Abstract
The comparability of studies of extra-articular proximal femur fractures is compromised by the lack of a widely accepted, simple classification system with clinical and prognostic relevance. The aim of the study is to define the complication profile as well as differences relating to age, gender and survival rate of simple trochanteric fractures, intertrochanteric comminuted and subtrochanteric fractures. Records of 335 consecutive patients were analysed. Patients had a median follow-up of 10 (1–56) months, and were treated operatively with three intramedullary nailing systems. Simple trochanteric fractures (n=67) show wound healing problems (1.5%). Median age is m/f 77(45–98) years/ 85(39–101), and two-year survival rate is m/f 50.3%/ 84.9%. Intertrochanteric comminuted fractures (n=204) show the highest complications (25%), 9.7% femoralhead perforations, 3.5% hardware related problems and 11.8% wound healing problems. Median age is m/f 75(41–94) years/ 85(54–100), survival rate is m/f 92.7%/ 66.5%. Complication rate is 17.0% in subtrochanteric fractures (n=64), no femoralhead perforation but 9.1% other hardware problems and 7.8% wound healing problems. Median age is m/f 72(24–91) years/ 83(38–99), survival rate is m/f 92.3%/ 67.9%. Females show higher complication rates compared to males (19% versus 10%). The three types of fractures show different patterns of complications, survival rates, age, and sex distribution.
Résumé
La comparaison des études sur les fractures extra-articulaires de l’extrémité supérieure du fémur sont compromises par l’absence d’une classification clinique et pronostique simple et largement acceptée. Le but de cette étude était de définir le profil des complications ainsi que les différences selon l’âge, le sexe, le taux de survie pour les fractures trochantériennes simple, les fractures intertrochantériennes comminutives et les fractures sous trochantériennes. Une série de 335 patients consécutifs, traités avec 3 systèmes de clou centro- médullaires, était analysée prospectivement avec un suivi median de 10 mois (1–56). Les fractures trochantériennes simple (n=67) avaient des problèmes de cicatrisation des parties molles (1,5%); respectivement Homme/Femmes, l’âge median était 77 ans et 85 ans et la survie à 2 ans 50,3% et 84,9%. Les fractures intertrochantériennes comminutives (n=204) avaient le plus de complications (25%): perforations céphaliques (9,7%), problèmes de matériel (3,5%), difficultés de cicatrisation de paroi (11,8%); respectivement H/F, l’âge median était 75 ans et 85 ans et la survie à 2 ans 92,7% et 66,5%. Les fractures sous trochantériennes (n=64) avaient 17% de complications :aucune perforation céphalique mais 9,1% d’autres problèmes liés au matériel et 7,8% de difficultés de cicatrisation de paroi; respectivement H/F, l’âge moyen était 72 ans et 83 ans et la survie 92,3% et 67,9%. Les femmes avaient un taux de complications plus élevé que les hommes (19% versus 10%). Les trois types de fractures montraient des caractéristiques différentes en termes d’âge, de sexe, de complications et de taux de survie.
Introduction
Complication rates of proximal femoral fixation procedures of between 10–25% revision operations are often reported [1, 2, 4, 7, 10, 15, 21, 23]. These rates are unacceptably high. General surgical complications, such as haematomas, seromas and infections, must be separated from specific technical problems, such as incorrect reduction and unsatisfactory hardware placement resulting in surgical revision. Hardware-related complications included femoral head perforation of the proximal screw, intra-operative femoral shaft cracks, and hardware breakage. Hardware dislocations and non-union [22, 25] also occurred.
In the past decades, several classifications of inter- and sub-trochanteric femur fractures have been published [8, 16–19, 24, 27]. As opposed to intra-articular proximal femur fractures, no simple, uniform classification has been established for clinical use or scientific purposes for extra-articular proximal femur fractures. At present, the most common classification in scientific investigations is the AO classification [19]. In clinical settings, fractures are primarily classified as stable and unstable intertrochanteric and subtrochanteric fractures. A clear definition with therapeutic and prognostic value of simple and complex fracture types does not exist. The clear distinction between intertrochanteric and subtrochanteric fracture types is just as unclear and leads to difficulties in clinical discussions, such as the comparison of the internationally published studies [2, 3, 21].
The aim of this study is the evaluation of complication rates of different types of proximal extra-articular femur fractures, and a definition of three different fracture types based on the distinguishing fracture characteristics, with clinical, therapeutic and prognostic relevance.
