Abstract
The authors followed up 20 patients with multiple diaphyseal fractures of the radius and ulna who were treated nonoperatively and who healed with axial deviation >5° in at least one plane 20.4±6.7 years after radiographic evidence of fracture union. Mean age at follow-up was 28.6±6.4 years. Radiographs were measured soon after reduction, at 10 days from reduction, at the end of treatment, and at follow-up (17/20). Both elbow and forearm range of motion (ROM) were compared with those of the contralateral side. At follow-up, ROM was normal and radiographs showed angular deviations <5°.
Résumé
A un recul moyen de 20.4±6.7 ans, les auteurs étudient 20 patients avec des fractures diaphysaires multiples du radius et du cubitus, traitées non-opérativement et qui avaient consolidé avec une déviation axiale de plus de 5° dans au moins un plan. L’âge moyen au recul était de 28.6±6.4 ans. Les radiographies étaient mesurées juste après la réduction,10 jours plus tard , à la fin du traitement et au dernier recul. La mobilité du coude et de l’avant-bras était comparée au côté opposé. Au recul les mobilités étaient normales et les radiographies montraient des déviations de moins de 5°.
Introduction
Forearm diaphyseal fractures account for about 45% of childhood fractures and over 62% of upper limb fractures. In most cases, the age of the children affected is <5 years, with fractures occurring in the middle third of this age range accounting for 15–18% of all cases [11]. Recent studies report an increasing tendency to perform closed or, if necessary, open reduction and internal fixation (CRIF vs. ORIF) using Kirschner wires or elastic intramedullary nails [9, 13, 15]. The aim of our retrospective study of paediatric cases treated non-surgically between 1970 and 2000 was to detect motor deficit and/or axial deviations at the end of growth in fractures not optimally aligned at consolidation.
Methods
We reviewed the clinical records and radiographs of 215 patients with multiple forearm diaphyseal fractures who were hospitalised and treated in the Second Department of Orthopaedics. Among these, 70 underwent simple reduction and plaster cast application and presented at consolidation with an axial deviation >5° in at least one plane. All patients were contacted by telephone, but only 20 presented themselves for clinical follow-up and three refused to be submitted to X-ray examination. Therefore, our study included 15 males and five females. The fracture was on the left side in 11 cases and on the right in nine. Associated lesions were Gustilo I open fracture and simple slipped epiphysis of the homolateral distal radius. Median age at fracture was 7.5 years (range: 3.8–13.6; mean: 8.2±3 SD). Median age at follow-up was 27 years (range: 7–41; mean: 28.6±6.4 SD). Median time to radiographic evidence of fracture union and follow-up, expressed as years, was 19 (range: 11–34.8; mean: 20.4±6.7 SD).
For all fractures, treatment included non-surgical reduction under general anaesthesia and application of an above-elbow plaster cast for 40 days, with adequate rotation of the forearm to obtain optimal reduction. The first radiograph was made soon after reduction and application of the plaster cast; the final one was made at plaster cast removal. A second forearm plaster was not required.
We evaluated 20 patients who presented themselves for follow-up evaluation of elbow and wrist range of motion (ROM) and forearm pronation/supination movements and compared these findings with those of the contralateral arm which had no trauma. The radiographs of the treated patients who underwent follow-up evaluation were measured by the three authors independently without consultation. The degrees of axial deviation and the percentage of lateral shift were measured on the post-reduction radiographs at 10 days and at consolidation. We considered an axial deviation ≤5° to indicate acceptable alignment.
Results
Clinical results of these 20 patients showed that the fractured limb and contralateral limb had the same ROM. All of the patients who engaged sports (not competitive) before the injury fully resumed their activities after the fracture. At the time of the follow-up two patients had physically demanding jobs (blacksmith, truck driver). The results of radiograph measurements immediately after reduction, at 10 days after reduction, and at consolidation are reported in Tables 1, 2 and 3. At follow-up, radiographs did not show axial deviations ≥5° and, therefore, the bones were considered to be aligned.
Table 1.
Measurement of axial deviations immediately after reduction
| Mean ± SD | Median (range) | |
|---|---|---|
| Frontal plane-varus-valgus (degrees) | 10±3.4 | 8.5 (8–15) |
| Sagittal plane-procurvatum- recurvatum (degrees) | 12.8±5.5 | 10 (8–25) |
| Frontal lateral shift (%) | 56±28.5 | 50 (20–100) |
| Sagittal lateral shift (%) | 51.4±30 | 50 (10–100) |
Table 2.
