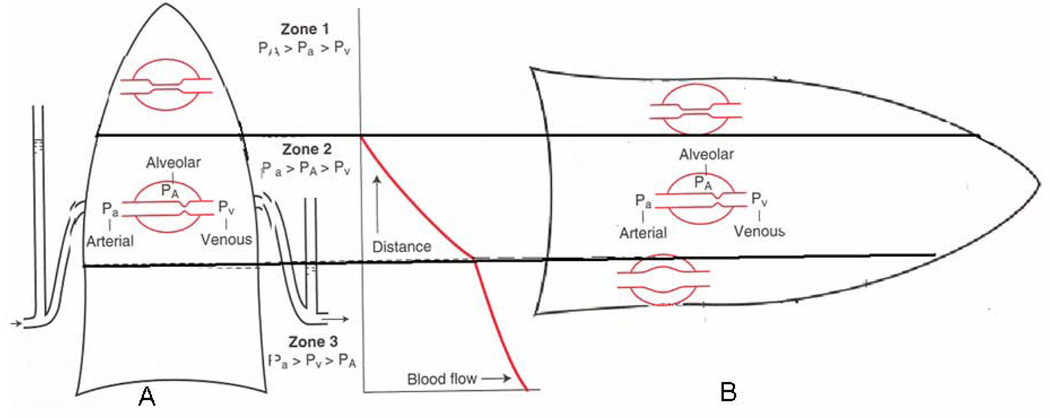
Pulmonary blood flow may change profoundly with changes in patient position. (12) Perfusion and ventilation are best in the dependent parts of the lungs. (Figure 3) In anesthetized patients, positive-pressure ventilation provides the best ventilation to the non-dependent lung zones. During head-up tilt, ventilation of the dependent lung is improved by displacement of the abdominal viscera downward from the diaphragm.
Figure 3.
West zones of the lungs (Modified with permission from West et al., J Appl Physiol 1964;19:713–24 (2)).
This is a schematic presentation of the ventilation-perfusion relationships in the lungs, which shows dependency of the venous pressure on the gravity. Perfusion in the lungs is established in the zone 3, at the point when venous pressure overcomes alveolar pressure. A – upright position, B- supine position. Pa – arterial pressure, PA - alveolar pressure, PV – venous pressure
B. Lateral Position
The lateral position is used for surgical approach for patients requiring temporal lobe craniotomy, skull base and posterior fossa procedures, as well as for the retroperitoneal approach to thoracolumbar spine. (Figure 4) Benefits: This position provides the best surgical approach to the temporal lobe. Risks: Brachial plexus injuries, stretch injuries, pressure palsies, and ventilation-perfusion mismatch may occur. Hemodynamics and Ventilation. Lateral positioning leads to gravitational changes of ventilation-perfusion relationship in the lung. The best perfusion occurs in the dependent lung zones. In an awake patient in lateral position, Zone 3 West is occupying the dependent 18 cm of lung tissue. Lung tissue above 18 cm from bed level is not perfused. (13) (Figure 3) During general anesthesia and positive pressure ventilation, the non-dependent lung zones are ventilated better relative to the dependent zones, worsening ventilation-perfusion mismatch.
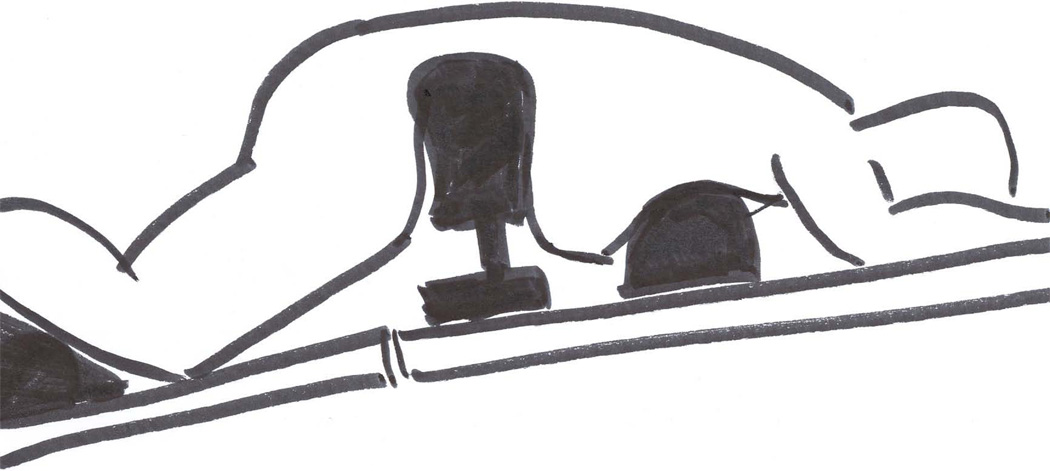
Figure 4.
Lateral positioning (Adapted with permission from Youmans Neurological Surgery, Fifth Edition, pp 559, 601(3)).
A- dependent arm is hung under the operating table, an upper arm is placed on the arm board, B – dependent arm is positioned on the operating table and an arm board, an upper arm is placed over the trunk on the pillow.
