Abstract
Background
The study of Hospitalizations for ambulatory care sensitive conditions (ACSH) has been proposed as an indirect measure of access to and receipt of care by older persons at the entryway to the Spanish public health system. The aim of this work is to identify the rates of ACSH in persons 65 years or older living in different small-areas of the Community of Madrid (CM) and to detect possible differences in ACSH.
Methods
Cross-sectional, ecologic study, which covered all 34 health districts of the CM. The study population consisted of all individuals aged 65 years or older residing in the CM between 2001 and 2003, inclusive. Using hospital discharge data, avoidable ACSH were selected from the list of conditions validated for Spain. Age- and sex-adjusted ACSH rates were calculated for the population of each health district and the statistics describing the data variability. Point graphs and maps were designed to represent the ACSH rates in the different health districts.
Results
Of all the hospitalizations, 16.5% (64,409) were ACSH. Globally, the rate was higher among men: 33.15 per 1,000 populations vs. 22.10 in women and these differences were statistically significant (p < 0.05) in each district. For men the range was 70.82 and the coefficient of variation (CV) was 0.47, while for women the range was 43.69 and the CV was 0.48. In 93.1% of cases, the ACSH were caused by hypertensive cardiovascular disease, heart failure or pneumonia. A centripetal pattern can be observed, with lower rates in the districts in the center of the CM. This geographic distribution is maintained after grouping by sex.
Conclusion
A significant variation is demonstrated in "preventable" hospitalizations between the different districts. In all the districts the men present rates significantly higher than women. Important variations in the access are observed the Primary Attention in spite of existing a universal sanitary cover.
Background
Hospitalizations for ambulatory care sensitive conditions (ACSH) are an indicator of the use of hospital resources for health problems that could have been prevented, treated or controlled in primary health care (PHC) [1]. This indicator was developed in the late 1980s by Billings in the United States to examine access to health care by the indigent population[2]. It is a direct indicator of potentially avoidable hospitalizations and an indirect indicator of access to PHC and its capacity to manage health problems. In fact, several studies have concluded that high rates of ACSH indicate suboptimal PHC, understood as inappropriate care with regard to type, place, intensity or timing of management of the health problem[3,4].
In Spain there is growing interest in evaluating primary care by using health outcome indicators[5] such as ACSH. To understand this interest one must be aware of the profound changes produced in the Spanish health system in the last 25 years, especially with regard to the organization and management of primary care [6]. The Spanish health care system is mainly publicly financed and is designed to provide access to all the country's residents, regardless of their socioeconomic level or geographical differences. It is a highly decentralized system, with 17 Regional Health Services managed by Regional Governments [6]. The primary care level is based in Health Centers where the Primary Health Care Team, made up of doctors, nurses, a social worker and clerical staff, provide care for a population of 5,000–25,000 people (1,700–1,800 persons per family doctor) [6].
Although many small-area studies have been carried out to identify variations in ACSH in persons under 65 [7], few such studies have been made in older persons, despite their importance both demographically and in terms of health resource use[8]. By 2050, Spain will be the country with the largest proportion of population over 60 (44.1%)[9], however no study of ACSH in the older population has been made in this country.
Thus, the study of ACSH has been proposed as an indirect measure of access to and receipt of care by older persons at the entryway to the Spanish public health system. The objective of this work is to identify the rates of ACSH in persons 65 years or older living in different small-areas of the Community of Madrid (CM) and to detect possible differences in ACSH.
Methods
This was a cross-sectional, ecologic study. Health care in the CM is organized into 11 health areas (with a public reference hospital in each) which are in turn divided into health districts. The health district was used as the territorial unit of analysis. The study covered all 34 health districts of the CM, with a total population of 5,372.433 inhabitants in 2001.
The study population consisted of all individuals aged 65 years or older residing in the CM between 2001 and 2003, inclusive. Three age groups were created for the presentation of results: 65–74 years, 75–84 years and 85 or older.
We analyzed all hospitalizations during the years 2001–2003. The Continuous Municipal Population Census was the source of data for population characteristics (size and structure). Information on hospitalization episodes was obtained from the Minimum Basic Data Set on Hospital Discharges and Ambulatory Surgery (CMBD-AH, in Spanish). The CMBD-AH is a registry of all hospitalization episodes, which includes administrative data (age, sex, residence, type of admission, etc.) and clinical data (principal diagnosis and other secondary diagnoses, diagnostic and therapeutic procedures); all public and private hospitals in the CM are required to report these data. This study was based on hospitalizations in public hospitals, which represent 71% of all hospitalizations in the CM. These data files were supplied by the Health Information Service of the General Directorate of Informatics, Communications and Technological Innovation of the Regional Health Ministry of the Community of Madrid.
Diagnoses and procedures in the CMBD-AH are coded in accordance with the International Classification of Diseases, 9th revision, Clinical Modification (ICD 9-CM). Avoidable ACSH were selected from the list of conditions validated for Spain by Caminal, et al (Table 1) [10].
Table 1.