Materials and methods
We present the data of 335 (m=82/f=253) patients, who underwent nailing fixation of a proximal femur fracture in one of three accident-surgery hospitals between 1998 and 2003. Ten patients with incomplete records were excluded from a total of 345 consecutively operations. Three intramedullary nail systems were used (PFN n=124/ Synthes, Bettlach/ Swiss, gliding nail n=116/ Plus Orthopedics, Marl/ Germany and Gamma nail n=95/ Stryker, Mülheim/ Germany). A comparison between the nail systems is not an objective of this study.
The median follow-up time was 10 months (1–56 months) and included all dead patients. The (median) age of the total study population was 83 years, with a range from 24 to 101 years.
The medical records included the course of the operation, the in-patient stay, and the postoperative out-patient treatment. Follow-up was by questionnaire or by telephone interview. In view of the patients’ advanced age, contact was also made with the patients’ relatives, family doctor or other persons close to the patient, if necessary. Medical records of subsequent in-hospital treatment were also evaluated, if applicable.
The three fracture types were defined after reviewing all data of the study. During the study period all fractures were classified according to the AO system.
Statistical methods
Statistical analysis addressed the following questions:
The differences in the relative frequency of specific hardware-related complications, iatrogenic complications and wound healing problems in the three fracture types (assessed by Fisher’s exact test after combining fracture Types 2 and 3, because they did not differ with respect to the three complication rates, or with the likelihood-ratio test in the case of missing observations, as explained for question 3).
Differences in survival at 24 months depending on the fracture types and sex (according to the Kaplan--Meier method) together with their standard errors.
- Since some hardware related complications were only observed up to 12 months after the operation, the risk of complication had to be calculated for patients with a shorter follow-up time. This was achieved using a risk model which took into account missing observations due to loss of follow up. If c denotes the proportion of patients at risk for a complication and λ denotes the hazard rate for a complication for those who are at risk, the likelihood of the observations for a patient with time at risk Ti is calculated by the formula:
The two parameters λ and c and their 95% confidence intervals were estimated by maximum likelihood. Since there was no difference in the parameters between Type 2 and 3 fractures, the two groups were combined. There were no hardware related complications for Type 1 fracture. Therefore it was not possible to estimate both parameters using our model. We, therefore, assumed that the parameter λ was the same for Type 1 fractures in order to calculate the 95% confidence interval for the estimated value of zero % complications. The iatrogenic and the wound-healing complications all occurred so soon after the operation that this approach was not necessary.
Results
Three distinct types of fractures (Fig. 1) could be differentiated, with specific complication profiles concerning age and sex distribution (Fig. 2) and survival rates (Fig. 3). A total of 64/335 complications were observed, with surgical revision required in 60 patients (Table 1). Of the 64 complications, 0/67 in Type 1 fractures, 22/204 in Type 2 and 4/64 in Type 3 fractures were directly related to osteosynthesis hardware; among them were 17 femoral head perforations, one hardware dislocation and one implant fracture, five intra-operative shaft cracks and two pseudarthroses. Due to the small numbers, the total number of hardware related complications was used for further statistical calculations. Complicated wound healing was observed in 30 cases, of which 19 were haematomas and seromas, and 11 infections. Technical complications, such as incorrect reduction of the fracture or unfavourable implant placement, required eight revisions. They did not represent fracture-typical parameters and therefore were not taken into further consideration in the analysis. The same applied for four cases of postoperative femoral shaft fractures, which all occurred after new trauma.
Fig. 1.

Three types of extra-articular proximal femur fracture
Fig. 2.

Average age of male (y) and female (x) of subgroups Type 1, 2 and 3 fractures together with their 95% confidence limits
Fig. 3.
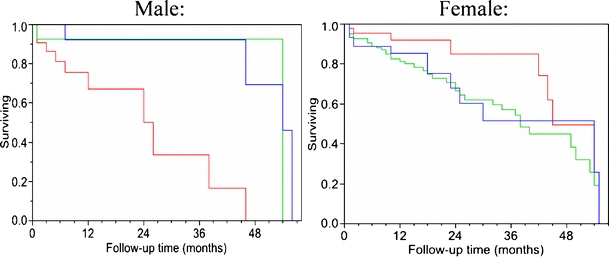
Kaplan--Meier curves for overall survival (m/ f by fracture Type 1(red)/2(green)/3(blue))
Table 1.
