Abstract
Between 2000 and 2004, 40 cases (average age 38, range 16–65 years) of spinal tuberculosis were treated with anterior debridement and iliac bone graft with one-stage anterior or posterior instrumentation in our unit. All patients received at least 2 weeks of regular antituberculous chemotherapy before surgery. We followed up all patients for 12–48 months (mean 22 months). Local symptoms of all patients were relieved significantly 1–3 weeks postoperatively; 23 of 25 cases (92%) with neurogical deficit had excellent or good clinical results. Erythrocyte sedimentation rates (ESR) returned from 51 mm/h to 32 mm/h (average) two weeks postoperatively. Kyphosis degrees were corrected by a mean of 16°. Fusion rate of the grafting bone was 72.5% one year postoperatively and 90% two years postoperatively. Severe complications did not occur. We therefore believe that patients undergoing anterior debridement and iliac bone grafting with one-stage anterior or posterior instrumentation achieve satisfactory clinical and radiographic outcomes.
Résumé
Entre 2000 et 2004 les auteurs ont traités 40 patients (de 16 à 65 ans, en moyenne 38 ans) atteints de tuberculose rachidienne par débridement antérieur et greffe iliaque avec instrumentation antérieure ou postérieure en un temps. Tous avaient reçu une chimiothérapie anti-tuberculeuse au moins deux semaines avant l’opération. Le suivi moyen était de 22 mois (12 à 48 mois). Les signes locaux s’étaient significativement améliorés dans les 3 semaines suivant la chirurgie et 23 cas parmi 25 avec un déficit neurologique avaient un résultat clinique bon ou excellent. La vitesse de sédimentation passait en moyenne de 51 mm/h à 32 mm/h en 2 semaines et le degré de cyphose était corrigé de 16°. Le taux de fusion de la greffe osseuse était de 72,5% à 1 an et de 90% à 2 ans. Il n’y avait pas de complication graves. Nous pensons que cette technique est satisfaisante.
Introduction
There is a still high incidence of tuberculosis, especially in developing countries, where the spine is involved more often than other skeletal sites [12]. It was generally accepted that regular antituberculous chemotherapy was the key point for spinal tuberculosis management, with surgical treatment when needed. But when and how surgical intervention should be performed has remained controversial. The purpose of this study was to discuss the indications for surgical management of spinal tuberculosis and the strategy of the surgical treatment. Our conclusion was that the indications for surgical intervention for spinal tuberculosis are as follows: caseous abscesses or sequestered bone formation, local back pain unrelieved by conservative treatment, initial kyphotic angle more than 30° [11], evidence of instability on radiographs, and cord compression with considerable neurological deficit. Active tuberculosis was absolutely not a contraindication. Anterior debridement and iliac bone graft with one-stage anterior or posterior instrumentation is recommended. It was safe and feasible to graft bone and perform internal fixation in the tuberculous lesion after debridement.
Materials and methods
We evaluated 40 patients with spinal tuberculosis retrospectively, accounting for 40.8% of a total 98 cases treated in our unit, who underwent surgical treatment between 2000 and 2004. There were 28 male and 12 female patients with an average age of 38 (16–65) years. The cervical spine was involved in three patients, the thoracic spine in eight, the thoracic-lumbar spine (T11-L2) in 11 and the lower lumbar spine in 18. The diagnosis was based on clinical and radiological evaluation. The ESR was used to evaluate whether the lesion was “active” or not, and whether the disease was healed. Additional imaging, in the form of MRI and/or CT, was used to ascertain the extent of lesion, the site and degree of compression of the cord. In this series the lesion was limited to the anterior and middle column, with no abnormal signals on MRI posterior to the pedicles. A definitive diagnosis was made by histological examination of tissue removed at surgery. The final diagnosis which could not be proved histologically was excluded; thus one case with pyogenic infection in the cervical spine was not included in this study.
