Abstract
Virus-like particles (VLPs) represent a promising vaccine against severe acute respiratory syndrome coronavirus (SARS CoV). In this study, recombinant baculovirus vAcS and vAcME were constructed to express the S protein and the M and E proteins of SARS CoV, respectively. Electron microscope analysis demonstrated the formation of VLPs in vAcME and vAcS coinfected insect cells. Mice immunized four times with VLPs developed high antibody titres against SARS CoV. In addition, VLPs elicited cell-mediated immunity as demonstrated by enhanced interferon-γ and interleukin-4 production. VLPs also conferred protective immunity against the infection of Spike protein pseudotyped murine leukaemia virus. Our findings demonstrate that SARS CoV VLPs are immunogenic and can elicit strong SARS CoV-specific humoral and cellular immune responses in mice. This is the first study describing the immunogenicity of SARS CoV VLPs, providing valuable data for developing a protective vaccine against SARS CoV infection.
Keywords: baculovirus expression vector system, immune response, severe acute respiratory syndrome, coronavirus, vaccine, virus-like particles
Introduction
Severe acute respiratory syndrome (SARS) has become a priority for health-care agencies around the world because of its transmissibility, associated mortality and the potential for pandemic spread. As of 31 December 2003, 8096 cases had been identified worldwide and 774 people had died, a mortality rate of about 9·6% (World Health Organization statistics [http://www.who.int/csr/sars/country/004-04-21/en/]). A novel coronavirus, SARS coronavirus (SARS CoV), was identified as the causative agent of SARS.1–5
The SARS CoV is markedly different from all three coronavirus groups known today. The virus genome is a positive-strand RNA of 29 kilobases, which encodes a RNA-dependent RNA polymerase and four main viral structural proteins: spike (S), envelope (E), membrane (M) and nucleocapsid (N).4 Electron microscopy of the viral particles revealed that it was an enveloped virion, with diameter ranging from 80 to 120 nm.1
In the Coronaviridae family, the S protein belongs to the family of type I membrane glycoproteins, which are responsible for both binding to receptors on host cells and membrane fusion.6,7 The S protein also contains important virus-neutralizing epitopes, and amino acid changes in the S protein can dramatically affect viral virulence.7 The cellular receptor of SARS CoV and the receptor-binding domain (RBD) on S protein have been identified.8,9 Previous studies showed that the RBD in the S1 region of S protein played a critical role in neutralizing antibody induction, angiotensin-converting enzyme 2 (ACE2) binding and virus entry.10 Depletion of RBD-specific antibodies from sera significantly reduced serum-neutralizing capability,11 indicating that this domain is dominant in neutralizing antibody induction.
The M protein is the most abundant structural protein, spanning the membrane bilayer three times, with a long C-terminal cytoplasmic domain inside the virion and a short N-terminal domain outside.12 The N protein is an internal phosphoprotein with molecular weight 50 000–60 000, which interacts with viral genomic RNA to form the helical nucleocapsid.4,13 The small E protein is a minor structural component, containing a hydrophobic region flanked by hydrophilic termini.14
Previous evidence indicates that M protein plays a key role in coronavirus assembly. In some viruses, such as murine hepatitis virus, M and E proteins are the only requirements for particle formation; the interactions between the M and E proteins result in the virus budding through the membrane.15,16 The S protein is dispensable but is incorporated when present.
In this report, two recombinant baculoviruses were constructed: vAcME containing the M and E genes, and vAcS containing the S gene. These two viruses were coinfected in Sf21 cells to generate virus-like particles (VLPs). Western blot and immunogold labelling indicated that SARS CoV proteins were assembled into the VLPs. The SARS CoV VLPs induced humoral and cellular immune responses against SARS CoV and were characterized in a mouse model. Our data collectively showed that SARS CoV VLPs induced both specific antibody and cell-mediated immune responses in immunized mice.