Total complications related to type of fracture, censoring ignored
| Type 1 | Type 2 | Type 3 | |
|---|---|---|---|
| n=67 | n=204 | n=64 | |
| Femur head perforation | – | 17/8.3% | – |
| Hardware dislocation | – | 1/0.5% | – |
| Shaft fracture | – | 3/1.5% | 2/3.1% |
| Pseudarthrosis | – | – | 2/3.1% |
| Hardware fracture | – | 1/0.5% | – |
| Haematoma | 1/1.5% | 15/7.4% | 3/4.7% |
| Infection | – | 9/4.4% | 2/3.1% |
| Osteosynthesis-caused | – | 22/10.8% | 4/6.3% |
| Wound healing | 1/1.5% | 24/11.8% | 5/7.8% |
| Iatrogenic | 4/5.9% | 3/1.5% | 1/1.6% |
| Total | 5/7.5% | 49/24.0% | 10/15.6% |
The complication rates of hardware related complications (p=0.0004), and wound healing problems (p=0.015) differed significantly between the two fracture types, with Types 2 and 3 combined due to a lack of difference between the two (Table 2), while femoral head perforation only occurred in Type 2 fractures. The hardware related complications occurred on average 5 months (95% confidence interval from 3 to 9 months) after the operation. In addition, seven complications were estimated to have been missed due to loss of follow-up.
Table 2.
Fracture type and complications, statistical analysis
| Type of complication | Type of fracture | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Type 1 (n=67) | Type 2&3 (n=268) | ||||||||
| N | % | LL% | UL% | N | % | LL% | UL% | ||
| Osteosynthesis-caused | 0 | 0 | 0 | 6.81 | 26 | 12.2a | 8.1 | 17.8 | 0.0004 |
| Wound healing | 1 | 1.5 | 0.04 | 8.04 | 29 | 10.8 | 7.4 | 15.2 | 0.015 |
| Total (patients) | 1 | 1.5 | 0.04 | 8.04 | 51b | 21.1a | 16.2 | 26.8 | <0.0001 |
aThe estimated complication rates take into account missing data.
bThe total for all patients is not the sum of all complications, because there are four patients with two complications, i.e., we compare the proportion of patients with at least one complication.
Definition of the fracture types/complication profile
Type 1- simple trochanteric femur fracture
Simple trochanteric fractures with sufficient support of the two main fragments exhibited a low complication rate in our data base following intramedullary osteosynthesis. This is a simple fracture in the cancellous metaphysis of the femur. The favourable complication rates were observed in all two- and three-segment fracture types. According to the AO classification, these are 31A1 simple fractures and fractures with a lesser trochanter fragment, according to AO 31A 2.1 or with a fracture of the greater trochanter.
We observed 67 Type 1 fractures (20.0%), (22 men/ 32.8%; 45 women/ 67.2%).
Patients with Type 1 fractures had a median age of 82 years (39–101 years). Men had a median age of 77 years (45–98 years), women 85 years (39–101 years).
The two-year survival rate in patients with Type 1 fractures was 73.9±8.1% (50.3±17.0% for men and 84.9±8.0% for women).
We observed no specific hardware-related complications. In 1.5% a postoperative haematoma required revision. No infection was observed. The overall complication rate for Type 1 fractures amounted to 1.5%.
Type 2- intertrochanteric comminuted fracture
This group included proximal femur fractures with fracture of both trochanters, in some cases combined with distally located fragments and extensive destruction. This group had the highest complication rates. The fractures were located in the cancellous metaphysis, with a possible extension into the cortical bone of the diaphysis. The Type 2 group includes AO fracture Types 31 A2.2, A2.3 and A3.3. The fundamental characteristic of this fracture type is the intertrochanteric comminution zone, which makes it impossible to support the two main fragments solidly during anatomical reduction.
With 204 cases (60.1%), this was the largest fracture group in this study (41 men/ 20.1%; 163 women/ 79.9%).
Patients with Type 2 fracture were 83.5 years old (41–100 years) in the median, men 75 (41–94) years, women 85 (54–100) years.
The two year survival rate in patients with Type 2 fractures was 71.6±4.8% (92.7±4.1% for men and 66.5±5.7% for women).
