Abstract
Thyroid eye disease (TED) is an autoimmune condition in which intense inflammation leads to orbital tissue remodeling, including the accumulation of extracellular macromolecules and fat. Disease progression depends upon interactions between lymphocytes and orbital fibroblasts. These cells engage in a cycle of reciprocal activation which produces the tissue characteristics of TED. Peroxisome proliferator-activated receptor-γ (PPARγ) may play divergent roles in this process, both attenuating and promoting disease progression. PPARγ has anti-inflammatory activity, suggesting that it could interrupt intercellular communication. However, PPARγ activation is also critical to adipogenesis, making it a potential culprit in the pathological fat accumulation associated with TED. This review explores the role of PPARγ in TED, as it pertains to crosstalk between lymphocytes and fibroblasts and the development of therapeutics targeting cell-cell interactions mediated through this signaling pathway.
1. INTRODUCTION
Peroxisome proliferator-activated receptors (PPARs) are members of the nuclear hormone receptor superfamily that bind to DNA as heterodimers formed with retinoid X receptors (RXRs) [1]. These heterodimers control gene expression by binding to a specific cis acting DNA element known as the peroxisome proliferator response element (PPRE) found in the promoter or enhancer regions of target genes. PPRE binding can occur in the presence or absence of ligand and can either induce or repress gene transcription in a cell-specific manner. The ability of PPAR-RXR heterodimers to transactivate genes results not only from their binding to DNA, but also from their association with transcriptional coactivators or corepressors. Usually, agonist binding to these receptors inhibits corepressor and promotes coactivator binding, resulting in increased transcription of target genes.
Three PPAR subtypes, PPARα (NR1C1), PPARβ/δ (NUC1, NR1C2), and PPARγ (NR1C3), are encoded by separate genes [2]. Three isoforms of PPARγ, PPARγ1, PPARγ2, and PPARγ3 are generated by alternative splicing of the same mRNA [3]. PPARs are differentially expressed in a variety of tissues and are important to the regulation of lipid and carbohydrate metabolism, energy homeostasis, cellular differentiation, apoptosis, and immunity and inflammatory responses [2, 4–6]. The physiological functions of PPARα and PPARγ have been well characterized, whereas the physiological function of PPARβ/δ is poorly understood although the protein is widely distributed [3]. PPARα is expressed in brown adipose tissue, liver, kidney, heart, and skeletal muscle, but is also detected in cells of the vasculature and the immune system [1, 3, 7–10]. Its activation affects transcriptional expression of many genes involved in fatty acid oxidation, lipid metabolism, and inflammation [8, 11]. PPARα agonists (including the fibrates) have been reported to increase levels of high-density lipoproteins (HDL), lower those of triglycerides and decrease weight gain [12, 13]. They also induce adipogenesis in fibroblasts in vitro through the induction of genes such as high-mobility group AT-hook 2 (HMGA2) and leptin [8, 14–18].
PPARγ is highly expressed in adipose tissue, colon, retina, and in cells of the immune system, including platelets [1, 3–5, 19–25]. The PPARγ1 isoform is the more widely expressed, while PPARγ2 is mainly found in adipose tissue and liver [3, 26]. PPARγ3 mRNA is detectable in mouse macrophages, but little is known about the protein expression and functional significance of this isoform [3, 27]. Synthetic PPARγ agonists, including drugs of the thiazolidinedione (TZD) family (e.g., ciglitazone, pioglitazone, rosiglitazone and troglitazone), have potent insulin-sensitizing properties [3, 28, 29]. Because of this, rosiglitazone and pioglitazone are often prescribed for the treatment of type 2 diabetes mellitus [3]. These and naturally occurring PPARγ ligands, such as lysophosphatidic acid [30], nitrolinoleic acid [31], prostaglandin D2(PGD2), and 15-deoxy-Δ12,14-prostaglandin J2(15d-PGJ2) [32, 33], are also potent promoters of adipogenesis [3, 28, 34–37]. PGD2 and 15d-PGJ2 are derived from arachidonic acid by the catalytic activities of the cyclooxygenase-2 (Cox-2) and prostaglandin D synthase enzymes [28, 32, 33]. PGD2 spontaneously undergoes a series of dehydration reactions to form the PGJ family of prostaglandins, including 15d-PGJ2, and 15d-PGD2, which can also transactivate PPARγ and induce adipogenesis [28, 38–41]. Many of the genes under PPARγ control are important to glucose uptake, lipid metabolism and storage, as well as adipogenesis, explaining the ability of PPARγ ligands to increase insulin sensitivity and to trigger the differentiation of fibroblasts to adipocytes [8, 42–44]. Others act to dampen inflammation by decreasing TNFα, IL-6, and IL-8 production, suggesting potential therapeutic applications in chronic inflammatory diseases [45]. It has been suggested that the adipogenic action of PPARγ could serve as another of its anti-inflammatory functions because remodeling of inflamed tissue to fat may render it more quiescent [28]. Others would argue that adipogenesis is a proinflammatory action because an increase in fat mass would result in increased release of proinflammatory adipocytokines [36]. In any case, increased adipogenesis may lead to disease, even if it serves to attenuate active inflammation. Thyroid eye disease (TED) provides a cogent example of such a circumstance. This review will explore the role that PPARγ and lymphocytes play in advancing pathological tissue remodeling in TED and how PPARγ may be exploited as a target for therapeutic strategies.
2. THYROID EYE DISEASE
TED is a condition in which intense inflammation leads to remodeling and expansion of the connective and adipose tissues of the orbit, including proliferation and differentiation of fibroblasts to adipocytes, fat deposition, and disordered accumulation of extracellular matrix glycosaminoglycans (GAGs) [8, 46, 47]. Accumulation of GAGs is accompanied by dramatic swelling due to their prodigious water-binding capacity [48, 49]. The increased volume of orbital connective tissue leads to forward protrusion of the eye (exophthalmos), accompanied by nerve and muscle damage [28, 50–56]. In patients with severe TED, the initial inflammation subsides, but infiltration of muscle fibers by fibroblasts leads to fibrosis, potentially limiting their motility [46, 47, 50–52]. In addition to exophthalmos and extraocular muscle dysfunction, clinical features of TED include periorbital edema, eyelid retraction, dry eye, pain, optic neuropathy, double vision, and vision loss [28, 50, 53, 57].
TED is closely associated with Graves' disease (GD), a common autoimmune disorder in which stimulatory autoantibodies against the thyroid-stimulating hormone receptor (TSH-R) cause the thyroid to produce excess thyroid hormone [50, 54, 58, 59]. In addition to the hypermetabolic consequences of hyperthyroidism, clinically apparent TED develops in approximately 50–60% of patients with GD [50, 54–56]. Furthermore, a subset of patients with severe TED develop pretibial dermopathy, a distinctive thickening of the skin, usually occurring on the anterior lower leg [60, 61]. Although the pathogenesis of the hyperthyroid state in GD is relatively well understood, many questions remain regarding the induction and perpetuation of the orbital (and pretibial) disease that develops in some patients. It is likely that the hyperthyroid state does not promote connective tissue accumulation within the orbit. Euthyroid GD patients remain at risk for developing TED [62, 63]. Furthermore, TED does not usually occur in patients with non-Graves’ hyperthyroidism [64]. It has been suggested that the orbit is a secondary target of autoimmune attack, involving the same autoantigen (TSH-R), but resulting in consequences distinct from those in the thyroid [50, 58, 65]. However, TSH-R mRNA and protein are expressed widely in many tissues which are unaffected in GD, so the basis for the anatomical restriction of TED remains unclear [50, 66]. Moreover, no convincing evidence currently exists for TSH-R mediating any important biological events in orbital connective tissues.
To date, there are no effective means of preventing the onset of TED or for predicting which GD patients are likely to exhibit extrathyroidal complications. A study by Khoo et al. [67] suggested that the presence of thyroid-stimulating antibodies combined with the absence of antibodies against thyroid peroxidase is a predictor, but other reports contradict these findings [68, 69]. Current treatment options for TED exist, including corticosteroid treatment, external beam radiation, and surgery, but these interventions are aimed only at the consequences of the disease, and they fail to prevent or reverse pathological alteration of orbital tissues [70]. Histological examination of orbital tissue in TED suggests that its development and progression involve interactions between lymphocytes and fibroblasts [28]. Understanding these complex interactions may both lead to the identification of biomarkers predictive of advanced disease and provide effective early treatments. It is thought that autoreactive B lymphocytes initiate the disease state by producing antibodies against self-antigen, such as the TSH-R [58]. Next, in a poorly understood and likely variable event, autoantibody production results in orbital fibroblast activation [71]. Activated fibroblasts release chemoattractants that recruit T lymphocytes and monocytes to the orbit [28, 37, 50, 72–77]. These bone marrow-derived cells cooperate with the resident fibroblasts and are engaged in a cycle of reciprocal activation which ultimately produces the pathological changes in the orbit characteristic of TED [50].
3. INTERACTIONS BETWEEN LYMPHOCYTES AND FIBROBLASTS
Orbital tissue from patients with TED is infiltrated by T helper type I (Th1) and T helper type 2 (Th2) lymphocytes, B lymphocytes, mast cells, and macrophages [47, 50, 59, 78–82]. It is currently thought that these cells, once recruited to the orbit, generate cytokines which participate in driving tissue reactivity and remodeling. Autoimmune responses, like that found with TED, are governed primarily by the actions of B and T lymphocytes. Lymphocytes are migratory cells that proliferate extensively and develop into activated effector cells when they encounter specific antigen in the proper costimulatory context. Normally, the antigens to which lymphocytes respond are foreign and several tolerance mechanisms act to prevent the development of reactivity to self antigens or autoimmunity [83, 84]; but these tolerance mechanisms sometimes fail and autoimmunity develops. B lymphocytes are key to this phenomenon, as activated autoreactive B lymphocytes produce autoantibodies and are a critical source of support for the function of other immune cells, such as T lymphocytes and fibroblasts [85].