Categories of Ambulatory Care Sensitive Conditions (ACSC) used to evaluate the capacity of Primary Care to avoid hospitalizations
| Vaccine-preventable diseases and other diseases | ICD-9 Codes |
| 1. Diphtheria | 32 |
| 2. Tetanus | 37 |
| 3. Acute poliomyelitis | 45 |
| 4. Homophiles meningitis | 320.0 |
| 5. Rheumatic fever | 390; 391 |
| Syphilis | |
| 6. Congenital syphilis | 90 |
| Tuberculosis | |
| 7. Other tuberculosis | 012–018 |
| Diabetes | |
| 8. Diabetes with general complications | 250.1; 250.2; 250.3 |
| 9. Hypoglycemic coma | 251.0 |
| 10. Gangrene+ diabetes with peripheral circulatory disorders | 785.4 + 250.7 |
| Disorders of fluid, electrolyte, and acid-base balance | |
| 11. Volume depletion/dehydration | 276.5 |
| 12. Hypotassemia | 276.8 |
| Acute respiratory infections | |
| 13. Peritonsillar abscess | 475 |
| Hypertensive cardiovascular disease | |
| 14. Malignant essential hypertension | 401.0 |
| 15. Malignant hypertensive kidney disease | 403.0 |
| 16. Malignant hypertensive heart and kidney disease | 404.0 |
| 17. Malignant secondary hypertension | 405.0 |
| 18. Ischemic heart disease | 410 – 414 |
| 19. Cerebrovascular disease | 430; 431; 436; 437.2 |
| Congestive heart failure (CHF) | |
| 20. Malignant hypertensive heart disease with CHF | 402.01 |
| 21. Benign hypertensive heart disease with CHF | 402.11 |
| 22. Hypertensive heart disease, unspecified, with CHF | 402.91 |
| 23. Heart failure | 428 |
| 24. Acute pulmonary edema, unspecified | 415.4 |
| Pneumonia | |
| 25. Pneumonia due to Hemophilus influenza | 482.2 |
| 26. Pneumonia due to Streptococcus | 482.3 |
| 27. Pneumonia due to other specified organism | 483 |
| 28. Bronchopneumonia/Pneumonia, organism unspecified | 485; 486 |
| Bleeding or perforated ulcer | |
| 29. Acute or chronic gastric ulcer or unspecified. | 531.0; 531.2; 531.4; 531.6 |
| 30. Acute or chronic duodenal ulcer or unspecified | 532.0; 532.2; 532:4; 532.6 |
| 31. Peptic ulcer, site unspecified, acute or chronic or unspecified | 533.0; 533.2; 533.4; 533.6 |
| Acute appendicitis with complications | |
| 32. Acute appendicitis with generalized peritonitis | 540.0 |
| 33. Acute appendicitis with peritoneal abscess | 540.1 |
| Urinary tract infections | |
| 34. Acute pyelonephritis | 590.1 |
| Pelvic inflammatory disease | |
| 35. Inflammatory disease of ovary, fallopian tube, pelvic cellular tissue and peritoneum | 614 |
Source: Caminal et al [10]
Age- and sex-adjusted ACSH rates were calculated for the population of each health district. The population was stratified into 5-year age groups from 65 to 99 years, with a single population group for those 100 years of age or older. The rates were standardized by the direct method, with the 2001 population of the CM used as the reference population. The data for the three years of the study were combined to produce more stable rates.
In the data analysis, we calculated the ACSH rates and the statistics describing the data variability (coefficient of variation, systematic coefficient of variation, weighted coefficient of variation and the ratio of variation) [11-13]. The Chi-square test was applied to determine if there were significant differences between observed and expected hospitalizations, and Student's t was used to test for differences in the ACSH rates by sex. The Pearson correlation was calculated to test for associations among the different ACSH. Point graphs and maps were designed to represent the ACSH rates in the different health districts.
Results
For the years 2001–2003, the CMBD-AH registered a total of 390,017 hospital discharges for the study group of persons 65 years and older in the 34 health districts of the CM. The study population was 60% female and the mean age was 78.9 years (76.9 years in men and 80.5 years in women). Of all the hospitalizations, 16.5% (64,409) were ACSH.
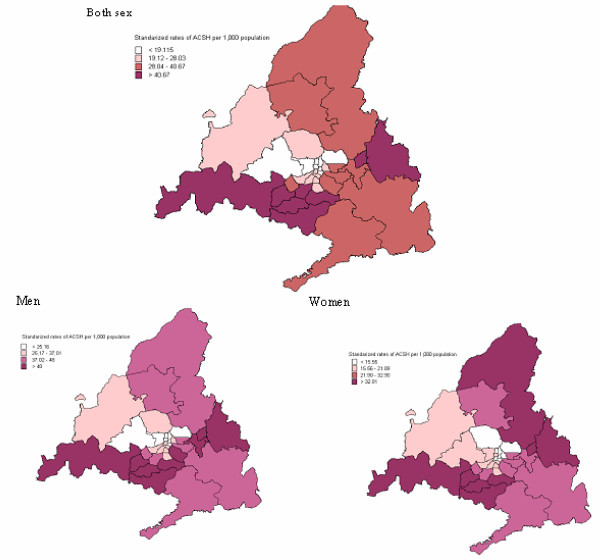
Table 2 shows the ACSH rates per 1,000 population for men and women in each of the 34 health districts. The main result shown in this table is that ACSH rates were higher in men than in women, and these differences were statistically significant (p < 0.05) in each district. Men also had higher ACSH rates than women in each age group studied. These differences were studied by health district, and statistically significant differences were found in each age group (p < 0.05). Figure 1 shows the standardized rates grouped by quartiles for all ACSH in the 34 health districts. A centripetal pattern can be observed, with lower rates in the districts in the center of the CM. This geographic distribution is maintained after grouping by sex.