Special attention is required for positioning of the patient’s dependent (lower) arm because of the potential danger of axillary artery compression and brachial plexus injury. The dependent arm can be positioned in hanging or ventral position and may be rested on a low padded arm board, inserted between the table and head fixator. Alternatively, the forearm can be hung on a pillow and towels wrapped over the arm and forearm. The shoulder should be abducted, and the elbow flexed. An axillary roll, inflatable pillow or a gel pad should be placed under the upper chest (not directly in the axilla) in order to take pressure off of the dependent shoulder and prevent arm ischemia, brachial plexus injury, and compartment syndrome. It is also critical to support the patient’s head with a pillow or gel pad in order to minimize angulation of the cervical spine, what may be achieved with the simultaneous inflation of the both inflatable pillows under the chest and the head. (14) If there is no arterial line, palpation of radial pulse of the dependent forearm can be helpful in verifying optimal positioning. The nondependent (upper) arm may be positioned on the “airplane” armrest or on a pillow placed anterior to the patient’s body
The Park-bench position is a modification of lateral position and provides the surgeon with better access to the posterior fossa, as compared to the lateral position. The upper arm is positioned along the lateral trunk and the upper shoulder is taped towards the table. The lower extremities should be slightly flexed, and a pillow should be placed between the legs (particularly the knees). Reverse Trendelenbourg and marked flexion of the legs at hips and knees should be avoided, as it can lead to the lower extremity venous stasis and decrease of venous return to the heart. Leg wrapping with compression bandages can be used to prevent venous pooling.
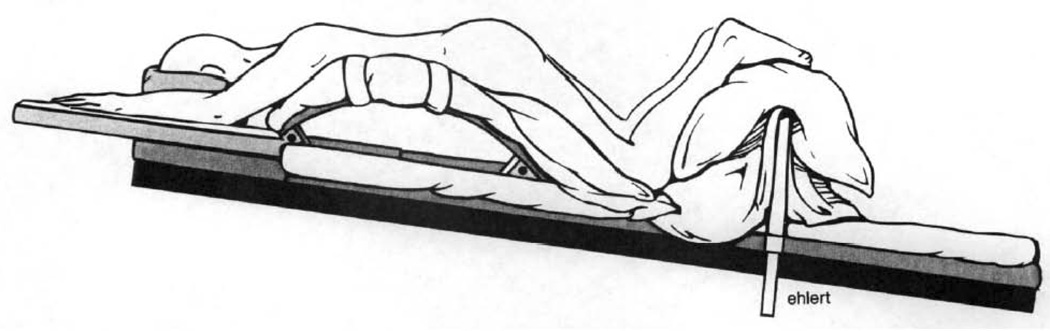
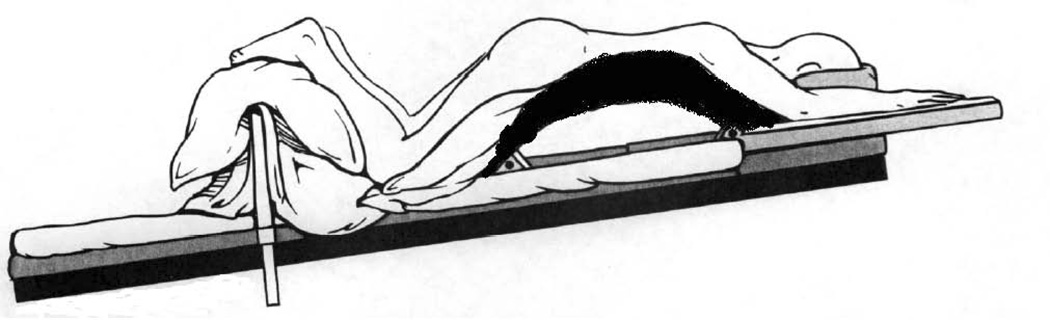
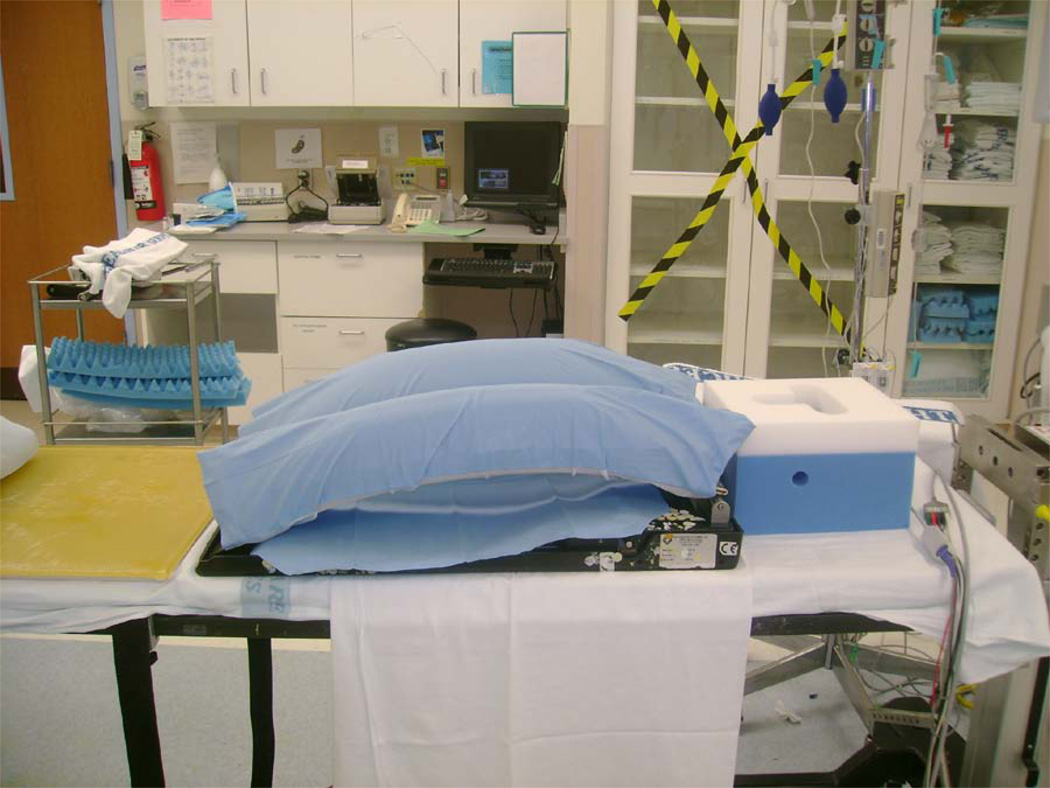
C. Prone Position
The prone position is commonly utilized for approaches to the posterior fossa, suboccipital region and posterior approaches to spine. (Figure 5) Benefits: This is a good position for posterior approaches, and there is a lower incidence of venous air embolism compared to the sitting position. Risks: This is the logistically the most difficult positioning due to challenges associated with providing adequate oxygenation, ensuring adequate ventilation, maintaining hemodynamics, and securing intravenous lines and the tracheal tube. Access to the patients’ airway is poor. Pressure sores, vascular compression, brachial plexus injuries, air embolism, blindness, and/or quadriplegia can occur.