Fibroblasts were once viewed as merely structural bystanders in the cellular microenvironment, producing extracellular matrix components, but otherwise uninvolved in the regulation of tissue homeostasis. Now, it is understood that fibroblasts are a highly interactive cell type, described as “sentinel cells,” which are able to detect events that endanger homeostasis, to communicate these dangers to cells of the immune system, and to respond directly to these threats via proliferation and differentiation to effector cells that support tissue integrity [58, 66, 72]. Fibroblasts do not merely respond to immune stimulation, but actively participate in the inflammatory pathway through the synthesis of proinflammatory mediators, including IL-1, IL-6, and IL-8 [28, 73, 74]. They interact with bone marrow-derived cells in the orbit and are key to the pathophysiology of TED [8, 37, 50, 65, 72, 73, 75, 76]. As described earlier, the clinical symptoms of TED result from excess extracellular macromolecular deposition, fibrosis, and fat accumulation in the orbit [48, 57]. Several differences have been identified that distinguish orbital fibroblasts harvested from patients with TED from those derived from normal orbital tissues and nonorbital anatomic sites. Orbital fibroblasts from patients with TED synthesize excess GAGs, including hyaluronan, are unusually proliferative and can differentiate into adipocytes, leading to accumulation of fat [50, 86, 87]. In addition, they do not express IL-1 receptor antagonist at levels found in other fibroblasts. This results in excessively high levels of Cox-2 and PGE2 in response to proinflammatory cytokines [47, 50, 59, 77, 86, 88–91]. They also display lymphocyte costimulatory molecules such as CD40 [59, 77, 86, 88]. These characteristics suggest that the fibroblast phenotype underlies the selective anatomic distribution of TED-associated inflammation and tissue remodeling [37, 47, 50, 59, 73, 75, 92, 93].
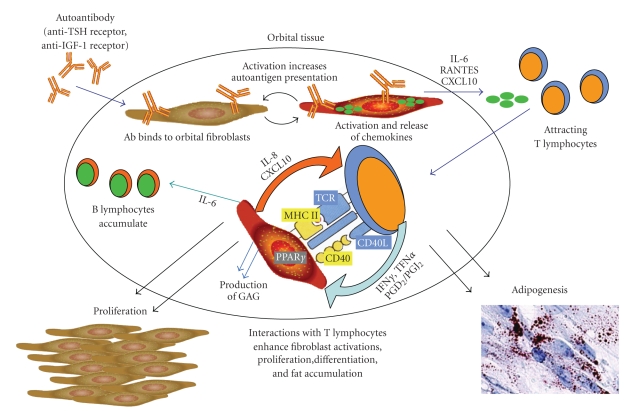
The unique features of orbital fibroblasts provide an environment in which TED might develop, but the disease is characterized also by mononuclear cell infiltration [48, 59, 94]. Substantial data support the concept that infiltrating T lymphocytes interact with fibroblasts, activate them, and result in their proliferation, synthesis of extracellular macromolecules, and differentiation to adipocytes [50, 59]. A summary of this model for the pathogenesis of TED is depicted in Figure 1. It is thought that autoantigen expression by orbital fibroblasts instigates T lymphocyte recruitment to the orbit [48, 95, 96]. The autoantigen may be TSH-R or another protein, such as insulin-like growth factor-1 receptor (IGF-1R) [34, 48, 54, 94–98]. Recruited T lymphocytes stimulate orbital tissue remodeling by initiating fibroblast proliferation and hyaluronan synthesis [50]. They also contribute to the perpetuation of the inflammatory response by (1) stimulating fibroblast production of chemokines, like IL-16 and RANTES, and cytokines, like IL-6, that initiate T and B lymphocyte migration to local environments, and (2) increasing fibroblast presentation of autoantigens [50, 73, 74, 76, 77, 99]. The T lymphocyte-fibroblast interaction occurs via costimulatory molecules, adhesion molecules, and cytokines like IFNγ, IL-1β, and TNFα [50, 99]. One mechanism by which T lymphocytes may communicate with orbital fibroblasts is through the CD40-CD40 ligand pathway [50, 74, 88]. CD40 is a cell surface receptor found on antigen-presenting cells, whereas CD40 ligand (CD40L, CD154) is expressed on T lymphocytes [50]. Ligation of CD40 on B lymphocytes or other antigen-presenting cells is necessary for efficient activation of T-lymphocyte effector functions [100, 101]. Recently, it has been shown that orbital fibroblasts from TED patients express high levels of CD40, which is upregulated in the presence of IFNγ, produced by infiltrating T lymphocytes [74, 76, 77, 99]. Activation by CD40L induces hyaluronan synthesis, IL-6 and IL-8, Cox-2 and PGE2 [50, 74, 86, 102]. Thus, the CD40-CD40L bridge is one potential pathway through which T lymphocytes could influence fibroblast activation and proliferation in TED [50].
Figure 1.
According to one current model, TED is triggered by binding and activation of orbital fibroblasts by autoantibodies. These autoantibodies could be specific for antigens such as TSH-R and/or IGF-1R. Activated orbital fibroblasts release chemokines, including IL-16, RANTES, and CXCL10, which recruit T lymphocytes into the orbit. These lymphocytes then interact with fibroblasts, potentially activating each other, further promoting cytokine production (IFNγ, TNFα, PGD2, and 15d-PGJ2) and secretion of T cell-activating factors by the fibroblasts (IL-8 and CXCL10). Fibroblasts are also stimulated to secrete IL-6 (promoting B cell differentiation) and to increase autoantigen presentation, both of which amplify the overall response. The interactions of fibroblasts with T cells result in the deposition of extracellular matrix molecules, fibroblast proliferation, and fat accumulation.
Fibroblasts respond to T lymphocyte-mediated activation by releasing factors that recruit, activate, and promote the proliferation of T lymphocytes, thus participating in the perpetuation of inflammation [35, 50, 103]. In patients with clinically significant TED, even in those whose hyperthyroidism is well controlled, B and T lymphocytes have been shown to display a distinctly activated phenotype different from those derived from control donors [59]. This sustained activation following treatment of hyperthyroidism contributes to orbital inflammation and tissue remodeling observed in late-stage TED. A recent study found that orbital fibroblasts from TED patients may modulate the activity of T lymphocytes through the production of CXCL10 [35]. TED patients with active disease had higher serum CXCL10 levels than patients with inactive disease. CXCL10 release enhances the migration of T lymphocytes into the orbit, where they secrete IFNγ and TNFα. IFNγ levels were higher in TED patients than in patients with GD without orbital involvement. IFNγ and TNFα synergistically induced CXCL10 release by orbital fibroblasts, thereby perpetuating a positive feedback loop [35, 50, 103]. PPARγ activation was found to play an inhibitory role in this process, both in vivo and in vitro [35].
4. PPARγ LIGANDS AND INFLAMMATION
PPARγ ligands attenuate activity of inflammatory bowel disease in animal models [35, 104–106], experimental autoimmune encephalomyelitis [107, 108], arthritis [21], and psoriasis [109]. Clinical trials have shown that they ameliorate inflammation in patients with mild-to-moderate cases of ulcerative colitis [1, 110, 111]. At least some of the anti-inflammatory effects of PPARγ ligands result from direct actions on cells of the innate and adaptive immune system [23, 112–114]. In macrophages, they inhibit activation and production of inflammatory cytokines such as TNFα, IL-1β, and IL-6 [25, 115, 116]. In addition, PPARγ activation has been shown to skew macrophage differentiation into a more anti-inflammatory phenotype [117]. In dendritic cells, PPARγ agonists downregulate the synthesis of chemokines involved in the recruitment of T lymphocytes [35, 118].
Evidence for a physiological role of PPARγ in regulating B lymphocyte function was generated in studies using PPARγ-haploinsufficient mice [21]. B lymphocytes derived from these mice exhibit increased proliferation and survival, enhanced antigen specific immune response, and spontaneous NF-κB activation [1, 21]. Our laboratory has shown that normal and malignant mouse and human B lymphocytes express PPARγ and that exposure to certain PPARγ ligands inhibits their proliferation and can induce apoptosis [24, 113, 119]. Several anti-inflammatory mechanisms of PPARγ have been suggested, including inhibition of NF-κB, AP1 and STAT transcription factors [120, 121]. A recent study demonstrated that some of these effects are PPARγ-independent [122]. PPARγ also regulates inflammation by blocking gene transcription through “transrepression.” Several models of transrepression by PPARγ have been proposed. In one of them, PPARγ-RXR complexes are thought to sequester coactivators, thereby downregulating other transcription factors. A second model suggests that interactions between transcription factors result in mutual antagonism of gene activation [123]. A recent report by Pascual et al. demonstrated a PPARγ ligand-dependent sumoylation of PPARγ that leads to its recruitment to repressor complexes in the promoter regions of inflammatory genes regulated by NF-κB. This prevents their release and suppresses proinflammatory gene expression [124].
PPARγ also plays a role in T lymphocyte regulation, and its level is upregulated following activation [5, 125]. PPARγ ligands inhibit T lymphocyte proliferation and reduce the production of IFNγ, TNFα, and IL-2 [23, 126, 127]. These inhibitory effects result from the direct interaction between PPARγ and the transcription factor nuclear factor of activated T cells (NFAT) [128]. Recent observations reported by Wohlfert et al. could illuminate yet another mechanism through which PPARγ controls immune responses [129]. They investigated the connection between PPARγ and CD4+ CD25+ regulatory T lymphocytes (Tregs). Tregs have been demonstrated to play a key role in regulating autoimmunity and immune responses [130–132]. There are two different subtypes of Tregs: thymus-derived natural Tregs (nTregs) and inducible or adaptive Tregs (iTregs). nTregs are always present in normal individuals as a functionally mature population constitutively expressing CD25, while iTregs are CD4+ CD25+ T lymphocytes which differentiate from CD4+ CD25− effector T lymphocytes in the periphery under a specific cytokine stimulation [133, 134]. Wohlfert et al. showed that ciglitazone enhanced the conversion of effector T lymphocytes into iTregs. Moreover, PPARγ expression in nTregs was required for the in vivo effects of ligand treatment in a murine model of graft-versus-host disease. These findings suggest that PPARγ ligands may enhance the activity of regulatory T lymphocytes while dampening the activation of other T lymphocyte subsets. The anti-inflammatory potential of PPARγ may be relevant to TED because this transcription factor is present in orbital tissues from TED patients, its activity may be involved in the regulation of IFNγ-induced chemokine expression, and its activators might attenuate the recruitment of activated T lymphocytes to sites of inflammation [35, 106, 118, 135, 136]. Together, the evidence indicates that PPARγ ligands could interrupt communication between mononuclear cells and fibroblasts [1, 35, 50]. However, PPARγ ligands may also promote T lymphocyte synthesis of IL-8 [137, 138]. Thus, the effects of PPARγ on T lymphocytes are complex and require further study.
