Abstract
Context:
The Foot and Ankle Ability Measure (FAAM) is a region-specific, non–disease-specific outcome instrument that possesses many of the clinimetric qualities recommended for an outcome instrument. Evidence of validity to support the use of the FAAM is available in individuals with a wide array of ankle and foot disorders. However, additional evidence to support the use of the FAAM for those with chronic ankle instability (CAI) is needed.
Objective:
To provide evidence of construct validity for the FAAM based on hypothesis testing in athletes with CAI.
Design:
Between-groups comparison.
Setting:
Athletic training room.
Patients or Other Participants:
Thirty National Collegiate Athletic Association Division II athletes (16 men, 14 women) from one university.
Main Outcome Measure(s):
The FAAM including activities of daily living (ADL) and sports subscales and the global and categorical ratings of function.
Results:
For both the ADL and sports subscales, FAAM scores were greater in healthy participants (100 ± 0.0 and 99 ± 3.5, respectively) than in subjects with CAI (88 ± 7.7 and 76 ± 12.7, respectively; P < .001). Similarly, for both ADL and sports subscales, FAAM scores were greater in athletes who indicated that their ankles were normal (98 ± 6.3 and 96 ± 6.9, respectively) than in those who classified their ankles as either nearly normal or abnormal (87 ± 6.6 and 71 ± 11.1, respectively; P < .001). We found relationships between FAAM scores and self-reported global ratings of function for both ADL and sports subscales. Relationships were stronger when all athletes, rather than just those with CAI, were included in the analyses.
Conclusions:
The FAAM may be used to detect self-reported functional deficits related to CAI.
Keywords: outcomes, evaluative instrument, self-report, ankle sprains
Key Points.
Scores on the Foot and Ankle Ability Measure activities of daily living and sports subscales were greater in healthy athletes than in those with chronic ankle instability and were greater in the athletes who indicated that their ankles were normal than in those who indicated that their ankles were nearly normal or abnormal.
The Foot and Ankle Ability Measure may be used to detect self-reported functional deficits related to chronic ankle instability.
Scores on the sports subscale of the Foot and Ankle Ability Measure and on the sports global rating of function had a strong relationship.
Junge et al1 reported that lateral ankle sprains occur more frequently than any other musculoskeletal injury in sports. Once injured, athletes are more susceptible to recurrent injury associated with chronic ankle instability (CAI).2,3 In fact, recurrent lateral ankle sprains have been documented in up to 73% of cases.2 Following repeated injury, an athlete commonly experiences residual symptoms including ankle instability and activity limitations4 that may prompt him or her to seek rehabilitation. Subjective information from self-reported outcome instruments can provide valuable information for clinicians treating individuals with ankle instability.5,6 If self-reported outcome instruments are to be implemented appropriately, evidence must be available to support their use.7
Self-reported outcome instruments can be discriminative or evaluative.8 The selection of one type over the other depends on the desired use of the instrument. Discriminative instruments can be used to identify individuals with a particular disorder (eg, CAI).8 The Ankle Instability Instrument9 and Cumberland Ankle Instability Tool10 are examples of discriminative instruments. Evaluative instruments are designed to measure an individual's change in status over time, thereby assessing the effectiveness and outcome of treatment.8 The Foot and Ankle Disability Index (FADI)11 and Foot and Ankle Ability Measure (FAAM)12 are examples of evaluative instruments.
Information acquired from an evaluative instrument is useful only if evidence is available to support the interpretation of scores obtained in the specific population in which the instrument is intended to be used.7,13 This includes evidence for content validity, construct validity, reliability, and responsiveness. Reliability relates to score stability, and responsiveness describes the ability of the instrument to detect changes in an individual's status over time. Evidence of content validity is determined by the specific items on the instrument and what they measure. Evidence for construct validity includes how the scores on the instrument relate to other measures of the construct. Hypothesis testing is used to determine if the instrument performs as expected and is a method that is capable of providing evidence for construct validity.7,13 For example, one would expect individuals with more severe impairments to score lower than individuals with less severe impairments.
