Abstract
Context: Various techniques have been described for assessing conditions that cause pain at the patellofemoral (PF) joint. The Clarke sign is one such test, but the diagnostic value of this test in assessing chondromalacia patella is unknown.
Objective: To (1) investigate the diagnostic value of the Clarke sign in assessing the presence of chondromalacia patella using arthroscopic examination of the PF joint as the “gold standard,” and (2) provide a historical perspective of the Clarke sign as a clinical diagnostic test.
Design: Validation study.
Setting: All patients of one of the investigators who had knee pain or injuries unrelated to the patellofemoral joint and were scheduled for arthroscopic surgery were recruited for this study.
Patients or Other Participants: A total of 106 otherwise healthy individuals with no history of patellofemoral pain or dysfunction volunteered.
Main Outcome Measure(s): The Clarke sign was performed on the surgical knee by a single investigator in the clinic before surgery. A positive test was indicated by the presence of pain sufficient to prevent the patient from maintaining a quadriceps muscle contraction against manual resistance for longer than 2 seconds. The preoperative result was compared with visual evidence of chondromalacia patella during arthroscopy.
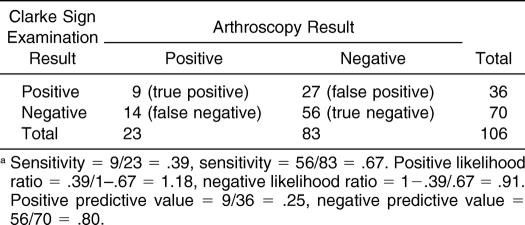
Results: Sensitivity was 0.39, specificity was 0.67, likelihood ratio for a positive test was 1.18, likelihood ratio for a negative test was 0.91, positive predictive value was 0.25, and negative predictive value was 0.80.
Conclusions: Diagnostic validity values for the use of the Clarke sign in assessing chondromalacia patella were unsatisfactory, supporting suggestions that it has poor diagnostic value as a clinical examination technique. Additionally, an extensive search of the available literature for the Clarke sign reveals multiple problems with the test, causing significant confusion for clinicians. Therefore, the use of the Clarke sign as a routine part of a knee examination is not beneficial, and its use should be discontinued.
Keywords: patellofemoral pain, knee evaluation, grind test, knee extensor mechanism
Key Points.
Anterior knee pain is common in both the general population and athletes.
The Clarke sign has often been used to assess chondromalacia patella and other patellofemoral syndromes, but its clinical diagnostic value is suspect.
Based on our results, we do not recommend use of the Clarke sign to diagnose any patellofemoral syndrome.
Anterior knee pain due to a variety of patellofemoral (PF) conditions is commonplace in the general population and especially among athletes. 1–7 Percy and Strother 8 and Malek and Mangine 9 claimed that the most common complaint pertaining to knee pain involves the PF joint, whereas Garrick 10 believed that anterior knee pain was the most common overuse syndrome affecting athletes. The PF articulation is quite complex and has been the focus of much debate and controversy during the last century. 2, 11–13 Given the multifactoral causes of PF pain and the lack of evidence-based examination and intervention techniques, PF pain challenges the clinician to thoroughly investigate all potential anatomical and biomechanical factors involved to assist the patient.
For most of the 20th century, the indiscriminate use of the term chondromalacia patella (CP) meant that most clinicians employed it when referring to any person who experienced anterior knee pain. 8, 10, 14 Casscells 15 claimed that CP was overdiagnosed and overtreated, especially in younger patients, and that fewer than 20% of athletes with retropatellar or peripatellar pain had actual CP. 15, 16 According to Fulkerson, 14 Budinger was the first to describe lesions to the articular cartilage of the patella in 1906, and Koenig was the first to use the term chondromalacia patella in 1924. Since then, authors have published more than 400 articles in the English literature attempting to decipher the causes and subsequent treatments of PF disorders, including CP. 9 Presently, the term is reserved for lesions of the articular cartilage that can be assigned arthroscopically to 1 of 4 stages. 17 Very often, athletes present with classical anterior knee pain syndromes and have normal-appearing articular cartilage. 12 In the recent literature, CP is described as a diagnostic entity all its own and is only one of many PF disorders or syndromes.
