Abstract
The management of fractures of the proximal shaft of the humerus has been evolving since the development of new techniques and new implants in recent years. It seems that this kind of fracture has an increasing incidence in the older, osteoporotic population. In the last 2 years, we have operated on 17 patients, with an average age of 65, who had proximal humeral shaft fractures treated by minimally invasive percutaneous osteosynthesis (MIPO) technique using the metaphyseal locking compression plate. Our study evaluated the surgical technique used and the outcome for these patients with regards to their range of movement and shoulder function. Our results showed that all the patients could achieve at least 140º of shoulder abduction in the first 6 months after the operation, except for three patients who had shoulder impingement. These patients had an average Constant score of 76.8. All fractures had bony union at 6 months, except one, which was probably due to poor reduction in the initial operation. Another complication that we encountered was radial nerve neuropraxia. The ways to prevent these complications are discussed. In conclusion, MIPO fixation using the metaphyseal locking compression plate is a good option for the management of proximal humeral shaft fractures. It provides early functional recovery, but we had to pay special attention to some of the surgical details in order to minimise complications.
Résumé
La prise en charge des fractures de la diaphyse humérale proximale s’est modifiée depuis le développement de nouvelles techniques et de nouveaux implants. La fréquence de ces fractures semble avoir augmentée dans la population agée et ostéoporotique. Au cours des 2 derniéres années nous avons opérés 17 patients de 65 ans en moyenne, par la technique de l’ostéosynthèse mini invasive per-cutanée (MIPO) en utilisant un plaque métaphysaire à vis verrouillées. Nos résultats montraient que tous les patients atteignaient au moins 140 degrés d’abduction dans les 6 premiers mois sauf trois patients qui avaient un conflit dans l’épaule. Le score de Constant moyen était de 76,8. Toutes les fractures étaient consolidées à 6 mois sauf une probablement à cause d’une mauvaise réduction initiale. La neuropraxie du radial était une autre complication rencontrée. La prévention de ces complications est discutée. Cette technique de traitement permet une récupération fonctionnelle rapide mais nécessite une grande attention des détails pour prévenir les complications.
Introduction
Fracture of the proximal shaft of the humerus is a very common orthopaedic problem, but is not an easy problem to tackle. Treating these fractures by conservative means by using a U-slab or hanging cast is a possible option, and these successful conservative treatments have been described in the literature over the past 20 years [3, 9, 10, 18].
However, in actual practice, treating these fractures using the conservative method requires a lot of patient compliance. Poor patient selection is another critical point leading to failure. Conservative treatment for obese patients and those with poor and fragile skin easily fails [17].
Antegrade nailing in treating proximal humeral shaft fracture was also well described in the literature. Successful treatment using nailing was shown to treat shaft fractures effectively [4, 5, 13]. However, a higher rate of non-union or failed fixation was also found in patients having proximal humeral shaft fractures fixed with nails [1, 16]. Ender nailing was also described in the literature for treating simple humeral shaft fractures in multiple trauma or unstable patients with less blood loss and short surgical time, but fracture comminution seemed to be a relative contraindication [4].
With advances in modern medical care, old people who are still very active can easily injure themselves because of increased outdoor activities. An increasing incidence of fractures of the humeral shaft with osteoporosis has been noticed in our society [15]. A better method of immobilisation is needed in this group of patients for the fracture, which is osteoporotic and known to heal slowly, and yet to decrease the chance of joint stiffness associated with long-term immobilisation.
On the other hand, for young fit patients, using cast immobilisation will require a prolonged period of rehabilitation. Both the shoulder and elbow will be stiff and difficult to mobilise after about 6 weeks of immobilisation. This group of patients may need to be absent from work for a very long time before they can join the work force in society.
With the advance of the new design of the locking plate system, especially the metaphyseal locking plate, those proximal humerus shaft fractures with poor bone quality can be stably fixed. The many reported successes using the minimally invasive plate osteosynthesis (MIPO) technique in treating long bone fractures in both the upper and lower limbs [2, 7, 8, 11, 12], has led us to treat these fractures in the last 2 years using locking plates with the MIPO technique.