In a systematic review of the literature, Eechaute et al5 identified evaluative instruments for individuals with CAI and evidence to support their use. Four instruments met the criteria of this review: the Ankle Joint Functional Assessment Tool,14 the Foot and Ankle Outcome Score,15 the FADI,11 and the FAAM.12 The authors5 concluded that the FADI and FAAM were the most appropriate evaluative instruments to quantify functional disabilities in athletes with CAI. One advantage of the FADI and FAAM is that they both have a sports subscale in addition to an activities of daily living (ADL) subscale. The sports subscale may be particularly useful when addressing the limitations of athletes with CAI.
Hale and Hertel16 found that the FADI had evidence of content validity, construct validity, reliability, and responsiveness for individuals with CAI. Subsequently, the FADI underwent rigorous psychometric analysis, including analysis with item response theory. Four items related to pain and one related to sleeping were removed from the ADL subscale to improve psychometric properties of the instrument.12 The sports subscale remained unchanged. The resulting new instrument, the FAAM, has evidence of content validity, construct validity, reliability, and responsiveness for athletes with a broad range of musculoskeletal disorders of the leg, ankle, and foot.12 Descriptions of the FAAM, including its specific properties, have been provided in detail.5,7,12,13 Compared with competing instruments, the FAAM has undergone the most advanced psychometric testing, but further evidence supporting its use specifically in athletes with CAI would be beneficial.5
The purpose of our study was to offer evidence of construct validity for the FAAM based on hypothesis testing in athletes with CAI. We hypothesized that FAAM scores (1) would be different between a group of athletes with CAI and a group of healthy athletes, (2) would be able to distinguish between a self-reported normal and abnormal level of function, and (3) would be related to the global rating of function values.
Methods
Participants
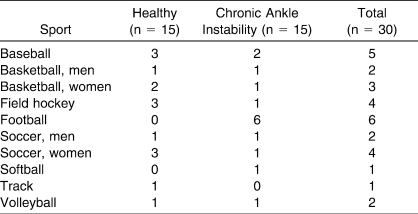
Participants were National Collegiate Athletic Association Division II athletes from one university. A single announcement about the study was made at each team's meeting, including a call for volunteers and inclusion criteria. A total of 53 athletes expressed interest in the study. Fifteen athletes with CAI (10 men, 5 women; age = 20.4 ± 1.4 years, height = 178.9 ± 10.7 cm, mass = 84.3 ± 17.9 kg) met the appropriate inclusion criteria based on information gathered from a screening questionnaire and a medical history. From the remaining 38 athletes, we selected the first 15 healthy volunteers (6 men, 9 women; age = 19.8 ± 1.0 years, height = 171.3 ± 10.3 cm, mass = 69.0 ± 15.2 kg) who met the appropriate criteria based on information gathered from the same screening questionnaire and medical history. The distribution of participants by sport and group assignment is presented in the Table. Before data collection began, all subjects read and signed a consent form. The study was approved by the university's Institutional Review Board.
Table.
Distribution of Athletes by Sport and Group Assignment
Procedures
Each potential participant completed the screening questionnaire and provided a medical history. The same investigator (J.M.D.) administered the screening questionnaires and obtained medical histories. At the time of the study, this investigator had 10 years of clinical athletic training experience and specialized in examination, evaluation, and rehabilitation of athletes with ankle instability.
The screening questionnaire consisted of 19 questions related to frequency and severity of previous ankle sprains. We included participants in the CAI group if they reported at least 2 lateral ankle sprains,3 episodes of “giving way,”17 residual symptoms (ie, pain, weakness, swelling, or instability) during functional activities,16 that the condition limited the ability to participate in sports activities, and that they would participate in treatment for their conditions. We excluded subjects from the CAI group if they reported ankle injury within the last 3 months, history of a lower extremity fracture on the same side as the affected ankle, concussion within the last 6 months, or current participation in a rehabilitation program for the affected ankle.