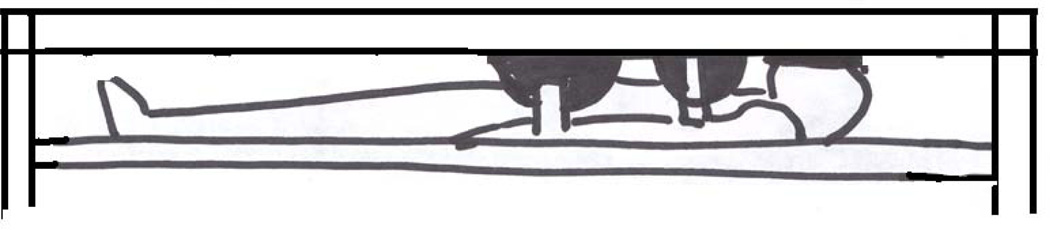
Figure 5.
(A) Prone positioning and the main frames used for spine surgery. Wilson frame. Positioning on the Wilson frame: abdomen is partially compressed, pelvis is partially supported, legs are positioned below the trunk, head is positioned on the pillow (Adapted with permission from Youmans Neurological Surgery, Fifth Edition, pp 559, 601(3)); (B), (C) – Wilson frame.
(D). Andrews frame. Positioning on the Andrews frame: abdomen hangs free, pelvis is partially supported, legs are positioned below the heart, head is positioned on the foam pillow, or headrest; (E) – Andrews frame (OSI ANDREWS SST 3000 model 5820 Spine Surgery Table, Ideal Medical, Monroe, GA, www. idealmedicalequipment.com)
(F). Relton Hall frame. Positioning on the Relton Hall frame: abdomen hangs free, pelvis is supported, legs are positioned below the heart, head is positioned on the foam pillow or headrest; (G) – Relton Hall frame. (Adapted with permission from Relton JE, Hall JE. An operation frame for spinal fusion. A new apparatus designed to reduce hemorrhage during operation. J Bone Joint Surg Br. 1967, 49(2): 327–32)
(H). Jackson table. Positioning on the Jackson table: (I) - step I : the patient is lying on the Jackson table, (J) - step II: Jackson frame is put over the patient, the thoracic pad is adjusted to support shoulders and thoracic cage, 2 side pelvic pads are adjusted to the pelvis, and 2 other side pads are adjusted to support the thighs, the patient is compressed between the table and the frame; (K) - step III: after the flipping into prone position has been completed and the Jackson table has been removed from the patients back, the patient is lying on the Jackson frame: abdomen hangs free, pelvis is supported, legs are supported and are positioned at the heart level, head may be positioned on a foam pillow or headrest, or may be fixed with the Mayfield frame; (L) – Jackson table, (M) – Jackson frame.
Hemodynamics and Ventilation. Turning the patient prone from the supine position increases intraabdominal pressure, decreases venous return to the heart, and increases systemic and pulmonary vascular resistance. (15) With the head-up tilt or in kneeling position with flexed lower extremities, pooling of venous blood in the lower part of the body occurs, decreasing venous return and causing hypotension. (16) Although the cardiovascular responses to turning prone have not been fully characterized, data suggest that left-ventricular ejection fraction and cardiac index may decrease, potentially causing hemodynamic instability. (15 17, 18)
Oxygenation and oxygen delivery, however, may improve with prone positioning because of improved matching of ventilation and perfusion. The relationship between ventilation and perfusion may be improved because: 1) Perfusion of the entire lungs improves (12), 2) Increase in intraabdominal pressure decreases chest wall compliance, which under positive-pressure ventilation, improves ventilation of the dependent zones of the lung, and 3) Previously atelectatic dorsal zones of lungs may open.
Characteristic challenges with prone positioning include disconnection of pulse oximetry, arterial line, and tracheal tube, leading to hypoventilation, desaturation, hemodynamic instability, and altered anesthetic depth. To prevent anesthesia disasters, pulse oximetry and the arterial line should be left connected during the turn, whenever possible. Monitoring of invasive blood pressure is especially important in patients with heart or lung disease and trauma patients. For uncomplicated elective surgeries, when invasive blood pressure monitoring is not used, standard ASA monitoring should be applied.
