Abstract
The clinical results after total hip replacements using noncemented stems have shown considerable variability over the years; the design and characteristics of the implant seemed to play a role in explaining this fact. The purpose of this paper is to report the clinical, radiographic and densitometry results of total hip arthroplasties using a stem designed for noncemented implantation and to engage and load the femur proximally. Fifty-eight consecutive patients (62 hips) followed for an average of 4.3 years (range 36–70 months) were clinically and radiographically followed up at three weeks, three months, six months, one year, and yearly thereafter. The average pre-operative Harris hip score was 49 increasing to 98 at the latest follow-up. There were no cases of aseptic or septic loosening. The average subsidence at three years was 0.45 mm (SD ± 0.36 mm). Radiographically all hips were classified as stable, and evident changes compatible with new bone apposition were observed in 64% of the cases. The extended proximal geometry of the device seems to favour initial and secondary stability as reflected by the low subsidence values over time. The maintenance of periprosthetic bone stock and the absence of stress shielding can be explained by the predominantly proximal loading pattern of the stem.
Résumé
Les résultats cliniques des arthroplasties totales de hanche utilisant des tiges non-cimentées ont été très variables au cours des années, les caractéristiques de l’implant semblant jouer un rôle important. Le but de ce travail est de rapporter les résultats cliniques et radiologiques d’arthroplasties avec une tige non-cimentée avec appui proximal. 58 patients consécutifs (62 hanches) suivi en moyenne pendant 4,3 ans (36 à 70 mois) étaient étudiés à 3 semaines, 3 mois, 6 mois, 1 an puis tous les ans. Le score moyen de Harris pré-opératoire était de 49, augmentant à 98 au dernier examen. Il n’y avait pas de descellement aseptique ou septique. L’enfoncement moyen à 3 ans était de 0,45 mm (SD 0,36 mm). Radiologiquement toutes les hanches étaient stables et des modifications compatibles avec une ostéoformation était visible dans 64% des cas. La géométrie proximale de la tige semble favoriser la stabilité initiale et secondaire comme le montre le faible enfoncement au fil du temps. La conservation du stock osseux et l’absence de déviation des contraintes peuvent s’expliquer par la mise en charge proximale de la prothès.
Introduction
Even though the short-term results of porous-coated cementless hip replacements were promising [2, 8], subsequent follow-up studies have shown high incidences of thigh pain, subsidence of the femoral component, and aseptic loosening [19, 20, 23]. In addition, the proximal stress shielding associated with cylindrical, fully coated uncemented stems designed to engage the diaphysis exclusively have been of clinical concern, especially after the first decade of follow-up [4, 20].
From the design standpoint, several attempts have been made to maintain the loads proximally in the femur. The results associated with these stem designs are inconclusive, as suggested by the reported clinical results [6, 11, 13]. A novel cementless femoral stem designed to provide a more proximal metaphyseal fit by incorporating a lateral expansion in the proximal body (Revelation Hip System, Encore, Austin, TX) was developed based on biomechanical studies [9, 10]. These studies stressed the importance of the contribution of the soft tissues to the forces acting upon the hip and suggested the use of the lateral femoral cortex as an additional base of support for the stem.
The so-called lateral-flare stem was first custom manufactured beginning in 1992, and its clinical results in the young population are reported elsewhere [16] . The lateral flare stem was made available as a standardized off-the-shelf prosthesis in 1997. Even though the presence of a lateral flare is the prominent feature in both implants, several design characteristics were modified for the off-the-shelf stem used in the present study. The surface finish of the proximal third of the stem, which was HA-coated with proximal macro-grooves in the custom stems, was changed to a circumferential porous coating; a more aggressively tapered and polished distal stem (3°) and a fixed anteverted neck (12°) were also introduced.
We prospectively evaluated the short- to mid-term clinical and radiographic results in 58 consecutive patients (62 hips) after primary total hip arthroplasties using a porous-coated, lateral-flare hip stem. The emphasis of the present report is on the femoral component.