This study is a retrospective study to evaluate the techniques and outcomes of those patients with proximal humeral shaft fractures treated by metaphyseal locking compression plates and the MIPO technique in the last 2 years. With regards to the outcome, we focused on the functional range of the shoulder, the time to achieve full recovery and the complications encountered.
Materials and methods
We included all the adult patients that had displaced proximal humeral shafts treated using the MIPO technique from July 2004 to March 2006. The indication for operating on these fractures was all displaced fractures of the proximal 1/3 shaft of the humerus. All patients with open injury, pre-existing nerve injury, multiple injury patients, or pathological fractures were excluded.
All of these fractures were treated using a locking compression plate inserted by the MIPO technique. These patients were then regularly seen in the clinic by one of the three surgeons with X-ray on follow-up. The range of movement of the shoulder of each patient was charted by the physiotherapist and occupational therapist. Their findings were confirmed by the surgeons during each follow-up.
Surgical technique
After general anaesthesia, the patient was put in a beach-chair position. A 5-cm incision was made at the anteromedial border of the deltoid muscle. The incision should be about 5-cm distal to the acromium. The dissection stopped when the sub-muscular plane was reached. The sub-muscular plane was also developed laterally underneath the deltoid muscle. Care must be taken to avoid injury to the axillary nerve. Another 5-cm incision was made over the lateral side of the distal shaft of the humerus. The brachialis muscle was split with blunt dissection. The distal end of the incision was limited by the anatomical course of the radial nerve. We used 8-cm from the lateral epicondyle as the landmark for the radial nerve where it pierces the lateral intermuscular septum and winds along the lateral border of the humerus. The nerve was usually not explored, and retraction was done gently. The muscle was split by blunt dissection until the periosteum was reached to avoid trapping the nerve between the plate and the bone.
The proximal fragment was usually positioned in an abducted and internally rotated position. Therefore, the assistant should align the fracture by abduction and internal rotation of the distal fragment to obtain a reasonable alignment. A sub-muscular tunnel can be developed by the plate itself with the 4.5-milimetre locking sleeve as the handle.
The metaphyseal locking compression plate (Synthes, Bettlach) was pre-contoured using the image intensifier. The proximal fragment was fixed with 3.5-mm locking screws, while the distal part by the 5-mm locking screws. The fracture reduction was confirmed with an image intensifier using both the anteroposterior and lateral views.
Usually, three to four 3.5-mm locking screws engaging six to seven cortices can be achieved and are good enough even for osteoporotic bone. The distal part can be fixed with two or more 5-mm locking screws engaging four or more cortices because it is in the diaphyseal area.
The final alignment of the fracture and the implant are checked under an image intensifier. A drain is optional. The wound is then sutured with subcuticular sutures. The patient is allowed to perform free active shoulder and elbow mobilisation the day after the operation. The patient is usually allowed to leave the hospital 2 to 3 days after the operation with an out-patient physiotherapy session.
Results
From July 2004 to March 2006, we treated 17 patients with proximal humeral fracture using the MIPO technique. There were seven male and ten female patients. The ages ranged from 42 to 82 years of age. The average age was 65. Fifteen of the patients have been followed up for at least 6 months. The range was from 6 to 24 months; the average was 15.4 months. All of the injuries were due to accidental falls. One patient was a victim of a road traffic accident (case 3), and one patient fell from a height of 5 feet (case 4). Ten cases involved the dominant side, while the other seven did not. All but one were mono-traumas, except for one patient who had a fracture of the neck of the femur (case 8).
According to the AO classification, three patients belonged to type A, nine patients belonged to type B, and five patients belonged to type C. All of the fractures mainly involved in the proximal 1/3 of the shaft. However, ten of them had fractures extending into the humeral neck area. Furthermore, of these ten patients, four had fractures extending into the greater tuberosity area (cases 1, 3, 8, and 9), and they all were AO classification type C fractures (Table 1).
Table 1.
