Abstract
The successful outcome of total knee arthroplasty (TKA) is very much dependent on precise positioning of the components. Inaccuracy may result in complaints as well as in early mechanical failure. Between March 2003 and September 2005, 69 TKA procedures were performed by the computer navigated technique. The postoperative outcome of this cohort was compared with the same number of TKAs done by the traditional technique. The lower limb anatomical axis was determined in all cases pre- and postoperatively by weight-bearing anteroposterior (AP) and lateral full length X-rays. The positions of femoral and tibial components were recorded. Comparing the data in the navigation group on the AP view, 96.6% of femoral and 96.9% of tibial components and on the lateral view in 95.4% of femoral and in 95.4% of tibial components, the overall postoperative axis in 95.4% fell in the range considered in the literature as optimal. In the traditional group on the AP view, 75.7% of femoral and 68.1% of tibial components and on the lateral view 81.8% of femoral and 63.6% of tibial components, the overall postoperative axis in 60.6% fell between the values considered optimal in the literature. It seems to be proven that the computer navigated total knee arthroplasty technique ensures positioning of components significantly more precisely compared with the traditional surgical method. Accuracy of navigation depends on the software used, on the correct detection of anatomical reference points, and on a potentially uneven thickness of the cement layer during final insertion of the components. The computer navigated technique does not substitute professional skill and experience, since it merely transmits information for the surgeon. The decision is in the hands of the doctor during the entire procedure. The real benefits of the computer navigated technique require further research and can be determined only after long-term analyses.
Résumé
Le succés de l’arthroplastie totale de genou dépend beaucoup du positionnement des implants. Entre mars 2003 et septembre 2005, 69 athroplasties étaient réalisées avec une technique de navigation informatique. Le devenir de ce groupe était comparé avec le même nombre d’arthroplasties faites avec la technique traditionnelle. L’axe anatomique du membre inférieur était déterminé par des radiographies antéro-postérieures en charge et de profil en extension. Dans le groupe navigué, la position des implants était optimale sur les radio de face pour 96,6% des pièces fémorales, 96,9% des pièces tibiales, sur les radio de profil pour 95,4% des pièces fémorales et tibiales, avec un bon axe dans 95,4% des cas. Dans le groupe traditionnel, les chiffres étaient: 75,7% pour les pièces fémorales, 68,1% pour les pièces tibiales sur les radio de face et 81,8% pour les pièces fémorales, 63,6% pour les pièces tibiales sur les radio de profil avec un bon axe dans 60,6% des cas. Il semble prouvé que l’utilisation de la navigation informatique permette un meilleur positionnement des implants que la méthode conventionnelle. L’efficacité de la navigation dépend du logiciel utilisé, de la précision du repérage anatomique et éventuellement de l’épaisseur de la couche de ciment lors de l’implantation définitive. Cette technique ne remplace pas l’expérience du chirurgien mais transmet des informations fiables, les décisions restant entre les mains de l’opérateur pendant toute l’intervention. Le bénéfice réel sera établi après des études à long terme.
Introduction
Survival expectancy of total knee arthroplasty (TKA) is basically influenced by three factors: design of the implant, positioning of the components, and soft tissue balance. Prosthesis manufacturers have developed anatomical implants, and intra- and extramedullary aiming devices help the surgeon to position the components accurately. Success however is very much dependent on the doctor’s experience and skill. Inadequate insertion of components affects the soft tissue balance. These factors indicated the need for a system to assist in both proper positioning of the components and intraoperative analysis of soft tissue balance.
Computer-guided tomography (CT) requires preoperative CT images. Comparing the three-dimensional image with the identical anatomical reference points, the CT image and the limb of a given patient can be evaluated. With the help of the resultant three-dimensional image the bone resection planes can be determined.
Kinematical navigation does not require preoperative CT images. During the operation specific anatomical reference points are to be registered by infrared signalling transducers fixed into the femur and tibia. The surgeon sets the resection planes based on the graphic images produced by these transducers. Both systems only transmit information for the surgeon, but the decision is in the hands of the doctor during the surgical procedure.