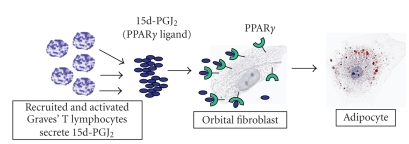
End-stage TED can culminate with permanent pathological changes including the differentiation of fibroblasts to adipocytes that contribute to increased connective tissue volume [28]. Adipogenesis is regulated by the interplay of several factors, including PPARα and γ [8, 28, 42, 139]. Natural and synthetic activators of PPARγ are known to stimulate lipid accumulation and the expression and secretion of adiponectin [28, 34, 139, 140]. PPARγ antagonists prevent triglyceride accumulation in orbital fibroblasts exposed to PPARγ agonists. This supports the concept that PPARγ expression and activation are crucial for adipocytic differentiation [28, 35, 36]. PPARγ levels are higher in orbital tissue from patients with active TED than in controls or individuals with inactive TED [35, 135]. Responses of orbital fibroblasts to PPARγ ligands provide an interesting link to T lymphocyte activity. T lymphocytes from patients with GD express constitutively high levels of Cox-2, and produce substantial PGD2 and 15d-PGJ2 [28, 141]. We have developed the model depicted in Figure 2, in which T lymphocyte infiltration of the orbit results in adipocytic differentiation of fibroblasts [28, 142]. In fact, coculture of orbital fibroblasts from TED patients with activated T lymphocytes results in cytoplasmic accumulation of lipid droplets in fibroblasts [28].
Figure 2.
T lymphocytes in TED patients express constitutively elevated levels of Cox-2, one enzyme critical to the production of the naturally-occurring PPARγ ligand 15d-PGJ2. When these lymphocytes infiltrate the orbit, 15d-PGJ2 is secreted in resident fibroblasts result in their differentiation into adipocytes.
5. PPARγ AND TISSUE REMODELING
Adipogenesis has been suggested to be a mechanism for stanching chronic inflammation [28]. Alternatively, this process may promote further inflammation by increasing proinflammatory adipocytokine production [36]. Orbital adipocytes express immunoreactive and functional TSH-R [8, 34, 54, 87, 95, 97, 98]. Positive correlation between TSH-R, PPARγ, and other adipocytic differentiation markers has been observed in tissues from TED patients [34]. Upregulation of an autoantigen on the surface of orbital fibroblasts could enhance the recruitment of autoreactive T lymphocytes to the orbit, fueling inflammation [36, 55]. Whether adipogenesis serves to abate or amplify inflammation, the associated increase in orbital tissue mass is undesirable. Thus, despite anti-inflammatory actions of PPARγ, its proadipogenic functions in the orbit might worsen the disease, contraindicating the use of agents activating this pathway in TED [36]. Several case reports have described development of exophthalmos in patients receiving TZD treatment for type 2 diabetes [28, 36, 143]. In particular, a patient with stable and inactive TED experienced aggravated disease with orbital fat expansion following pioglitazone therapy [28, 35, 36].
6. PPARγ AS A THERAPEUTIC TARGET
PPARγ modulators with selective activities would be required if PPARγ function is to be targeted as a TED therapeutic. Identification of selective PPARγ modulators, or SPPARγMs, has been sought as a better therapy for type 2 diabetes [3, 144]. In this context, designing partial PPARγ agonists that display insulin-sensitizing activity but lack adipogenic properties might be attractive [3, 144, 145]. The SPPARγMs take advantage of both the large ligand-binding domain of PPARγ and the complex interactions between PPARγ and its coactivators and corepressors [1, 3, 144, 146]. The ligand binding domain mediates interactions with transcriptional coactivator or corepressor proteins through ligand-dependent conformational changes in the C-terminal activation function 2 (AF2) α-helix [1, 144, 146]. In the absence of ligand, PPARγ functions as an active transcriptional repressor by binding both target genes and transcriptional corepressors [1]. Binding of classical ligands causes the AF2 α-helix to move in such a way that a high-affinity binding site for nuclear receptor coactivator proteins is created while corepressor proteins are dislodged from their binding sites [1, 144, 146–149]. Therefore, the structural change in AF2 resulting from agonist binding serves to both inhibit corepressor interaction and promote coactivator recruitment [1]. Because the position of the AF2 domain relative to the ligand binding domain determines whether coactivators or corepressors are recruited, ligands that fit into the binding domain without directly interacting with the AF2 helix, such as SPPARγMs, can act as agonists for some receptor functions and as antagonists for others [1, 3, 144, 145, 150–153].
Although not yet clinically available, several SPPARγMs have shown promise as potential glucose-lowering agents in type 2 diabetes. For example, metaglidasen has been shown in vitro to act as a partial PPARγ agonist/antagonist, with only a weak ability to recruit coactivators, such as CBP, DRIP205/TRAP220, and p300 [144]. Compared to rosiglitazone, metaglidasen is less adipogenic in primary human adipocytes and mouse 3T3-L1 adipocytes. In rodent models of insulin resistance, both metaglidasen and another SPPARγM, PAT5A, increased insulin sensitivity to levels comparable to those seen with rosiglitazone, with only weak adipogenic potential [3, 144, 154]. Consistent with the preclinical findings, metaglidasen appears to have comparable efficacy to pioglitazone and rosiglitazone in type 2 diabetics, without the undesirable side effect of weight gain [144]. Since developing SPPARγMs to target insulin resistance seems achievable, it is anticipated that the anti-inflammatory properties of PPARγ will be targeted in the future [3].
7. FUTURE PROSPECTS
PPARγ may play an important role in the development of TED. Studies have taken advantage of the availability of orbital tissue from TED patients. Orbital tissues from patients with GD but without TED are far less available. Potential differences between orbital tissues from “normal” and TED patients have not been fully explored. Similarly, few comparisons between tissues from early and late stage TED patients have been possible. Thus, an animal model of TED with fidelity to human disease is critical.
T lymphocytes and fibroblasts exist as multiple phenotypic subsets in the orbit. Aniszewski et al. [82] found that the phenotypes of orbital T lymphocytes in TED patients changed with disease duration. From that report, the T helper lymphocyte Th1 subset may predominate early, while Th2 lymphocytes may become more abundant later. Furthermore, as discussed previously, the role of Tregs in TED may differ from that of Th1 and Th2 lymphocytes. Studies comparing PPARγ expression and function in each of these subpopulations may lead to better understanding of the role that this transcription factor plays in TED.
Like T lymphocytes, orbital fibroblasts exist in multiple subpopulations. Two major subsets of orbital fibroblast are defined based on their expression of a surface protein known as Thy-1 (CD90) whose function is unknown [37, 73, 155, 156]. The balance between Thy-1 negative and Thy-1 positive populations in the orbit may prove important to normal regulation of inflammation because these subsets exhibit distinct biosynthetic capabilities [73]. However, this balance may also be critical to the development and progression of TED. Depending on the signaling environment and their phenotype, fibroblasts can be stimulated to differentiate into myofibroblasts or lipofibroblasts [37, 157]. Myofibroblasts are important in wound healing, but they may also contribute to fibrosis in late-stage TED patients [158]. The presence of lipofibroblasts is an indication of pathology; in TED, their presence may result in excess orbital fat deposition [28]. Data suggest that the potential for terminal differentiation depends on Thy-1 display. TGF-β triggers differentiation of Thy-1+ fibroblasts into myofibroblasts, identified by their expression of α-SMA [157]. Adipocytic differentiation occurs in the Thy-1− subset [37, 157]. PPARγ expression or function may differ between Thy-1+ and Thy-1− subsets, explaining their divergent potential for differentiation.
Finally, TED is one of several pathological conditions in which chronic inflammation leads to tissue remodeling and inappropriate fat deposition. Sjögren syndrome, inflammatory bowel disease, nonalcoholic fatty liver disease, and atherosclerosis are examples [159–162]. PPARγ has been shown to play a major role in the regulation of atherogenesis by countering the inflammation-provoking action of platelet adhesion and activation [3]. Because PPARγ has been implicated in these diseases, it may prove an important determinant in diseases such as TED.
ACKNOWLEDGMENTS
This research was supported by Grants no. EY014564, EY017123, EY011708, ES01247, DE011390, EY08976, DK063121, T32 HL66988, and T32 HL007152, as well as the Research to Prevent Blindness Foundation. The continued support of the Bell Charitable Foundation is gratefully acknowledged.
