Abstract
Twenty-five patients underwent scapulectomy for various tumours between 1989 and 2005. We describe 23 patients with scapular tumours who were followed-up for a minimum of 2 years after scapulectomy. The average age was 29 years, and two-thirds of the patients were male. Nineteen patients had malignant neoplasms, of which chondrosarcoma was most common, followed by Ewing’s sarcoma. Surgical staging was by Enneking’s system, with stage IIB being the most frequent. Fifteen patients underwent total scapulectomy, and the rest had their glenoid retained. With an average follow-up period of 66.7 months (23–202 months), functional and oncological outcomes were evaluated for all patients. Two patients had superficial wound infections requiring antibiotics, and one had skin necrosis requiring skin cover. Functional outcome was satisfactory in 13 patients. Cosmetically and emotionally acceptable surgery, scapulectomy made 19 patients continuously disease free, while four patients died of disease. The 5-year survival rate of 19 patients with malignant tumours was 75.9%. Retention of the glenohumeral articulation (subtotal) resection gives superior functional results.
Résumé
Etude de 23 patients opérés par scapulectomie pour tumeur entre 1989 et 2005 et suivi au minimum 2 ans. L’âge moyen était de 29 ans et 2/3 des patients étaient des hommes. La tumeur était maligne chez 19 patients, le chondrosarcome étant le plus frequent suivi par le sarcome d’Ewing. Le stade chirurgical était noté selon le système de Enneking, et le stade II B était le plus frequent. Quinze patients avaient une scapulectomie totale, les autres avaient la glène conservée. Avec un suivi moyen de 66,7 mois (23–202), le devenir fonctionnel et oncologique était évalué pour tous les patients. Deux patients avaient une infection superficielle et un autre une nécrose cutanée nécessitant une couverture chirurgicale. L’évolution fonctionnelle était favourable pour 13 patients. Esthétiquement et émotionnellement acceptable ces scapulectomies avaient pour résultats 19 patients indemnes de maladie tandis que 4 décédaient de la maladie. La survie à 5 ans des 19 patients avec tumeur maligne était de 75,9%. La scapulectomie sub-totale avec conservation de la glène donnait de meilleurs résultats fonctionnels.
Introduction
The shoulder girdle is the third most common site for tumours of bone and soft tissues and occurs in the proximal humerus, scapula and clavicle, in that order [1]. Most common tumours involving the scapula are round cell tumours, metastatic tumours and chondrosarcomas. There is a high incidence of malignant transformation of an osteochondroma in the shoulder girdle [10].
Forequarter amputation was considered an appropriate treatment for malignant tumours of the scapula and shoulder girdle. However, it is associated with significant morbidity in terms of the loss of the whole upper limb, severe cosmetic defect, phantom limb sensation and devastating psychological effects. Scapulectomy allows oncologically acceptable wide margins of resection without the need for amputation. Because the functional capacity of the upper limb is mainly centred on the hand, scapulectomy in carefully selected cases has a specific role in the management of tumours of the scapula.
Patients and methods
Between August 1989 and September 2005, 25 patients underwent scapulectomy for various tumours. We describe 23 patients with a minimum 2-years’ follow-up (Table 1). The age of the patients ranged from 3 years to 65 years. Eighteen patients were male and five were female. Patients presented to us with swelling, with or without pain, mostly involving the right scapula. Patients who had undergone primary humeral resections as part of a Tikhoff–Linberg [8, 11] procedure, shoulder fusion, or who had received some forms of allograft reconstruction or had a follow-up of less than 24 months, were excluded from the study.
Table 1.