Materials and methods
Construction of recombinant baculoviruses
The S, E and M genes of SARS CoV were amplified from the WH20 strain (GenBank accession no. AY772062) by reverse transcription polymerase chain reaction (RT-PCR) with the following primers: 5′-GGGGGATCCATGTTTATTTTCTTATTATTT-3′ and 5′-GGGGAATTCTTATGTGTAATGTAATTTGAC-3′ for S gene; 5′-GGGGGATCCATGGCAGACAACGGTACTATT-3′ and 5′-GGGGAATTCTTACTGTACTAGCAAAGCAAT-3′ for M gene; 5′-GGGCCCGGGATGTACTCATTCGTTTCGGAA-3′ and 5′-GGGGGTACCTTAGACCAGAAGATCAGGAAC-3′ for E gene. The products of the S and M genes were digested with BamHI and EcoRI and then ligated to pFastBac DUAL, under the control of the polyhedron promoter, to generate pFBS and pFBM, respectively. The E gene PCR products were digested with SmaI and KpnI and then inserted into pFBM, under the control of the p10 Promoter, to generate pFBME. The constructs were inserted into AcMNPV Bacmid (Invitrogen, Carlsbad, CA) by transposition. The recombinant bacmids were transfected into Sf21 cells using Lipofectin to produce two recombinant baculoviruses: vAcS and vAcME. All viral stocks were prepared and manipulated according to the standard protocol.17
Production and purification of SARS CoV VLPs
The Sf21 cells were coinfected with vAcS and vAcME at a multiplicity of infection (MOI) of 5. At 96 hr post-infection, cells and medium were harvested and freeze–thawed twice in phosphate-buffered saline (PBS). The lysates were pelleted at 150 000 g for 3 hr, and then were placed on a sucrose density gradient from 30% (w/w) to 50% (w/w) for centrifugation at 200 000 g for 3 hr. A visible band between the 30% and 40% sucrose layers was collected, and pelleted at 150 000 g for 3 hr. The pellets were resuspended in PBS. The presence of SARS CoV VLPs in the purified preparations was analysed by electron microscopy and Western blots.
Electron microscopy and immunogold electron microscopy
Electron microscopy was used to examine VLP formation in insect cells. Briefly, Sf21 cells were infected with vAcS and vAcME at a MOI of 5, respectively, or coinfected with vAcS and vAcME at a MOI of 5. Ninety-six hours post-infection, infected cells were collected, fixed and analysed under the electron microscope. For negative staining, an aliquot of the VLP samples was placed on a carbon-coated grid. After standing for 5 min, grids were stained with 2% of phosphotungstic acid (PTA) for 2 min. The PTA was then drained and the grids were examined directly under the electron microscope. For immunogold labelling, purified VLPs were loaded onto a collodion-coated electron microscope grid for 12 hr. After the removal of excess sample solution, an S protein-specific antibody [provided by Lin-fa Wang, Commonwealth Scientific and Industrial Research Organization (CSIRO) Livestock Industries, Australian Animal Health Laboratory, Geelong, Australia] was added onto the grid and incubated for 1·5 hr at room temperature. Following three washes in PBS for 5 min per wash at room temperature, grids were incubated with 10 nm gold-conjugated anti-rabbit immunoglobulin G for 1·5 hr. After three 5-min washes in PBS, the samples were stained with 2% PTA for 2 min, drained, and examined under the electron microscope.
Mouse immunizations
Eight- to 12-week-old female BALB/c mice were purchased from HuBei Center for Disease Control (CDC) (Hubei, Wuhan, China), randomly divided into groups of five mice per group, and given pathogen-free water and food for maintenance. Mice were immunized with purified SARS CoV VLPs formed by S, M and E proteins at 0, 10, 20 and 30 days. 100 μg VLPs were immunized via subcutaneous injection in 200 μl sterile PBS with Freund's adjuvant at prime stage and incomplete Freund's adjuvant at boost stage. Mice were immunized with PBS and Freund's adjuvant mixture as negative controls.
Enzyme-linked immunosorbent assay (ELISA)
The humoral immune response to SARS CoV immunized with VLPs was evaluated on days 0, 10, 20, 30, 40, 50 and 60. Blood samples were collected by retro-orbital capillary plexus puncture. Antibody titres were determined using ELISA. Briefly, 96-well plates were coated with inactivated SARS CoV as antigen (200 ng per well in PBS buffer) at 4° overnight. Plates were blocked with PBS containing 1% bovine serum albumin (BSA) at room temperature for 2 hr. After three washes in PBS containing 0·05% Tween-20, 500-fold diluted sera were added, and plates were incubated for 2 hr at 37°. After three washes, alkaline phosphatase (AP)-conjugated anti-mouse immunoglobulin G were added to the plates for 1 hr at 37°. After removal of the unbound conjugates and washing, the para-nitrophenylphosphate (PNPP) substrate was added to the plates. Optical densities (OD) were then read at 405 nm in an ELISA reader. Results were given as the arithmetic mean ± standard error of the individual tests.