Patient characteristics and results
| Case | Sex/age | Injury | Co-morbidities | R/L/dominant a | Neck involved | Tuberosity involved | AO class | Complication | FU/month b | 3 Month; flex/abd/ER/IR c | 6 Month; flex/abd/ER/IR | Constant score | Removal | 1 year |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F/72 | Fall | Nil | R/D | Yes | Yes | 12C3 | 24 | 150/170/50/T12 | 170/170/50/T5 | 95 | No | FROM d | |
| 2 | F/70 | Fall | Hypertension | R/D | No | No | 12A1 | 24 | 135/140/60/T12 | 170/170/50/T5 | 90 | No | FROM | |
| 3 | M/42 | RTA | Nil | L/N | Yes | Yes | 12C1 | Shoulder impingement | 22 | 105/95/0/L1 | 125/120/30/T11 | 72 | 16 months | FROM after removal |
| 4 | M/43 | Fall | Nil | L/N | No | No | 12B2 | 21 | 160/160/45/T8 | 160/160/50/T5 | 91 | No | FROM | |
| 5 | F/78 | Fall | Diabetes, hypertension | R/D | Yes | No | 12B1 | 18 | 110/100/15/L4 | 140/140/30/T10 | 84 | No | FROM (compare to L) | |
| 6 | M/74 | Fall | Hypertension | L/N | Yes | No | 12B2 | 18 | 160/160/45/T5 | 160/160/45/T5 | 87 | No | FROM | |
| 7 | M/44 | Fall | Nil | R/D | Yes | No | 12B1 | Impingement in neutral rotation | 18 | 140/100/30/T10 | 140/140/40/T4 | 71 | 16 months | FROM after removal |
| 8 | F/79 | Fall | Diabetes, hypertension | R/D | Yes | Yes | 12C1 | 17 | 100/95/10/L5 | 160/160/30/T6 | 66 | No | FROM | |
| 9 | F/82 | Fall | Diabetes, hypertension, Atrial fibrillation | R/D | Yes | Yes | 12C1 | Radial nerve palsy | 16 | 120/85/45/T12 | 130/85/45/T10 | 65 | No | Same as 6 months |
| 10 | F/59 | Fall | Nil | L/N | No | No | 12A1 | 12 | 120/120/30/T7 | 165/165/40/T7 | 95 | No | FROM | |
| 11 | F/80 | Fall | Pulmonary embolism | R/D | Yes | No | 12B1 | Radial nerve palsy; impingement | 10 | 90/70/20/L1 | 90/10020/L1 | 50 | No | Not done |
| 12 | M/44 | Fall | Nil | L/N | No | No | 12A2 | Radial nerve palsy | 9 | 130/13/40/T8 | 140/140/40/T4 | 89 | No | Not done |
| 13 | F/54 | Fall | Nil | L/N | Yes | No | 12B2 | 8 | 150/140/50/T8 | 150/140/60/T8 | 80 | No | Not done | |
| 14 | F/67 | Fall | Nil | R/D | No | No | 12B1 | Delay union; impingement | 8 | 90/90/20/L5 | 100/90/20/L1 | 46 | No | Not done |
| 15 | F/74 | Fall | Diabetes, hypertension | R/D | No | No | 12B1 | 6 | 80/80/15/L3 | 130/110/45/T10 | 71 | No | Not done | |
| 16 | M/80 | Fall | Alzheimer’s, carcinoma of prostate | L/N | Yes | No | 12C1 | 3 | 90/85/45/L3 back to Spain | 58 (3/12) | No | Not done | ||
| 17 | M/57 | Fall | Diabetes, chronic renal failure | R/D | No | No | 12C1 | 3 | 160/145/20/T8 | 89 (3/12) | No | Not done |
aRight/left/dominant
bFollow-up/month
cFlexion/abduction/external rotation/internal rotation
dFull range of movement
Regarding the range of shoulder movement, 94% of the patients had achieved at least 90 degrees of abduction by 3 months. At 6 months, all patients could achieve up to around 140° of abduction, except for three that had impingement symptoms (cases 3, 11, and 14). All ten patients that had been seen for 1 year could achieve a full range of movement, except one patient (case 9). The flexion range was usually better and more quickly achieved compared to the abduction range. All patients complained of no pain or only mild pain on exertion.