The patient is usually anesthetized in the supine position, and is then turned prone on a chest rolls or on a special frame. The head should be kept in the neutral position. All catheters, invasive monitors and the tracheal tube should be carefully secured before turning the patient prone. Pressure sores (of breasts, penis, soft tissue at the bone points, ears, eyes) are the most frequent complications of prone positioning (4) Therefore, special frames (e.g. Wilson, Relton-Hall frame, Andrews frame, Jackson table and frame (Figure 5)), which provide support to the chest but leave the abdominal wall and pelvis free, are often used. Chest rolls may be used to support the chest wall, and allow free movement of the chest and abdominal wall. Free movement of the abdominal is desirable for 3 reasons: 1) improved excursion of the diaphragm, and improved oxygenation ventilation, 2) a decrease in intraabdominal pressure and decreased surgical bleeding 3) and improvement of venous return from lower extremities and pelvis. The breast should not be exposed to pressure.
The effects of the prone position on hemodynamic stability and respiratory mechanics are frame dependent. (16, 19–21) Positioning on the Jackson table provides the most stable hemodynamics and does not increase dynamic lung compliance. (19–21)
Eyes, nose, and ears should be protected against pressure, eyelids should be closed. If the head is positioned on a specially designed pillow (with holes for the eyes and nose), the eyes and nose should be periodically checked for lack of pressure (no less than once every 30 minutes) and head should be repositioned if needed. Blindness is a rare (in about 0.2% of cases), but it is a devastating complication of spine surgery during prone position, where prolonged of surgery and the magnitude of the blood loss may be risk factors.(22) Positioning of the head at the body level, or higher, avoiding the head-down position and associated venous congestion. On the other hand, elevation of the head for posterior fossa surgery or cervical spine surgery may increase the risk for air embolism. The upper extremities may be positioned along the body or abducted on to padded armboards. If abduction is used, great care must be exercised to avoid hyperextension of the arms to prevent brachial plexus injury.
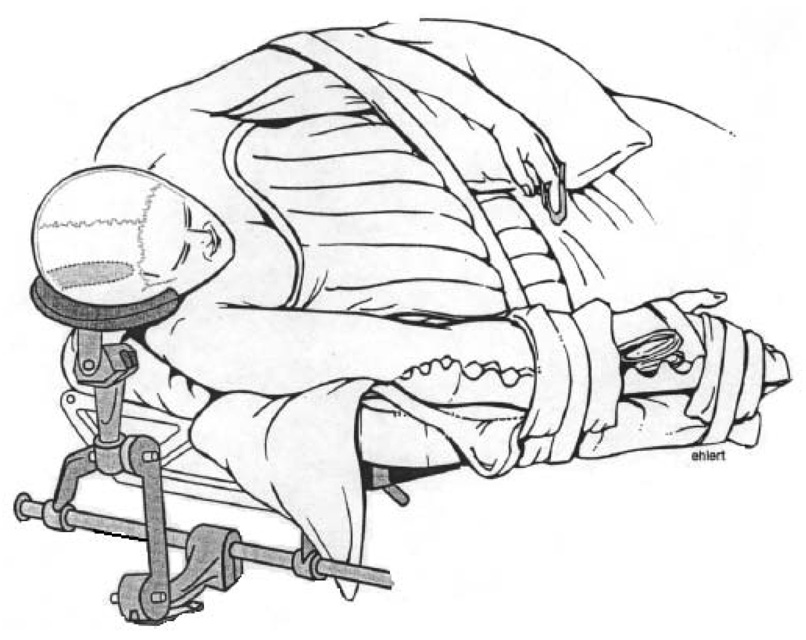
The Concorde position is a modification of the prone position. (Figure 6) This is the best positioning for surgical approach to occipital transtentorial and supracerebellar infratentorial area. The head is typically skeletally fixed and flexed, but may be laterally flexed if needed. The body is positioned in reverse Trendelenburg and chest rolls are placed under the trunk. The arms are tucked alongside to the trunk, and the knees are flexed. Specific complications include necrosis of the chin and an obstruction of cerebral venous outflow.
Figure 6.
Concorde positioning (Adapted with permission from Youmans Neurological Surgery, Fifth Edition, p 604(3)).
The head is flexed, arms are tucked to the trunk, and legs are flexed at the knees.