Table 2.
Age-standardized* hospitalization rates for ACSCs in men and women, by health district in the Community of Madrid
| Men** | Women** | |||
| Health district | Number of hospitalizations | Rates per 1,000 population | Number of hospitalizations | Rates per 1,000 population |
| 101 Arganda | 638 | 47.35 | 660 | 31.39 |
| 102 Moratalaz | 1,186 | 43.60 | 976 | 22.01 |
| 103 Retiro | 668 | 24.43 | 736 | 13.31 |
| 104 Vallecas | 2,632 | 48.80 | 2,601 | 28.15 |
| 201 Coslada | 492 | 42.47 | 571 | 32.74 |
| 202 Salamanca | 710 | 19.66 | 688 | 8.30 |
| 203 Chamartín | 565 | 17.66 | 585 | 9.73 |
| 301 Alcalá de Henares | 1,443 | 60.72 | 1,325 | 38.41 |
| 302 Torrejón de Ardoz | 686 | 75.53 | 592 | 43.22 |
| 401 Ciudad Lineal | 1,380 | 28.08 | 1,250 | 14.88 |
| 402 San Blás | 1,148 | 38.10 | 1,066 | 22.92 |
| 403 Hortaleza | 654 | 23.11 | 628 | 14.00 |
| 501 Alcobendas | 1,292 | 47.73 | 1,289 | 33.38 |
| 502 Colmenar Viejo | 402 | 37.69 | 417 | 25.66 |
| 503 Tetuan | 733 | 20.76 | 727 | 10.89 |
| 504 Fuencarral | 909 | 25.40 | 906 | 15.28 |
| 601 Majadahonda | 469 | 22.62 | 576 | 15.64 |
| 602 Collado Villalba | 671 | 29.16 | 698 | 19.98 |
| 603 Moncloa | 489 | 20.82 | 520 | 11.50 |
| 701 Centro | 1,017 | 36.32 | 1,272 | 18.85 |
| 702 Chamberí | 757 | 19.74 | 994 | 17.76 |
| 703 Latina | 1,627 | 30.08 | 1,753 | 19.93 |
| 801 Mostoles | 1,051 | 59.95 | 1,206 | 41.11 |
| 802 Alcorcón | 871 | 45.44 | 831 | 26.47 |
| 803 Navalcarnero | 696 | 54.23 | 751 | 35.71 |
| 901 Leganés | 968 | 46.23 | 900 | 28.89 |
| 902 Fuenlabrada | 883 | 88.48 | 827 | 51.87 |
| 1001 Parla | 849 | 74.59 | 932 | 51.99 |
| 1002 Getafe | 1,040 | 59.02 | 1,008 | 34.89 |
| 1101 Aranjuez | 782 | 43.57 | 687 | 25.15 |
| 1102 Arganzuela | 957 | 35.48 | 939 | 16.65 |
| 1103 Villaverde | 868 | 34.91 | 800 | 21.77 |
| 1104 Carabanchel | 1,822 | 34.95 | 1,724 | 19.72 |
| 1105 Usera | 866 | 30.84 | 753 | 16.57 |
Data source: CMBD-AH, 2001–2003. Health Information Service of the General Directorate of Informatics, Communications and Technological Innovation of the Regional Health Ministry of the Community of Madrid.
ACSC: Ambulatory Care Sensitive Conditions * Rates standardized by the direct method ** p < 0.05 with Student's t-test
Figure 1.
Map of standardized ACSH rates grouped by cuartiles, by health district.
Table 3 shows the rates and variation statistics for all ACSH. Globally, the rate was higher among men: 33.15 per 1,000 population vs. 22.10 in women. For men the range was 70.82 and the coefficient of variation (CV) was 0.47, while for women the range was 43.69 and the CV was 0.48. In both cases the systematic coefficient of variation (SCV) was larger than 0.20.
Table 3.