All patients received regular antituberculous chemotherapy with four kinds of drugs 2–8 weeks before surgery. 22 patients with cervical, thoracic, and thoracic-lumbar level involvement underwent anterior debridement, spinal cord decompression, distraction for kyphosis correction and iliac bone graft with one stage anterior plate or screw-rod systems instrumentation. 18 lumbar spine patients received posterior transpedicular screw fixation and distraction in the intervertebral space in the prone position, followed by anterior debridement, decompression and iliac bone graft with further distraction in the supine position. Broad-spectrum antibiotic was used intravenously for all patients 5 to 7 days postoperatively. Regular antituberculous chemotherapy continued for 10–18 months postoperatively. Bracing was used within the initial three months postoperatively.
The rehabilitation programme included psychotherapy, vocational training, exercise therapy and prevention of complications. If the systematic and local symptoms were relieved considerably without fever, ESR was in the normal limitation, there was no recurrence for at least 3 months after returning to work or solid fusion was obtained, the chemotherapy could be stopped and the disease was assumed to be healed.
All clinical outcomes were evaluated by a spine surgeon not included in the therapeutic team and radiographic data were evaluated as to whether bone fusion was obtained and how much kyphotic deformity corrected by an independent radiologist. When bone fusion was in question, another radiologist was called for confirmation.
Results
When the clinical and radiological diagnosis was made, the patients were immobilised in bed and given nutritional support.
In this series, all cases were followed-up for a mean of 22 months (range 12–48 months). All patients’ incisions were primarily healed within 14 days, with no sinus tract forming. Focal and systematic symptoms of all patients were strikingly relieved 1–3 weeks postoperatively, and the ESR fell significantly 2–6 weeks postoperatively (Table 1). In three patients, the ESR was more than 80 mm/h when primary diagnosis was made. After regular antituberculous chemotherapy with four kinds of drugs for at least 8 weeks, the ESR did not fall at all, but rather their neurological deficits became worse nearly to complete paraplegia. To save their neurological function, operation was performed to debride and decompress the spinal cord. Two weeks later, ESR descended to below 60 mm/h, and the neurological function recovered. In the follow-up period, no recurrence was found in any of the patients.
Table 1.
ESR of pre-and post-operation
| ESR (mm/h) | < 40 | 40–60 | 60–80 | 80–100 | >100 | |
|---|---|---|---|---|---|---|
| Patients | Preoperative | 18 | 11 | 8 | 2 | 1 |
| Postoperative (2 w) | 28 | 10 | 2 | 0 | 0 | |
At the last follow-up, 25 patients with neural deficit were clinically improved at least one grade according to the Frankel grading system, including six cases with complete bladder recovery. According to the grading in Table 2 [10], the clinical results of 23 cases (92%) were excellent or good. Radiographically, union of the grafted bone was observed in 29 patients 1 year after surgery, with 72.5% fusion rate. And two years after surgery, the fusion rate was 90% whereby 36 patients obtained fusion. Kyphotic deformity was corrected by an average of about 16° by the surgery. In the follow-up period, the correction was lost by 1°, an occurrence of 6.3%.
Table 2.
Criteria for clinical results
| Excellent | Complete relief of pain in back and limbs |
| No limitation of physical activity | |
| Able to return to accustomed employment | |
| Analgesics not used | |
| Good | Relief of most pain in back and limbs |
| Physical activities slightly limited | |
| Able to return to accustomed employment | |
| Analgesics used only infrequently | |
| Fair | Partial relief of pain in back and limbs |
| Physical activities definitely limited | |
| Able to return to accustomed employment with limitations, or return to lighter work | |
| Mild analgesics medication used frequently | |
| Poor | Little or no relief of pain in back and limbs |
| Physical activities greatly limited | |
| Unable to return to accustomed employment | |
| Analgesics medication used regularly |
In this series there were no serious intraoperative or postoperative complications. No complications related to instrumentation occurred.