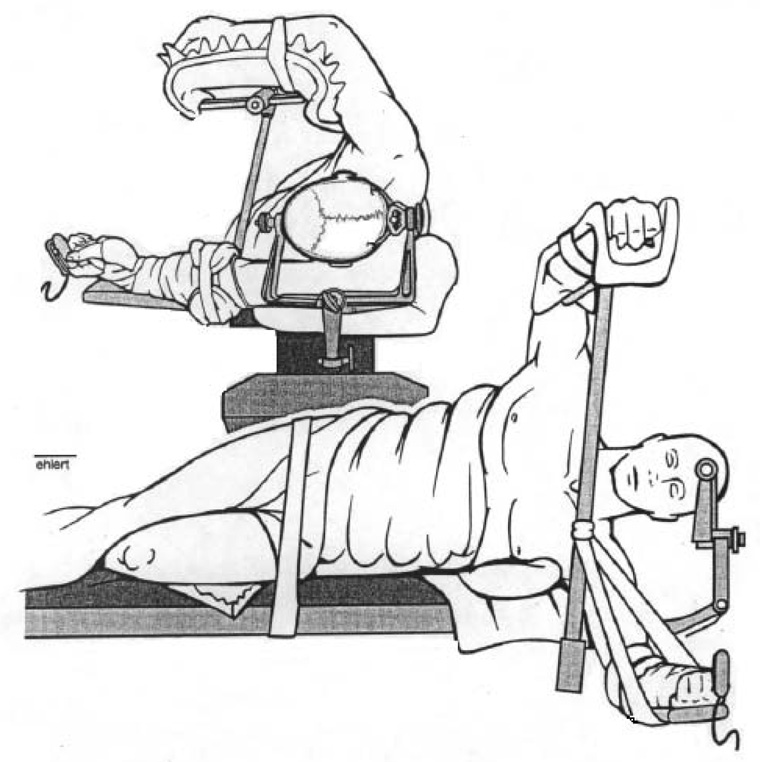
D. Sitting Position
This position is most commonly utilized for posterior fossa surgery and cervical laminectomy. (Figure 7 A,B) Benefits: This position provides optimal surgical exposure for posterior fossa surgery because tissue retraction and risks of cranial nerve damage are reduced, cerebral venous drainage is improved and bleeding is less. The patient’s airway is accessible to the anesthesiologist. Risks: Venous air embolism (VAE), paradoxical air embolism, bradycardia or cardiac arrest due to brain stem manipulations can occur. Macroglossia, upper airway obstruction, (23) pneumocephalus, (24) subdural hematoma, and quadriplegia (25) have also been reported. Despite well described risks involved with the sitting position, there is no evidence of increased mortality rate. (26–28) A recent national survey has demonstrated that the sitting position is still utilized for posterior fossa surgery in about half of practices in USA. (2) Relative contraindications to the sitting position include: open ventriculoatrial shunt, signs of cerebral ischemia when upright and awake, right-to-left shunt as with patent foramen ovale, and cardiac instability.
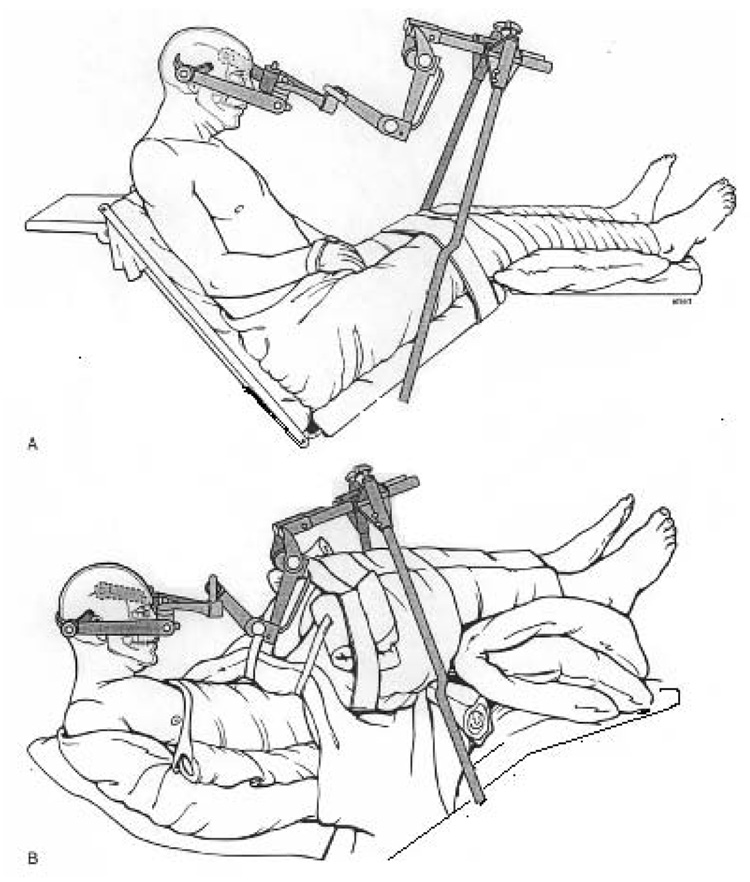
Figure 7.
Sitting positioning (Adapted with permission from Youmans Neurological Surgery, Fifth Edition, p 605(3)).
A – classical sitting position, B- modified (semirecumbent) position.
Hemodynamics and Ventilation. The classic sitting position causes postural hypotension in about 1/3 of patients, and 2–5% of patients suffer severe hypotension (decrease in blood pressure more than by half from baseline). (29) The major hemodynamic consequence is decrease in venous return, leading to decrease in cardiac output and hypotension. Therefore, hemodynamic instability and cardiac disease are relative contraindications for prone positioning. Wrapping of the legs with elastic bandages (e.g. ACE bandage) prevents pooling of blood in the lower extremities and should be applied in every case. The modified sitting (semirecumbent) position provides better venous return and less hemodynamic instability. (Figure 7B) With head-up tilt venous drainage via internal jugular veins is improved which results in decreased intracranial pressure. However, jugular veins may also collapse in sitting position, (8) and careful head positioning to avoid hyperflexion and hyperextension is required to prevent stretching or obstruction of the vertebral venous outflow.
Ventilation in sitting position is improved compared to the supine position due to downward shift of the diaphragm, which decreases intraabdominal pressure, improves ventilation of the dependent zones, and decreases ventilation-perfusion mismatch. However, low perfusion pressure secondary to decreased venous return may affect oxygenation. Therefore, preventing hypovolemia and maintaining normal pulmonary perfusion pressure are crucial for maintaining an adequate oxygen delivery in sitting position.