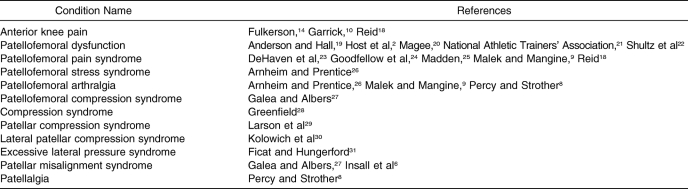
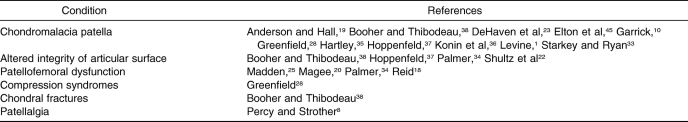
A myriad of terms has been used to describe the various maladies that present with pain at the PF joint ( Table 1). In an attempt to eradicate the confusion over terms and conditions, several investigators have attempted to organize the extensive literature into clinical classification systems to better assist the clinician in accurately assessing these overlapping conditions. 6, 11, 14, 17, 32 At best, all of this literature can be overwhelming for health care clinicians. Further complicating matters is the inconsistent information, including testing procedures and what constitutes a positive result, contained in various educational textbooks used by students. Unfortunately, athletic trainers are only left with noninvasive clinical techniques to assess anterior knee pain because arthroscopy is the most definitive diagnostic tool.
Table 1. Partial List of Terms Used to Describe Patellofemoral Joint Disorders.
One examination technique described for the PF joint is the Clarke sign (CS) or test. Most authors describe it as a stand-alone test, 4, 18–20, 28, 33, 34 but some authors use the term indiscriminately to describe pain or grinding (or both) with any PF test. 26, 35 As such, the available research on the diagnostic value of the CS is very limited and scarce. Accordingly, our purposes were to investigate the diagnostic value of the CS in assessing the presence of CP using arthroscopic examination of the PF joint as the “gold standard” and, secondly, to discuss the historical perspective of the CS.
METHODS
Participants
One hundred-six healthy individuals (37 women, 69 men; age, 27.1 ± 11.4 years) volunteered and signed a consent form to participate in this study. The consent form and study design were approved by the respective institutional review boards.
Preparticipation Screening
All potential participants were patients of the second investigator (R.L.R.) and presented to the office with knee symptoms from various causes. The participants had no subjective complaints of anterior knee discomfort and no objective clinical or radiographic findings of PF injury. However, they had other knee conditions requiring arthroscopic intervention.
Testing Procedures
The examination technique known as the CS is described as a clinical technique used for the assessment of CP. 19, 20, 28, 33, 35–38 All participants were positioned supine with both lower extremities supported on the examination table. The examiner (R.L.R. performed all testing to eliminate intertester variability) then placed the web space of his thumb and index finger against the superior pole of the participant's patella ( Figure 1). The examiner asked the participant to perform an isometric quadriceps contraction. A positive test was indicated by the presence of pain sufficient to prevent the patient from maintaining a quadriceps contraction against resistance longer than 2 seconds. A negative test meant the participant could contract the quadriceps and hold it for 2 seconds while pain free.
Figure 1. Correct examiner technique for the Clarke sign.

Data Reduction
Several statistical methods can be used to determine the diagnostic value of a clinical technique. To truly determine the diagnostic accuracy of a clinical examination technique such as the CS, it must be compared with the “gold standard”: in this case, visual evidence during arthroscopy. The first method to help clarify the ability of the CS to clinically diagnose CP is the calculation of specificity and sensitivity. Sensitivity is defined as the proportion of patients with a condition who have a positive test result and is calculated by taking the number of true positives (as determined by the gold standard) and dividing it by the sum of the true positives and false negatives. 39 Conversely, specificity is defined as the proportion of patients without a condition who have a negative test result and is calculated by taking the number of true negatives (as determined by the gold standard) and dividing it by the sum of the true negatives and false positives. 39 In other words, 100% sensitivity means that when the test is positive, the correlative condition is always present; 100% specificity means that when the test is negative, the condition is never present, and in an ideal world, the test in question never provides a false impression. Obviously, clinical examination tools that are 100% accurate all of the time do not exist.