In our department a kinematical navigation system was used to validate its usefulness, possible advantages and disadvantages, and its accuracy in TKA compared with the traditional surgical method.
Materials and method
Between March 2003 and September 2005, 69 TKA procedures were performed by the computer navigated technique at the Semmelweis University Orthopaedic Department, Budapest, Hungary. A total of 31 procedures were done on the right knee and 38 on the left knee in 47 female and 22 male patients whose average age was 69.4 (49–83) years. The control group contained 69 knees of 63 patients undergoing the traditional operation in the same time period. In this group there were 38 procedures on the right and 31 on the left knee in 51 female and 18 male patients. Their average age was 68.1 (50–85) years.
Patient selection for either the navigated or traditional (control) group was randomised. Before surgery all patients had weight-bearing anteroposterior (AP) and lateral full length lower limb X-rays. The preoperative anatomical axes of the lower limbs were determined. After the operation weight-bearing AP and lateral full extent lower limb as well as lateral femur and tibia X-rays were taken. The AP and lateral position of femoral and tibial components and the postoperative anatomical axis of the lower limbs were determined. The X-rays were taken with a standardised method and the pictures were evaluated.
By evaluating the X-ray images, the optimal range of components was determined referring to data from the literature [15]. The position was considered as optimal if the femoral component in the AP view was between 82 and 86°, in flexion-extension between 0 and 4°, the tibial component in the AP view was between 87 and 92°, its inclination between 0 and 5°, and the postoperative anatomical axis was between 5 and 10°.
By evaluating the resultant numerical data collected from both the navigated and traditional implanting procedures, the percentage of cases fitted in the optimal range were compared, and the standard deviation was established by means of statistical analyses and average surpass of optimal range in both of the groups. Complications were also recorded in both groups.
Stryker Scorpio prostheses were used in every case. Navigation procedures were carried out with the “Stryker Navigation System” developed by Leibinger (Fig. 1). This is a kinematical system, which does not necessitate a preoperative CT scan. At the beginning of our navigation procedures, the powered wireless signalling devices were fixed into the iliac crest, the femur, and the tibia, and they communicated with an infrared camera. The upgraded MS Windows-based software developed from 1.01 to version 2.0 no longer required the iliac crest signalling device. The reference area outlined by the signalling devices made it possible to assign the anatomical points required for navigation using the pointing device. The pushbuttons on the pointer provide the possibility for steering the program in any direction, and the surgeon does not need additional assistance. While registering anatomical reference points, first the centre of the hip joint is registered by its repeated movement. The centre of the knee joint at the level of the femur and tibia as well as the centre of the ankle joint and the aspect of the AP view of the joint are also to be registered. Using these data the mechanical axis of the limb can be determined.
Fig. 1.

Stryker kinematical navigation set
To establish the locations of the medial and lateral epicondyles of the femur, it is essential to determine Whiteside’s line as well as the AP axis of the tibia for rotational position of components. Clarifying the joint surfaces of the femur and tibia aids in establishing the level of resection of these bones. Having finished the entire registration, the system monitor provides means to control the preoperative axis and kinematics of the joint. During the resections the positions of resection blocks are adjustable, and the resected planes can be assessed. This system also assists in elaborating proper soft tissue balance.
Results
The average preoperative anatomical axis of the lower limbs was 5.2 ± 8.6° (10° varus-12° valgus) in navigated cases. In the cases treated traditionally (control group) the preoperative anatomical axis was 8 ± 7.99° (17° varus-28° valgus).
As far as the AP position is concerned, the femoral component was 83.9 ± 1.1° (82–87°) in the navigated cohort, and the average deviation from optimum was 0.001°; 96.6% of cases were found to be between the optimal limits.
In the control group the AP position of the femoral component was 84.7 ± 2.4° (80–93°), and the average deviation from optimum was 0.5°; 75.7% of cases were found to be between the optimal limits (Fig. 2).
Fig. 2.