Regarding the functional assessment of the affected shoulder, the Constant score was used to evaluate the shoulder function at 6 months postoperatively. The highest score was 95, and the lowest score was 46. The lowest three scores (including cases 11 and 14) that were less than 60 belonged to the patients with complications like shoulder impingement or radial nerve palsy. The overall average score at 6 months postoperatively was 76.8. Generally speaking, the patients who were older, tended to have slower and poorer recovery. In the younger patient group, the average score in 6 months was 83. The presence of co-morbidities seemed not to be an adverse factor to rehabilitation. This was well demonstrated in case 17 where the patient could achieve a Constant score of 89 at 3 months postoperatively, even though he had diabetes and chronic renal failure. There were a few complications seen in our series. There were four cases (cases 3, 7, 11, and 14) of shoulder impingement causing restriction of abduction. Two of them achieved a full range of movement after the implants were removed (cases 3 and 7). These two cases were the only two cases that had implants removed. There was one delayed union complicated by loosening (case 14). However, the patient was symptom free.
There were three cases of radial nerve neuropraxia (cases 9, 11, and 12). One patient (case 12) recovered in 4 months, the other one (case 11) recovered in 6 months, and the last patient (case 9) needed 8 months for complete recovery.
Discussion
It is a well known fact that we are getting better medical care each day, and our average life expectancy is getting longer. It had come to our attention that there is an increasing incidence of osteoporotic fractures in healthy old people. Moreover, fracture patterns that used to be due to relatively high energy, like humerus shaft fracture, now appear in the older population because of osteoporosis. With the advance of the new locking plate design, we found that using a metaphyseal locking plate is particularly useful in those proximal humeral fractures, especially with osteoporotic bone. The development of the MIPO technique and bridging plate osteosynthesis have helped a great deal in better and faster healing in osteoporotic fractures.
Although conservative treatment continues to be one of the most commonly accepted forms of management for humerus shaft fracture, problems usually arise when the fracture occurs at the proximal third of the shaft of the humerus. This is because the strong deltoid muscle tends to displace the proximal fragment in abduction. Simply by placing a U-slab or a hanging cast, it is very difficult to reduce the abducted proximal fragment. In our locality, because of the humid and hot conditions, the use of a cast or slab is sometimes quite troublesome and unacceptable to patients. It sometimes leads to complications like skin irritations or pressure sores around the axilla and chest region. Also, the use of immobilisation can lead to stiffness in the shoulder and elbow. This is especially true in our group of patients, who are generally older patients. Therefore, it is not hard to believe that most of our patients are very accepting of this surgical treatment.
Intramedullary nailing is one of the treatment options in proximal humeral shaft fractures. However, it had been shown that this treatment carries a slightly higher risk of failed fixation, especially in comminuted and osteoporotic patients [4, 17]. Besides, if the fracture extends into the tuberosity of the proximal humerus, antegrade nailing is technically not feasible because of the fixation problem. Shoulder pain related to the insertion of the nail is also a common complication that is still unsolved [4]. Non-union or delayed union was also relatively common and required revision with bone grafting [4]. In order to achieve primary bone healing, anatomical reduction and plating are required. This process is slow and usually inevitably means extensive soft tissue dissection. On the other hand, secondary bone healing by callus formation is fast and effective, but the use of casting, Ender nails, or interlocking nails still have their own weaknesses that have not been resolved [4]. In view of these problems, plating with the MIPO technique seems to be a reasonable and feasible option in treating fractures of the proximal third of the shaft.
The use of bridging plate osteosynthesis has been discussed and described recently in the literature to fix the humerus shaft fracture with good results [5, 11]. Nevertheless, the instrument used was still the ordinary dynamic compression plate (DCP) or low contact dynamic compression plate (LC-DCP). In our series, the average age was 65, with the oldest patient being 82 years old. With the use of the locking plate, nearly all fractures healed uneventfully. There was no early loosening of the implant due to failure of fixation. Although we had one case of delayed union in a 67-year-old lady, the patient is symptom free regarding the delayed union area. We have analysed the problem in this case; the reason was likely due to the poor reduction of the fracture. Since the fracture was a simple short wedge, the mal-reduction left a large fracture gap which would inevitably lead to delayed union, especially when the fixation was very stable. The patient was initially reluctant to have a revision of the fixation despite the fact that we explained to her about the possible risk. She finally agreed to surgery, and the non-union site was bone grafted one month ago. We are still following up her progress.