ACSH rates and variation statistics, by sex. Community of Madrid
| All ACSC hospitalizations | ||||
| Both sexes | Men | Women | ||
| N | Health districts | 34 | 34 | 34 |
| Population | 2,428,373 | 972,093 | 1,456,280 | |
| Cases | 64,409 | 32,221 | 32,188 | |
| Rates | Crude rate | 26.52 | 33.15 | 22.10 |
| Adjusted rate | 26.27 | 35.57 | 20.45 | |
| Minimum | 12.20 | 17.66 | 8.30 | |
| Maximum | 69.03 | 88.48 | 51.99 | |
| Percentile 5 | 12.64 | 19.16 | 9.37 | |
| Percentile 25 | 19.12 | 25.16 | 15.55 | |
| Percentile 50 | 28.03 | 37.01 | 21.89 | |
| Percentile 75 | 40.67 | 48.00 | 32.90 | |
| Percentile 95 | 66.56 | 78.77 | 51.90 | |
| Variation statistics | CV | 0.47 | 0.47 | 0.48 |
| SCV | 0.33 | 0.20 | 0.37 | |
| wCV | 0.61 | 0.62 | 0.61 | |
| Chi-square | <0.001 | <0.001 | <0.001 | |
| Ratio of variation | RV | 5.66 | 5.01 | 6.26 |
| RV P5-P95 | 5.26 | 4.11 | 5.54 | |
| RV P25-P75 | 2.13 | 1.91 | 2.12 | |
CV: coefficient of variation. SCV: systematic coefficient of variation. wCV: weighted coefficient of variation. RV: ratio of variation. ACSC: Ambulatory Care Sensitive Conditions. ACSH: Hospitalizations for Ambulatory Care Sensitive Conditions
In 93.1% of cases, the ACSH were caused by hypertensive cardiovascular disease, heart failure or pneumonia. The remaining 6.9% were divided among several causes, most notably, 3.9% for ulcer and 1.1% for diabetes mellitus. In 36.3% (23,375) of cases, the hospitalizations were for hypertensive cardiovascular disease; 56.4% of these were in men and 43.6% in women (p < 0.001). Some 35.5% of hospitalizations (22,863) were for heart failure, 37.3% of which were in men and 62.7% in women (p < 0.001). About 21.3% of all ACSH (13,749) were for pneumonia, 60.4% in men and 39.6% in women (p < 0.001).
Table 4 shows the rates and variation statistics for each of the three most frequent causes of hospitalizations. In all three cases, the lowest adjusted rates were found in women. All three types of hospitalizations showed a high level of variability. The lowest variability was seen for hypertensive cardiovascular disease (SCV = 0.23), and the highest for pneumonia (SCV = 0.69), both after adjusting for sex and when calculated separately for men and women. As can be seen, pneumonia was the condition with the widest variability in ACSH rates.
Table 4.
ACSH rates and variation statistics, by cause of hospitalization.
| Hypertensive cardiovascular disease | Heart failure | Pneumonia | ||||||||
| Both sexes | Men | Women | Both sexes | Men | Women | Both sexes | Men | Women | ||
| N | Health districts | 34 | 34 | 34 | 34 | 34 | 34 | 34 | 34 | 34 |
| Population | 2,428,373 | 972,093 | 1,456,280 | 2,428,373 | 972,093 | 1,456,280 | 2,428,373 | 972,093 | 1,456,280 | |
| Rates | Cases | 23,375 | 13,189 | 10,186 | 22,863 | 8,538 | 14,325 | 13,749 | 8,298 | 5,451 |
| Crude rate | 9.41 | 8.78 | 9.84 | 9.63 | 13.57 | 6.99 | 5.66 | 8.54 | 3.74 | |
| Adjusted rate | 9.30 | 9.66 | 8.97 | 9.58 | 13.94 | 6.65 | 5.59 | 9.57 | 3.39 | |
| Minimum | 3.64 | 7.30 | 2.48 | 3.64 | 3.84 | 2.96 | 1.1 | 1.92 | 0.75 | |
| Maximum | 27.39 | 41.09 | 18.42 | 25.38 | 25.21 | 25.65 | 16.96 | 28.71 | 9.81 | |
| Percentile 5 | 3.74 | 7.94 | 2.95 | 3.74 | 4.61 | 3.45 | 1.27 | 2.04 | 0.86 | |
| Percentile 25 | 8.37 | 11.71 | 5.67 | 6.79 | 6.63 | 6.66 | 3.23 | 5.38 | 2.14 | |
| Percentile 50 | 10.02 | 14.60 | 6.86 | 9.50 | 9.82 | 9.75 | 5.27 | 8.80 | 3.54 | |
| Percentile 75 | 13.59 | 18.36 | 9.65 | 14.39 | 14.23 | 15.47 | 10.17 | 15.26 | 6.78 | |
| Percentile 95 | 20.38 | 28.44 | 15.15 | 21.36 | 20.97 | 22.14 | 15,94 | 26.39 | 9.58 | |
| Variation statistics | CV | 0.43 | 0.44 | 0.46 | 0.51 | 0.55 | 0.50 | 0.61 | 0.62 | 0.61 |
| SCV | 0.23 | 0.16 | 0.28 | 0.32 | 0.22 | 0.38 | 0.69 | 0.57 | 0.77 | |
| wCV | 0.54 | 0.55 | 0.57 | 0.69 | 0.74 | 0.67 | 0.84 | 0.85 | 0.84 | |
| Chi-square | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| Ratio of variation | RV | 7.52 | 5.63 | 7.43 | 6.97 | 6.57 | 8.67 | 15.28 | 14.95 | 13.08 |
| RV P5-P95 | 5.45 | 3.58 | 5.14 | 5.72 | 4.55 | 6.42 | 12.58 | 12.94 | 11.10 | |
| RV P25-P75 | 1.62 | 1.57 | 1.70 | 2.12 | 2.15 | 2.32 | 3.15 | 2.84 | 3.16 | |
CV: coefficient of variation. SCV: systematic coefficient of variation. wCV: weighted coefficient of variation. RV: ratio of variation. ACSH: Hospitalizations for Ambulatory Care Sensitive Conditions
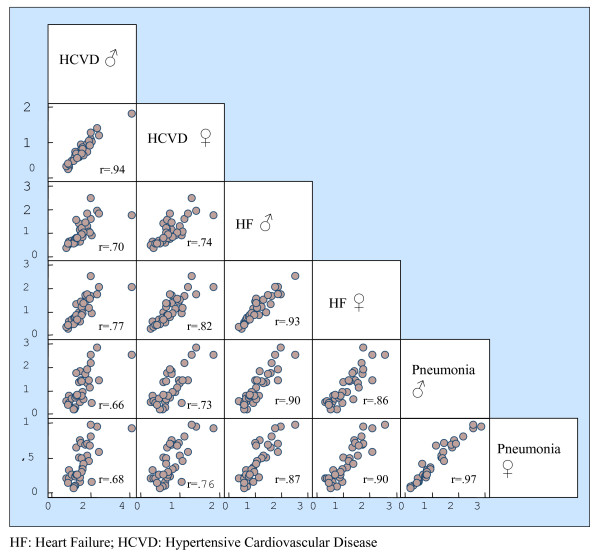
The coefficients of correlation were calculated between the different causes of hospitalization. The results were 0.91 between the hospitalization rate for heart failure and pneumonia, 0.80 between hypertensive cardiovascular disease and heart failure, and 0.73 between hypertensive cardiovascular disease and pneumonia. The correlations for these diseases by sex are shown in Figure 2.