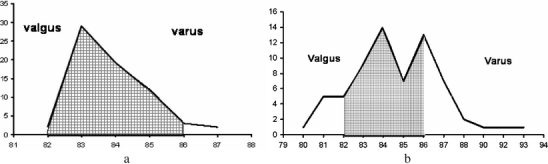
AP positioning of femoral component in navigated (a) and control (b) groups. Optimal range: 82–86°. The value registered in navigated cases was 83.9 ± 1.1° (82–87°); 96.6% in the optimal range. Average deviation from the optimal range was 0.001°. The value registered in the control group was 84.7 ± 2.4° (80–93°); 75.7% in the optimal range. Average deviation from the optimal range was 0.5°
Flexion-extension positioning of the femoral component was 0.8 ± 1.4° (−1–8°) in the navigated group, and the average deviation from the optimal range was 0.1°; 95.4% of all cases were found to be between the optimal limits.
In the control group this parameter was 2.4 ± 3.1° (0–15°), and the average deviation from optimum was 0.6°; 81.8% of cases were found to be between the optimal limits.
Regarding the AP position of the tibial component, it was 89.3 ± 1.1° (82–87°) in the navigated group, and the average deviation from optimum was 0.001°; 96.9% of cases were found to be between the optimal limits.
In the control cohort this parameter was 89 ± 2.8° (81–96°), and the average deviation from optimum was 0.6°; 68.1% of cases were found to be between the optimal limits (Fig. 3).
Fig. 3.
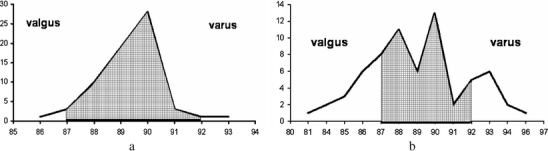
AP positioning of tibial component in navigated (a) and control (b) groups. Optimal range: 87–92°. The value registered in navigated cases was 89.3 ± 1.2° (86–93°); 96.9% in the optimal range. Average deviation from the optimal range was 0.001°. The value registered in the control group was 89 ± 2.8° (81–96°); 68.1% in the optimal range. Average deviation from the optimal was range 0.6°
Flexion-extension positioning of the tibial component was measured at 3.2 ± 1.5° (0–6°) in the navigated cohort, and the average deviation from the optimal range was 0.001°; 95.4% of all cases were found to be between the optimal limits.
In the control group this parameter was 4.7 ± 2.8° (−2–12°), and the average deviation from optimum was 0.6°; 63.6% of cases were found to be between the optimal limits.
Measuring the postoperative limb axis, in the navigated group it was 6.8 ± 1.3° (3–10°), and the average deviation from optimum was 0.1°; 95.4% of cases were found to be between the optimal limits. In the control group the axis was 6.4 ± 3.4° (−3–18°), and the average deviation from optimum was 1.0°; 60.6% of cases were found to be between the optimal limits (Fig. 4).
Fig. 4.
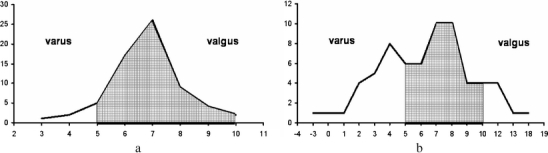
Postoperative anatomical axis in navigated (a) and control (b) groups. Optimal range: 5–10°. Values detected in navigated cases: 6.8 ± 1.3° (3–10°); 95.4% in the optimal range. Average deviation from the optimal range was 0.1°. Values detected in control cases: 6.4 ± 3.4° (−3–18°); 60.6% in the optimal range. Average deviation from the optimal range was 1.0°
Evaluating the positioning of prosthesis components, the average of the results of axial parameters was between the optimal limits in both the navigated and traditionally operated groups. The same was observed as far as the postoperative limb axis is concerned.
However, there was a difference in standard deviation between the two groups. The same result was observed related to the average deviation from the optimal range. Both of these differences were significant (p < 0.01).
One septic complication occurred in the navigated group which required a two-stage revision procedure. Two other complications were observed: one delayed wound healing and one deep vein thrombosis. In the control group one case of delayed wound healing occurred.
Discussion
Progress in medical science and technology produces more sophisticated knee prosthesis systems and easier and more precise implantation instruments.