References
- 1.Glass CK, Ogawa S. Combinatorial roles of nuclear receptors in inflammation and immunity. Nature Reviews Immunology. 2006;6(1):44–55. doi: 10.1038/nri1748. [DOI] [PubMed] [Google Scholar]
- 2.Duez H, Fruchart J-C, Staels B. PPARs in inflammation, atherosclerosis and thrombosis. Journal of Cardiovascular Risk. 2001;8(4):187–194. doi: 10.1177/174182670100800402. [DOI] [PubMed] [Google Scholar]
- 3.Ray DM, Spinelli SL, O'Brien JJ, Blumberg N, Phipps RP. Platelets as a novel target for PPARγ ligands: implications for inflammation, diabetes, and cardiovascular disease. BioDrugs. 2006;20(4):231–241. doi: 10.2165/00063030-200620040-00004. [DOI] [PubMed] [Google Scholar]
- 4.Braissant O, Foufelle F, Scotto C, Dauça M, Wahli W. Differential expression of peroxisome proliferator-activated receptors (PPARs): tissue distribution of PPAR-α, -β, and -γ in the adult rat. Endocrinology. 1996;137(1):354–366. doi: 10.1210/endo.137.1.8536636. [DOI] [PubMed] [Google Scholar]
- 5.Harris SG, Phipps RP. The nuclear receptor PPAR γ is expressed by mouse T lymphocytes and PPAR γ agonists induce apoptosis. European Journal of Immunology. 2001;31(4):1098–1105. doi: 10.1002/1521-4141(200104)31:4<1098::aid-immu1098>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 6.Ray DM, Bernstein SH, Phipps RP. Human multiple myeloma cells express peroxisome proliferator-activated receptor γ and undergo apoptosis upon exposure to PPARγ ligands. Clinical Immunology. 2004;113(2):203–213. doi: 10.1016/j.clim.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Jones DC, Ding X, Daynes RA. Nuclear receptor peroxisome proliferator-activated receptor α (PPARα) is expressed in resting murine lymphocytes. The PPARα in T and B lymphocytes is both transactivation and transrepression competent. Journal of Biological Chemistry. 2002;277(9):6838–6845. doi: 10.1074/jbc.M106908200. [DOI] [PubMed] [Google Scholar]
- 8.Pasquali D, Pierantoni GM, Fusco A, et al. Fenofibrate increases the expression of high mobility group AT-hook 2 (HMGA2) gene and induces adipocyte differentiation of orbital fibroblasts from Graves' ophthalmopathy. Journal of Molecular Endocrinology. 2004;33(1):133–143. doi: 10.1677/jme.0.0330133. [DOI] [PubMed] [Google Scholar]
- 9.Auboeuf D, Rieusset J, Fajas L, et al. Tissue distribution and quantification of the expression of mRNAs of peroxisome proliferator-activated receptors and liver X receptor-α in humans: no alteration in adipose tissue of obese and NIDDM patients. Diabetes. 1997;46(8):1319–1327. doi: 10.2337/diab.46.8.1319. [DOI] [PubMed] [Google Scholar]
- 10.Marx N, Duez H, Fruchart J-C, Staels B. Peroxisome proliferator-activated receptors and atherogenesis: regulators of gene expression in vascular cells. Circulation Research. 2004;94(9):1168–1178. doi: 10.1161/01.RES.0000127122.22685.0A. [DOI] [PubMed] [Google Scholar]
- 11.Plutzky J. Inflammation in atherosclerosis and diabetes mellitus. Reviews in Endocrine & Metabolic Disorders. 2004;5(3):255–259. doi: 10.1023/B:REMD.0000032414.17672.5c. [DOI] [PubMed] [Google Scholar]
- 12.Auwerx J, Schoonjans K, Fruchart J-C, Staels B. Transcriptional control of triglyceride metabolism: fibrates and fatty acids change the expression of the LPL and apo C-III genes by activating the nuclear receptor PPAR. Atherosclerosis. 1996;124(supplement 1):S29–S37. doi: 10.1016/0021-9150(96)05854-6. [DOI] [PubMed] [Google Scholar]
- 13.Brown JD, Plutzky J. Peroxisome proliferator-activated receptors as transcriptional nodal points and therapeutic targets. Circulation. 2007;115(4):518–533. doi: 10.1161/CIRCULATIONAHA.104.475673. [DOI] [PubMed] [Google Scholar]
- 14.Zhou X, Benson KF, Ashar HR, Chada K. Mutation responsible for the mouse pygmy phenotype in the developmentally regulated factor HMGI-C. Nature. 1995;376(6543):771–774. doi: 10.1038/376771a0. [DOI] [PubMed] [Google Scholar]
- 15.Battista S, Fidanza V, Fedele M, et al. The expression of a truncated HMGI-C gene induces gigantism associated with lipomatosis. Cancer Research. 1999;59(19):4793–4797. [PubMed] [Google Scholar]
- 16.Anand A, Chada K. In vivo modulation of Hmgic reduces obesity. Nature Genetics. 2000;24(4):377–380. doi: 10.1038/74207. [DOI] [PubMed] [Google Scholar]
- 17.Arlotta P, Tai AK-F, Manfioletti G, Clifford C, Jay G, Ono SJ. Transgenic mice expressing a truncated form of the high mobility group I-C protein develop adiposity and an abnormally high prevalence of lipomas. Journal of Biological Chemistry. 2000;275(19):14394–14400. doi: 10.1074/jbc.m000564200. [DOI] [PubMed] [Google Scholar]
- 18.Brandes R, Arad R, Bar-Tana J. Adipose conversion of cultured rat primary preadipocytes by hypolipidemic drugs. Biochimica et Biophysica Acta. 1986;877(2):314–321. doi: 10.1016/0005-2760(86)90309-7. [DOI] [PubMed] [Google Scholar]
- 19.Nencioni A, Grünebach F, Zobywlaski A, Denzlinger C, Brugger W, Brossart P. Dendritic cell immunogenicity is regulated by peroxisome proliferator-activated receptor γ . Journal of Immunology. 2002;169(3):1228–1235. doi: 10.4049/jimmunol.169.3.1228. [DOI] [PubMed] [Google Scholar]
- 20.Akbiyik F, Ray DM, Gettings KF, Blumberg N, Francis CW, Phipps RP. Human bone marrow megakaryocytes and platelets express PPARγ, and PPARγ agonists blunt platelet release of CD40 ligand and thromboxanes. Blood. 2004;104(5):1361–1368. doi: 10.1182/blood-2004-03-0926. [DOI] [PubMed] [Google Scholar]
- 21.Setoguchi K, Misaki Y, Terauchi Y, et al. Peroxisome proliferator-activated receptor-γ haploinsufficiency enhances B cell proliferative responses and exacerbates experimentally induced arthritis. Journal of Clinical Investigation. 2001;108(11):1667–1675. doi: 10.1172/JCI13202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cunard R, Ricote M, DiCampli D, et al. Regulation of cytokine expression by ligands of peroxisome proliferator activated receptors. Journal of Immunology. 2002;168(6):2795–2802. doi: 10.4049/jimmunol.168.6.2795. [DOI] [PubMed] [Google Scholar]
- 23.Clark RB, Bishop-Bailey D, Estrada-Hernandez T, Hla T, Puddington L, Padula SJ. The nuclear receptor PPARγ and immunoregulation: PPARγ mediates inhibition of helper T cell responses. Journal of Immunology. 2000;164(3):1364–1371. doi: 10.4049/jimmunol.164.3.1364. [DOI] [PubMed] [Google Scholar]
- 24.Padilla J, Leung E, Phipps RP. Human B lymphocytes and B lymphomas express PPAR-γ and are killed by PPAR-γ agonists. Clinical Immunology. 2002;103(1):22–33. doi: 10.1006/clim.2001.5181. [DOI] [PubMed] [Google Scholar]
- 25.Ricote M, Li AC, Willson TM, Kelly CJ, Glass CK. The peroxisome proliferator-activated receptor-γ is a negative regulator of macrophage activation. Nature. 1998;391(6662):79–82. doi: 10.1038/34178. [DOI] [PubMed] [Google Scholar]
- 26.Fajas L, Auboeuf D, Raspé E, et al. The organization, promoter analysis, and expression of the human PPARγ gene. Journal of Biological Chemistry. 1997;272(30):18779–18789. doi: 10.1074/jbc.272.30.18779. [DOI] [PubMed] [Google Scholar]
- 27.Ricote M, Huang J, Fajas L, et al. Expression of the peroxisome proliferator-activated receptor γ (PPARγ) in human atherosclerosis and regulation in macrophages by colony stimulating factors and oxidized low density lipoprotein. Proceedings of the National Academy of Sciences of the United States of America. 1998;95(13):7614–7619. doi: 10.1073/pnas.95.13.7614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Feldon SE, O'Loughlin CW, Ray DM, Landskroner-Eiger S, Seweryniak KE, Phipps RP. Activated human T lymphocytes express cyclooxygenase-2 and produce proadipogenic prostaglandins that drive human orbital fibroblast differentiation to adipocytes. The American Journal of Pathology. 2006;169(4):1183–1193. doi: 10.2353/ajpath.2006.060434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lehmann JM, Moore LB, Smith-Oliver TA, Wilkison WO, Willson TM, Kliewer SA. An antidiabetic thiazolidinedione is a high affinity ligand for peroxisome proliferator-activated receptor γ (PPARγ) Journal of Biological Chemistry. 1995;270(22):12953–12956. doi: 10.1074/jbc.270.22.12953. [DOI] [PubMed] [Google Scholar]
- 30.McIntyre TM, Pontsler AV, Silva AR, et al. Identification of an intracellular receptor for lysophosphatidic acid (LPA): LPA is a transcellular PPARγ agonist. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(1):131–136. doi: 10.1073/pnas.0135855100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schopfer FJ, Lin Y, Baker PRS, et al. Nitrolinoleic acid: an endogenous peroxisome proliferator-activated receptor γ ligand. Proceedings of the National Academy of Sciences of the United States of America. 2005;102(7):2340–2345. doi: 10.1073/pnas.0408384102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Forman BM, Tontonoz P, Chen J, Brun RP, Spiegelman BM, Evans RM. 15-deoxy-Δ12,14-prostaglandin J 2 is a ligand for the adipocyte determination factor PPARγ . Cell. 1995;83(5):803–812. doi: 10.1016/0092-8674(95)90193-0. [DOI] [PubMed] [Google Scholar]