Figure 2.
Correlation of rates of ACSC avoidable hospitalizations.
Discussion
This study demonstrates the existence of high ACSH rates in the elderly population, and that these rates are higher in men than in women. It also shows that there is considerable variability in these rates, even in a health system like Spain's, which offers universal coverage.
The ACSH rates found are similar to those obtained in studies in other countries for this age group [14-17], and are higher than those observed in persons under 65, both in Spain [18-20] and in other countries [21-23]. The ACSH rates in older men are higher than those in women, both globally and for the three most frequent avoidable causes of hospitalization, a finding that is consistent with the results of other studies [1,14]. Factors associated with different patterns of morbidity and use of services by men and women as well as sex-linked factors may explain this finding[24]. With regard to the differences in morbidity between men and women, men were seen to have a higher prevalence of diseases like heart failure, asthma or chronic bronchitis, which were included in the list of ambulatory care sensitive conditions (ACSC) used in this study, while women had a higher prevalence of non-fatal chronic diseases (arthrosis, osteoporosis, and osteomuscular problems and depression in general), conditions that were not included in the ACSC list but may lead to both lower quality of life and lower mortality [25-27] than in men. On the other hand, studies have shown that women use primary care services more than men do, whereas they make less use of hospital services[28,29]. The gender-associated role of family caregiver may also lead some women to reject hospitalization out of a need to meet their caregiver responsibilities[24].
However, there is a high correlation between ACSH rates in men and women by districts, that is, districts with higher numbers of admissions for men also have higher numbers of admissions for women. This may indicate the existence of a common factor such as deficiencies in PHC, different admission policies in the reference hospitals in these districts, or sociodemographic differences.
Considerable variation in ACSH rates in persons 65 years or older has also been reported by other authors[14,22,30-32], however it is less pronounced than what has been found in persons under 65[23,33-35]. Our study found less variability than that described in studies of the Medicare population[34]. These differences may be due to factors that depend on characteristics of the population, of health providers or of both [36]. The difference between our results and those of other studies could be attributed to the fact that that the global ACSC indicator used in our work is different from the list used in studies in the United States. This would be the case if we had used only the whole list with all the ACSC codes. However, the differences were maintained when we looked at the breakdown by specific conditions, such as pneumonia, in which the diagnostic codes are similar to those used in other studies [7,21,37].
Some methodological aspects of this work require a comment. First, it was based on secondary data; therefore it has limitations with regard to the validity of the principal diagnosis at discharge and the level of completeness of some of the important variables, such as home address, which limit the georeferencing of a large number of cases.
Second, the study was made only in public hospitals, which represent 71% of the hospitalizations in the CM. We chose not to include data collected in private hospitals for two main reasons: a) The data provided were frequently incomplete; b) It had previously been shown that inclusion of data from private hospitals had no impact on the ACSH rates (correlation coefficient of 0.938 between the datasets with and without private hospitals) [35].
Third, the three CMBD-AH data files did not contain all the variables needed to identify specific patients, therefore it was not possible to eliminate readmissions [11,12].
Fourth, because this study was based on aggregate data, it should be noted that an association among variables at an aggregate level does not necessarily mean that the association exists at the individual level[38].
Fifth, the indicator used has been validated for Spain[10], therefore this should not constitute a limitation. The list of ACSCs used is not specific to the elderly population, which could represent a limitation on its use in that population, mainly for chronic clinical conditions so severe that even patients with appropriate access to PHC could not have avoided hospitalization.
ACSH have been used by a variety of authors as an indirect measure to evaluate different aspects of the health system. In the United States, the ACSH indicator has been used to study and identify problems related with access to ambulatory care. Thus, areas with high rates of ACSH would have greater problems of access than those with lower rates. Various studies in the United States have found an inverse relation between ACSH rates and various indicators such as having medical insurance[37,39], income level[21,22,40], and related variables (race[41,42], residence in rural or urban areas[43,44], etc).