Neutralization assay
Neutralizing antibodies against SARS CoV were analysed using SARS CoV S protein-pseudotyped murine leukaemia viruses (MLV).18 Vero-E6 cells (1 × 105 per well) were seeded in a 96-well cell culture plate, and plates were then incubated overnight at 37° with 5% CO2 until confluent monolayers had formed. Serum samples collected at day 60 were heated at 56° for 30 min and used for testing. Sera were diluted two-fold from 1 : 1 to 1: 64 and incubated with 100 TCID50 of MLV (SARS) pseudotypes at 37° for 1 hr. Sera from PBS-immunized mice were used as negative controls. After incubation, 100 μl of serum/virus mixture was transferred from each well of the incubation plate to a 96-well cell culture plate containing Vero-E6 cells. Following 4 hr of incubation at 37°, serum/virus mixtures were replaced by cell culture medium. The plates were incubated at 37° with 5% CO2 for 3 days, and the number of green fluorescence cells was counted under a fluorescence microscope. The neutralization effect was evaluated by calculating the percentage reduction of the green fluorescence cell number in serum sample wells infected with pseudotyped virus in comparison to that in wells with mock group serum samples infected with the same dose of pseudotyped virus. [i.e. (the number of green fluorescence cells in control wells − the number of green fluorescence cells in sample wells)/(the number of green fluorescence cells in control wells) × 100%].
ELISPOT assay
Ten days after the final boost immunization with SARS CoV VLPs, interferon-γ (IFN-γ) and interleukin-4 (IL-4) were measured in splenocytes from spleens according to the manufacturer protocols (Mabtech AB, Stockholm, Sweden). Ninety-six-well nitrocellulose plates were coated with 100 μl/well of 5 μg/ml rat anti-mouse IFN-γ or IL-4 in PBS. Following overnight incubation at room temperature, the plates were then washed three times with PBS containing 0·25% Tween-20 and blocked with PBS containing 5% FBS for 2 hr at 37°. After three washes with PBS containing 0·25% Tween-20, 1 × 105 splenocytes in a 100 μl reaction volume containing 2 μg/ml recombinant S protein (the specific antigens), 5 μg/ml concanavalin A (positive control), or medium alone (negative control) were seeded to each well. Plates were then incubated overnight at 37° with 5% CO2 and washed with PBS. Biotinylated anti-mouse IFN-γ or IL-4 monclonal antibodies (mAbs_ at 1 : 500 dilution were added and plates were incubated for 2 hr at room temperature. After washing, avidin–horseradish peroxidase was added for 1 hr at room temperature. Following five washes with PBS, individual IFN-γ or IL-4 plates were developed as dark spots after a 10-min reaction with the peroxidase substrate-3-amino-9-ethylcarbazole (AEC). The reactions were stopped by rinsing the wells with demineralized water. Plates were air-dried at room temperature and read on an ELISPOT reader (Hitech Instruments, Luton, UK). Spot-forming cells (SFC) per 106 splenocytes were calculated. Medium backgrounds were consistently <10 SFC per 106 splenocytes.
Results
Production and characterization of SARS CoV VLPs
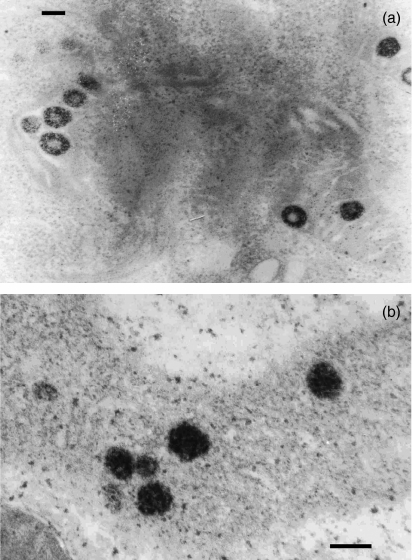
To study whether VLPs can form in insect cells, Sf21 cells were infected with recombinant baculoviruses vAcS and vAcME, respectively. Analysis of the cell sections infected with vAcS exhibited no particulate structures in the cytoplasm and nucleus. However, cells infected with recombinant viruses vAcME had large numbers of particulate structures distributed throughout the cytoplasm. As shown in Fig. 1(a), after infection of insect cells with recombinant baculovirus vAcME, which expresses E and M proteins, VLPs were observed in the cytoplasm at 96 hr post-infection, with a diameter of approximately 100 nm. The results demonstrated that M and E proteins were sufficient for the assembly of particles and that S alone could not assemble into VLPs.