Participants were included in the healthy group if they did not have a history of ankle sprain, lower extremity fracture, or concussion within the last 6 months. Because athletes in this group had not sustained lateral ankle sprains, they were not specifically questioned about episodes of giving way, weakness, or swelling.
Following screening, each participant completed the self-reported outcome instrument, which included the FAAM, 2 global ratings of function, and 1 overall categorical rating of function.
Self-Reported Outcome Instrument
The FAAM comprises the separately scored 21-item ADL and 8-item sports subscales.18 Each item is scored on a 5-point Likert scale anchored by 4 (no difficulty at all) and 0 (unable to do). Item score totals, which range from 0 to 84 for the ADL subscale and from 0 to 32 for the sports subscale, are transformed to percentage scores.19 A higher score represents a higher level of function for each subscale.
To supplement FAAM scores, participants completed a global rating of function scale at the end of each FAAM subscale and an overall categorical rating of function at the end of the FAAM.18 On global rating scales, subjects rated the level of function with respect to ADL and sports on a 0% to 100% level. Zero percent indicates an inability to perform the listed ADL or sports tasks, whereas 100% reflects the level of function before injury. On the categorical rating scale, participants rated their ankles as normal, nearly normal, abnormal, or severely abnormal.
Statistical Analyses
We used separate, independent t tests to determine whether differences existed in FAAM subscale scores between healthy and CAI groups and between volunteers who indicated a normal versus an abnormal categorical rating of function overall. A Kendall tau rank correlation coefficient measured the relationship between FAAM scores and subjects' global rating scores for both the ADL and sports subscales. We analyzed our data with SPSS (version 11.0; SPSS Inc, Chicago, IL); the α level was set a priori at .05.
Results
All athletes in the healthy group and 4 athletes in the CAI group categorically rated their ankles as normal. Of the remaining athletes in the CAI group, 10 categorically rated their ankles as nearly normal, and 1 rated the ankle as abnormal. Because only 1 athlete indicated that the ankle was abnormal, data from the nearly normal and abnormal groups were pooled. We used the pooled data of these athletes (n = 11) when we compared them with those who rated their ankles as normal (n = 19).
Activities of Daily Living Subscale Results
For the ADL subscale, FAAM scores were different between healthy (100 ± 0.0) and CAI (88 ± 7.7) groups (t1,28 = 6.03, P < .001). The FAAM scores were greater in participants who indicated that their ankles were normal (98 ± 6.3) than in those who indicated that their ankles were nearly normal or abnormal (87 ± 6.6) (t1,28 = 4.37, P < .001).
Sports Subscale Results
Compared with CAI athletes (76 ± 12.7), healthy athletes scored higher (99 ± 3.5) on the sports subscale (t1,28 = 6.71, P < .001). The FAAM scores were greater in those who indicated that their ankles were normal (96 ± 6.9) than in those who indicated that their ankles were either nearly normal or abnormal (71 ± 11.1, t1,28 = 7.55, P < .001).