Illustrative case
A 31-year-old woman was admitted to the hospital for back pain and radicular pain in the bilateral lower extremities. Neurological examination showed a 2/5 paraparesis in both lower extremities. Radiological studies showed destruction from T11 to L1 vertebral bodies with anterior epidural abscess, compressing the spinal cord antereioly (Figs. 1 and 2). The kyphotic deformity was 70° and her ESR was 68 mm/h before treatment began. After oral antituberculous chemotherapy for 3 weeks, the ESR decreased to 41 mm/h. Then, she was treated with single-stage anterior radical debridement, decompression of the spinal cord, autogenous iliac bone grafting and plate fixation (Z-plate system, Sofamor-Danek). Back pain improved immediately after surgery and resolved gradually in 3 months. The postoperative kyphotic correction was satisfactory from 70° to 38° (Fig. 3). Additional regular antituberculous chemotherapy for a total period of one year was performed and no recurrence was found at the final follow-up.
Fig. 1.
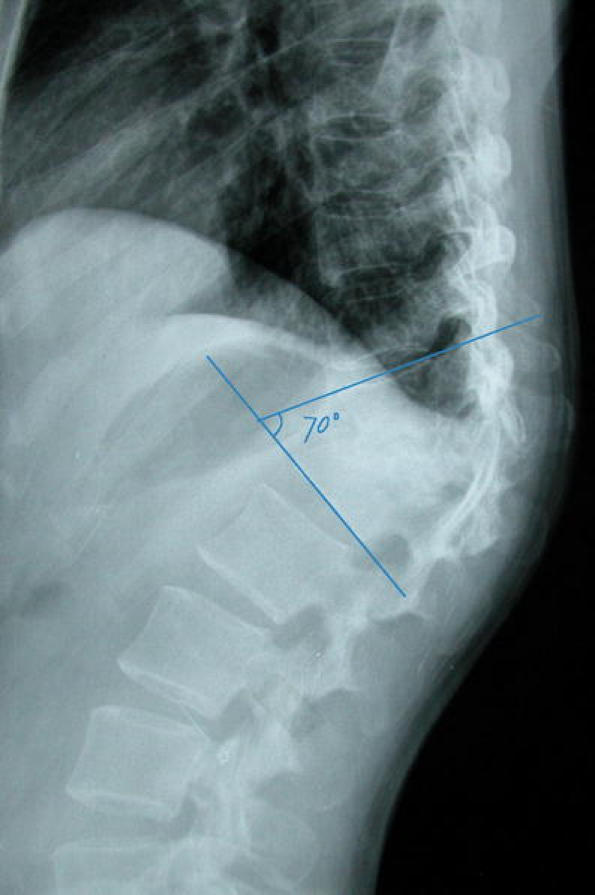
Preoperative plain lateral radiograph showing destruction from T11 to L1 vertebral dodies with kyphotic deformity at a 70° angle
Fig. 2.
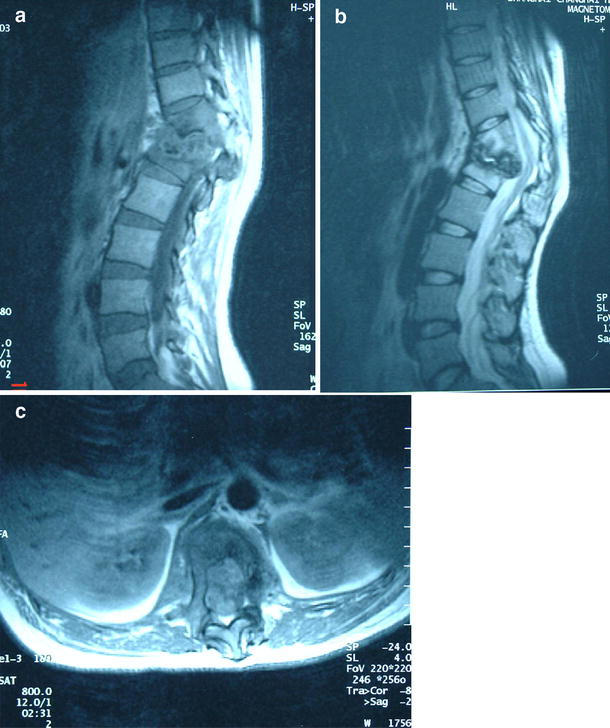
Preoperative sagittal (a and b) and axial (c) MRI showing destruction from T11 to L1 vertebral dodies and discs, especially T12 body, with anterior epidural abscess and spinal cord compression
Fig. 3.