Progress in knee replacements has been aided by precise knowledge of biomechanics of the knee joint. Apart from the material and shape of the implants, it has been apparent that precise positioning is essential regarding long-term survival [3, 5, 11, 15]. It is not always a simple goal to achieve, e.g., in cases of severe varus or valgus deformity, or extreme obesity of the patient [6]. The suboptimal lower limb axis or rotational malposition of components results in uneven load bearing, impairment of soft tissue balance, and ultimately in serious wear of polyethylene and early component loosening. Even if the positioning of components is precise, but soft tissue balance is incorrect, the survival of the prosthesis is jeopardized [9].
These demands indicated the need to devise computer-aided knee prosthesis navigation systems [4, 12], which have become more and more sophisticated ever since. First CT navigated systems were created, but they had the disadvantage of necessitating pre- and postoperative CT imaging. Later kinematical navigation systems appeared that did not require CT pictures. They were equipped with early software versions and communicated with the computer via a data cable. This was later changed to contemporary software and a wireless infrared communication system. The accuracy of the present systems has been extensively analysed in the literature [1, 7, 10, 12, 15].
Navigation has not been a widely accepted method; however, a number of publications appeared that reported on early experiences. The primary aim of our institution has been to examine the Stryker navigation system devised by Leibinger. Our experience commenced using software variety 1.1, which required three infrared signalling devices fixed by screws into the iliac crest, the distal femoral, and the proximal tibial bone. During surgery the traditional resection blocks were used. These facts required extended draping and one additional incision over the iliac crest, therefore prolonging the operation time. Today the sophisticated up-to-date resection templates do not require opening the medullary cavity, resulting in much less postoperative blood loss. Due to development of software the iliac crest signalling transducer has become redundant. These developments considerably reduced the operating theatre time and patients do not suffer from the infamous iliac pain.
Our outcome values match the values published in the literature [1–3, 13, 15]; AP and lateral positioning of knee prostheses was considerably more accurate compared with the traditional procedures. Checking our geometrical data after navigation aided operations: from the femoral components in the AP view 96.6% and in the lateral view 95.4%; from the tibial components in the AP view 96.9% and in the lateral view 95.4%. From the position of postoperative axis 95.4% of cases matched the range considered optimal by the present authors and the literature.
Following traditional TKA operations: from the femoral components in the AP view 75.7% and in the lateral view 81,8%; from the tibial components in the AP view 68.1% and in the lateral view 63.6%. From the position of postoperative axis 60.6% of cases fell between the optimal limits. Figures 2, 3, and 4 showing the numerical data on graphic tables illustrate widened Gauss curves in control groups.
The average of detected data fell into the optimal range in both groups; however, there was a difference in distribution (Table 1). The navigation method significantly decreased the extent of divergence from the average and from the optimal range, and almost entirely excluded results out of the optimal range. The few and insignificant inaccuracies may be the results of either incorrect registration or uneven cement layer, or minimal displacement of the transducer fixing screws. Inaccuracy may follow if the transducer’s battery is running down and an improper or weak signal is transmitted to the camera.
Table 1.
Detected and standard deviation values of navigated and control groups
| Preop. | Postop. | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AP axis | Femur AP | Femur lat. | Tibia AP | Tibia lat. | AP axis | |||||||
| Navigated | Average | SD | Average | SD | Average | SD | Average | SD | Average | SD | Average | SD |
| 5.2° | 8.6° | 83.9° | 1.1° | 0.8° | 1.4° | 89.3° | 1.2° | 3.2° | 1.5° | 6.8° | 1.3° | |
| Control | Average | SD | Average | SD | Average | SD | Average | SD | Average | SD | Average | SD |
| 2.9° | 7.99° | 84.7° | 2.4° | 2.4° | 3.1° | 89.0° | 2.8° | 4.7° | 2.8° | 6.4° | 3.4° | |
Postoperative control of rotational position can exclusively be established by postoperative CT, a test which was not considered to be ethical. In the literature a number of positive experiences have been published in this regard [3, 11].
In our opinion the greatest advantage of the navigation method is that the surgeon can assess the soft tissue balance and can also evaluate kinematics intraoperatively. In this procedure one can assess medial and lateral instability, and check rotation of the tibia.