At the 1-year follow-up, all patients except one patient, who is the oldest (case 9) in our study could achieve a full range of movement. She is an 82-year-old lady with multiple medical problems. She required long-term warfarin for her atrial fibrillation, and she also had a history of multiple transient ischaemic attacks. These problems might have contributed to her poor rehabilitation, especially in the first few months, because she could not attend physiotherapy on a regular basis. Unfortunately, she also had radial nerve palsy postoperatively. This would usually lead to delayed rehabilitation.
Although we found that most of the patients could achieve a reasonable range within 3 to 4 months, there was one complication that needs to be discussed. In cases 3, 7, 11, and 14, the patients had impingement of variable severity. The incidence of this problem was quite high when we compared our results with the others [5, 11]. Probably, it was because nearly all of our fractures involved the proximal humerus. Therefore, the plate we used tended to be placed more proximally in order to have a more stable fixation in the proximal fragment. The more proximally the plate goes, the higher the chance that the plate may hit the acromium during abduction. In our series, this problem was solved simply by removing the plate early. Since these patients were moving their shoulders after the operation, rehabilitation after removal was not difficult, and they could all achieve a full range soon after the removal. In the future, with more confidence in the locking plate, it could be placed more distally to prevent this complication, while good fracture stability is still achievable. This problem was dramatically illustrated in both patients 3 and 7 (Fig. 1). With special attention to this point, we had very good results in our patients with the operation done just 3 months earlier (Fig. 2).
Fig. 1.
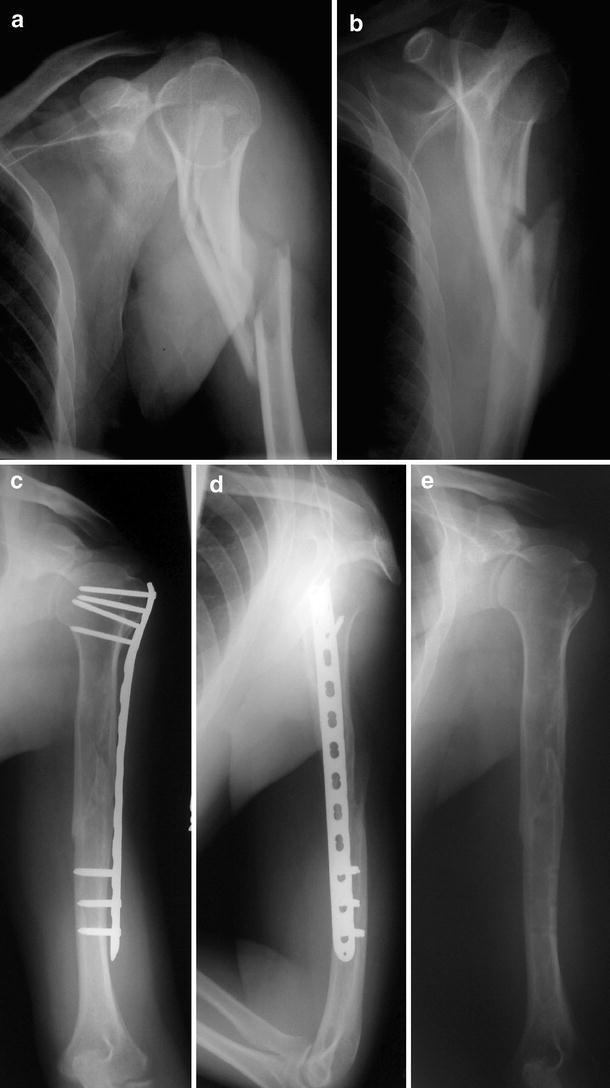
a, b: AP and lateral X-ray showing fracture of the left proximal shaft of the humerus (12-C1). c, d: AP and lateral X-ray of the humerus 6 months after the operation. Notice that the proximal tip of the plate is just short of the greater tuberosity. e: X-ray after removal of the plate showing complete fracture union of the humerus, and the patient could achieve full abduction after 2 weeks of self-mobilisation exercise
Fig. 2.