Postoperative plain lateral radiograph showing anterior debridement, bone graft and internal fixation anteriorly. The kyphotic deformity was corrected to 38°
Discussion
Tuberculosis is still common in today’s society, especially in developing countries. Over the past two decades, the incidence of tuberculosis has tended to increase [1, 12]. Spinal involvement is the most common form of skeletal tuberculosis, accounting for half of the cases [12]. Because of its complications such as late-onset neurological deficit, instability and kyphotic deformity, and poor chemotherapy effectiveness, more and more authors emphasise the important role of surgery in treating spinal tuberculosis [2, 3]. Recently, with further study of this disease and understanding of the biomechanics of the spine, the surgical approach has become more and more reasonable. Moon [9] reported that combining chemotherapy with anterior autogenous bone grafting following radical debridement is an efficient method to cure spinal tuberculosis and prevent the progression of kyphotic deformity. But without instrumentation, the grafted bone may displace, be absorbed and a long period of external fixation may be required, so the therapeutic effect of this surgery is affected. Thus, many authors began to explore the feasibility of internal fixation after debridement and bone grafting [5]. It has been proven that tubercle bacillus has no adhesiveness to autogenous bone and instruments, and it is safe to graft bone and use instrumentation in an infection focus [13]. In our series, all cases were performed with autogenous iliac bone and internal fixation, instant stabilisation was obtained and the fusion rate was 90% 2 years after surgery.
Analysing our series, we find that the indications to operate on spinal tuberculosis are as follows: caseous abscesses or sequestered bone formation, local back pain unrelieved by conservative treatment, initial kyphotic angle more than 30°, evidence of instability on radiographs, cord compression with considerable neurological deficit [4, 9]. Spinal tuberculosis is a common cause of severe kyphotic deformity. In spite of effective treatment for spinal tuberculosis with modern antituberculous drugs, it is common to find residual kyphosis and instability at the end of treatment. Patients with severe deformity after healing may develop late-onset paraplegia after 5–20 years [7]. Jain [6] suggested that patients with spinal tuberculosis who are likely to develop severe kyphosis on completion of treatment should be identified and have surgery in the active stage of the disease to improve kyphosis. An ESR value more than 80 mm/h, considered to be active tuberculosis, is not an absolute contraindication for surgery. In our study, there were three patients whose ESR values were more than 80 mm/h, even a case more than 100 mm/h, and they showed no response at all for antituberculous drugs; but 2 weeks after operation, their ESR values descended significantly. Certainly, reconstruction of spinal stability is beneficial to heal spinal tuberculosis and avoid recurrence. In this series, there were 25 patients (62.5%) who were subject to neurological complications. In the follow-up period, 23 of them (92%) had excellent or good clinical results and returned to accustomed employment.
Radical debridement is the key point of operation for spinal tuberculosis [4]. In spinal tuberculosis, many studies indicate that the involvement of the vertebral body is very frequent, and few cases have been found involving the posterior column [3, 13]. In our series, MRI showed that all cases involved the anterior column and no posterior column involvement was found. Thus, we suggest that when operating on spinal tuberculosis, anterior debridement and autogenous bone graft with one-stage instrumentation anteriorly or posteriorly is preferred. Iliac bone is the preferable resource for grafting. It has been reported that when there is antero-lateral decompression without bone graft anteriorly, the kyphotic angle achieved at 6 months cannot be maintained and should increase to final follow-up at 2 years [7]. In our series, the correction of kyphotic deformity had a mean of 16°, and at the recent follow-up the kyphotic angle was 15°, so that there was no statistically significant difference over the whole follow-up period. Anterior bone grafting can strut the spine and prevent late-onset loss of correction of kyphotic deformity.