Figure 1.
Electron microscopic analysis of VLPs in insect cells. (a) VLPs in the cytoplasm 96 hr post-infection with recombinant baculoviruses expressing M and E proteins. (b) VLPs in the cytoplasm 96 hr post-coinfection with recombinant baculoviruses vAcME, and vAcS expressing S protein. Bar = 100 nm.
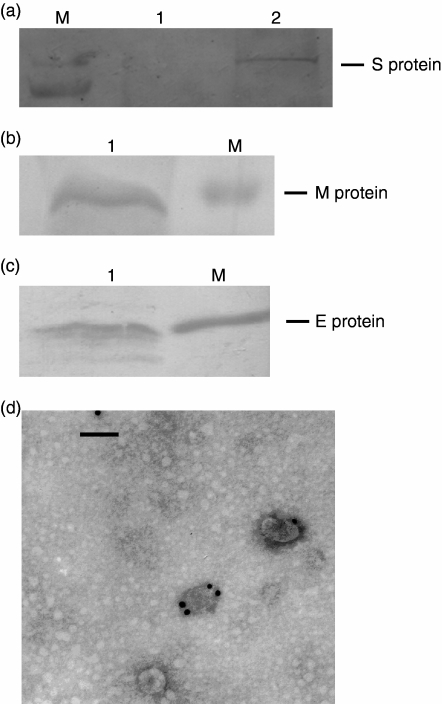
The S proteins contain important virus-neutralizing epitopes that elicit neutralizing antibody in the host species. To assemble S protein into VLPs for further usage as vaccine, insect Sf21 cells were coinfected with vAcME and vAcS at a MOI of 5. At 96 hr post-infection, the infected cells were harvested and VLPs were purified by sucrose gradient centrifugation. VLPs were observed in the cytoplasm of infected insect cells (Fig. 1b). To investigate whether the S protein was incorporated within the VLPs, purified VLPs were assessed by Western blot using SARS CoV S-protein-specific antibody. A distinct protein band of approximately 180 000 molecular weight corresponding to the SARS CoV S protein was detected, indicating that the S protein was assembled into the VLPs (Fig. 2a). In addition, two bands corresponding to M (Fig. 2b) and E (Fig. 2c) proteins were detected using antibodies against M and E protein, respectively. The results showed that SARS CoV VLPs contained S, M and E proteins.
Figure 2.
Analysis of SARS CoV VLPs. (a) Western blot analysis using rabbit anti-SARS S antibody: lane 1, vAcME-infected sf21 cells; lane 2, purified VLPs. (b) Western blot analysis using rabbit anti-SARS M antibody. Lane 1: purified VLPs; (c) Western blot analysis using rabbit anti-SARS E antibody: lane 1, purified VLPs. (d) Electron micrograph of immunogold-labelled purified SARS CoV VLPs (with vAcME and vAcS). VLPs were probed using a rabbit anti-SARS S antibody counterstained with gold spheres coupled to anti-rabbit IgG. Bar = 100 nm.
To further examine the morphology of VLPs and the location of the S protein in the particles, isolated VLPs were immunogold labelled with S-protein-specific antibody and observed by negative staining electron microscopy. Our results demonstrated the presence of the S protein on the surface of VLPs (Fig. 2d).