Screws temporarily fixing the transducer devices caused no complications in our series. The tourniquet time was reduced to under 120 min after the first ten operations. Duration of the surgical procedure was not recorded because of continuous software upgrades.
The kinematical navigation system has a further advantage: it does not necessitate a preoperative CT scan image. It is more convenient for the patient, who is not subjected to extra radiation. On the other hand a CT scan would further increase the costs of this expensive system.
Long-term follow-up assessments will tell only in the future whether navigation has a positive effect on survival of knee prostheses [8, 9].
Considering and accepting the fact that the survival of knee prostheses is prolonged by optimal positioning and well-balanced soft tissues, a computer-assisted navigation method will fulfill these expectations.
One has to note that the computer-assisted navigation method is purely a tool; it does not replace the surgeon, but merely provides him/her with information, and the operating doctor evaluates this information. The machine cannot substitute knowledge and skill.
Regarding the future of knee prostheses, further development is expected in the field of computer-assisted navigation methods. An interweave of minimally invasive arthroplasty and navigation already indicates this progression [2, 14]. In such cases navigation can provide substantial aid to facilitate precision in a surgical area with limited vision. Our preliminary experiences are promising. Apart from this there are experiments using navigation methods in knee revision surgery [8].
The navigation methods furnish utmost assistance in cases of severe axial and post-traumatic deformities as well as in minimally invasive arthroplasties, and it may help during revision and perhaps can be used for training purposes.
References
- 1.Amiot LP, Poulin F (2004) Computed tomography-based navigation for hip, knee, and spine surgery. Clin Orthop 421:77–86 [DOI] [PubMed]
- 2.Archibeck MJ, White RE Jr (2004) What’s new in adult reconstructive knee surgery. J Bone Joint Surg Am 86-A:1839–1849 [DOI] [PubMed]
- 3.Chauhan SK, Scott RG, Breidahl W, Beaver RJ (2004) Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br 86-B:372–377 [DOI] [PubMed]
- 4.Delp SL, Stulberg DS, Davies B, Picard F, Leitner F (1998) Computer assisted knee replacement. Clin Orthop 354:49–56 [DOI] [PubMed]
- 5.Engh GA (2003) The difficult knee: severe varus and valgus. Clin Orthop 416:58–63 [DOI] [PubMed]
- 6.Foran J, Mont MA, Etienne G, Jones LC, Hungerford DS (2004) The outcome of total arthroplasty in obese patients. J Bone Joint Surg Am 86-A:1609–1615 [DOI] [PubMed]
- 7.Jenny JY, Boeri C (2003) Total knee prosthesis implantation with a non-image-based navigation system: rationale, technique, case-control comparative study with a conventional instrumented implantation. Tech Orthop 18:160–166 [DOI] [PubMed]
- 8.Nizard R (2002) Computer assisted surgery for total knee arthroplasty. Acta Orthop Belg 68:215–230 [PubMed]
- 9.Porter ML, Gambhir AK, Pradhan N (2004) Image-guided surgery for total knee replacement. J Bone Joint Surg Am 86-A:1096 [DOI] [PubMed]
- 10.Sparmann M, Wolke B, Czupalla H, Banzer D, Zink A (2003) Positioning of total knee arthroplasty with and without navigation support. A prospective, randomised study. J Bone Joint Surg Br 86-B:830–835 [PubMed]
- 11.Stöckl B, Nofler M, Rosiek R, Fischer M, Krismer M, Kessler O (2004) Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop 426:180–186 [DOI] [PubMed]
- 12.Stulberg DS, Loan PB, Sarin V (2002) Computer-assisted navigation in total knee replacement: results of an initial experience in thirty-five patients. J Bone Joint Surg Am 84-A(Suppl 2):S90–S98 [PubMed]
- 13.Stulberg DS (2003) How accurate is current TKR instrumentation? Clin Orthop 416:177–184 [DOI] [PubMed]
- 14.Tria AJ Jr, Coon TM (2003) Minimal incision total knee arthroplasty: early experience. Clin Orthop 416:185–190 [DOI] [PubMed]
- 15.Victor J, Hoste D (2004) Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop 428:131–139 [DOI] [PubMed]