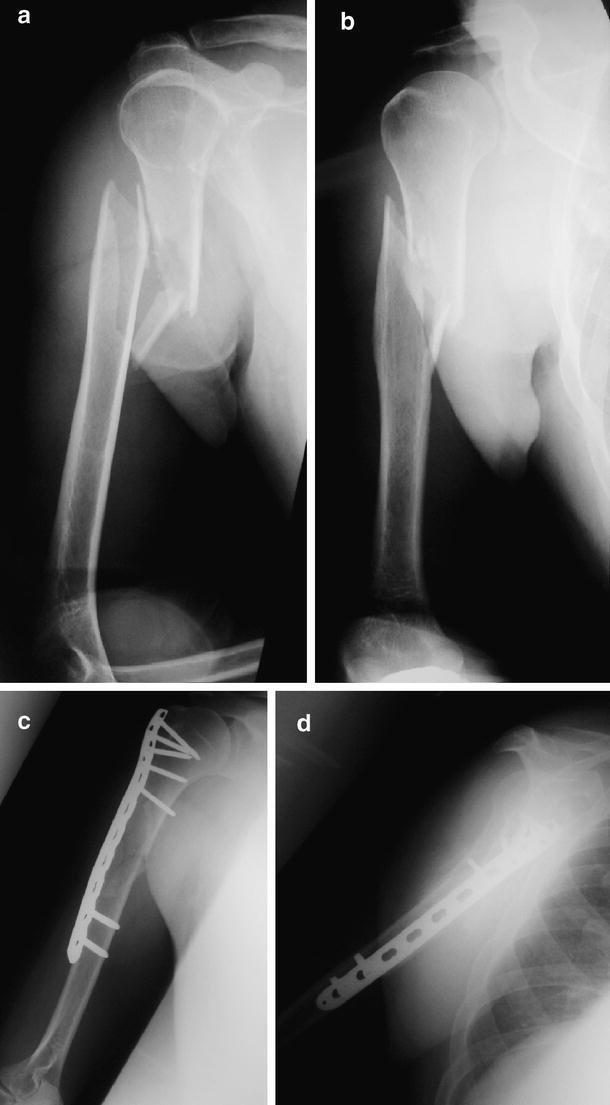
a, b: AP and lateral X-ray of the right humerus showing 12-C1 fracture of the proximal shaft of humerus. c, d: AP and lateral X-ray of the right humerus 6 weeks after operation
Putting the plate on the lateral side of the humerus is especially helpful in reducing the proximal humerus shaft fracture because most have an abducted proximal fragment. Actually, the proximal approach was similar to that described by Fernandez [3]. We think that by approaching the proximal part just anterior to the deltoid muscle, would cause the least risk to the axillary nerve. The distal approach is not described by others using the MIPO technique [1, 11]. An anterior plating technique is used in these papers in order to avoid the radial nerve. We think that the anterior plating technique is best for the mid-shaft of the humerus. However, for the proximal shaft, we think that anterior plating will pose extra technical difficulties in reduction and fixation, and lateral plating using our technique is helpful and efficient.
The anatomical landmark of the radial nerve is well described in papers and texts. Usually, we would use 8 cm from the lateral epicondyle as the lowest point that the plate can reach. Otherwise, the plate may have a very high chance of catching the radial nerve. Although we tried our very best to avoid this complication, we still encountered three cases of neuropraxia of the radial nerve (cases 9, 11, and 12) despite careful placement of the plate. For these three patients, the radial nerve recovered spontaneously. The younger patient needed 4 months to have full recovery, while the oldest one needed 8 months. We suggest that this problem was very likely due to the traction of the nerve during fixation of the distal part of the plate. Therefore, we strongly advise that extra attention has to be paid for retraction as well as the fixation of the distal part of the plate.