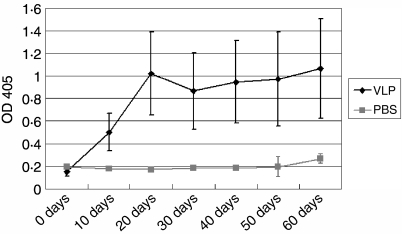
Detection of SARS CoV-specific antibodies
The immunogenicity of VLPs produced in insect cells was evaluated by immunizing mice. Mice were immunized via subcutaneous injection four times in 30 days; each time, with 100 μg SARS CoV VLPs. Serum samples were collected before each immunization and the levels of antibody responses were determined by ELISA using inactivated SARS CoV as coating antigens. Our data demonstrated that the VLPs were highly immunogenic in mice. As shown in Fig. 3, 10 days after the priming, an increase in antibodies was observed in the sera of immunized groups. The antibody titres in immunized groups peaked 10 days after the first boost (20 days after the prime). Antibody levels reduced slightly 10 days after the second boost (30 days after the prime). Antibody levels began to increase again after the third boost (40 days after the prime) and reached a plateau 60 days after the prime. The quantity of antibody production and the time for antibody level maintenance showed typical characteristics of the humoral immune response. The results showed that SARS CoV VLPs can induce high levels of SARS-CoV-specific antibodies in mice. Antibody titres in control groups remained at baseline throughout the study.
Figure 3.
The time–course of humoral immune responses to SARS CoV stimulated by VLPs. Mice (five per group) were each immunized with 100 μg SARS-CoV VLPs or PBS alone at days 0, 10, 20 and 30.
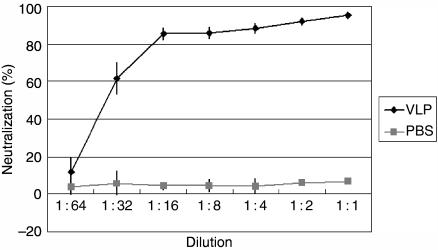
Neutralizing activity assay
SARS CoV infection is initiated by the attachment of the S protein to the cellular receptor ACE2. To detect the neutralizing activity of sera from immunized mice, Vero-E6 cells were challenged with MLV (SARS) pseudotypes. As shown in Fig. 4, sera from VLP-immunized mice exhibited a concentration-dependent neutralizing activity, and the neutralization reached 90% at dilutions of 1 : 8, whereas sera from the control mice did not show any significant neutralizing activity.
Figure 4.
Neutralization of SARS CoV S protein pseudotyped MLV by sera from mice immunized with PBS or SARS-CoV VLPs. The percentage reduction of green cell number compared to that in the control wells was calculated as described in the Materials and methods.
Characterization of the cellular immune response to SARS CoV
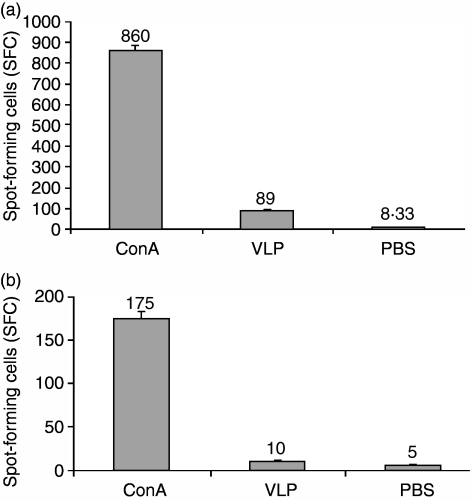
Immune responses in vaccinated mice were further investigated by measuring cytokine production. The type of immune response was determined by measurement of IFN-γ, a marker for T helper type 1 (Th1) responses, and IL-4, for Th2 responses. As shown in Fig. 5(a), immunization in mice with SARS CoV VLPs resulted in approximately a 10-fold increase in the number of IFN-γ-secreting splenocytes compared to those in mice immunized with PBS. Our data also indicated that IL-4 production was significantly less than IFN-γ in splenocytes isolated from immunized mice (Fig. 5b), suggesting a cellular response with Th1 bias.
Figure 5.
SARS CoV S protein-specific IFN-γ and IL-4 ELISPOT in lymphocytes. (a) IFN-γ production; (b) IL-4 production. SFC per 106 cells.
Discussion
Most of the reported SARS vaccines belong to inactivated virus vaccines and subunit vaccines.19,20 To make an inactive virus vaccine, native viruses needed to be grown on a large scale, and then must be isolated and inactivated with chemical agents. These processes are expensive, laborious and risky because of the need to grow and handle large quantities of infectious virus. Therefore, the inactive virus strategy is limited in its applications by safety considerations. In contrast, the subunit vaccine is a safer approach. The most important advantage of subunit vaccine is that the infectious virus can be entirely excluded from vaccine production, and consequently the risks associated with the production and reversion to virulent genotypes can be entirely eliminated. However, some subunit vaccines based on recombinant proteins are poorly immunogenic because of incorrect folding of the target protein or poor presentation to the immune system. As a specific class of subunit vaccine, VLP-based vaccines are currently under investigation for several human viruses, such as papillomavirus,21 bluetongue virus,22 hepatitis virus,23 rotavirus24 and influenza virus.25,26 These studies demonstrate that VLPs offer a promising approach to recombinant vaccine development because of their robust immunogenicity, their ability to elicit protective neutralizing antibodies and their advantageous safety profiles.