The anterior approach leads the surgeon directly to the lesion and allows good visualisation. Even more, decompression of the spinal cord anteriorly can be obtained directly and completely. Instrumentation following debridement and bone graft can provide instant stability for the spinal column, which can lead patients to resume exercise, as our study shows this occurs at a mean of 12 days after operation. And a relatively stable internal environment can prevent recurrence of tuberculosis [1]. In this series, there was no recurrence. For lower lumbar (L3-5) tuberculosis in 18 patients in our study, there was not an appropriate internal fixation system to use clinically, so we performed posterior transpedicular screw fixation and distraction of the intervertebral space in the prone position, followed by anterior debridement, decompression and iliac bone graft with further distraction in the supine position [8]; this has been proven as a useful technique.
It should be emphasised that regular antituberculous chemotherapy is very important to cure spinal tuberculosis and prevent its recurrence. Surgery cannot replace chemotherapy in managing spinal tuberculosis. After operation, bracing for three months is recommended.
References
- 1.Altman GT, Altman DT, Frankovitch KF (1996) Anterior and posterior fusion for children with tuberculosis of the spine. Clin Orthop 325:225–231 [DOI] [PubMed]
- 2.Chen WJ, Chen CH, Shih CH (1995) Surgical treatment of tuberculosis spondylitis: 50 patients followed for 2–8 years. Acta Orthop Scand 66:137–142 [DOI] [PubMed]
- 3.Dai LY, Jiang LS, Wang W et al (2005) One-stage anterior autogenous bone grafting and instrumentation in the surgical management of spinal tuberculosis. Spine 30(20):2342–2349 [DOI] [PubMed]
- 4.Griffiths DL, Seddon H, Ball J et al (1982) A 10-year assessment of a controlled trial comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong. Eighth report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg 64:393–398 [DOI] [PubMed]
- 5.Guven O, Kumano K, Yalcin S et al (1994) A single stage posterior and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine 19:1039–1043 [DOI] [PubMed]
- 6.Jain AK (2002) Tuberculosis of the spine with neurological complications. Clin Orthop 398:75–84 [DOI] [PubMed]
- 7.Jain AK, Aggarwal PK, Arora A et al (2004) Behaviour of the kyphotic angle in spinal tuberculosis. Int Orthop 28:110–114 [DOI] [PMC free article] [PubMed]
- 8.Kim DJ, Yun YH, Moon SH et al (2004) Posterior instrumentation using compressive laminar hooks and anterior interbody arthrodesis for the treatment of tuberculosis of the lower lumbar spine. Spine 29:275–279 [DOI] [PubMed]
- 9.Moon MS (1997) Tuberculosis of the spine. Controversies and a new challenge. Spine 22(15):1791–1797 [DOI] [PubMed]
- 10.Morelos O, Pozzo AO (2004) Selective instrumentation, reduction and repair in low-grade isthmic spondylolisthesis. Int Orthop 28:180–182 [DOI] [PMC free article] [PubMed]
- 11.Swanson AN, Pappou IP, Cammisa FP et al (2006) Chronic infections of the spine: surgical indications and treatments. Clin Orthop Relat Res 444:100–106 [DOI] [PubMed]
- 12.Tuli SM (1997) Tuberculosis of the skeletal system: bone, joints, spine and bursal sheaths, 2nd edn. Bangalore: Jaypee Brothers
- 13.Yilmaz C, Selek HY, Gurkan I et al (1999) Anterior instrumentation for the treatment of spinal tuberculosis. J Bone Joint Surg Am 81(9):1261–1267 [DOI] [PubMed]