- 33.Kliewer SA, Lenhard JM, Willson TM, Patel I, Morris DC, Lehmann JM. A prostaglandin J 2 metabolite binds peroxisome proliferator-activated receptor γ and promotes adipocyte differentiation. Cell. 1995;83(5):813–819. doi: 10.1016/0092-8674(95)90194-9. [DOI] [PubMed] [Google Scholar]
- 34.Kumar S, Coenen MJ, Scherer PE, Bahn RS. Evidence for enhanced adipogenesis in the orbits of patients with Graves' ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 2004;89(2):930–935. doi: 10.1210/jc.2003-031427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Antonelli A, Rotondi M, Ferrari SM, et al. Interferon-γ-inducible α-chemokine CXCL10 involvement in Graves' ophthalmopathy: modulation by peroxisome proliferator-activated receptor-γ agonists. Journal of Clinical Endocrinology & Metabolism. 2006;91(2):614–620. doi: 10.1210/jc.2005-1689. [DOI] [PubMed] [Google Scholar]
- 36.Starkey K, Heufelder AE, Baker G, et al. Peroxisome proliferator-activated receptor-γ in thyroid eye disease: contraindication for thiazolidinedione use? Journal of Clinical Endocrinology & Metabolism. 2003;88(1):55–59. doi: 10.1210/jc.2002-020987. [DOI] [PubMed] [Google Scholar]
- 37.Smith TJ, Koumas L, Gagnon A, et al. Orbital fibroblast heterogeneity may determine the clinical presentation of thyroid-associated ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 2002;87(1):385–392. doi: 10.1210/jcem.87.1.8164. [DOI] [PubMed] [Google Scholar]
- 38.Söderström M, Wigren J, Surapureddi S, Glass CK, Hammarström S. Novel prostaglandin D2-derived activators of peroxisome proliferator-activated receptor-γ are formed in macrophage cell cultures. Biochimica et Biophysica Acta. 2003;1631(1):35–41. doi: 10.1016/s1388-1981(02)00322-0. [DOI] [PubMed] [Google Scholar]
- 39.Kim J, Yang P, Suraokar M, et al. Suppression of prostate tumor cell growth by stromal cell prostaglandin D synthase-derived products. Cancer Research. 2005;65(14):6189–6198. doi: 10.1158/0008-5472.CAN-04-4439. [DOI] [PubMed] [Google Scholar]
- 40.Fukushima M. Biological activities and mechanisms of action of PGJ2 and related compounds: an update. Prostaglandins, Leukotrienes and Essential Fatty Acids. 1992;47(1):1–12. doi: 10.1016/0952-3278(92)90178-l. [DOI] [PubMed] [Google Scholar]
- 41.Fitzpatrick FA, Wynalda MA. Albumin-catalyzed metabolism of prostaglandin D2. Identification of products formed in vitro. Journal of Biological Chemistry. 1983;258(19):11713–11718. [PubMed] [Google Scholar]
- 42.Tontonoz P, Hu E, Spiegelman BM. Stimulation of adipogenesis in fibroblasts by PPARγ2, a lipid-activated transcription factor. Cell. 1994;79(7):1147–1156. doi: 10.1016/0092-8674(94)90006-x. [DOI] [PubMed] [Google Scholar]
- 43.Kubota N, Terauchi Y, Miki H, et al. PPARγ mediates high-fat diet-induced adipocyte hypertrophy and insulin resistance. Molecular Cell. 1999;4(4):597–609. doi: 10.1016/s1097-2765(00)80210-5. [DOI] [PubMed] [Google Scholar]
- 44.Rosen ED, Sarraf P, Troy AE, et al. PPARγ is required for the differentiation of adipose tissue in vivo and in vitro. Molecular Cell. 1999;4(4):611–617. doi: 10.1016/s1097-2765(00)80211-7. [DOI] [PubMed] [Google Scholar]
- 45.Delerive P, Fruchart J-C, Staels B. Peroxisome proliferator-activated receptors in inflammation control. Journal of Endocrinology. 2001;169(3):453–459. doi: 10.1677/joe.0.1690453. [DOI] [PubMed] [Google Scholar]
- 46.Kazim M, Goldberg RA, Smith TJ. Insights into the pathogenesis of thyroid-associated orbitopathy: evolving rationale for therapy. Archives of Ophthalmology. 2002;120(3):380–386. doi: 10.1001/archopht.120.3.380. [DOI] [PubMed] [Google Scholar]
- 47.Han R, Smith TJ. T helper type 1 and type 2 cytokines exert divergent influence on the induction of prostaglandin E2 and hyaluronan synthesis by interleukin-1β in orbital fibroblasts: implications for the pathogenesis of thyroid-associated ophthalmopathy. Endocrinology. 2006;147(1):13–19. doi: 10.1210/en.2005-1018. [DOI] [PubMed] [Google Scholar]
- 48.Smith TJ, Hoa N. Immunoglobulins from patients with Graves' disease induce hyaluronan synthesis in their orbital fibroblasts through the self-antigen, insulin-like growth factor-I receptor. Journal of Clinical Endocrinology & Metabolism. 2004;89(10):5076–5080. doi: 10.1210/jc.2004-0716. [DOI] [PubMed] [Google Scholar]
- 49.Smith TJ, Bahn RS, Gorman CA. Connective tissue, glycosaminoglycans, and diseases of the thyroid. Endocrine Reviews. 1989;10(3):366–391. doi: 10.1210/edrv-10-3-366. [DOI] [PubMed] [Google Scholar]
- 50.Feldon SE, John Park DJ, O'Loughlin CW, et al. Autologous T-lymphocytes stimulate proliferation of orbital fibroblasts derived from patients with Graves' ophthalmopathy. Investigative Ophthalmology & Visual Science. 2005;46(11):3913–3921. doi: 10.1167/iovs.05-0605. [DOI] [PubMed] [Google Scholar]
- 51.Kahaly G, Förster G, Hansen C. Glycosaminoglycans in thyroid eye disease. Thyroid. 1998;8(5):429–432. doi: 10.1089/thy.1998.8.429. [DOI] [PubMed] [Google Scholar]
- 52.Tallstedt L, Norberg R. Immunohistochemical staining of normal and Graves' extraocular muscle. Investigative Ophthalmology & Visual Science. 1988;29(2):175–184. [PubMed] [Google Scholar]
- 53.Trokel SL, Jakobiec FA. Correlation of CT scanning and pathologic features of ophthalmic Graves' disease. Ophthalmology. 1981;88(6):553–564. doi: 10.1016/s0161-6420(81)34993-8. [DOI] [PubMed] [Google Scholar]
- 54.Zhang L, Baker G, Janus D, Paddon CA, Fuhrer D, Ludgate M. Biological effects of thyrotropin receptor activation on human orbital preadipocytes. Investigative Ophthalmology & Visual Science. 2006;47(12):5197–5203. doi: 10.1167/iovs.06-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ludgate M, Baker G. Unlocking the immunological mechanisms of orbital inflammation in thyroid eye disease. Clinical & Experimental Immunology. 2002;127(2):193–198. doi: 10.1046/j.1365-2249.2002.01792.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatton MP, Rubin PA. The pathophysiology of thyroid-associated ophthalmopathy. Ophthalmology Clinics of North America. 2002;15(1):113–119. doi: 10.1016/s0896-1549(01)00004-9. [DOI] [PubMed] [Google Scholar]
- 57.Bahn RS, Heufelder AE. Pathogenesis of Graves' ophthalmopathy. The New England Journal of Medicine. 1993;329(20):1468–1475. doi: 10.1056/NEJM199311113292007. [DOI] [PubMed] [Google Scholar]
- 58.Prabhakar BS, Bahn RS, Smith TJ. Current perspective on the pathogenesis of Graves' disease and ophthalmopathy. Endocrine Reviews. 2003;24(6):802–835. doi: 10.1210/er.2002-0020. [DOI] [PubMed] [Google Scholar]
- 59.Douglas RS, Gianoukakis AG, Goldberg RA, Kamat S, Smith TJ. Circulating mononuclear cells from euthyroid patients with thyroid-associated ophthalmopathy exhibit characteristic phenotypes. Clinical & Experimental Immunology. 2007;148(1):64–71. doi: 10.1111/j.1365-2249.2006.03316.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Rapoport B, Alsabeh R, Aftergood D, McLachlan SM. Elephantiasic pretibial myxedema: insight into and a hypothesis regarding the pathogenesis of the extrathyroidal manifestations of Graves' disease. Thyroid. 2000;10(8):685–692. doi: 10.1089/10507250050137761. [DOI] [PubMed] [Google Scholar]
- 61.Daumerie C, Ludgate M, Costagliola S, Many MC. Evidence for thyrotropin receptor immunoreactivity in pretibial connective tissue from patients with thyroid-associated dermopathy. European Journal of Endocrinology. 2002;146(1):35–38. doi: 10.1530/eje.0.1460035. [DOI] [PubMed] [Google Scholar]
- 62.Kim JM, LaBree L, Levin L, Feldon SE. The relation of Graves' ophthalmopathy to circulating thyroid hormone status. British Journal of Ophthalmology. 2004;88(1):72–74. doi: 10.1136/bjo.88.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Burch HB, Wartofsky L. Graves' ophthalmopathy: current concepts regarding pathogenesis and management. Endocrine Reviews. 1993;14(6):747–793. doi: 10.1210/edrv-14-6-747. [DOI] [PubMed] [Google Scholar]
- 64.Reid JR, Wheeler SF. Hyperthyroidism: diagnosis and treatment. American Family Physician. 2005;72(4):623–630. [PubMed] [Google Scholar]
- 65.Bartalena L, Wiersinga WM, Pinchera A. Graves' ophthalmopathy: state of the art and perspectives. Journal of Endocrinological Investigation. 2004;27(3):295–301. doi: 10.1007/BF03345280. [DOI] [PubMed] [Google Scholar]