Venous Air Embolism (VAE)
The mechanisms of VAE include negative venous pressure and exposure of veins and boney venous sinuses to air. When the site of surgery is exposed to air and located above the level of the heart, air may be entrained in the veins and boney venous sinuses, and air may enter the pulmonary circulation. A large VAE may decrease cardiac output by creating an airlock and decreasing left ventricular output. The incidence of VAE in sitting position may approximate 20–50% when precordial Doppler monitoring is used for detection (30) and 76% with transesophageal echocardiography (TEE) is used for detection. (31) Patent foramen ovale should be excluded before every case as it is a source of paradoxical air embolism. Therefore, preoperative “bubble test” in awake patients using TEE or transthoracic echocardiography is advocated by some authors if the sitting position is considered. (32)
In addition to standard monitoring, precordial transthoracic Doppler is recommended for early detection of VAE. (25) Although TEE is more sensitive in detecting VAE, precordial Doppler is inexpensive, readily available, easy to use, and noninvasive. Optimal placement of the precordial probe should be guided by the recognizing the highest pitch over the right upper sternal border with the intravenous injection of agitated saline. When precordial Doppler or TEE are unavailable, VAE should be considered when end tidal CO2 suddenly decreases in the presence of hypotension, not explained by other causes. An atrial catheter (multiorifice or single orifice) placed at the high level of the right atrium may be helpful for air aspiration. Correct positioning may be verified using intravenous electrocardiography, chest radiography, or TEE. However, the therapeutic value of the right atrial catheter may be limited. The most important treatment for VAE include irrigation of the surgical site with saline, rescue head-down tilt or left lateral positioning, and cardiovascular support with administration of inotropes.
Other Complications
The incidence of postoperative pneumocephalus in sitting position may reach 100% (20), and may be due to negative cerebral spinal fluid pressure and/or residual air during closure of the dura. Therefore, nitrous oxide should be discontinued 20–30 minutes before completion of the procedure. However, pneumocephalus can develop even without the use of nitrous oxide and may persist for weeks after surgery. Life-threatening tension pneumocephalus is rare (3%). (28)
Quadriplegia is a rare but devastating complication and results from cervical spine ischemia with neck and head hyperflexion. Elderly patients with cervical spine deformities and vascular pathologies have higher risk. (6) During positioning, sufficient distance betweeen chin and neck (at least 2 finger-breadth) is recommended to avoid neck hyperflexion.
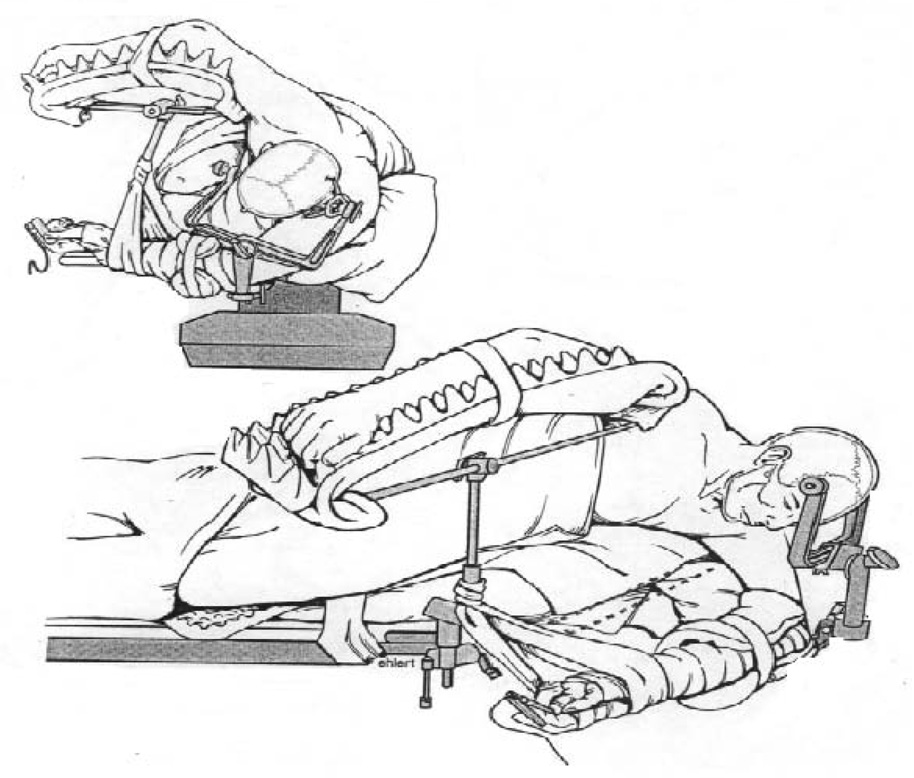
E. Three-Quarter Prone Position (Lateral Oblique, or Semiprone)
This position is used for posterior fossa and parieto-occipital surgery. (Figure 8) Benefits: The risk of VAE is lower compared to the sitting position. Risks include bleeding, brachial plexus injury, pressure sores, and macroglossia. The issues with hemodynamics and ventilation in this position are similar to those with lateral and/or prone positioning.
Figure 8.
Three-quarters (lateral oblique) positioning (Adapted with permission from Youmans Neurological Surgery, Fifth Edition, p 608).
The principles of three-quarter positioning resemble those for lateral position, but the head may be placed on the table and the dependent (lower) arm may be placed behind the body (coma or sleeping position). If a suboccipital approach is required, the nondependent (upper) shoulder should be taped down towards the foot. However, this can cause additional stretching of the brachial plexus (maneuvers to prevent brachial plexus injury are discussed in “Lateral Position” section).
IV. Summary
Positioning of the patient for neurological surgery is an important part of anesthesia care and poses many technical and physiological challenges. As discussed, recognition of the physiological changes with positioning and careful and meticulous positioning may decrease unwanted complications.