Demographic details, diagnosis, stage and type of resection of 23 patients with scapular tumours (M male, F female, CS chondrosarcoma, FS fibrosarcoma, OS osteosarcoma, RCB recurrent chondroblastoma, AF aggressive fibromatosis, PC plasmocytoma)
| S. no | Age | Gender | Diagnosis | Stage | Type of resection |
|---|---|---|---|---|---|
| 1 | 33 | M | CS | II A | II A |
| 2 | 46 | F | FS | II A | II A |
| 3 | 3 | M | OS | II B | II A |
| 4 | 6 | M | ES | II B | III A |
| 5 | 56 | M | CS | II B | III A |
| 6 | 17 | F | ES | II B | III A |
| 7 | 54 | M | MET | NA | III A |
| 8 | 39 | M | CS | II A | II A |
| 9 | 25 | M | ES | III B | II A |
| 10 | 18 | M | OC | B3 | II A |
| 11 | 42 | M | RCB | B3 | III A |
| 12 | 25 | M | AF | B3 | III A |
| 13 | 14 | M | ES | II B | III A |
| 14 | 17 | M | CS | II B | II A |
| 15 | 13 | F | ES | II A | III A |
| 16 | 42 | F | PC | I A | III A |
| 17 | 16 | F | NF | B3 | III A |
| 18 | 64 | M | CS | I A | III A |
| 19 | 14 | M | CS | II B | III A |
| 20 | 31 | M | MET | NA | III A |
| 21 | 38 | M | CS | II B | II A |
| 22 | 65 | M | CS | II B | III A |
| 23 | 21 | M | ES | II B | III A |
Surgical staging was by Enneking’s [5] system, with plain radiographs, computerised tomogram (CT scan) and magnetic resonance imaging (MRI); stage IIB was encountered most commonly. Pre-operative histopathological diagnosis was reached with open biopsies in ten patients and by closed needle biopsies in 13. Nineteen patients had malignant neoplasms, of which chondrosarcoma was the most common, followed by Ewing’s sarcoma and cases of plasmacytoma, aggressive fibromatosis, recurrent chondroblastoma, solitary metastasis from adenocarcinoma of the lung (primary in remission) and neurofibroma (Table 1). One patient with a large osteochondroma underwent scapulectomy because of the size of the tumour. Two cases were of secondary chondrosarcoma arising from long-standing osteochondroma. The patients with aggressive fibromatosis and recurrent chondroblastoma presented to us after local resections had been done elsewhere.
Scapular resections were performed according to the system described by Malawer [5]. Eight patients underwent subtotal scapulectomy (type IIA) (Fig. 1), where the neck of the scapula and the glenoid were retained, and 15 patients underwent total scapulectomy (type IIIA) (Fig. 2). In all cases resections and primary soft tissue reconstruction were carried out as a single procedure. The deltoid and trapezius were sutured together and to the acromion process in type IIA resections. Teres minor and major were attached to the thoracic wall.
Fig. 1.
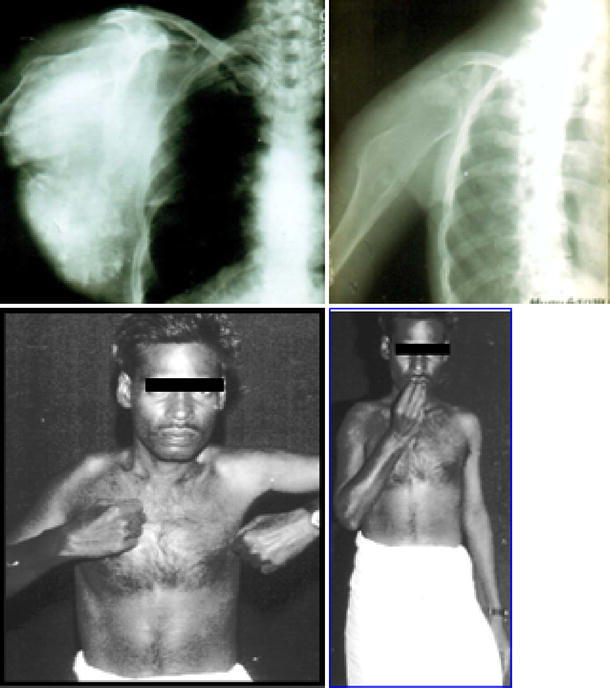
Top, left Pre-operative anteroposterior shoulder radiograph of a patient with chondrosarcoma of the right scapula. Top, right Post-operative radiograph of the same patient after type IIA resection. Bottom, left and right Sixteen-year follow-up picture of the patient, who has good functional results and is oncologically continuously disease free
Fig. 2.

Top, left Pre-operative anteroposterior shoulder radiograph of patient with metastasis in the scapula. Top, right Coronal T1-weighted MRI images of the shoulder showing the metastatic deposit involving the scapula. Bottom, left Post-operative anteroposterior shoulder radiograph of the same patient after type IIIA resection. Bottom, right Post-operative follow-up picture taken at the 1 year follow-up. Note a drooping of the shoulder. The patient died of disease at 23 months after surgery, due to pulmonary metastasis
Patients with Ewing’s sarcoma and osteosarcoma received neo-adjuvant chemotherapy. The drugs used were cisplatin, Adriamycin and ifosfamide with mesna for osteosarcoma; vincristine, Adriamycin, cyclophosphamide and actinomycin D for Ewing’s sarcoma. One patient underwent additional right upper lobectomy for solitary lung metastasis under cover of chemotherapy.
Patients were encouraged to begin passive motion in the early post-operative period as soon as pain relief was adequate. They wore a comfortable sling and were allowed to increase the activity as tolerated. They were persuaded to move the elbow, forearm and hand, to maintain normal function.
Results
The patients were followed-up monthly for the first 6 months and 6 monthly thereafter. With an average follow-up time of 66.7 months (range 23–202 months), the patients were examined for complications and functional and oncological outcomes.