The National Health Service in the United Kingdom uses ACSH rates as an indicator of the quality of primary care[43,45]. It has been proposed to use this indicator in Spain, initially, for the same purpose as in previous studies that have focused on the pediatric [46,47], and general population [18,19,48]. However, this use of the indicator to evaluate the quality of the Spanish primary care model is subject to debate[19] because the results may be influenced, not only by the capacity to reduce health problems in Primary Care, but also by other variables, such as morbidity, different patterns of use of health resources, and the use of specialist care[49].
In light of the foregoing, Spanish researchers are increasingly proposing that the ACSH indicator be used to evaluate access to health services. Although the Spanish health care system provides universal coverage, in practice equal access does not exist [6] especially for older people, who are the main users of primary care. The results of this paper point in this direction.
Although other studies are needed, our data show small-area differences in ACSH rates in the CM, despite the region's relative homogeneity. It would be useful to have more precise knowledge of the present situation and to identify the factors (number of physicians, transportation time to the health center, income, educational level, differences in morbidity, disability...) that may influence the variability in avoidable hospitalizations in the elderly population. It is hoped that this study will encourage the use of this indicator as a way to detect problems associated with access to care in a health system with universal coverage.
Conclusion
In older people in the Community of Madrid, avoidable hospitalizations for ACSC were responsible for a considerable proportion of hospital admissions occurring in the study period, amounting to about 16.5%. The most frequent causes of these hospitalizations were, in decreasing order, hypertensive cardiovascular disease, heart failure and pneumonia. Wide variability was found in ACSH rates by sex (higher in men) and by geographic areas of analysis.
Abbreviations
ACSC, Ambulatory Care Sensitive Conditions; ACSH, Hospitalizations for Ambulatory Care Sensitive Conditions; CM, Community of Madrid; CMBD-AH, Minimum Basic Data set on Hospital Discharges and Ambulatory Surgery. SCV, Systematic Coefficient of Variation; CV, Coefficient of Variation. ICD-CM, International Classification of Diseases 9th revision, Clinical Modification. PHC, Primary Health Care. RV, Ratio of Variation. wCV, Weighted Coefficient of Variation. HCVD, Hypertensive Cardiovascular Disease. HF, Heart Failure.
Competing interests
The author(s) declare that they have no competing interest.
Authors' contributions
PM, AA and AO conceived the study and participated in its design. JMR helped write the manuscript. PM performed the analysis and wrote the first draft. All the authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
The authors would like to thank Drs. S. Peiró and J. Librero for their assistance in producing the graphs, and Drs. F. Rodríguez-Artalejo, M.V. Zunzunegui and L. García-Olmos for their comments on earlier versions of this article.
We would like to thank the reviewers for their thoughtful comments, which have been very helpful in enriching and improving our work.
This study was partially funded with grants from the Fondo de Investigaciones Sanitarias, Instituto de Salud Carlos III (Spanish Ministry of Health) PI030767, PI051898, RD06/0013/1013.
Contributor Information
Purificacion Magan, Email: pmagan@h12o.es.
Angel Otero, Email: angel.otero@uam.es.
Angel Alberquilla, Email: aalberquilla.gapm11@salud.madrid.org.
Jose Manuel Ribera, Email: jribera.hcsc@salud.madrid.org.
References
- Kozak LJ, Hall MJ, Owings MF. Trends in avoidable hospitalizations, 1980–1998. Health Aff (Millwood) 2001;20:225–232. doi: 10.1377/hlthaff.20.2.225. [DOI] [PubMed] [Google Scholar]
- Billings J, Teicholz N. Uninsured patients in District of Columbia hospitals. Health Aff (Millwood) 1990;9:158–165. doi: 10.1377/hlthaff.9.4.158. [DOI] [PubMed] [Google Scholar]
- Caminal J, Starfield B, Sánchez E, Casanova C, Morales M. The role of primary care in preventing ambulatory care sensitive conditions. Eur J Public Health. 2004;14:246–251. doi: 10.1093/eurpub/14.3.246. [DOI] [PubMed] [Google Scholar]
- Ansari Z, Laditka J, Laditka S. Access to health care and hospitalization for ambulatory care sensitive conditions. Med Care Res Rev. 2006;63:719–741. doi: 10.1177/1077558706293637. [DOI] [PubMed] [Google Scholar]
- Villalbí JR, Pasarín M, Montaner I, Cabezas C, Starfield B. Evaluación de la atención primaria de salud. Aten Primaria. 2003;31:382–385. doi: 10.1016/S0212-6567(03)70703-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Casasnovas G, Costa-Font J, Planas I. Diversity and regional inequalities in the Spanish 'system of health care services'. Health Econ. 2005;14:S221–235. doi: 10.1002/hec.1038. [DOI] [PubMed] [Google Scholar]