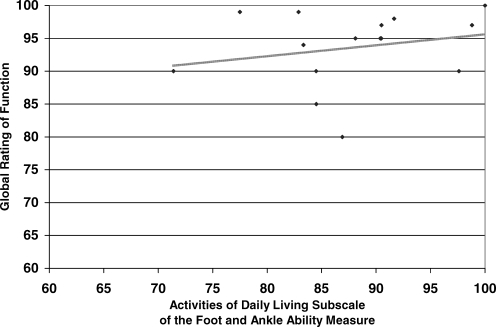
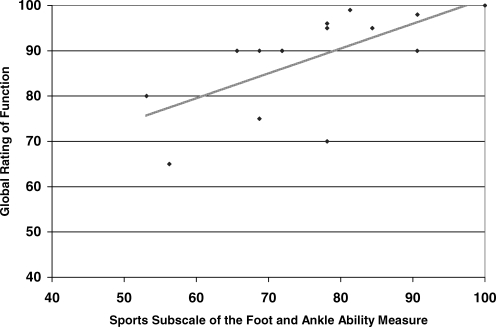
Relationship Between the Foot and Ankle Ability Measure and the Global Rating of Function
A moderate relationship (r = .64, P < .001) between scores on the ADL subscale and ADL global rating of function was evident when all athletes (n = 30) were included in the analysis. However, this relationship was weak (r = .23, P = .25) when only athletes from the CAI group were included in the analysis (Figure 1). A strong relationship (r = .79, P < .001) existed between scores on the sports subscale and sports global rating of function when all athletes were included in the analysis. This relationship was moderate (r = .57, P = .005) when only the CAI athletes were included in the analysis (Figure 2).
Figure 1. Scatterplot showing the relationship between scores on the activities of daily living subscale of the Foot and Ankle Ability Measure and the global rating of function for activities of daily living (n = 15). Data are from participants with chronic ankle instability only (2 athletes scored 100 on both measures).
Figure 2. Scatterplot showing the relationship between scores on the sports subscale of the Foot and Ankle Ability Measure (FAAM) and the global rating of function for sports (n = 15). Data are from participants with chronic ankle instability only (2 athletes scored 100 on both measures).
Discussion
Our study provides evidence of construct validity for the FAAM based on hypothesis testing in athletes with CAI. The ADL and sports subscale scores of the FAAM were greater in healthy athletes than in athletes with CAI and greater in athletes who classified their ankles as normal, than those who did not. Relationships were present between FAAM scores and self-reported global ratings of function for both ADL and sports subscales.
The primary finding of our study suggests that the FAAM is appropriate for use in collegiate athletes with CAI. Our findings are in agreement with those of Hale and Hertel,16 who reported that the FADI distinguished between healthy participants (n = 19) and those with CAI (n = 31) among 50 recreationally active individuals. Similarly, athletes with CAI in our study scored lower on both ADL and sports subscales compared with healthy athletes. Likewise, differences in mean scores between groups were greater on the sports subscale (23 points) than on the ADL subscale (12 points). These results imply that collegiate athletes with CAI have fewer limitations with ADLs than with sports activities and that the sports subscale can elucidate these limitations.
As anticipated, athletes who rated their ankles as normal scored higher than those who scored their ankles as anything less than normal. Similarly, we expected that athletes with CAI would rate their ankles as either abnormal or severely abnormal. However, in the CAI group, 4 athletes rated their ankles as normal; 10, as nearly normal; 1, as abnormal; and 0, as severely abnormal. This information suggests that these athletes were functioning at high levels. Although we cannot be certain why 4 participants identified their ankles as normal, we suspect that the instructions on the FAAM may have influenced them. Specifically, the instructions state: “Describe your level of function over the past week.” These athletes may not have participated in certain activities during the past week because of their ankle disorders. Post hoc analysis of the data from the 4 CAI athletes who rated their ankles as normal revealed that the FAAM scores were lower on both ADL (89 ± 11.3) and sports (87 ± 9.8) subscales in these 4 participants than in those whom we classified as healthy (ADL = 100 ± 0, sports = 98 ± 3.5, P = .001). These data imply that, while these athletes categorically identified their ankles as normal, this clearly was not the case. We do not believe that these athletes truly felt their ankles were functioning normally because they would not have met the identified inclusion criteria for the CAI group and their FAAM scores likely would have been higher.
Despite the high level of function of the athletes in the CAI group, the FAAM still was able to distinguish between healthy and CAI participants. Of course, caution must be exercised when drawing conclusions from a comparison of unequal and small sample sizes. Although we do not recommend solely using the self-reported categorical rating of function for classifying CAI and healthy athletes given its less-than-ideal specificity, it does appear to have some value (100% sensitive) for identifying those who have CAI. However, the clinician must remember that the primary function of the FAAM is to measure changes in status from one point to another rather than to classify subjects based on status.