Box 1. Summary of Task Force Consensus on the Prevention of Perioperative Peripheral Neuropathies Relevant to Positioning for Neurosurgery (1)
Preoperative assessment
Ascertain that patients can comfortably tolerate the anticipated operative position
Upper extremity positioning
Arm abduction should be limited to 90° in supine patients; patients who are positioned prone may comfortably tolerate arm abduction greater than 90°
Position arms to decrease pressure on ulnar groove (humerus). When arms are tucked at the side, neutral forearm position is recommended. When arms are abducted on armboards, either supination or a neutral forearm position is acceptable.
Prolonged pressure on the radial nerve in the spiral groove of the humerus should be avoided.
Extension of the elbow beyond a comfortable range may stretch the median nerve.
Lower extremity positioning
Prolonged pressure on the peroneal nerve at the fibular head should be avoided.
Neither extension nor flexion of the hip increases the risk of femoral neuropathy.
Protective padding
Padded armboards may decrease the risk of upper extremity neuropathy.
The use of chest rolls in laterally positioned patients may decrease the risk of upper extremity neuropathies.
Padding at the elbow and at the fibular head may decrease the risk of upper and lower extremity neuropathies, respectively.
Equipment
Properly functioning automated blood pressure cuffs on the upper arms do not affect the risk of upper extremity neuropathies.
Shoulder braces in steep head-down positions may increase the risk of brachial plexus neuropathies.
Postoperative assessment
A simple postoperative assessment of extremity nerve function may lead to early recognition of peripheral neuropathies.
Documentation
Charting specific position actions during the care of patients may result in improvements of care by (1) helping practitioners focus attention on relevant aspect of patient positioning; and (2) providing information that continuous improvement processes can use to lead to refinement in patient care.
Footnotes
(Adapted from American Society of Anesthesiologists Task Force on the Prevention of Perioperative Peripheral Neuropathies: Practice Advisory for the Prevention of Perioperative Peripheral Neuropathies. Anesthesiology 2000; 92: 1168–1182)
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Society of Anesthesiologists. Task Force on the Prevention of Perioperative Peripheral Neuropathies: Practice Advisory for the Prevention of Perioperative Peripheral Neuropathies. Anesthesiology. 2000;92:1168–1182. doi: 10.1097/00000542-200004000-00036. [DOI] [PubMed] [Google Scholar]
- 2.Shapiro H, Drummond J. Neurosurgical Anesthesia. In: Miller RD, editor. Anesthesia. 4th ed. New York, NY: Churchill Livingstone Inc.; 1994. pp. 1897–1946. [Google Scholar]
- 3.Clatterbuck R, Tamargo R. Surgical Positioning and Exposures for Cranial Procedures. In: Winn H, editor. Youmans Neurological Surgery. 5 ed. Philadelphia, Pennsylvania: Sounders Elsevier Inc; 2004. pp. 623–645. [Google Scholar]
- 4.Goodkin R, Mesiwala A. General Principles of Operative Positioning. In: Winn HR, editor. Youmans Neurological Surgery. 5th ed. Sounders: Elsevier Inc.; 2004. pp. 595–621. [Google Scholar]
- 5.Toole JF. N Engl J Med. Vol. 279. 1968. Effects of change of head, limb and body position on cephalic circulation; pp. 307–311. [DOI] [PubMed] [Google Scholar]
- 6.Vandam L. Positioning of Patients for Operation. In: Rogers M, Tinker J, Covino B, Longnecker D, editors. Principles and Practice of Anesthesiology. Mosby-Year Book, Inc.; 1993. [Google Scholar]
- 7.Todd M, Warner D. Neuroanesthesia: A Critical Review. In: Rogers MC, Tinker J, Covino B, Longnecker D, editors. Principles and Practice of Anesthesiology. St Luis Missouri: Mosby-Year Book, Inc.; 1993. [Google Scholar]
- 8.Cirovic S, Walsh C, Fraser WD, Gulino A. The effect of posture and positive pressure breathing on the hemodynamics of the internal jugular vein. Aviat Space Environ Med. 2003;74:125–131. [PubMed] [Google Scholar]
- 9.Epstein HM, Linde HW, Crampton AR, et al. The vertebral venous plexus as a major cerebral venous outflow tract. Anesthesiology. 1970;32:332–337. doi: 10.1097/00000542-197004000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Enderby GE. Postural ischaemia and blood-pressure. Lancet. 1954;266:185–187. doi: 10.1016/s0140-6736(54)91258-1. [DOI] [PubMed] [Google Scholar]
- 11.Cucchiara R, Faust R. Patient Positioning. In: Miller RD, editor. Miller's Anesthesia. 4th ed. New York, NY: Churchill Livingstone Inc; 1994. pp. 1057–1074. [Google Scholar]
- 12.West JB, Dollery CT, Naimark A. Distribution of Blood Flow in Isolated Lung; Relation to Vascular and Alveolar Pressures. J Appl Physiol. 1964;19:713–724. doi: 10.1152/jappl.1964.19.4.713. [DOI] [PubMed] [Google Scholar]