Another method to determine the diagnostic values of a clinical test is to use positive and negative predictive values. 40 The positive predictive value is the percentage of patients with a positive test who have the condition, in this case CP. Similarly, the negative predictive value is the percentage of patients with a negative test who do not have the condition.
The best statistical method for determining the diagnostic accuracy of a clinical test is likelihood ratios. 39 Likelihood ratios (LRs) are used to estimate to what extent a clinical examination technique measures what it is supposed to measure by comparing the clinical test with the results of the gold standard findings. A positive LR is calculated by dividing the sensitivity (the rate of true positives) by the rate of false positives, whereas a negative LR is calculated by dividing the rate of false negatives by the specificity (rate of true negatives). 39 After calculating these ratios, a table is used to identify any shift in probability that the condition is present or absent. 41 In other words, higher LRs (eg, >10) indicate that clinical examination techniques are beneficial in ruling in the condition; lower LRs (eg, <0.1) are beneficial in ruling out the condition, and LRs near 1.0 provide no useful information as to the presence or absence of the condition. 39, 41
RESULTS
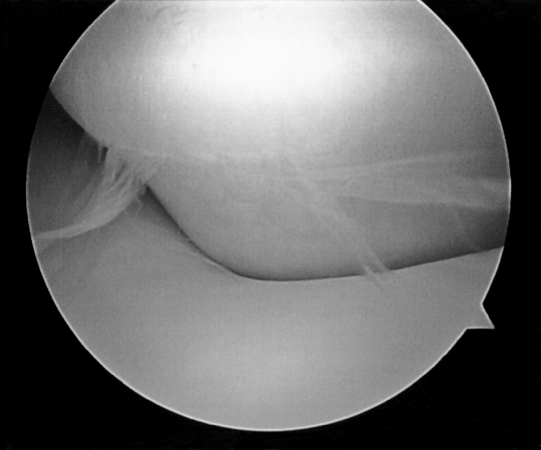
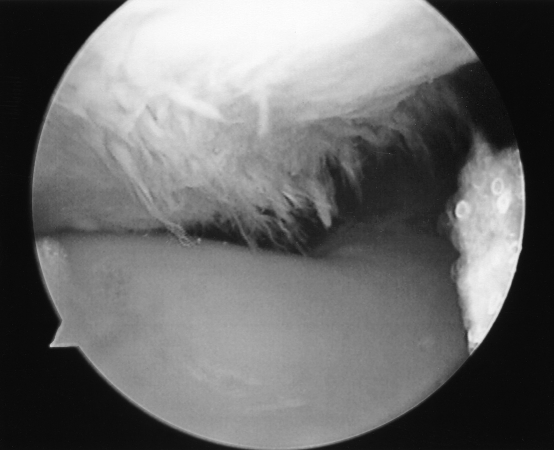
During arthroscopy, all patients had a thorough and systematic evaluation of the PF articulation by both visual inspection and probing ( Figure 2). The presence of CP as defined by the Outerbridge and Dunlop 17 classification system was noted ( Figure 3) and recorded. The arthroscopic findings were then compared with the recorded preoperative clinical examination findings in order to determine the diagnostic values of the CS ( Table 2).
Figure 2. Arthroscopic image of a normal patella.
Figure 3. Arthroscopic image of grade III chondromalacia patella. The participant had a negative Clarke sign on examination.
Table 2. Clarke Sign Diagnostic Valuesa.