Measurement of axial deviations at radiographic control of limbs in a plaster cast at 10 days after reduction
| Mean ± SD | Median (range) | |
|---|---|---|
| Frontal plane-varus-valgus (degrees) | 8.2±3 | 7.5 (3.8–13.6) |
| Sagittal plane-procurvatum- recurvatum (degrees) | 28.6±6,4 | 27 (7–41) |
| Lateral shift (%) | 20.4±6.7 | 19 (11–34.8) |
Table 3.
Measurement of axial deviations at consolidation
| Mean ± SD | Median(range) | |
|---|---|---|
| Frontal plane-varus-valgus (degrees) | 12.5±3.2 | 11 (8–20) |
| Sagittal plane-procurvatum- recurvatum (degrees) | 14.8±5.1 | 15 (8–25) |
| Frontal lateral shift (%) | 65±27.7 | 50 (30–100) |
| Sagittal lateral shift (%) | 65.6±26 | 50 (25–100) |
Discussion
The treatment of multiple forearm fractures is aimed at obtaining optimal reduction, especially in terms of adequate rotation, which should be maintained until consolidation so that there is no tendency to spontaneous remodelling with growth [2, 11]. It is well known that post-fracture axial deviations in growing subjects are more easily and rapidly remodelled, with the younger the patient and the closer the fracture to the growth cartilage, the higher the tendency for remodelling [16]. According to some authors, malunions >20° are remodelled with growth in children <5 years of age [12] (Fig. 1); other authors report corrections of the deformity of about 1.5°/month [10]. Deviations >20° result in deficits of forearm pronation/supination [8, 12] and are probably due to alterations in the normal curvature of the radius, which is estimated to be 60.39% of the overall length of the radius starting from bicipital tuberosity and should not exceed 10% of radius length [3].
Fig. 1.
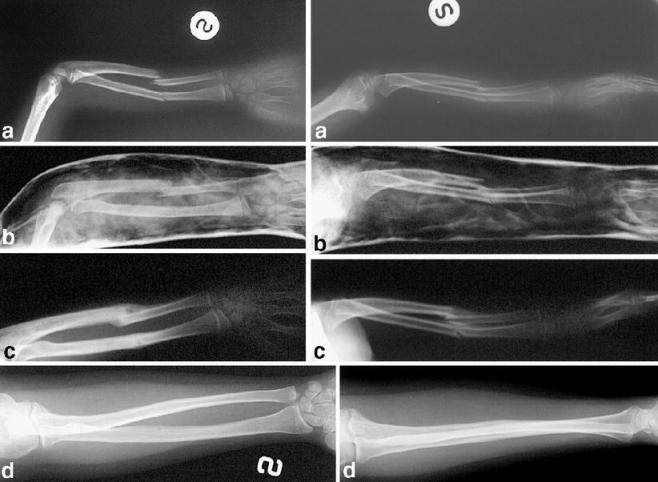
Female patient with a left forearm fracture. a 5.7 years, b: X-ray after 10 days, c: X-ray at consolidation, d, follow-up at 25 years of age
Measurements made on radiographs were reliable, as demonstrated by the data obtained by the three authors carrying out separate evaluations: there were no statistically significant differences, taking as reference the evaluations of the most experienced author (SB).
The analysis of the data for treated fractures showed a tendency to remodelling in children aged <7.5 years in the period between radiographic examination at 10 days and consolidation. This tendency was never observed in children aged >7.5 years (Fig. 2); however, the low number of fractures examined does not allow definitive conclusions to be drawn. These data seem to support the results reported by Gustilo and Anderson [4], Creasman et al. [2], Ostermann et al. [8], Jones and Weiner [7], Johari and Sinha [6], Hahn et al. [5], and Schmittenbecher et al. [14].
Fig. 2.