Materials and methods
Patients and demographics
Sixty-three patients who had undergone a primary total hip arthroplasty from January 1998 to December 2000 in our institution using a noncemented Revelation stem were followed. One patient died of unrelated causes two years after the surgery with an intact reconstruction and was not included in this study. Four additional patients were lost to follow-up despite several unsuccessful attempts at contacting them. The remaining 62 hips in 58 patients (30 men and 28 women) with an average age of 59 years old (range 27–79 years old) and a minimum of three years of follow-up (range 36–70 months) were studied. The preoperative diagnoses included primary osteoarthritis in 46 patients, avascular necrosis in seven patients, congenital hip dysplasia in three patients and post-traumatic osteoarthritis in two patients.
Surgical data
All operations were performed through a standard posterolateral approach that included splitting of the gluteus maximus, detachment of the short rotators and a T-shaped capsulotomy. The components were implanted without cement. The femur was prepared by straight reaming and implant-matched broaching to the templated size. The Revelation hip stem (Encore Orthopedics, Austin, TX) is made of titanium alloy (Ti6Al4V), porous-coated in the proximal one-third and has an extended proximal geometry (Fig. 1). The length of the stem from the medial femoral cut to the tip varies from 105–115 mm in the smaller sizes (sizes 9, 10.5, 12) to 120–130 mm in the larger stems (sizes 13.5, 15 and 16.5). The distal two-thirds of the stem is tapered (3°), polished, and intended to ensure proper alignment within the femoral canal, minimizing distal contact and load transfer. The anteversion is built directly into the neck of the stem (12°). In each case, and after insertion of the components, the capsule and the external rotators were re-approximated using heavy nonabsorbable sutures through drill holes on the greater trochanter. The patients are routinely allowed full weight-bearing immediately after the surgery (Figs. 2 and 3).
Fig. 1.

a The Revelation hip stem. Top-to-bottom view of the prosthesis: the anteverted neck and the plug-type trapezoidal proximal geometry can be appreciated. b The lateral flare designed to engage the proximal lateral cortex is the distinctive feature, along with a tapered, polished distal portion to minimize distal contact
Fig. 2.
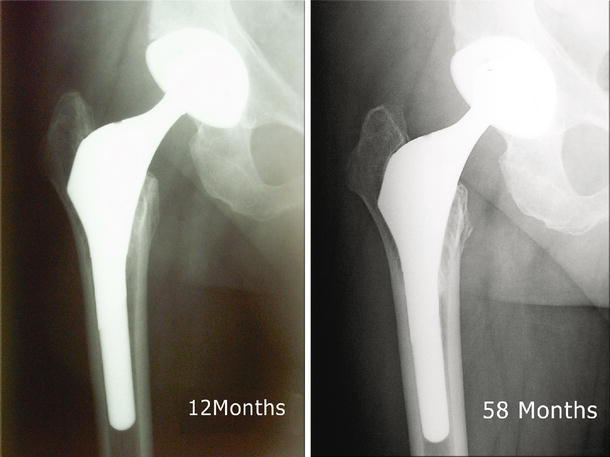
AP films of a 60-year-old male 12 and 58 months after a primary total hip replacement. The stem did not subside, and there is preservation of bone stock
Fig. 3.

View of the proximal stem and the bone response elicited in a 45-year-old patient 24 months after the primary total hip replacement
Clinical evaluations
Clinical evaluations were performed before the operation, three, six and 12 months after the surgery, and yearly thereafter. The Harris hip score (HHS) was used to evaluate the outcome of the operations. The changes in hip scores were evaluated with the Student t-test (statistical significance was determined at P < 0.05).
Radiographic evaluation
Radiographic evaluations were done preoperatively, at three months and yearly after the index operation. The axial migration of the stem was measured using a previously described method [26], which included digitization of the radiographs and measurement of the distance from the tip of the greater trochanter to a reference point in the stem. These were made from the outermost tip of the lateral flare of the prosthesis to a reproducible bony landmark in the greater trochanter present on both films. The vertical distance between the two points was then calculated on each film and the difference was considered as a measure of the subsidence of the prosthesis. Three different sets of readings were made on each digitized film by a single observer (AL). The reported subsidence represents the average value of each set of measurements. The intra-observer error was calculated to be 0.32 mm.