- 66.Smith TJ. Insights into the role of fibroblasts in human autoimmune diseases. Clinical & Experimental Immunology. 2005;141(3):388–397. doi: 10.1111/j.1365-2249.2005.02824.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Khoo DH, Ho SC, Seah LL, et al. The combination of absent thyroid peroxidase antibodies and high thyroid-stimulating immunoglobulin levels in Graves' disease identifies a group at markedly increased risk of ophthalmopathy. Thyroid. 1999;9(12):1175–1180. doi: 10.1089/thy.1999.9.1175. [DOI] [PubMed] [Google Scholar]
- 68.Wright-Pascoe R, Smikle MF, Barton EN, James OB. Limited usefulness of antithyroperoxidase and antithyroglobulin assays in Jamaicans with Graves' disease. Human Antibodies. 1999;9(3):161–164. [PubMed] [Google Scholar]
- 69.Eckstein AK, Plicht M, Lax H, et al. Clinical results of anti-inflammatory therapy in Graves' ophthalmopathy and association with thyroidal autoantibodies. Clinical Endocrinology. 2004;61(5):612–618. doi: 10.1111/j.1365-2265.2004.02143.x. [DOI] [PubMed] [Google Scholar]
- 70.Liu D, Feldon SE. Thyroid ophthalmopathy. Ophthalmology Clinics of North America. 1992;5:597–622. [Google Scholar]
- 71.Lehmann GM, Feldon SE, Smith TJ, Phipps RP. Immune mechanisms in thyroid eye disease. doi: 10.1089/thy.2007.0407. Thyroid. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Smith RS, Smith TJ, Blieden TM, Phipps RP. Fibroblasts as sentinel cells. Synthesis of chemokines and regulation of inflammation. The American Journal of Pathology. 1997;151(2):317–322. [PMC free article] [PubMed] [Google Scholar]
- 73.Koumas L, Smith TJ, Phipps RP. Fibroblast subsets in the human orbit: Thy-1+ and Thy-1- subpopulations exhibit distinct phenotypes. European Journal of Immunology. 2002;32(2):477–485. doi: 10.1002/1521-4141(200202)32:2<477::AID-IMMU477>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- 74.Sempowski GD, Rozenblit J, Smith TJ, Phipps RP. Human orbital fibroblasts are activated through CD40 to induce proinflammatory cytokine production. American Journal of Physiology. 1998;274(3):C707–C714. doi: 10.1152/ajpcell.1998.274.3.C707. [DOI] [PubMed] [Google Scholar]
- 75.Smith TJ. Orbital fibroblasts exhibit a novel pattern of responses to proinflammatory cytokines: potential basis for the pathogenesis of thyroid-associated ophthalmopathy. Thyroid. 2002;12(3):197–203. doi: 10.1089/105072502753600133. [DOI] [PubMed] [Google Scholar]
- 76.Heufelder AE, Smith TJ, Gorman CA, Bahn RS. Increased induction of HLA-DR by interferon-γ in cultured fibroblasts derived from patients with Graves' ophthalmopathy and pretibial dermopathy. Journal of Clinical Endocrinology & Metabolism. 1991;73(2):307–313. doi: 10.1210/jcem-73-2-307. [DOI] [PubMed] [Google Scholar]
- 77.Smith TJ, Sempowski GD, Berenson CS, Cao HJ, Wang H-S, Phipps RP. Human thyroid fibroblasts exhibit a distinctive phenotype in culture: characteristic ganglioside profile and functional CD40 expression. Endocrinology. 1997;138(12):5576–5588. doi: 10.1210/endo.138.12.5563. [DOI] [PubMed] [Google Scholar]
- 78.Hufnagel TJ, Hickey WF, Cobbs WH, Jakobiec FA, Iwamoto T, Eagle RC. Immunohistochemical and ultrastructural studies on the exenterated orbital tissues of a patient with Graves' disease. Ophthalmology. 1984;91(11):1411–1419. doi: 10.1016/s0161-6420(84)34152-5. [DOI] [PubMed] [Google Scholar]
- 79.de Carli M, D'Elios MM, Mariotti S, et al. Cytolytic T cells with Th1-like cytokine profile predominate in retroorbital lymphocytic infiltrates of Graves' ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 1993;77(5):1120–1124. doi: 10.1210/jcem.77.5.8077301. [DOI] [PubMed] [Google Scholar]
- 80.Grubeck-Loebenstein B, Trieb K, Sztankay A, Holter W, Anderl H, Wick G. Retrobulbar T cells from patients with Graves' ophthalmopathy are CD8+ and specifically recognize autologous fibroblasts. Journal of Clinical Investigation. 1994;93(6):2738–2743. doi: 10.1172/JCI117289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Jaume JC, Portolano S, Prummel MF, McLachlan SM, Rapoport B. Molecular cloning and characterization of genes for antibodies generated by orbital tissue-infiltrating B-cells in Graves' ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 1994;78(2):348–352. doi: 10.1210/jcem.78.2.8106623. [DOI] [PubMed] [Google Scholar]
- 82.Aniszewski JP, Valyasevi RW, Bahn RS. Relationship between disease duration and predominant orbital T cell subset in Graves' ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 2000;85(2):776–780. doi: 10.1210/jcem.85.2.6333. [DOI] [PubMed] [Google Scholar]
- 83.Powell JD. The induction and maintenance of T cell anergy. Clinical Immunology. 2006;120(3):239–246. doi: 10.1016/j.clim.2006.02.004. [DOI] [PubMed] [Google Scholar]
- 84.Melchers F. Anergic B cells caught in the act. Immunity. 2006;25(6):864–867. doi: 10.1016/j.immuni.2006.11.003. [DOI] [PubMed] [Google Scholar]
- 85.Smith TJ. B cell depletion in Graves' disease: the right answer to the wrong question? Journal of Clinical Endocrinology & Metabolism. 2007;92(5):1620–1622. doi: 10.1210/jc.2007-0463. [DOI] [PubMed] [Google Scholar]
- 86.Cao HJ, Wang H-S, Zhang Y, Lin H-Y, Phipps RP, Smith TJ. Activation of human orbital fibroblasts through CD40 engagement results in a dramatic induction of hyaluronan synthesis and prostaglandin endoperoxide H synthase-2 expression: insights into potential pathogenic mechanisms of thyroid-associated ophthalmopathy. Journal of Biological Chemistry. 1998;273(45):29615–29625. doi: 10.1074/jbc.273.45.29615. [DOI] [PubMed] [Google Scholar]
- 87.Valyasevi RW, Erickson DZ, Harteneck DA, et al. Differentiation of human orbital preadipocyte fibroblasts induces expression of functional thyrotropin receptor. Journal of Clinical Endocrinology & Metabolism. 1999;84(7):2257–2562. doi: 10.1210/jcem.84.7.5838. [DOI] [PubMed] [Google Scholar]
- 88.Smith TJ, Sciaky D, Phipps RP, Jennings TA. CD40 expression in human thyroid tissue: evidence for involvement of multiple cell types in autoimmune and neoplastic diseases. Thyroid. 1999;9(8):749–755. doi: 10.1089/thy.1999.9.749. [DOI] [PubMed] [Google Scholar]
- 89.Cao HJ, Han R, Smith TJ. Robust induction of PGHS-2 by IL-1 in orbital fibroblasts results from low levels of IL-1 receptor antagonist expression. American Journal of Physiology. 2003;284(6):C1429–C1437. doi: 10.1152/ajpcell.00354.2002. [DOI] [PubMed] [Google Scholar]
- 90.Smith TJ, Jennings TA, Sciaky D, Cao HJ. Prostaglandin-endoperoxide H synthase-2 expression in human thyroid epithelium: evidence for constitutive expression in vivo and in cultured KAT- 50 cells. Journal of Biological Chemistry. 1999;274(22):15622–15632. doi: 10.1074/jbc.274.22.15622. [DOI] [PubMed] [Google Scholar]
- 91.Smith TJ. The putative role of prostaglandin endoperoxide H synthase-2 in the pathogenesis of thyroid-associated orbitopathy. Experimental and Clinical Endocrinology and Diabetes. 1999;107(supplement 5):S160–S163. doi: 10.1055/s-0029-1212175. [DOI] [PubMed] [Google Scholar]
- 92.Smith TJ. The putative role of fibroblasts in the pathogenesis of Graves' disease: evidence for the involvement of the insulin-like growth factor-1 receptor in fibroblast activation. Autoimmunity. 2003;36(6-7):409–415. doi: 10.1080/08916930310001603000. [DOI] [PubMed] [Google Scholar]
- 93.Smith TJ, Parikh SJ. HMC-1 mast cells activate human orbital fibroblasts in coculture: evidence for up-regulation of prostaglandin E2 and hyaluronan synthesis. Endocrinology. 1999;140(8):3518–3525. doi: 10.1210/endo.140.8.6881. [DOI] [PubMed] [Google Scholar]
- 94.Smith TJ. Unique properties of orbital connective tissue underlie its involvement in Graves' disease. Minerva Endocrinologica. 2003;28(3):213–222. [PubMed] [Google Scholar]
- 95.Bahn RS, Dutton CM, Natt N, Joba W, Spitzweg C, Heufelder AE. Thyrotropin receptor expression in Graves' orbital adipose/connective tissues: potential autoantigen in Graves' ophthalmopathy. Journal of Clinical Endocrinology & Metabolism. 1998;83(3):998–1002. doi: 10.1210/jcem.83.3.4676. [DOI] [PubMed] [Google Scholar]
- 96.Pritchard J, Han R, Horst N, Cruikshank WW, Smith TJ. Immunoglobulin activation of T cell chemoattractant expression in fibroblasts from patients with Graves' disease is mediated through the insulin-like growth factor I receptor pathway. Journal of Immunology. 2003;170(12):6348–6354. doi: 10.4049/jimmunol.170.12.6348. [DOI] [PubMed] [Google Scholar]
- 97.Feliciello A, Porcellini A, Ciullo I, Bonavolonta G, Avvedimento EV, Fenzi GF. Expression of thyrotropin-receptor mRNA in healthy and Graves' disease retro-orbital tissue. The Lancet. 1993;342(8867):337–338. doi: 10.1016/0140-6736(93)91475-2. [DOI] [PubMed] [Google Scholar]