- Weissman JS, Gatsonis C, Epstein AM. Rates of avoidable hospitalization by insurance status in Massachusetts and Maryland. Jama. 1992;268:2388–2394. doi: 10.1001/jama.268.17.2388. [DOI] [PubMed] [Google Scholar]
- Laditka J, Laditka S. Insurance status and access to primary health care:disparate outcomes for potentially preventable hospitalization. J Health Soc Policy. 2004;19:81–100. doi: 10.1300/J045v19n02_04. [DOI] [PubMed] [Google Scholar]
- Koklikoff L, Hagist C. Who's going broke? Comparing healthcare costs in ten OECD countries. Cambridge: National Bureau of Economic research; 2005. [Google Scholar]
- Caminal J, Mundet X, Ponsa J, Sanchez E, Casanova C. [Hospitalizations due to ambulatory care sensitive conditions: selection of diagnostic codes for Spain] Gac Sanit. 2001;15:128–141. doi: 10.1016/s0213-9111(01)71532-4. [DOI] [PubMed] [Google Scholar]
- Diehr P, Cain KC, Kreuter W, Rosenkranz S. Can small-area analysis detect variation in surgery rates? The power of small-area variation analysis. Med Care. 1992;30:484–502. doi: 10.1097/00005650-199206000-00003. [DOI] [PubMed] [Google Scholar]
- Diehr P, Cain K, Ye Z, Abdul-Salam F. Small area variation analysis. Methods for comparing several diagnosis-related groups. Med Care. 1993;31:YS45–53. [PubMed] [Google Scholar]
- McPherson K, Wennberg JE, Hovind OB, Clifford P. Small-area variations in the use of common surgical procedures: an international comparison of New England, England, and Norway. N Engl J Med. 1982;307:1310–1314. doi: 10.1056/NEJM198211183072104. [DOI] [PubMed] [Google Scholar]
- Laditka SB, Laditka JN. Geographic variation in preventable hospitalization of older women and men: implications for access to primary health care. J Women Aging. 1999;11:43–56. doi: 10.1300/J074v11n04_04. [DOI] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB. Increased hospitalization risk for recently widowed older women and protective effects of social contacts. J Women Aging. 2003;15:7–28. doi: 10.1300/J074v15n02_02. discussion 185–187. [DOI] [PubMed] [Google Scholar]
- Blustein J, Hanson K, Shea S. Preventable hospitalizations and socioeconomic status. Health Aff (Millwood) 1998;17:177–189. doi: 10.1377/hlthaff.17.2.177. [DOI] [PubMed] [Google Scholar]
- Carter M, Porell F. Vulnerable populations at risk of potentially avoidable hospitalizations: the case of nursing home residents with Alzheimer's disease. Am J Alzheimers Dis Other Demen. 2005;20:349–358. doi: 10.1177/153331750502000605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquez-Calderon S, Rodriguez del Aguila MM, Perea-Milla E, Ortiz J, Bermudez-Tamayo C. [Factors associated with hospitalization for ambulatory care sensitive conditions in municipalities] Gac Sanit. 2003;17:360–367. doi: 10.1157/13053648. [DOI] [PubMed] [Google Scholar]
- Caminal Homar J, Starfield B, Sanchez Ruiz E, Hermosilla Perez E, Martin Mateo M. [Primary health care and hospitalizations in ambulatory care sensitive conditions in Catalonia] Rev Clin Esp. 2001;201:501–507. doi: 10.1016/s0014-2565(01)70896-x. [DOI] [PubMed] [Google Scholar]
- Bermudez-Tamayo C, Marquez-Calderon S, Aguila MRd, Perea-Milla E, Ortiz J. Organizational characteristics of primary care and hospitalization for to the main ambulatory care sensitive conditions. Aten Primaria. 2004;15:305–311. doi: 10.1157/13059762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappas G, Hadden WC, Kozak LJ, Fisher GF. Potentially avoidable hospitalizations: inequalities in rates between US socioeconomic groups. Am J Public Health. 1997;87:811–816. doi: 10.2105/ajph.87.5.811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roos LL, Walld R, Uhanova J, Bond R. Physician visits, hospitalizations, and socioeconomic status: ambulatory care sensitive conditions in a canadian setting. Health Serv Res. 2005;40:1167–1185. doi: 10.1111/j.1475-6773.2005.00407.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Billings J, Anderson GM, Newman LS. Recent findings on preventable hospitalizations. Health Aff (Millwood) 1996;15:239–249. doi: 10.1377/hlthaff.15.3.239. [DOI] [PubMed] [Google Scholar]
- Rohlfs I, Borrell C, Fonseca M. Género, desigualdades y salud pública: conocimientos y desconocimientos. Gac Sanit. 2000;14:60–71. [Google Scholar]
- Arber S. Gender and class inequalities in health: understanding the differentials. London: Aldershot:Gower Company; 1989. [Google Scholar]
- Macran S, Clarke L, Joshi H. Women's health: dimensions and differentials. Soc Sci Med. 1996;42:1203–1216. doi: 10.1016/0277-9536(95)00432-7. [DOI] [PubMed] [Google Scholar]
- Macintyre S, Hunt K, Sweeting H. Gender differences in health: are things really as simple as they seem? Soc Sci Med. 1996;42:617–624. doi: 10.1016/0277-9536(95)00335-5. [DOI] [PubMed] [Google Scholar]