Complications
There were no intra-operative complications. Two patients developed superficial wound infection, which settled with a course of antibiotics. One patient developed skin necrosis necessitating skin cover.
Functional outcome
Functional outcome was evaluated with Enneking’s modified system of functional evaluation of surgical management of musculoskeletal tumours [6]. This system rates combined range of movement at the shoulder, pain, stability, deformity, strength, functional activity and emotional acceptance. Four patients died during the follow-up period, and their functional results were recorded as those on their last follow-up visit. Cosmetically, all patients had loss of shoulder contour. Patients with type IIIA resections (total scapulectomy) had drooping of the shoulder. Restriction of shoulder abduction was the major functional limitation, but they had normal hand and wrist functions. Excellent functional rates were achieved in five patients, good in eight patients, fair in seven and poor in three (Table 2).
Table 2.
Follow-up, functional and oncological outcome of 23 patients after scapulectomy (CDF continuously disease free, DOD died of disease)
| S. no | Follow-up (months) | Complications | Functional outcome | Oncological outcome |
|---|---|---|---|---|
| 1 | 202 | Excellent | CDF | |
| 2 | 42 | Excellent | DOD | |
| 3 | 28 | Good | DOD | |
| 4 | 104 | Fair | CDF | |
| 5 | 103 | Wound infection | Poor | CDF |
| 6 | 93 | Fair | CDF | |
| 7 | 23 | Fair | DOD | |
| 8 | 91 | Good | CDF | |
| 9 | 32 | Good | DOD | |
| 10 | 84 | Excellent | CDF | |
| 11 | 81 | Good | CDF | |
| 12 | 76 | Good | CDF | |
| 13 | 76 | Good | CDF | |
| 14 | 76 | Good | CDF | |
| 15 | 68 | Wound infection | Fair | CDF |
| 16 | 67 | Fair | CDF | |
| 17 | 59 | Skin necrosis | Poor | CDF |
| 18 | 54 | Fair | CDF | |
| 19 | 53 | Poor | CDF | |
| 20 | 39 | Fair | CDF | |
| 21 | 30 | Good | CDF | |
| 22 | 30 | Excellent | CDF | |
| 23 | 25 | Excellent | CDF |
Oncological outcome
Three patients died from pulmonary metastases. One patient died from local recurrence and multiple metastases. Nineteen patients were continuously disease free at the time of their latest follow-up (Table 2). The 5-year Kaplan–Meier survival rates of 19 patients with malignant tumours was 75.9% (Fig. 3).
Fig. 3.
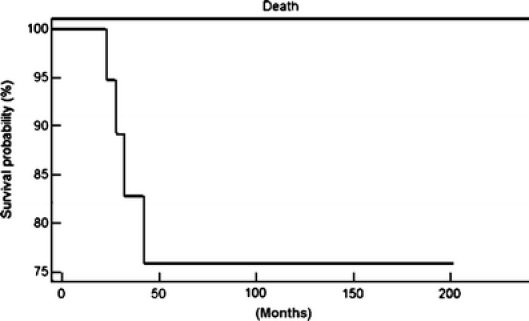
Kaplan–Meier curves showing the 5-year survival rate of patients with scapular tumours
Discussion
First mention of a scapular resection in the literature is of a partial scapulectomy performed by Lister [9] for an aneurysmal lesion of the subscapular artery. Syme, in his monograph, described scapulectomy for tumours of this region. However, scapulectomy fell into disrepute when De Nancrede [3] reported high local recurrence in his review of 65 scapulectomies for primary malignant tumours.
Various surgical options for scapular tumours have been described. Total scapular prostheses after resection of scapular tumours have been used, but the long-term results are not known [16]. Similarly, various allografts have been described [2, 12, 13] in the literature, but they are associated with problems such as graft fracture and collapse. The scapula can be considered as a sophisticated sesamoid bone in the muscles of the shoulder girdle [4]. Hence, after scapulectomy, if muscle envelope can be reconstructed and the glenoid fossa undisturbed, useful shoulder function may be expected. Functional outcome depends on the retention of the glenoid and reconstruction of muscles around the shoulder, namely the deltoid and trapezius.
Papaioannou and Francis [14] classified scapulectomies as partial, subtotal, near total, total and radical. They reported on 26 scapulectomies and opined that subtotal scapulectomy with retention of the glenohumeral joint resulted in better function. Samilson et al. [15] in 1968 reviewed 37 cases and agreed with them.
We used the surgical technique described by Malawer [10], which is based on the anatomical structure removed during operation. According to this system, scapular resections are classified into six types. Each type is further subdivided into two, according to status of the abductor mechanism: A, intact and B, partial or complete resection. Loss of the abductor mechanism usually results in some form of functional disability [10].