The baculovirus expression vector system has been extensively used for producing virus-like particles. So far, more than 30 different VLPs of human and animal viruses, including SARS CoV, have been obtained.27,28 The VLPs are used to investigate virus assembly, protein interaction, vaccines, and as delivery vectors. The current study investigated the assembly of SARS CoV VLPs in insect cells using recombinant baculoviruses. We constructed recombinant baculoviruses containing the SARS CoV E and M genes, and then infected insect cells to examine the minimum requirements for VLP formation. Our results showed that the E and M proteins coexpressed in insect cells generated VLPs, which exhibited spheriform structures resembling SARS CoV virions. This phenomenon resembles the findings of previous studies on other coronaviruses.12 In our study, we used VLPs not only to investigate the assembly and budding of SARS CoV particles but also to determine the possibility of their application as a SARS CoV vaccine. Therefore, we intended to incorporate the S protein into VLPs. The S protein is the receptor binding protein, playing a crucial role in viral infection, and it is the main target for neutralizing antibody vaccine design. Upon coinfecting insect cells with vAcME and vAcS, we demonstrated that SARS CoV VLPs formed and were visible in infected cells when viewed under a electron microscope. To confirm that the S protein is incorporated into the VLPs, the VLPs were examined under the electron microscope by immunogold labelling. The electron microscope results showed that VLPs were tagged along with gold-conjugated immunoglobulin G, indicating that S proteins were assembled into the VLPs. Successful incorporation of the S protein onto the surface of the VLPs makes it possible to use such VLPs as vaccines against SARS CoV.
To further investigate the immunogenicity of VLPs, mice were immunized with purified VLPs. Serum were collected at 10-day intervals post-immunization and tested by ELISA to examine the time–course of the change in neutralizing antibody titre. Our observations of immunogenicity in mice showed that SARS CoV VLPs induced high levels of neutralizing antibody. From the dynamic variation of specific antibody titres, the booster immunizations played important roles in the generation of high levels of specific antibodies. Neutralizing activity analyses against S protein pseudotyped MLV showed that VLP-induced neutralizing antibodies neutralized ∼60% infectivity of MLV (SARS) pseudotypes at 1 : 32 dilutions and ∼90% at 1 : 8 dilutions. Apart from the humoral response, SARS CoV VLPs also induced a Th1-dominated immune response. Immunity associated with a Th1-type immune response is thought to be essential for the control of intracellular pathogens; therefore, changing the bias of the immune response may be an attractive feature of a SARS CoV VLPs vaccine.
Previous studies on SARS CoV VLPs focused on the assembly of virions and did not investigate their immunogenicities.27,28 We report here on the construction of SARS CoV VLPs, their immunogenicities, and their potential for use as an anti-SARS vaccine. Our results showed that SARS CoV VLPs produced in insect cells can induce a cellular immune response and neutralizing antibodies against SARS CoV protein. The non-replicative nature and the lack of viral genomic RNA make VLPs safe for broad and repeated application. VLPs can be repeatedly administered to vaccinate individuals29 and thus represent an attractive vaccine strategy against SARS infection.
Acknowledgments
This work was supported in part by the National 973 and 863 grants (nos 2005CB523000 and 2005AA219070) from the Ministry of Science and Technology, China and an EU grant (DISSECT no.SP22-CT-2004–511060). We thank Tsanan Giroglou from Georg-Speyer-Haus, Institute for Biomedical Research, Germany, for providing the pMP71-eGFP-pre, pSV-Mo-MLV gagpol and pHMV-SARS S CD 19 plasmids. We thank Lin-fa Wang from the Commonwealth Scientific and Industrial Research Organization (CSIRO) Livestock Industries, Australian Animal Health Laboratory, Geelong, Australia for providing the S protein-specific antibody. We thank Dr Qinxue Hu for his critical reading of the manuscript.