- 13.Kaneko K, Milic-Emili J, Dolovich MB, et al. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol. 1966;21:767–777. doi: 10.1152/jappl.1966.21.3.767. [DOI] [PubMed] [Google Scholar]
- 14.Della Valle AG, Salonia-Ruzo P, Peterson MGE, Salvati EA, Sharrock NE. Inflatable Pillows as Axillary Support Devices During Surgery Performed in the Lateral Decubitus Position Under Epidural Anesthesia. Anesth. Analg. 2001;93:1338–1343. doi: 10.1097/00000539-200111000-00062. [DOI] [PubMed] [Google Scholar]
- 15.Toyota S, Amaki Y. Hemodynamic evaluation of the prone position by transesophageal echocardiography. J Clin Anesth. 1998;10:32–35. doi: 10.1016/s0952-8180(97)00216-x. [DOI] [PubMed] [Google Scholar]
- 16.Yokoyama M, Ueda W, Hirakawa M, Yamamoto H. Hemodynamic effect of the prone position during anesthesia. Acta Anaesthesiol Scand. 1991;35:741–744. doi: 10.1111/j.1399-6576.1991.tb03382.x. [DOI] [PubMed] [Google Scholar]
- 17.Hering R, Wrigge H, Vorwerk R, et al. The effects of prone positioning on intraabdominal pressure and cardiovascular and renal function in patients with acute lung injury. Anesth Analg. 2001;92:1226–1231. doi: 10.1097/00000539-200105000-00027. [DOI] [PubMed] [Google Scholar]
- 18.Sudheer PS, Logan SW, Ateleanu B, Hall JE. Haemodynamic effects of the prone position: a comparison of propofol total intravenous and inhalation anaesthesia. Anaesthesia. 2006;61:138–141. doi: 10.1111/j.1365-2044.2005.04464.x. [DOI] [PubMed] [Google Scholar]
- 19.Wadsworth R, Anderton JM, Vohra A. The effect of four different surgical prone positions on cardiovascular parameters in healthy volunteers. Anesthesia. 1996;51:819–822. doi: 10.1111/j.1365-2044.1996.tb12608.x. [DOI] [PubMed] [Google Scholar]
- 20.Palmon SC, Kirsch JR, Depper JA, Toung TJK. The effect of the prone position on pulmonary mechanics is frame dependent. Anesth Analg. 1998;87:1175–1180. doi: 10.1097/00000539-199811000-00037. [DOI] [PubMed] [Google Scholar]
- 21.Dharmavaram S, Jellish WS, Nockels RP, Shea J, Mehmod R, Ghanayem A, Kleinman B, Jacobs W. Effect of prone positioning systems on hemodynamic and cardiac function during lumbar spine surgery: an echocardiographic study. Spine. 2006;31:1388–1393. doi: 10.1097/01.brs.0000218485.96713.44. [DOI] [PubMed] [Google Scholar]
- 22.Practice advisory for perioperative visual loss associated with spine surgery: a report by the American Society of Anesthesiologists Task Force on Perioperative Blindness. Anesthesiology. 2006;104:1319–1328. doi: 10.1097/00000542-200606000-00027. [DOI] [PubMed] [Google Scholar]
- 23.Ellis SC, Bryan-Brown CW, Hyderally H. Massive swelling of the head and neck. Anesthesiology. 1975;42:102–103. doi: 10.1097/00000542-197501000-00017. [DOI] [PubMed] [Google Scholar]
- 24.Di Lorenzo N, Caruso R, Floris R, et al. Pneumocephalus and tension pneumocephalus after posterior fossa surgery in the sitting position: a prospective study. Acta Neurochir (Wien) 1986;83:112–115. doi: 10.1007/BF01402388. [DOI] [PubMed] [Google Scholar]
- 25.Hitselberger WE, House WF. A warning regarding the sitting position for acoustic tumor surgery. Arch Otolaryngol. 1980:106–169. doi: 10.1001/archotol.1980.00790260001001. [DOI] [PubMed] [Google Scholar]
- 26.Matjasko J, Petrozza P, Cohen M, Steinberg P. Anesthesia and surgery in the seated position: analysis of 554 cases. Neurosurgery. 1985;17:695–702. doi: 10.1227/00006123-198511000-00001. [DOI] [PubMed] [Google Scholar]
- 27.Young ML, Smith DS, Murtagh F, et al. Comparison of surgical and anesthetic complications in neurosurgical patients experiencing venous air embolism in the sitting position. Neurosurgery. 1986;18:157–161. doi: 10.1227/00006123-198602000-00007. [DOI] [PubMed] [Google Scholar]
- 28.Duke DA, Lynch JJ, Harner SG, et al. Venous air embolism in sitting and supine patients undergoing vestibular schwannoma resection. Neurosurgery. 1998;42:1282–1286. doi: 10.1097/00006123-199806000-00047. discussion 6–7. [DOI] [PubMed] [Google Scholar]
- 29.Black S, Cucchiara R. Tumor Surgery. In: RF Cucchiara SB, Michenfelder JD, editors. Clinical Neuroanesthesia. Second ed. NY, New York 10011: 1998. pp. 334–366. [Google Scholar]
- 30.Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: a critical appraisal. Br J Anaesth. 1999;82:117–128. doi: 10.1093/bja/82.1.117. [DOI] [PubMed] [Google Scholar]
- 31.Papadopoulos G, Kuhly P, Brock M, et al. Venous and paradoxical air embolism in the sitting position. A prospective study with transoesophageal echocardiography. Acta Neurochir (Wien) 1994;126:140–143. doi: 10.1007/BF01476424. [DOI] [PubMed] [Google Scholar]
- 32.Standefer M, Bay JW, Trusso R. The sitting position in neurosurgery: a retrospective analysis of 488 cases. Neurosurgery. 1984;14:649–658. doi: 10.1227/00006123-198406000-00001. [DOI] [PubMed] [Google Scholar]