Hale and Hertel16 demonstrated a relationship between scores on the ADL and sports subscales of the FADI for the involved extremities of participants with CAI (r = .64). They noted a stronger relationship when examining a combined group that comprised the uninvolved lower extremity of participants with CAI and the matched lower extremity of healthy participants (r = .84).16 To determine whether scores on the FAAM and a subject's self-reported global rating of function for both the ADL and sports subscales were measuring the same or different constructs, we examined the relationship between these 2 scales in the CAI group alone and in a combined group of healthy athletes and those with CAI. Regardless of whether the CAI group alone or the combined group was examined, relationships were stronger between the sports subscale scores and the respective global ratings of function than between the ADL subscale scores and the respective global ratings. This phenomenon may be explained in part by the characteristics of the population that we examined. Despite this, only 32% (CAI group) and 62% (combined group) of the variance in scores is explained between the sports subscale scores and the global ratings. These results suggest that although the measures are related, they appear to capture unique information. Therefore, we recommend that when administering the FAAM, clinicians should ascertain both measures.
A noteworthy finding was that for the relationships between each FAAM subscale score and global rating of function, correlation values were weaker when only the CAI group was examined. In fact, the relationship between the ADL subscale score and global rating of function was no longer significant when the healthy group was removed. Inspection of the raw data indicated that this relationship was influenced heavily by healthy athletes who scored 100% on the subscale and rated the level of function as 100%. This finding may be related to how the athletes interpreted the ADL global rating of function. The ADL global rating of function is meant to represent more basic functional daily activities, but athletes may view sports participation as a daily activity. Therefore, although they may score high on the ADL items of the FAAM, they may rate global function lower because of their limitation in sports.
Limitations
Although our study provides evidence of construct validity for use of the FAAM in athletes with CAI, its scope was limited. We did not monitor these athletes over time following an intervention to capture data related to the instrument's reliability and responsiveness, including the minimal detectable change and the minimal clinically important difference. However, given that the sports subscales of the FADI and FAAM are identical and that sensitivity has already been established in the FADI,16 one could argue that the FAAM also would be sensitive to changes in status for athletes with CAI. Although Hale and Hertel16 identified the FADI as sensitive to change in recreationally active participants with CAI, they did not provide specific data related to the minimal detectable change and the minimal clinically important difference. Conversely, data related to the minimal detectable change and the minimal clinically important difference have been identified for the FAAM; however, these data are specific to the population and timeframes for which they were established.12 Therefore, additional study related to these variables in athletes and using the FAAM is warranted.
Conclusions
Our results suggest that the FAAM may be used to detect self-reported functional deficits related to CAI. Further testing that offers evidence for validity, reliability, and responsiveness, including defining values for the minimal detectable change and the minimal clinically important difference, in this population is needed.
Acknowledgments
We thank Jenilee Lasure, ATC, for assisting with the data collection.
Footnotes
Christopher R. Carcia, PhD, PT, SCS, contributed to analysis and interpretation of the data and drafting, critical revision, and final approval of the article. RobRoy L. Martin, PhD, PT, CSCS, contributed to conception and design, analysis and interpretation of the data, and critical revision and final approval of the article. Joshua M. Drouin, PhD, ATC, contributed to acquisition and analysis and interpretation of the data and critical revision and final approval of the article.