- 98.Crisp MS, Lane C, Halliwell M, Wynford-Thomas D, Ludgate M. Thyrotropin receptor transcripts in human adipose tissue. Journal of Clinical Endocrinology & Metabolism. 1997;82(6):2003–2005. [PubMed] [Google Scholar]
- 99.Heufelder AE, Bahn RS. Detection and localization of cytokine immunoreactivity in retro-ocular connective tissue in Graves' ophthalmopathy. European Journal of Clinical Investigation. 1993;23(1):10–17. doi: 10.1111/j.1365-2362.1993.tb00712.x. [DOI] [PubMed] [Google Scholar]
- 100.Howland KC, Ausubel LJ, London CA, Abbas AK. The roles of CD28 and CD40 ligand in T cell activation and tolerance. Journal of Immunology. 2000;164(9):4465–4470. doi: 10.4049/jimmunol.164.9.4465. [DOI] [PubMed] [Google Scholar]
- 101.Van Gool SW, Vandenberghe P, de Boer M, Ceuppens JL. CD80, CD86 and CD40 provide accessory signals in a multiple-step T-Cell activation model. Immunological Reviews. 1996;(153):47–83. doi: 10.1111/j.1600-065x.1996.tb00920.x. [DOI] [PubMed] [Google Scholar]
- 102.Zhang Y, Cao HJ, Graf B, Meekins H, Smith TJ, Phipps RP. Cutting edge: CD40 engagement up-regulates cyclooxygenase-2 expression and prostaglandin E2 production in human lung fibroblasts. Journal of Immunology. 1998;160(3):1053–1057. [PubMed] [Google Scholar]
- 103.Otto EA, Ochs K, Hansen C, Wall JR, Kahaly GJ. Orbital tissue-derived T lymphocytes from patients with Graves’ ophthalmopathy recognize autologous orbital antigens. Journal of Clinical Endocrinology and Metabolism. 1996;81(8):3045–3050. doi: 10.1210/jcem.81.8.8768872. [DOI] [PubMed] [Google Scholar]
- 104.Desreumaux P, Dubuquoy L, Nutten S, et al. Attenuation of colon inflammation through activators of the retinoid X receptor (RXR)/peroxisome proliferator-activated receptor γ (PPARγ) heterodimer: a basis for new therapeutic strategies. Journal of Experimental Medicine. 2001;193(7):827–838. doi: 10.1084/jem.193.7.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Su CG, Wen X, Bailey ST, et al. A novel therapy for colitis utilizing PPAR-γ ligands to inhibit the epithelial inflammatory response. Journal of Clinical Investigation. 1999;104(4):383–389. doi: 10.1172/JCI7145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Schaefer KL, Denevich S, Ma C, et al. Intestinal antiinflammatory effects of thiazolidenedione peroxisome proliferator-activated receptor-γ ligands on T helper type 1 chemokine regulation include nontranscriptional control mechanisms. Inflammatory Bowel Diseases. 2005;11(3):244–252. doi: 10.1097/01.mib.0000160770.94199.9b. [DOI] [PubMed] [Google Scholar]
- 107.Feinstein DL, Galea E, Gavrilyuk V, et al. Peroxisome proliferator-activated receptor-γ agonists prevent experimental autoimmune encephalomyelitis. Annals of Neurology. 2002;51(6):694–702. doi: 10.1002/ana.10206. [DOI] [PubMed] [Google Scholar]
- 108.Diab A, Deng C, Smith JD, et al. Peroxisome proliferator-activated receptor-γ agonist 15-deoxy-Δ 12,14-prostaglandin J2 ameliorates experimental autoimmune encephalomyelitis. Journal of Immunology. 2002;168(5):2508–2515. doi: 10.4049/jimmunol.168.5.2508. [DOI] [PubMed] [Google Scholar]
- 109.Ellis CN, Varani J, Fisher GJ, et al. Troglitazone improves psoriasis and normalizes models of proliferative skin disease: ligands for peroxisome proliferator-activated receptor-γ inhibit keratinocyte proliferation. Archives of Dermatology. 2000;136(5):609–616. doi: 10.1001/archderm.136.5.609. [DOI] [PubMed] [Google Scholar]
- 110.Lewis JD, Lichtenstein GR, Stein RB, et al. An open-label trial of the PPARγ ligand rosiglitazone for active ulcerative colitis. The American Journal of Gastroenterology. 2001;96(12):3323–3328. doi: 10.1111/j.1572-0241.2001.05333.x. [DOI] [PubMed] [Google Scholar]
- 111.Kornbluth A. What happened to drug trials in ulcerative colitis? Problems, PPARs, placebos, and (possible) progress. American Journal of Gastroenterology. 2001;96(12):3232–3234. doi: 10.1111/j.1572-0241.2001.05319.x. [DOI] [PubMed] [Google Scholar]
- 112.Clark RB. The role of PPARs in inflammation and immunity. Journal of Leukocyte Biology. 2002;71(3):388–400. [PubMed] [Google Scholar]
- 113.Ray DM, Akbiyik F, Bernstein SH, Phipps RP. CD40 engagement prevents peroxisome proliferator-activated receptor γ agonist-induced apoptosis of B lymphocytes and B lymphoma cells by an NF-κB-dependent mechanism. Journal of Immunology. 2005;174(7):4060–4069. doi: 10.4049/jimmunol.174.7.4060. [DOI] [PubMed] [Google Scholar]
- 114.Ray DM, Akbiyik F, Phipps RP. The peroxisome proliferator-activated receptor γ (PPARγ) ligands 15-deoxyΔ 12,14-prostaglandin J2 and ciglitazone induce human B lymphocyte and B cell lymphoma apoptosis by PPARγ-independent mechanisms. Journal of Immunology. 2006;177(8):5068–5076. doi: 10.4049/jimmunol.177.8.5068. [DOI] [PubMed] [Google Scholar]
- 115.Jiang C, Ting AT, Seed B. PPAR-γ agonists inhibit production of monocyte inflammatory cytokines. Nature. 1998;391(6662):82–86. doi: 10.1038/34184. [DOI] [PubMed] [Google Scholar]
- 116.Ricote M, Welch JS, Glass CK. Regulation of macrophage gene expression by the peroxisome proliferator-activated receptor-γ . Hormone Research. 2000;54(5-6):275–280. doi: 10.1159/000053271. [DOI] [PubMed] [Google Scholar]
- 117.Bouhlel MA, Derudas B, Rigamonti E, et al. PPARγ activation primes human monocytes into alternative M2 macrophages with anti-inflammatory properties. Cell Metabolism. 2007;6(2):137–143. doi: 10.1016/j.cmet.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 118.Gosset P, Charbonnier A-S, Delerive P, et al. Peroxisome proliferator-activated receptor γ activators affect the maturation of human monocyte-derived dendritic cells. European Journal of Immunology. 2001;31(10):2857–2865. doi: 10.1002/1521-4141(2001010)31:10<2857::aid-immu2857>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 119.Padilla J, Kaur K, Cao HJ, Smith TJ, Phipps RP. Peroxisome proliferator activator receptor-γ agonists and 15-deoxy-Δ 12,14-PGJ2 induce apoptosis in normal and malignant B-lineage cells. Journal of Immunology. 2000;165(12):6941–6948. doi: 10.4049/jimmunol.165.12.6941. [DOI] [PubMed] [Google Scholar]
- 120.Chen F, Wang M, O'Connor JP, He M, Tripathi T, Harrison LE. Phosphorylation of PPARγ via active ERK1/2 leads to its physical association with p65 and inhibition of NF-κ β . Journal of Cellular Biochemistry. 2003;90(4):732–744. doi: 10.1002/jcb.10668. [DOI] [PubMed] [Google Scholar]
- 121.Welch JS, Ricote M, Akiyama TE, Gonzalez FJ, Glass CK. PPARγ and PPARδ negatively regulate specific subsets of lipopolysaccharide and IFN-γ target genes in macrophages. Proceedings of the National Academy of Sciences of the United States of America. 2003;100(11):6712–6717. doi: 10.1073/pnas.1031789100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chawla A, Barak Y, Nagy L, Liao D, Tontonoz P, Evans RM. PPAR-γ dependent and independent effects on macrophage-gene expression in lipid metabolism and inflammation. Nature Medicine. 2001;7(1):48–52. doi: 10.1038/83336. [DOI] [PubMed] [Google Scholar]
- 123.Daynes RA, Jones DC. Emerging roles of PPARs in inflammation and immunity. Nature Reviews Immunology. 2002;2(10):748–759. doi: 10.1038/nri912. [DOI] [PubMed] [Google Scholar]
- 124.Pascual G, Fong AL, Ogawa S, et al. A SUMOylation-dependent pathway mediates transrepression of inflammatory response genes by PPAR-γ . Nature. 2005;437(7059):759–763. doi: 10.1038/nature03988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Harris SG, Phipps RP. Peroxisome proliferator-activated receptor γ (PPAR-γ) activation in naive mouse T cells induces cell death. Annals of the New York Academy of Sciences. 2000;905:297–300. doi: 10.1111/j.1749-6632.2000.tb06565.x. [DOI] [PubMed] [Google Scholar]
- 126.Kim HJ, Rho YH, Choi SJ, et al. 15-deoxy-Δ 12,14-PGJ2 inhibits IL-6-induced Stat3 phosphorylation in lymphocytes. Experimental and Molecular Medicine. 2005;37(3):179–185. doi: 10.1038/emm.2005.24. [DOI] [PubMed] [Google Scholar]
- 127.Soller M, Tautenhahn A, Brüne B, et al. Peroxisome proliferator-activated receptor γ contributes to T lymphocyte apoptosis during sepsis. Journal of Leukocyte Biology. 2006;79(1):235–243. doi: 10.1189/jlb.0205058. [DOI] [PubMed] [Google Scholar]
- 128.Yang XY, Wang LH, Chen T, et al. Activation of human T lymphocytes is inhibited by peroxisome proliferator-activated receptor γ (PPARγ) agonists. PPARγ co-association with transcription factor NFAT. Journal of Biological Chemistry. 2000;275(7):4541–4544. doi: 10.1074/jbc.275.7.4541. [DOI] [PubMed] [Google Scholar]