- Fernandez E, Schiaffino A, Rajmil L, Badia X, Segura A. Gender inequalities in health and health care services use in Catalonia (Spain) J Epidemiol Community Health. 1999;53:218–222. doi: 10.1136/jech.53.4.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gijsbers van Wijk CM, van Vliet KP, Kolk AM. Gender perspectives and quality of care: towards appropriate and adequate health care for women. Soc Sci Med. 1996;43:707–720. doi: 10.1016/0277-9536(96)00115-3. [DOI] [PubMed] [Google Scholar]
- Parchman M, Culler S. Preventable hospitalizations in primary care shortage areas. An analysis of vulnerable medicare beneficiaries. Arch Fam Med. 1999;8:487–491. doi: 10.1001/archfami.8.6.487. [DOI] [PubMed] [Google Scholar]
- Wolff J, Starfield B, Anderson G. Prevalence, expenditures and complications of multiple chronic conditions in the elderly. Arch intern med. 2002;162:2269–2276. doi: 10.1001/archinte.162.20.2269. [DOI] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB, Probst JC. More may be better: evidence of a negative relationship between physician supply and hospitalization for ambulatory care sensitive conditions. Health Serv Res. 2005;40:1148–1166. doi: 10.1111/j.1475-6773.2005.00403.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bindman AB, Grumbach K, Osmond D, Komaromy M, Vranizan K, Lurie N, Billings J, Stewart A. Preventable hospitalizations and access to health care. JAMA. 1995;274:305–311. doi: 10.1001/jama.274.4.305. [DOI] [PubMed] [Google Scholar]
- Wennberg DE, Wennberg JE. Addressing variations: is there hope for the future? Health Aff (Millwood) 2003. W3-614-617. [DOI] [PubMed]
- Alberquilla Á. "Estudio de la hospitalización evitable por condiciones senseibles a los cuidados ambulatorios (ACSC) y de sus factores condicionantes en la Comunidad de Madrid". Universidad Autónoma de Madrid, Departamento de Medicina Preventiva y Salud Pública; 2004. [Google Scholar]
- Wennberg J. Small area variations in health care delivery. Science. 1973;182:1102–1108. doi: 10.1126/science.182.4117.1102. [DOI] [PubMed] [Google Scholar]
- Bindman AB, Chattopadhyay A, Osmond DH, Huen W, Bacchetti P. The impact of Medicaid managed care on hospitalizations for ambulatory care sensitive conditions. Health Serv Res. 2005;40:19–38. doi: 10.1111/j.1475-6773.2005.00340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgenstern H. Uses of ecologic analysis in epidemiologic research. Am J Public Health. 1982;72:1336–1344. doi: 10.2105/ajph.72.12.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng F, O'Leary J, Sloss E, Lopez M, Dhanani N, Melnick G. The effect of medicare health maintenance organizations on hospitalization rates for ambulatory care-sensitive conditions. Med Care. 2006;44:900–907. doi: 10.1097/01.mlr.0000220699.58684.68. [DOI] [PubMed] [Google Scholar]
- Billings J, Zeitel L, Lukomnik J, Carey TS, Blank AE, Newman L. Impact of socioeconomic status on hospital use in New York City. Health Aff (Millwood) 1993;12:162–173. doi: 10.1377/hlthaff.12.1.162. [DOI] [PubMed] [Google Scholar]
- Gaskin DJ, Hoffman C. Racial and ethnic differences in preventable hospitalizations across 10 states. Med Care Res Rev. 2000;57:85–107. doi: 10.1177/107755800773743619. [DOI] [PubMed] [Google Scholar]
- Laditka JN, Laditka SB, Mastanduno MP. Hospital utilization for ambulatory care sensitive conditions: health outcome disparities associated with race and ethnicity. Soc Sci Med. 2003;57:1429–1441. doi: 10.1016/S0277-9536(02)00539-7. [DOI] [PubMed] [Google Scholar]
- Jankowski R. What do hospital admission rates say about primary care? Bmj. 1999;319:67–68. doi: 10.1136/bmj.319.7202.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Mueller K, Chen L, KConway The role of rural health clinics in hospitalization due to ambulatory care sensitive conditions: a study in Nebraska 2006 Summer;22(3):220-3. J Rural Health. 2006;22:220–223. doi: 10.1111/j.1748-0361.2006.00035.x. [DOI] [PubMed] [Google Scholar]
- Giuffrida A, Gravelle H, Roland M. Measuring quality of care with routine data: avoiding confusion between performance indicators and health outcomes. Bmj. 1999;319:94–98. doi: 10.1136/bmj.319.7202.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casanova C, Colomer C, Starfield B. Pediatric hospitalization due to ambulatory care-sensitive conditions in Valencia (Spain) Int J Qual Health Care. 1996;8:51–59. doi: 10.1093/intqhc/8.1.51. [DOI] [PubMed] [Google Scholar]
- Sarría A, Franco A, Redondo S, García L, Rodriguez A. Hospitalizaciones en menores de un año en la ciudad de madrid y su relación con el nivel social y la mortalidad infantil. An Esp Pediatr. 2002;57:220–226. [PubMed] [Google Scholar]
- Alberquilla Á, Fuentes C, Severiano S. Hospitalización evitable por Ambulatory Care Sensitive Conditions (ACSC) en la Comunidad de Madrid. Reflexiones sobre su uso como medida de resultado de la Atención Primaria. Rev Adm Sanit. 2003;1:657–678. [Google Scholar]
- Gérvas J, Caminal J. Las hospitalizaciones por Ambulatory Care Sensitive Conditions (ACSC) desde el punto de vista del médico de Atención Primaria. Rev Esp Salud Publica. 2007;81:7–13. doi: 10.1590/s1135-57272007000100002. [DOI] [PubMed] [Google Scholar]