The immediate postoperative and last follow-up X-rays were evaluated. Anteroposterior and lateral films of the involved hip as well as anteroposterior view of the pelvis were assessed along with clinical follow-ups. The stems were rated stable (evidence of osseointegration with the absence of radiolucent lines) or unstable (change in the position, continuous or progressive radiolucent line or evidence of migration). The presence of pelvic or femoral osteolysis, progressive radiolucent lines, stress shielding, cancellous or cortical thickening and visible periprosthetic bone density changes was recorded according to the zones described by Gruen et al. [12]. Peri- and postoperative fractures were recorded. Radiolucencies with a scalloped or cystic appearance of greater than 2 mm in width were documented as osteolysis.
Results
Clinical results
The mean preoperative HHS was 47 (range 36–58, CI 95% ± 1.7), and at the latest follow-up the mean score was 97 (range 87–100, CI 95% ± 1.1). Three patients complained of mild thigh pain during the first year after the index surgery; the pain was reproduced with passive extension of the hip and flexion of the knee. There were no cases of thigh pain after the 12-month landmark. Two patients developed distal deep vein thrombosis, and one patient had delayed wound healing. There were no intraoperative fractures. One patient died of unrelated cause two years after the index operation.
There were no revisions performed for femoral osteolysis or aseptic loosening of the femoral component. Two patients suffered late peri-prosthetic fractures (at 24 and 62 months after the index surgery) after falls, both requiring subsequent open reduction and internal fixation surgery.
Radiographic results
All hips were classified as stable at the time of the latest follow-up with bone ingrown in the metaphyseal area accompanied by minimal axial migration (Figs. 2 and 3). There were no visible osteolytic lesions on the femur or the pelvis.
The average subsidence was 0.51 mm (SD ± 0.31 mm) at three years. All measured migration occurred within the first two years after the index operation. Two patients who suffered late peri-prosthetic fractures required revision of the femoral component during open reduction and internal fixation. The subsidence data for these two patients were included until the date of the occurrence of the fracture. Thus, these measurements reflect the amount of axial migration in all patients with intact femurs. None of the hips showed any visible osteolytic lesions.
Discussion
The clinical results of non-cemented, porous-coated femoral hip stems appear to be influenced by multiple factors: among them the initial stability achieved in the immediate postoperative period, the surface finish and the pore diameter. Since bone ingrowth is impaired by excessive micromotion at the bone-implant interface [14], attaining stability and minimal micromotion immediately after surgery becomes essential. The excellent clinical results reported in this series can be attributed to specific design features of this femoral component aimed at achieving early stability. A lateral flare extends the metaphyseal medial-lateral dimension of the device and as a result, the cross-sectional diameter of the stem exceeds the diaphyseal cross-sectional diameter, allowing for a broader base of support in the metaphysis. The lateral flare of the stem is specifically intended to engage the endosteal surface of the lateral femur at or above the intersection point of the mid-femoral-neck axis and the medial cortex of the femur simultaneously [9]. A polished and tapered distal stem is used to ensure proper alignment within the femoral canal, minimizing distal contact and load transfer. The absence of a collar is another design feature of relevance. Even though the use of a collar may increase the axial compression to the bone [5], it may impede the wedging effect of the lateral flare [18]. Its value as an additional feature to maximize prosthesis–bone contact in the primary setting is secondary to the stabilizing effect imposed by the extended proximal geometry of the implant [17] and the collar, therefore, is not a feature of the design of this stem.
The sturdy fixation achieved by engaging the metaphysis and loading the femur both medially and laterally creates an inherently stable construction [17, 24, 25]. The proximal anterior bow and the flat posterior surface create a trapezoidal proximal cross-section allowing for a near complete filling of the metaphysis in both the anterior–posterior and the medial–lateral planes. The circumferential porous coating proximally favours additional biological fixation. As a consequence, the average axial migration consistently remained under 1 mm after three years of follow-up.