In Type 2 fractures, we observed 9.7% femoral head perforations. Implant dislocation was observed in 0.8%, and in 1.2% an implant fracture occurred. An intra-operative shaft fissure occurred in 1.5%. In this group we also observed haematomas in 7.4%, as well as wound infections in 4.4%.
As a whole, in Type 2 fractures specific hardware-related problems occurred in 13.2%, and wound healing difficulties in another 11.8%. This resulted in a total complication rate of 25.0%.
Type 3-subtrochanteric femur fractures
Proximal femur fractures, distal to the greater trochanter, i.e., diaphysal fractures within the cortical area of the proximal femur showed a different complication profile. In Type 3 fractures, there is a stable proximal main fragment consisting of the femoral head, femoral neck and greater trochanter; the course of the fracture can run proximal to the lesser trochanter as a reverse AO 31 A3.1 or traverse A3.2 fracture. Further, all fractures distal to the lesser trochanter are classified under this type.
Sixty-four patients (19.1%) were classified as Type 3 fractures; (19 men/ 29.7%; 45 women/ 70.3%). Patients with Type 3 fractures in the median were 81 years old (age range 24–99 years), men were 72 years (24–91 years), and women 83 years old (38–99 years).
The two-year survival rate in this group was 74.7±8.0% (92.3±7.4% in men, 67.9±10.4% in women).
Intra-operative femoral shaft fractures occurred in 3.1%, and a pseudarthrosis developed in 6.1%. We observed 4.7% haematomas and 3.1% infections in this group. Thus within the Type 3 fractures, we observed 9.2% specific hardware-related complications and 7.8% wound healing problems. This corresponded to an overall complication rate of 17.0%.
Age and gender as complication risk factors
The age groups 70–79 years and 80–89 years showed higher complication rates for specific hardware-dependent complications and femoral head perforations as opposed to<70 years and>89 years, but the differences were not statistically significant. Furthermore, women were more frequently affected by these complications than men (Table 3). The difference, however, also was not statistically significant. With respect to wound healing, we observed no age or sex-dependent differences.
Table 3.
Age, gender, complications, censoring ignored
| n | Osteosynthesis-caused (%) | Femoralhead-perforation (%) | Wound-healing(%) | |
|---|---|---|---|---|
| <70 years | 45 | 3 (6.7) | 3 (6.7) | 4 (8.9) |
| 70–79 years | 88 | 9 (10.2) | 7 (8.0) | 7 (8.0) |
| 80–89 years | 138 | 11 (8.0) | 5 (3.6) | 11 (8.0) |
| >89 years | 64 | 3 (4.7) | 2 (3.1) | 8 (12.5) |
| M | 82 | 2 (2.4) | 1 (1.2) | 6 (7.3) |
| F | 253 | 24 (9.5) | 16 (6.3) | 24 (9.5) |
Discussion
The indication for operative treatment of extra-articular proximal femur fractures is undisputed. This study demonstrated that, on the basis of the typical complication patterns, the fracture types could be divided into different statistically significant types. The different fracture forms exhibited a different sex- and age-dependent frequency peak in association with disconcordant survival rates. In the literature, this fact has found little consideration. For example, the quality of fracture reduction and implant placement has a direct influence on the femoral head perforation rate [5, 18, 20, 22]. According to our results, however, this dependency occurred only in intertrochanteric comminuted fractures. Thus, even studies with high levels of evidence [1, 23] must be questioned, because none of the applied classifications accounted for a sufficient division of the fracture types. The evaluation of treatment procedures, the quality assurance and the clinical discussion require a valid, simple classification of the fracture types. As opposed to other fractures, a classification of the proximal extra-articular femur fractures has not yet become generally accepted as demonstrated in a meta-analysis [3].
Fracture types, age, sex and mortality rate
Evidently, the impact of outside forces on bone as well as the bone architecture plays a role in the occurrence of the various fracture types. The structure of the bone in elderly individuals is mainly determined by the different degrees of osteoporosis. Singh (1970) showed changes of the trabecula structure of proximal femurs with increasing osteoporosis [26]. Another relevant fact is the cancellous architecture of the intertrochanteric bone as opposed to the cortical subtrochanteric bone. Besides the force of the trauma and the direction of the energy, the insertions of the large muscles, specifically the gluteus medius iliopsoas muscles in addition to the gluteus maximus, rectus femoris and the adductor muscles exert force on the femur. This muscle power alone can cause loads several times the weight of the body [6, 14]. During an accident, the total forces depend on the condition of the musculature as well as the spinal reflexes.