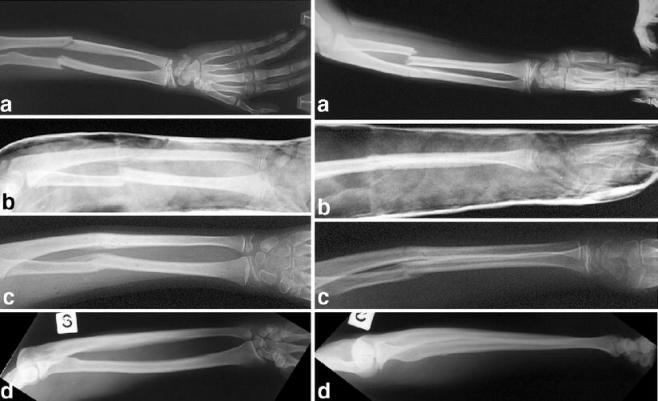
Male patient with a left forearm fracture. a 11.7 years, b X-ray after 10 days, c X-ray at consolidation, d follow-up at 34 years of age
Analysis of the remaining cases showed that remodelling occurs even when malunion is present in older children with residual growth potential. On the basis of our data, it is not possible to determine how many years a child aged over 10 years needs, to obtain complete correction of residual deformity. This remodelling potential has not yet been reported in the literature since there are no retrospective studies with sufficiently long mean follow-up in a sufficiently large case series.
As reported by Blount [1], we could observe that even 100% lateral shift – i.e. a simple contact of cortices – did not cause long-term consolidation or motility problems.
The three patients who refused the radiograph considered the examination unnecessary since their clinical conditions were normal. For these patients, we assumed a complete bone remodelling.
The study of malrotation was not possible since the radiographs available were not sufficient to carry out such an analysis.
Based on our retrospective review of these 20 cases, we draw the same conclusions expressed by Blount in 1955 in his volume Fractures in children, namely: “too many men treat roentgenograms instead of children”. Actually, axial deviations up to 20° and lateral shift reaching 100% are not a problem in growing children, at least not until 12–13 years of age.
Acknowledgements
We thank Doctor P.M. Peters for his review of this work, Doctor A. Capurro for the translation and S. Panichi for his work with the archives.
References
- 1.Blount WP (1955) Fractures in children. William & Wilkins, Baltimore
- 2.Creasman C, Zaleske DJ, Ehrlich MG (1984) Analyzing forearm fractures in children: the more subtle sign of impending problems. Clin Orthop Relat Res 188:40–53 [PubMed]
- 3.Firl M, Wunsch L (2004) Measurement of bowing of the radius. J Bone Joint Surg B 86:1047–1049 [DOI] [PubMed]
- 4.Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg A 58:453–458 [PubMed]
- 5.Hahn MP, Richter D, Muhr G, Ostermann PA (1997) Pediatric forearm fractures. Diagnosis, therapy and possible complications. Unfallchirurg 100:760–769 [DOI] [PubMed]
- 6.Johari AN, Sinha M (1999) Remodeling of forearm fractures in children. J Pediatr Orthop B 8:84–87 [PubMed]
- 7.Jones K, Weiner DS (1999) The management of forearm fractures in children: a plea for conservatism. J Pediatr Orthop 19:811–815 [DOI] [PubMed]
- 8.Ostermann PA, Richter D, Mecklenburg K, Ekkernkamp A, Muhr G, Hahn MP (1999) Pediatric forearm fractures: indications, technique, and limits of conservative management. Unfallchirurg 102:784–790 [DOI] [PubMed]
- 9.Qidwai SA (2001) Treatment of dyaphyseal forearm fractures in children by intramedullary Kirschner wires. J Trauma 50:303–307 [DOI] [PubMed]
- 10.Quairul IH, Kareem BA, Tan AB, Harwant S (2001) Early remodeling in children’s forearm fractures. Med J Malaysia 56[Suppl D]:34–37 [PubMed]
- 11.Rodrìguez-Merchan EC (2005) Pediatric fractures of the forearm. Clin Orthop Relat Res 432:65–72 [DOI] [PubMed]
- 12.Schlickewei W, Oberle M (2005) Forearm fractures in children. Unfalchirurg 108:223–234 [DOI] [PubMed]
- 13.Schmittenbecher PP (2005) State-of-the-art treatment of forearm shaft fractures. Injury. Int J Care Injured 36:SA25–SA34 [DOI] [PubMed]
- 14.Schmittenbecher PP, Dietz HG, Uhl S (1991) Late results of forearm fractures in childhood. Unfallchirurg 94:186–190 [PubMed]
- 15.Smith VA, Goodman HJ, Strongwater A, Smith B (2005) Treatment of pediatric both-bone forearm fractures: a comparison of operative techniques. J Pediatr Orthop 25:309–313 [DOI] [PubMed]
- 16.Vittas D, Larsen E, Tomp-Pederson S (1991) Angular remodelling of midshaft forearm fractures in children. Clin Orthop Relat Res 265:261–264 [PubMed]