References
- 1.Junge A, Langevoort G, Pipe A, et al. Injuries in team sport tournaments during the 2004 Olympic Games. Am J Sports Med. 2006;34((4)):565–576. doi: 10.1177/0363546505281807. [DOI] [PubMed] [Google Scholar]
- 2.Yeung M.S, Chan K.M, So C.H, Yuan W.Y. An epidemiological survey on ankle sprain. Br J Sports Med. 1994;28((2)):112–116. doi: 10.1136/bjsm.28.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Refshauge K.M, Kilbreath S.L, Raymond J. The effect of recurrent ankle inversion sprain and taping on proprioception at the ankle. Med Sci Sports Exerc. 2000;32((1)):10–15. doi: 10.1097/00005768-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Anandacoomarasamy A, Barnsley L. Long term outcomes of inversion ankle injuries. Br J Sports Med. 2005;39((3)):14. doi: 10.1136/bjsm.2004.011676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eechaute C, Vaes P, Van Aerschot L, Asman S, Duquet W. The clinimetric qualities of patient-assessed instruments for measuring chronic ankle instability: a systematic review. BMC Musculoskelet Disord. 2007;8:6. doi: 10.1186/1471-2474-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hintermann B. Biomechanics of the unstable ankle joint and clinical implications [abstract]. Med Sci Sports Exerc. 1999;31((suppl 7)):459S–469S. doi: 10.1097/00005768-199907001-00007. [DOI] [PubMed] [Google Scholar]
- 7.Martin R.L, Irrgang J.J. A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther. 2007;37((2)):72–84. doi: 10.2519/jospt.2007.2403. [DOI] [PubMed] [Google Scholar]
- 8.Kirshner B, Guyatt G. A methodological framework for assessing health indices. J Chronic Dis. 1985;38((1)):27–36. doi: 10.1016/0021-9681(85)90005-0. [DOI] [PubMed] [Google Scholar]
- 9.Docherty C.L, Gansneder B.M, Arnold B.L, Hurwitz S.R. Development and reliability of the Ankle Instability Instrument. J Athl Train. 2006;41((2)):154–158. [PMC free article] [PubMed] [Google Scholar]
- 10.Hiller C.E, Refshauge K.M, Bundy A.C, Herbert R.D, Kilbreath S.L. The Cumberland Ankle Instability Tool: a report of validity and reliability testing. Arch Phys Med Rehabil. 2006;87((9)):1235–1241. doi: 10.1016/j.apmr.2006.05.022. [DOI] [PubMed] [Google Scholar]
- 11.Martin R.L, Burdett R.G, Irrgang J.J. Development of the Foot and Ankle Disability Index (FADI) [abstract]. J Orthop Sports Phys Ther. 1999;29:32A–33A. [Google Scholar]
- 12.Martin R.L, Irrgang J.J, Burdett R.G, Conti S.F, Van Swearingen J.M. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26((11)):968–983. doi: 10.1177/107110070502601113. [DOI] [PubMed] [Google Scholar]
- 13.Martin R.L, Irrgang J.J, Lalonde K.A, Conti S. Current concepts review: foot and ankle outcome instruments. Foot Ankle Int. 2006;27((5)):383–390. doi: 10.1177/107110070602700514. [DOI] [PubMed] [Google Scholar]
- 14.Rozzi S.L, Lephart S.M, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther. 1999;29((8)):478–486. doi: 10.2519/jospt.1999.29.8.478. [DOI] [PubMed] [Google Scholar]
- 15.Roos E.M, Brandsson S, Karlsson J. Validation of the Foot and Ankle Outcome Score for ankle ligament reconstruction. Foot Ankle Int. 2001;22((10)):788–794. doi: 10.1177/107110070102201004. [DOI] [PubMed] [Google Scholar]
- 16.Hale S.A, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40((1)):35–40. [PMC free article] [PubMed] [Google Scholar]
- 17.Freeman M.A. Instability of the foot after injuries to the lateral ligament of the ankle. J Bone Joint Surg Br. 1965;47((4)):669–677. [PubMed] [Google Scholar]
- 18.Martin R. Foot and Ankle Ability Measure (FAAM). 2007. http://www.healthsciences.duq.edu/pdf/FAAM12-051.pdf. Accessed October 23,
- 19.Martin R. Scoring instructions for the FAAM. 2007. http://www.healthsciences.duq.edu/pdf/Scoringinstructions.pdf. Accessed October 23,