- 129.Wohlfert EA, Nichols FC, Nevius E, Clark RB. Peroxisome proliferator-activated receptor γ (PPARγ) and immunoregulation: enhancement of regulatory T cells through PPARγ-dependent and -independent mechanisms. Journal of Immunology. 2007;178(7):4129–4135. doi: 10.4049/jimmunol.178.7.4129. [DOI] [PubMed] [Google Scholar]
- 130.Onizuka S, Tawara I, Shimizu J, Sakaguchi S, Fujita T, Nakayama E. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor α) monoclonal antibody. Cancer Research. 1999;59(13):3128–3133. [PubMed] [Google Scholar]
- 131.Edinger M, Hoffmann P, Ermann J, et al. CD4 +CD25 + regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow transplantation. Nature Medicine. 2003;9(9):1144–1150. doi: 10.1038/nm915. [DOI] [PubMed] [Google Scholar]
- 132.Paust S, Cantor H. Regulatory T cells and autoimmune disease. Immunological Reviews. 2005;204(1):195–207. doi: 10.1111/j.0105-2896.2005.00247.x. [DOI] [PubMed] [Google Scholar]
- 133.Bluestone JA, Abbas AK. Natural versus adaptive regulatory T cells. Nature Reviews Immunology. 2003;3(3):253–257. doi: 10.1038/nri1032. [DOI] [PubMed] [Google Scholar]
- 134.Chen W, Jin W, Hardegen N, et al. Conversion of peripheral CD4 +CD25 - naive T cells to CD4 +CD25 + regulatory T cells by TGF-β induction of transcription factor Foxp3 . Journal of Experimental Medicine. 2003;198(12):1875–1886. doi: 10.1084/jem.20030152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Mimura LY, Villares SMF, Monteiro MLR, Guazzelli IC, Bloise W. Peroxisome proliferator-activated receptor-γ gene expression in orbital adipose/connective tissues is increased during the active stage of Graves’ ophthalmopathy. Thyroid. 2003;13(9):845–850. doi: 10.1089/105072503322401032. [DOI] [PubMed] [Google Scholar]
- 136.Marx N, Mach F, Sauty A, et al. Peroxisome proliferator-activated receptor-γ activators inhibit IFN-γ-induced expression of the T cell-active CXC chemokines IP-10, Mig, and I-TAC in human endothelial cells. Journal of Immunology. 2000;164:6503–6508. doi: 10.4049/jimmunol.164.12.6503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Harris SG, Phipps RP. Prostaglandin D2, its metabolite 15-d-PGJ2, and peroxisome proliferator activated receptor-γ agonists induce apoptosis in transformed, but not normal, human T lineage cells. Immunology. 2002;105(1):23–34. doi: 10.1046/j.0019-2805.2001.01340.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Harris SG, Smith RS, Phipps RP. 15-deoxy-Δ 12,14-PGJ2 induces IL-8 production in human T cells by a mitogen-activated protein kinase pathway. Journal of Immunology. 2002;168(3):1372–1379. doi: 10.4049/jimmunol.168.3.1372. [DOI] [PubMed] [Google Scholar]
- 139.Zhang J, Fu M, Cui T, et al. Selective disruption of PPARγ2 impairs the development of adipose tissue and insulin sensitivity. Proceedings of the National Academy of Sciences of the United States of America. 2004;101(29):10703–10708. doi: 10.1073/pnas.0403652101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Rosen ED. The transcriptional basis of adipocyte development. Prostaglandins Leukotrienes and Essential Fatty Acids. 2005;73(1):31–34. doi: 10.1016/j.plefa.2005.04.004. [DOI] [PubMed] [Google Scholar]
- 141.Shibata T, Kondo M, Osawa T, Shibata N, Kobayashi M, Uchida K. 15-deoxy-Δ 12,14-prostaglandin J2. A prostaglandin D2 metabolite generated during inflammatory processes. Journal of Biological Chemistry. 2002;277(12):10459–10466. doi: 10.1074/jbc.M110314200. [DOI] [PubMed] [Google Scholar]
- 142.Kahaly G, Hansen C, Felke B, Dienes HP. Immunohistochemical staining of retrobulbar adipose tissue in Graves’ ophthalmopathy. Clinical Immunology and Immunopathology. 1994;73(1):53–62. doi: 10.1006/clin.1994.1169. [DOI] [PubMed] [Google Scholar]
- 143.Levin F, Kazim M, Smith TJ, Marcovici E. Rosiglitazone-induced proptosis. Archives of Ophthalmology. 2005;123(1):119–121. doi: 10.1001/archopht.123.1.119. [DOI] [PubMed] [Google Scholar]
- 144.Zhang F, Lavan BE, Gregoire FM. Selective modulators of PPAR-γ activity: molecular aspects related to obesity and side-effects. PPAR Research. 2007;2007:7 pages. doi: 10.1155/2007/32696.32696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Rangwala SM, Lazar MA. The dawn of the SPPARMs? Science STKE. 2002;(121):PE9. doi: 10.1126/stke.2002.121.pe9. [DOI] [PubMed] [Google Scholar]
- 146.Nolte RT, Wisely GB, Westin S, et al. Ligand binding and co-activator assembly of the peroxisome proliferator- activated receptor-γ . Nature. 1998;395(6698):137–143. doi: 10.1038/25931. [DOI] [PubMed] [Google Scholar]
- 147.Heery DM, Kalkhoven E, Hoare S, Parker MG. A signature motif in transcriptional co-activators mediates binding to nuclear receptors. Nature. 1997;387(6634):733–736. doi: 10.1038/42750. [DOI] [PubMed] [Google Scholar]
- 148.Darimont BD, Wagner RL, Apriletti JW, et al. Structure and specificity of nuclear receptor-coactivator interactions. Genes & Development. 1998;12:3343–3356. doi: 10.1101/gad.12.21.3343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Xu HE, Stanley TB, Montana VG, et al. Structural basis for antagonist-mediated recruitment of nuclear co-repressors by PPARα . Nature. 2002;415(6873):813–817. doi: 10.1038/415813a. [DOI] [PubMed] [Google Scholar]
- 150.Burgermeister E, Schnoebelen A, Flament A, et al. A novel partial agonist of peroxisome proliferator-activated receptor-γ (PPARγ) recruits PPARγ-coactivator-1α, prevents triglyceride accumulation, and potentiates insulin signaling in vitro. Molecular Endocrinology. 2006;20(4):809–830. doi: 10.1210/me.2005-0171. [DOI] [PubMed] [Google Scholar]
- 151.Miller AR, Etgen GJ. Novel peroxisome proliferator-activated receptor ligands for type 2 diabetes and the metabolic syndrome. Expert Opinion on Investigational Drugs. 2003;12(9):1489–1500. doi: 10.1517/13543784.12.9.1489. [DOI] [PubMed] [Google Scholar]
- 152.Cock T-A, Houten SM, Auwerx J. Peroxisome proliferator-activated receptor-γ: too much of a good thing causes harm. EMBO Reports. 2004;5(2):142–147. doi: 10.1038/sj.embor.7400082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Rocchi S, Picard F, Vamecq J, et al. A unique PPARγ ligand with potent insulin-sensitizing yet weak adipogenic activity. Molecular Cell. 2001;8(4):737–747. doi: 10.1016/s1097-2765(01)00353-7. [DOI] [PubMed] [Google Scholar]
- 154.Misra P, Chakrabarti R, Vikramadithyan RK, et al. PAT5A: a partial agonist of peroxisome proliferator-activated receptor γ is a potent antidiabetic thiazolidinedione yet weakly adipogenic. Journal of Pharmacology and Experimental Therapeutics. 2003;306(2):763–771. doi: 10.1124/jpet.103.049791. [DOI] [PubMed] [Google Scholar]
- 155.Smith TJ, Sempowski GD, Wang H-S, Del Vecchio PJ, Lippe SD, Phipps RP. Evidence for cellular heterogeneity in primary cultures of human orbital fibroblasts. Journal of Clinical Endocrinology and Metabolism. 1995;80(9):2620–2625. doi: 10.1210/jcem.80.9.7673404. [DOI] [PubMed] [Google Scholar]
- 156.Morris RJ, Ritter MA. Association of Thy-1 cell surface differentiation antigen with certain connective tissues in vivo. Cell and Tissue Research. 1980;206(3):459–475. doi: 10.1007/BF00237975. [DOI] [PubMed] [Google Scholar]
- 157.Koumas L, Smith TJ, Feldon S, Blumberg N, Phipps RP. Thy-1 expression in human fibroblast subsets defines myofibroblastic or lipofibroblastic phenotypes. The American Journal of Pathology. 2003;163(4):1291–1300. doi: 10.1016/S0002-9440(10)63488-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Gabbiani G. The myofibroblast: a key cell for wound healing and fibrocontractive diseases. Progress in Clinical and Biological Research. 1981;54:183–194. [PubMed] [Google Scholar]
- 159.Barish GD, Narkar VA, Evans RM. PPARδ: a dagger in the heart of the metabolic syndrome. Journal of Clinical Investigation. 2006;116(3):590–597. doi: 10.1172/JCI27955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Qureshi K, Abrams GA. Metabolic liver disease of obesity and role of adipose tissue in the pathogenesis of nonalcoholic fatty liver disease. World Journal of Gastroenterology. 2007;13(26):3540–3553. doi: 10.3748/wjg.v13.i26.3540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Izumi M, Eguchi K, Nakamura H, Nagataki S, Nakamura T. Premature fat deposition in the salivary glands associated with Sjogren syndrome: MR and CT evidence. American Journal of Neuroradiology. 1997;18(5):951–958. [PMC free article] [PubMed] [Google Scholar]
- 162.Desreumaux P, Ernst O, Geboes K, et al. Inflammatory alterations in mesenteric adipose tissue in Crohn’s disease. Gastroenterology. 1999;117(1):73–81. doi: 10.1016/s0016-5085(99)70552-4. [DOI] [PubMed] [Google Scholar]