Conclusion
With the advance of the MIPO technique and locking plate design, the surgical treatment using internal fixation is now gaining ground in managing these fractures. Our study showed that the MIPO technique not only provides a fast and good functional recovery so that patients can get back to their normal life as soon as possible, but the locking plate design also helps in difficult situations, like osteoporotic fractures, that used to be impossible to fix surgically. We recommend this as an effective option, though careful technique and patient selection are crucial.
References
- 1.Ajmal M, O’Sullivan M, McCabe J, Curtin W (2001) Antegrade locked intramedullary nailing in humeral shaft fractures. Injury 32(9):692–694 [DOI] [PubMed]
- 2.Apivathakakul T, Arpornchayanon O, Bavornratanavech S (2005) Minimally invasive plate osteosynthesis (MIPO) of the humeral shaft fracture. Is it possible? A cadaveric study and preliminary report. Injury 36:530–538 [DOI] [PubMed]
- 3.Camden P, Nade S (1992) Fracture bracing of the humerus. Injury 23:245–248 [DOI] [PubMed]
- 4.Chao TC, Chou WY, Chung JC, Hsu CJ (2005) Humeral shaft fractures treated by dynamic compression plates, Ender nails and interlocking nails. Int Orthop 29(2):88–91 [DOI] [PMC free article] [PubMed]
- 5.Crates J, Whittle AP (1998) Antegrade interlocking nailing of acute humeral shaft fractures. Clin Orthop Relat Res 350:40–50 [DOI] [PubMed]
- 6.Fernandez Dell’Oca AA (2002) The principle of helical implants. Unusual ideas worth considering. Injury 33(Suppl 1):SA1–SA27 [DOI] [PubMed]
- 7.Gardner MJ, Griffith MH, Lorich DG (2005) Helical plating of the proximal humerus. Injury 36:1197–1200 [DOI] [PubMed]
- 8.Helfet DL, Shonnard PY, Levine D, Borrelli J Jr (1997) Minimally invasive plate osteosynthesis of distal fractures of the tibia. Injury 28(Suppl 1):42–48 [DOI] [PubMed]
- 9.Hunter SG (1982) The closed treatment of fractures of the humeral shaft. Clin Orthop 164:192–198 [PubMed]
- 10.Koch PP, Gross DF, Gerber C (2002) The results of functional (Sarmiento) bracing of humeral shaft fractures. J Shoulder Elbow Surg 11(2):143–150 [DOI] [PubMed]
- 11.Krettek C, Gerich T, Miclau T (2001) A minimally invasive medial approach for proximal tibia fractures. Injury 32(Suppl 1):SA4–SA13 [DOI] [PubMed]
- 12.Krettek C, Schandelmaier P, Miclau T, Tscherne H (1997) Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in the proximal and distal femoral fractures. Injury 28(Suppl 1):A20–A30 [DOI] [PubMed]
- 13.Lin J, Hou SM (1999) Antegrade locked nailing for humeral shaft fractures. Clin Orthop Relat Res 365:201–210 [DOI] [PubMed]
- 14.Livani B, Belangero WD (2004) Bridge plate osteoynsthesis of humeral shaft fractures. Injury 35:587–595 [DOI] [PubMed]
- 15.Nguyen TV, Center JR, Sambrook PN, Eisman JA (2001) Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the Dubbo Osteoporosis Epidemiology Study. Am J Epidemiol 153:587–595 [DOI] [PubMed]
- 16.Petsatodes G, Karataglis D, Papadopoulos P, Christoforides J, Gigis J, Pournaras J (2004) Antegrade interlocking nailing of humeral shaft fractures. J Orthop Sci 9(3):247–252 [DOI] [PubMed]
- 17.Ruedi T, Moshfegh A, Pfeiffer KM, Allgower M (1974) Fresh fractures of the shaft of the humerus. Conservative or operative treatment? Reconstr Surg Traumatol 14:65–74 [PubMed]
- 18.Sarmiento A, Kinman PB, Galvin EG, Schmitt RH, Phillips JG (1977) Functional bracing of fractures of the shaft of the humerus. J Bone Joint Surg Am 59(5):596–601 [PubMed]