Abbreviations:
- ACE2
angiotensin-converting enzyme 2
- CoV
coronavirus
- ELISA
enzyme-linked immunosorbent assay
- IFN-γ
interferon-γ
- IgG
immunoglobulin G
- IL-4
interleukin-4
- MLV
murine leukaemia viruses
- MOI
multiplicity of infection
- PBS
phosphate-buffered saline
- RBD
receptor-binding domain
- RT-PCR
reverse transcription polymerase chain reaction
- SARS
severe acute respiratory syndrome
- SFC
spot-forming cells
- VLPs
virus-like particles.
References
- 1.Ksiazek TG, Erdman D, Goldsmith CS, et al. A novel coronavirus associated with severe acute respiratory syndrome. N Engl J Med. 2003;348:1953–66. doi: 10.1056/NEJMoa030781. [DOI] [PubMed] [Google Scholar]
- 2.Drosten C, Gunther S, Preiser W, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. 2003;348:1967–76. doi: 10.1056/NEJMoa030747. [DOI] [PubMed] [Google Scholar]
- 3.Peiris JS, Lai ST, Poon LL, et al. Coronavirus as a possible cause of severe acute respiratory syndrome. Lancet. 2003;361:1319–25. doi: 10.1016/S0140-6736(03)13077-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marra MA, Jones SJ, Astell CR, et al. The genome sequence of the SARS-associated coronavirus. Science. 2003;300:1399–404. doi: 10.1126/science.1085953. [DOI] [PubMed] [Google Scholar]
- 5.Rota PA, Oberste MS, Monroe SS, et al. Characterization of a novel coronavirus associated with severe acute respiratory syndrome. Science. 2003;300:1394–9. doi: 10.1126/science.1085952. [DOI] [PubMed] [Google Scholar]
- 6.Bonavia A, Zelus BD, Wentworth DE, Talbot PJ, Holmes KV. Identification of a receptor-binding domain of the spike glycoprotein of human coronavirus HCoV-229E. J Virol. 2003;77:2530–8. doi: 10.1128/JVI.77.4.2530-2538.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kubo H, Yamada YK, Taguchi F. Localization of neutralizing epitopes and the receptor-binding site within the amino-terminal 330 amino acids of the murine coronavirus spike protein. J Virol. 1994;68:5403–10. doi: 10.1128/jvi.68.9.5403-5410.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Babcock GJ, Esshaki DJ, Thomas WD, Jr, Ambrosino DM. Amino acids 270–510 of the severe acute respiratory syndrome coronavirus spike protein are required for interaction with receptor. J Virol. 2004;78:4552–60. doi: 10.1128/JVI.78.9.4552-4560.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li W, Moore MJ, Vasilieva N, et al. Angiostensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature. 2003;426:450–4. doi: 10.1038/nature02145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.He Y, Li J, Heck S, Lustigman S, Jiang S. Antigenic and immunogenic characterization of recombinant baculovirus-expressed severe acute respiratory syndrome coronavirus spike protein: implication for vaccine design. J Virol. 2006;80:5757–67. doi: 10.1128/JVI.00083-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Du L, He Y, Wang Y, et al. Recombinant adeno-associated virus expressing the receptor-binding domain of severe acute respiratory syndrome coronavirus S protein elicits neutralizing antibodies. Implication for developing SARS vaccines. Virology. 2006;353:6–16. doi: 10.1016/j.virol.2006.03.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Haan CA, Kuo L, Masters PS, Vennema H, Rottier PJ. Coronavirus particle assembly: primary structure requirements of the membrane protein. J Virol. 1998;72:6838–50. doi: 10.1128/jvi.72.8.6838-6850.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Surjit M, Liu B, Kumar P, Chow VT, Lal SK. The nucleocapsid protein of the SARS coronavirus is capable of self association through a C-terminal 209 amino acid interaction domain. Biochem Biophys Res Comms. 2004;317:1030–6. doi: 10.1016/j.bbrc.2004.03.154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kuo L, Masters PS. The small envelope protein E is not essential for murine coronavirus replication. J Virol. 2003;77:4597–608. doi: 10.1128/JVI.77.8.4597-4608.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Corse E, Machamer CE. Infectious bronchitis virus E protein is targeted to the Golgi complex and directs release of virus-like particles. J Virol. 2000;74:4319–26. doi: 10.1128/jvi.74.9.4319-4326.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baudoux P, Carrat C, Besnardeau L, Charley B, Laude H. Coronavirus pseudoparticles formed with recombinant M and E proteins induce alpha interferon synthesis by leukocytes. J Virol. 1998;72:8636–43. doi: 10.1128/jvi.72.11.8636-8643.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gibco BRL. BAC-TO-BAC Baculovirus Expression Systems. Carlsbad, CA: GibcoBRL; 2002. [Google Scholar]