One of the theoretical disadvantages of the proximally porous-coated and tapered stems is their potential for intraoperative fractures during insertion due to the amount of force applied to achieve a satisfactory and stable press fit [3, 21]. The present stem is not press-fitted into the femur or driven down the diaphysis to achieve interference fit; instead, the broaching and preparation of the femur creates the necessary contour in the metaphysis for the stem to be toggled down and gently tapped during insertion into its resting position upon the medial and lateral cortices (“rest fit”) [17].
A high prevalence of thigh pain has been reported after cementless total hip replacements [1–3, 7, 15, 20, 23]. The causes of such pain include instability of the stem and a tight distal fit of a rigid stem. The relatively low prevalence of thigh pain and its absence after the first year of follow-up in our study is, we believe, attributable to the axial and torsional stability of the implant.
We have previously reported prospective bone mineral density data in a group of patients after total hip arthroplasty using a lateral flare stem showing periprosthetic bone maintenance throughout the entire follow-up period. The design and geometry of the prosthesis play a role in the pattern or distribution of such loads along the femur [22, 24, 27], and it is safe to say that the early stability achieved with a lateral flare geometry and the maximization of load transfer to the proximal femur seem to explain the particular pattern of bone remodelling, with maintenance of bone mass in loaded areas (Wolff’s law).
Finally, when axial migration, bone preservation and clinical results are compared, the mid-term results of total hip arthroplasty with an off-the-shelf Revelation femoral component compare favourably with its earlier custom counterpart [17, 24, 25].
Footnotes
Level of evidence: Therapeutic study, level IV (case series).
References
- 1.Bourne RB, Rorabeck CH, Ghazal ME, Lee MH (1994) Pain in the thigh following total hip replacement with a porous-coated anatomic prosthesis for osteoarthrosis. A five-year follow-up study. J Bone Joint Surg Am 76:1464–1470 [DOI] [PubMed]
- 2.Callaghan JJ, Dysart SH, Savory CG (1988) The uncemented porous-coated anatomic total hip prosthesis. Two-year results of a prospective consecutive series. J Bone Joint Surg Am 70:337–346 [PubMed]
- 3.Capello WN, Sallay PI, Feinberg JR (1994) Omniflex modular femoral component. Two- to five-year results. Clin Orthop 298:54–59 [PubMed]
- 4.Claus AM, Hopper RH Jr, Engh CA (2002) Fractures of the greater trochanter induced by osteolysis with the anatomic medullary locking prosthesis. J Arthroplasty 17:706–712 [DOI] [PubMed]
- 5.Dorr LD, Wan Z (1996) Comparative results of a distal modular sleeve, circumferential coating, and stiffness relief using the Anatomic Porous Replacement II. J Arthroplasty 11:419–428 [DOI] [PubMed]
- 6.Duffy P, Sher JL, Partington PF (2004) Premature wear and osteolysis in an HA-coated, uncemented total hip arthroplasty. J Bone Joint Surg Br 86:34–38 [PubMed]
- 7.Engh CA, Bobyn JD, Matthews JG 2nd (1984) Biologic fixation of a modified Moore prosthesis. Part I. Evaluation of early clinical results. Hip 1984:95–110 [PubMed]
- 8.Engh CA, Massin P (1989) Cementless total hip arthroplasty using the anatomic medullary locking stem. Results using a survivorship analysis. Clin Orthop 249:141–158 [PubMed]