Even after total scapulectomy useful function of the upper limb can be retained, as the function of the upper limb is centred mainly in the elbow and hand. Retention of glenohumeral articulation is important for the function of the shoulder joint after scapulectomy [7]. Gibbons et al. [7] reported function after scapulectomy for neoplasms of bone and soft tissues. In their series of 14 cases they noted that resection of 80% of the scapula had only a modest effect on function. They also noted that subtotal scapulectomy gave an excellent functional result if all or part of the glenohumeral joint could be preserved.
Results fell into two main groups in our study, with type IIA resections showing superior shoulder function over type IIIA resections. Retention of the glenohumeral joint alone was significant, as the amount of the other part of the scapula resected had no significant effect on shoulder function. All eight patients with type IIA resection had excellent-to-good functional results, compared with only five patients (33%) with type IIIA resections.
Most of the patients were functionally and emotionally satisfied with the results. These patients had difficulty in abduction and flexion that rarely affected day-to-day activities. The reduced range of movement occurred because of loss of muscle bulk and bony leverage for muscle actions. The loss of abduction was not a major problem, as they learned to compensate with the opposite arm.
Scapulectomy is a more realistic limb salvage option for bone and soft tissue tumours around the shoulder girdle. It is emotionally and cosmetically acceptable in most patients. Our study confirms the notion that retention of the glenohumeral articulation (subtotal) resection gives superior functional results.
References
- 1.Creighton JJ, Peimer CA, Mindell ER, Boone DC, Karacousis CP, Douglass HO (1985): Primary malignant tumors of the upper extremity: retrospective analysis of one hundred twenty-six cases. J Hand Surg [Am] 10:805–814 [DOI] [PubMed]
- 2.Damron TA, Rock MG, O’Connor MI, Johnson M, An KN, Prtichard DJ, Sim FH (1998) Functional laboratory assessment after oncologic shoulder joint resections. Clin Orthop 348:124–134 [PubMed]
- 3.De Nancrede CBG (1909) The original results after total excision of scapula for sarcoma. Ann Surg 30:1–22 [DOI] [PMC free article] [PubMed]
- 4.DePalma AF (1954) Scapulectomy and a method of preserving the normal configuration of the shoulder. Clin Orthop 4:217–224 [PubMed]
- 5.Enneking WF (1983) Musculoskeletal tumour surgery, vol 1. Churchill Livingstone, New York, pp 355–410
- 6.Enneking WF (1987) Modification of the system for functional evaluation of surgical management of musculoskeletal tumours. In Bristol-Myers/Zimmer Orthopaedic Symposium. Limb salvage in musculoskeletal oncology. Churchill Livingstone, New York, pp 626–639
- 7.Gibbons CL, Bell RS, Wunder JS, Griffin AM, O’Sullivan B, Catton CN, Davis AM (1998) Function after subtotal scapulectomy for neoplasm of bone and soft tissue. J Bone Joint Surg Br 80:38–42 [DOI] [PubMed]
- 8.Linberg BE (1928) Interscapulo-thoracic resection for malignant tumours of the shoulder joint region. J Bone Joint Surg 10:344–349 [PubMed]
- 9.Lister R (1820) Ossified aneurysmal tumour of subscapular artery. Edinb Med J 16:66–70
- 10.Malawer MM (1991) Tumours of the shoulder girdle. Technique of resection and description of a surgical classification. Orthop Clin North Am 22:7–35 [PubMed]
- 11.Malawer MM, Sugarbaker PH, Lampert M, Baker AR, Gerber NL (1985) The Tikhoff–Linberg procedure: report of ten patients and presentation of a modified technique of tumours of the proximal humerus. Surgery 97:518–528 [PubMed]
- 12.Mnaymneh WA, Temple HT, Malinin TI (2002) Allograft reconstruction after resection of malignant tumours of the scapula. Clin Orthop 405:223–229 [DOI] [PubMed]
- 13.O’Connor MI, Sim FH, Chao EY (1996) Limb salvage for neoplasms of the shoulder girdle. Intermediate reconstructive and functional results. J Bone Joint Surg Am 78:1872–1888 [DOI] [PubMed]
- 14.Papaioannou AN, Francis KC (1965) Scapulectomy for the treatment of primary malignant tumours of the scapula. Clin Orthop 41:125–132 [PubMed]
- 15.Samilson RL, Morris JM, Thompson RW (1968) Tumours of the scapula. A review of the literature and an analysis of 31 cases. Clin Orthop 58:105–115 [PubMed]
- 16.Wittig JC, Bickels J, Wodaja F, Kellar-Graney KL, Malawer MM (2002) Constrained total scapula reconstruction after resection of high grade sarcoma. Clin Orthop 397:143–155 [DOI] [PubMed]