- 18.Giroglou T, Cinatl J, Jr, Rabenau H, Drosten C, Schwalbe H, Doerr HW, von Laer D. Retroviral vectors pseudotyped with severe acute respiratory syndrome coronavirus S protein. J Virol. 2004;78:9007–15. doi: 10.1128/JVI.78.17.9007-9015.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Spruth M, Kistner O, Savidis-Dacho H, et al. A double-inactivated whole virus candidate SARS coronavirus vaccine stimulates neutralising and protective antibody responses. Vaccine. 2006;24:652–61. doi: 10.1016/j.vaccine.2005.08.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhou Z, Post P, Chubet R, Holtz K, McPherson C, Petric M, Cox M. A recombinant baculovirus-expressed S glycoprotein vaccine elicits high titers of SARS-associated coronavirus (SARS CoV) neutralizing antibodies in mice. Vaccine. 2006;24:3624–31. doi: 10.1016/j.vaccine.2006.01.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Evans TG, Bonnez W, Rose RC. A Phase 1 study of a recombinant viruslike particle vaccine against human papillomavirus type 11 in healthy adult volunteers. J Infect Dis. 2001;183:1485–93. doi: 10.1086/320190. [DOI] [PubMed] [Google Scholar]
- 22.Roy P, Bishop DH, LeBlois H, Erasmus BJ. Long-lasting protection of sheep against bluetongue challenge after vaccination with virus-like particles: evidence for homologous and partial heterologous protection. Vaccine. 1994;12:805–11. doi: 10.1016/0264-410x(94)90289-5. [DOI] [PubMed] [Google Scholar]
- 23.Jeong SH, Qiao M, Nascimbeni M, Hu Z, Rehermann B, Murthy K, Liang TJ. Immunization with hepatitis C virus-like particles induces humoral and cellular immune responses in nonhuman primates. J Virol. 2004;78:6995–7003. doi: 10.1128/JVI.78.13.6995-7003.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.O'Neal CM, Clements JD, Estes MK, Conner ME. Rotavirus 2/6 viruslike particles administered intranasally with cholera toxin, Escherichia coli heat-labile toxin (LT), and LT-R192G induce protection from rotavirus challenge. J Virol. 1998;72:3390–3. doi: 10.1128/jvi.72.4.3390-3393.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pushko P, Tumpey TM, Bu F, Knell J, Robinson R, Smith G. Influenza virus-like particles comprised of the HA,NA, and M1 proteins of H9N2 influenza virus induce protective immune responses in BALB/c mice. Vaccine. 2005;23:5751–9. doi: 10.1016/j.vaccine.2005.07.098. [DOI] [PubMed] [Google Scholar]
- 26.Galarza JM, Latham T, Cupo A. Virus-like particle (VLP) vaccine conferred complete protection against a lethal influenza virus challenge. Viral Immunol. 2005;18:244–51. doi: 10.1089/vim.2005.18.244. [DOI] [PubMed] [Google Scholar]
- 27.Huang Y, Yang ZY, Kong WP, Nabel GJ. Generation of synthetic severe acute respiratory syndrome coronavirus pseudoparticles: implications for assembly and vaccine production. J Virol. 2004;78:12557–65. doi: 10.1128/JVI.78.22.12557-12565.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ho Y, Lin PH, Liu CY, Lee SP, Chao YC. Assembly of human severe acute respiratory syndrome coronavirus-like particles. Biochem Biophys Res Comms. 2004;318:833–8. doi: 10.1016/j.bbrc.2004.04.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Koutsky LA, Ault KA, Wheeler CM, Brown DR, Barr E, Alvarez FB, Chiacchierini LM, Jansen KU. A controlled trial of a human papillomavirus type 16 vaccine. N Engl J Med. 2002;347:1645–51. doi: 10.1056/NEJMoa020586. [DOI] [PubMed] [Google Scholar]