Our data concerning the type of fracture, age, sex and survival period lead to additional conclusions:
The estimated two-year mortality rate using the Kaplan--Meier method for men with Type 1 fracture was 49.7% as opposed to a 15.1% mortality rate for women. At the same time, the mean age of men was below that of women.
The mortality rate of men with Type 2 and Type 3 fractures (7.3% and 7.7%) was less than that of the men with Type 1 fractures (49.7%).
The mean age of men with Type 3 fractures (61.1 years) was clearly lower than inType 1 fractures (76.4 years) and in Type 2 fractures (72.7 years). The frequency peak of women with Type 1–3 fractures was almost constant at 82 years.
Women with Type 2 fractures had the highest mean age (83.5 years). At the same time, this group represented the largest fracture subgroup (47.2%).
According to these observations, the fracture pattern followed different mechanisms in men and women independent of the traumatic energy. We draw the following conclusions from our results:
Simple fractures of Type 1 have a 50% mortality rate in the follow-up examination period in men, with frequent terminal illness, indicating poor general physical condition. Low-energy trauma leads to a simple trochanteric fracture. Osteoporosis is less pronounced in men than in women and muscle contraction does not suffice to tear off an additional trochanteric fragment. The large muscles react to the fall, with delay due to physical decline and slow reflexes. In women with less muscle mass, the fracture can occur even with moderate osteoporosis, in which case the bone structure is still strong enough to prevent comminution of bone around the greater and lesser trochanter. Surgical treatment of these fractures has few complications [15] and results are largely independent of the internal fixation technique, as demonstrated by Ender (1970) on the basis of twelve different fixation methods for stable trochanteric fractures [11].
Type 2 fractures occur in men in better physical condition with higher traumatic energy. Due to the powerful muscle actions, the two trochanters avulse in addition to the main fracture. The survival prognosis is better. In women, the fractures occur on the basis of osteoporosis. Low-energy trauma leads to falls at old age; the osteoporotic bone tends to fracture with much comminution. This type of fracture affected the largest number of patients.
From the surgical point of view, the Type 2 fracture is the most problematic. Apart from a high rate of specific hardware-related complications (13.2%), we observed a high rate of wound healing complications (11.8%), more than third of which were due to infections.
Type 3 fractures occur in men of younger age and represent high-energy trauma; the cancellous bone is quite strong in the intertrochanteric area and the bone tends to fracture in the less stable subtrochanteric area. These fractures are not caused by osteoporosis.
Prior to the introduction of intramedullary fixation devices, the surgical treatment of subtrochanteric fractures with angled plates or dynamic hip screws was a difficult and complicated procedure [23, 24]. Experimental studies point to substantially higher stability of intramedullary devices [9, 12, 13], and clinical investigations demonstrate the advantages of intramedullary nails [23]. We observed specific surgery-related complications in 9.2% and wound healing problems in 7.8% of these patients. Femoral head perforation of the osteosynthesis material did not occur with this type of fracture, indicating strong cancellous structure in the femoral head and neck. In bones with a cortical architecture, pseudarthrosis can develop. Furthermore, the shaft can break when the nail is hammered into bone weakened by the fracture.