- 9.Fetto J, Bettinger P, Austin K et al (1995) Re-examination of hip biomechanics during unilateral stance. Am J Orthop 1995:605–612 [PubMed]
- 10.Fetto J, Leali A, Moroz A (2002) Evolution of the Koch model of the biomechanics of the hip: clinical perspective. J Orthop Sci 7:724–730 [DOI] [PubMed]
- 11.Giannikas KA, Din R, Sadiq S, Dunningham TH (2002) Medium-term results of the ABG total hip arthroplasty in young patients. J Arthroplasty 17:184–188 [DOI] [PubMed]
- 12.Gruen TA, McNeice GM, Amstutz HC (1979) “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res 141:17–27 [PubMed]
- 13.Hernandez-Vaquero D, Murcia-Mazon A, Paz-Jimenez J, Alegre-Mateo R, Martinez-Garcia J, Pena-Vazquez J (1999) Behavior of the femoral stem in the Bihapro hip prosthesis. Orthopedics 22:1049–1053 [DOI] [PubMed]
- 14.Kim YH, Oh SH, Kim JS (2003) Primary total hip arthroplasty with a second-generation cementless total hip prosthesis in patients younger than fifty years of age. J Bone Joint Surg Am 85A:109–114 [DOI] [PubMed]
- 15.Lavernia C, D’Apuzzo M, Hernandez V, Lee D (2004) Thigh pain in primary total hip arthroplasty: the effects of elastic moduli. J Arthroplasty 19:10–16 [DOI] [PubMed]
- 16.Leali A, Fetto J, Insler H (2006) Favorable midterm results of total hip arthroplasties with a lateral flare uncemented stem. Clin Orthop Relat Res (in press) [DOI] [PubMed]
- 17.Leali A, Fetto J, Insler H, Elfenbein D (2002) The effect of a lateral flare feature on implant stability. Int Orthop 26:166–169 [DOI] [PMC free article] [PubMed]
- 18.Markolf KL, Amstutz HC, Hirschowitz DL (1980) The effect of calcar contact on femoral component micromovement. A mechanical study. J Bone Joint Surg Am 62:1315–1323 [PubMed]
- 19.Martell JH, Galante JO, Pierson RH, Jacobs JJ, Rosenberg AG, Maley M (1992) Clinical experience with primary cementless total hip arthroplasty. Chir Organi Mov 77:383–396 [PubMed]
- 20.McAuley JP, Culpepper WJ, Engh CA (1998) Total hip arthroplasty. Concerns with extensively porous coated femoral components. Clin Orthop 355:182–188 [DOI] [PubMed]
- 21.Meding JB, Ritter MA, Keating EM, Faris PM (1994) Clinical and radiographic evaluation of long-stem femoral components following revision total hip arthroplasty. J Arthroplasty 9:399–408 [DOI] [PubMed]
- 22.Rosenthall L, Bobyn JD, Tanzer M (1999) Bone densitometry: influence of prosthetic design and hydroxyapatite coating on regional adaptive bone remodelling. Int Orthop 23:325–329 [DOI] [PMC free article] [PubMed]
- 23.Van Wellen P, Demuynck M, Haentjens P, De Valkeneer O, Casteleyn PP, Vanden Berghe I, Opdecam P, Kesteleyn P (1993) Total hip arthroplasty with the porous-coated anatomic (PCA) prosthesis: the femoral component. Acta Orthop Belg 59(Suppl 1):282–286 [PubMed]
- 24.Walker PS, Culligan SG et al (1999) The effect of a lateral flare feature on uncemented hip stems. Hip Int 9:71–80
- 25.Walker PS, Culligan SG, Hua J, Muirhead-Allwood SK, Bentley G (2000) Stability and bone preservation in custom designed revision hip stems. Clin Orthop 373:164–173 [DOI] [PubMed]
- 26.Walker PS, Mai SF, Cobb AG, Bentley G, Hua J (1995) Prediction of clinical outcome of THR from migration measurements on standard radiographs. A study of cemented Charnley and Stanmore femoral stems. J Bone Joint Surg Br 77:705–714 [PubMed]
- 27.Zerahn B, Storgaard M, Johansen T, Olsen C, Lausten G, Kanstrup IL (1998) Changes in bone mineral density adjacent to two biomechanically different types of cementless femoral stems in total hip arthroplasty. Int Orthop 22:225–229 [DOI] [PMC free article] [PubMed]