References
- 1.Adams CI, Robinson CM, Court-Brown CM, McQueen MM (2001) Prospective randomized controlled trial of an intramedullary nail versus dynamic srew and plate for intertrochanteric fractures of the femur. J Orthop Trauma 15:394–400 [DOI] [PubMed]
- 2.Al-yassari G, Langstaff RJ, Jones WM, Al-Lami M (2002) The AO/ ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury 33:395–399 [DOI] [PubMed]
- 3.Audige L, Hanson B, Swiontkowski MF (2003) Implant-related complications in the treatment of unstable intertrochanteric fractures: meta-analysis of dynamic screw-plate versus dynamic screw-intramedullary nail devices. Int Orthop 27:197–203 [DOI] [PMC free article] [PubMed]
- 4.Banan H, Al-Sabti TA, Jimulia T, Hart AJ (2002) The treatment of unstable, extracapsular hip fractures with the AO/ ASIF proximal femoral nail (PFN)- our first 60 cases. Injury 33:401–405 [DOI] [PubMed]
- 5.Baumgaertner MR, Curtin SL, Lindskog DM, Keggi JM (1995) The value of Tip-apex distance in predicting failure of fixation of peritrochanteric fractures of the hip. J Bone Joint Surg (Am) 77-A:1058–1064 [DOI] [PubMed]
- 6.Bergmann G, Deuretzbacher G, Heller M (2001) Hip contact forces and gait patterns from routine activities. J Biomechanics 34:859–871 [DOI] [PubMed]
- 7.Boldin C, Seibert FJ, Fankhauser F (2003) The proximal femoral nail (PFN)- a minimal invasive treatment of unstable proximal femoral fractures: a prospective study of 55 patients with a follow- up of 15 month. Acta Orthop Scand 74:53–58 [DOI] [PubMed]
- 8.Boyd H, Griffin L (1949) Classification and treatment of trochanteric fractures. Arch Surg 58:853–866 [DOI] [PubMed]
- 9.Curtis MJ, Jinnah RH, Wilson V, Cunningham BW (1994) Proximal femoral fractures: a biomechanical study to compare intramedullary and extramedullary fixation. Injury 25:99–104 [DOI] [PubMed]
- 10.Domingo LJ, Cecilia D, Herrera A, Resines C (2001) Trochanteric fractures treated with a proximal femoral nail. Int Orthop 25:298–301 [DOI] [PMC free article] [PubMed]
- 11.Ender J (1970) Probleme beim frischen per- und subtrochanteren Oberschenkelbruch. Hefte Unfallheilk 106:2–11
- 12.Friedl W (1993) Relevance of osteotomy and implant characteristics in inter- and subtrochanteric osteotomies. Arch Orthop Trauma Surg 113:5–11 [DOI] [PubMed]
- 13.Haynes RC, Pöll RG, Miles AW, Weston RB (1997) An experimental study of the failure modes of the gamma locking nail and AO dynamic hip screw under static loading: a cadaveric study. Med Eng Phys 19:446–453 [DOI] [PubMed]
- 14.Heller MO, Bergmann G, Deuretzbacher G (2001) Musculo-sceletal loading conditions at the hip during walking and stair climbing. J Biomechanics 34:883–893 [DOI] [PubMed]
- 15.Herrera A, Domingo LJ, Calvo A (2002) A comparative study of trochanteric fractures treated with the gamma nail or the proximal femoral nail. Int Orthop 26:365–369 [DOI] [PMC free article] [PubMed]
- 16.Jensen JS, Michaelsen M (1975) Trochanteric femoral fractures treated with McLaughlin osteosynthesis. Acta Orthop Scand 46:795–803 [DOI] [PubMed]
- 17.Jensen JS (1980) Classification of trochanteric fractures. Acta Orthop Scand 51:803–810 [DOI] [PubMed]
- 18.Kyle RF, Cabanela ME, Russel TA (1994) Fractures of the proximal part of the femur. J Bone Joint Surg 76-A:924–950
- 19.Müller ME, Nazarian S, Koch P (1987) The comprehensive classification of fractures of the long bones. Springer, Berlin Heidelberg New York, 120–121
- 20.Parker MJ (1992) Cutting-out of the dynamic hip screw related to its position. J Bone Joint Surg 74-B:625 [DOI] [PubMed]
- 21.Parker MJ, Handoll HH (2002) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures (Cochrane Review). Cochrane Database Syst Rev 1 [DOI] [PubMed]
- 22.Rosenthal RE (1996) Prevention of complications with the gamma nail. Am J Orthop 25:729 [PubMed]
- 23.Sadowski C, Lubbeke A, Saudan M (2002) Treatment of reverse oblique and transverse intertrochanteric fractures with use of an intramedullary nail or 95° screw-plate: a prospective, randomized study. J Bone Joint Surg 84-A:372–381 [PubMed]
- 24.Seinsheimer F (1978) Subtrochanteric fractures of the femur. J Bone Joint Surg 60-A:300–306 [PubMed]
- 25.Simmermacher RKJ, Bosch AM, Van der Werken Ch (1999) The AO/ ASIF- proximal femoral nail (PFN): a new device for the treatment of unstable proximal femoral fractures. Injury 30:327–332 [DOI] [PubMed]
- 26.Singh M, Nagrath AR, Maihi PS (1970) Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg 52-A:457–467 [PubMed]
- 27.Trozo RG (1973) Surgery of the hip joint. Lea and Febiger, Philadelphia