Of 106 patients, 36 had a positive CS on clinical examination, and 70 had a negative CS. Of those patients with a positive preoperative CS examination, 27 had no arthroscopic evidence of CP, whereas the other 9 showed evidence of CP. With 27 false positive and 9 true positive CS findings, CS had only 25.0% positive predictive value. Simply stated, only 9 of the 36 patients with a positive CS test actually had the predicted finding at surgery. During surgery, 23 patients were noted to have objective evidence of CP, but of this group, only 9 had a positive CS preoperatively. Thus, 14 examinations were false negatives, indicating that the sensitivity of CS was only 39.1%, because only 9 of the 23 patients with evident CP had demonstrated the positive examination finding that was supposed to predict the condition. When CS was negative, 56 of 70 patients tested indeed had no evidence of CP, indicating a negative predictive value of 80.0%. Consequently, the specificity of CS was 67.5%, because 56 of the 83 patients who had no objective evidence of CP during surgery had a negative preoperative CS. Based on the sensitivity and specificity of the CS, the positive LR was 1.2 and the negative LR was 0.9.
DISCUSSION
Our first purpose was to ascertain the diagnostic value of the CS in assessing CP in patients undergoing arthroscopic surgery for reasons unrelated to the PF joint. Ideally, clinical tests available to a clinician are those that have both a high degree of sensitivity and specificity. An example is the Lachman test, which is 86% sensitive and 91% specific and is widely accepted as the most valid clinical test available to determine the integrity of the anterior cruciate ligament (ACL). 42 Our results show that the CS was 39.1% sensitive and 67.5% specific, values that fall well short of the threshold for adequate diagnostic utility. They are, in fact, virtually identical to the 39% sensitivity and 67% specificity noted by Guanche and Jones 43 when assessing the predictive value of the crank test for superior glenoid labral injury, which the authors concluded had “no significant diagnostic value whatsoever.”
The CS also failed to show a strong tendency in diagnostic predictive values. Although the negative predictive value of the CS was a somewhat reasonable 80.0%, the positive predictive value was only 25.0%. Thus, according to our data, a clinician relying on the CS for the correct diagnosis of CP would be wrong 38.7% (41/106) of the time. We would expect better predictive values for a clinical test that is so often mentioned in the literature and used by clinicians.
The most valuable tests available to the clinician are those that have high positive LRs and low negative LRs. 39 In our study, the positive LR for a positive CS was 1.2. That is, patients who truly had CP were 1.2 times as likely to have a positive CS as those who did not have CP. Such a small positive LR indicates an inconclusive and insignificant test. 44 In contrast, the Lachman test has a positive LR of 9.6, 42 indicating a large, often conclusive shift in probability that the ACL is ruptured. 44 Moreover, the LR for a negative CS was 0.9, indicating that patients who actually had CP had a negative CS examination 90.0% as often as those who did not have CP. Stated another way, patients who did not have CP were only 1.1 times as likely to have a negative CS as those who did have CP. Once more, the small shift in probability of obtaining a negative CS in patients who did have CP compared with those who did not indicates a very inconclusive and insignificant examination. 44 Using the Lachman test again for comparison, the negative LR is 0.15, 42 indicating a very large shift in probability that the ACL is not ruptured. 44 Based on all of these statistical findings, the CS has very little, if any, diagnostic value in detecting CP.
Our literature search produced only 1 group 45 that specifically addressed the efficacy of the CS in diagnosing CP. Recognizing that the validity and reliability for many clinical tests for CP had not been established, Elton et al 45 investigated several factors commonly employed by clinicians to assess CP, including PF joint pain history, Q-angle, resisted knee flexion-extension strength, full squat, crepitus, and patellar grind test (another name for the CS). They compared the preoperative clinical test results with arthroscopic evidence of CP in only 20 participants (versus our 106 participants). Their goal was to determine which techniques or factors showed a high correlation in diagnosing CP clinically. Of their participants with arthroscopically confirmed CP, 40.5% had a positive CS. A total of 5% of the matched control participants had a false positive CS, but there was no gold standard evidence of CP, as these participants did not undergo arthroscopy to confirm the absence of CP. Our poor diagnostic values for CS are consistent with those found by Elton et al. 45
Our second purpose was to present a detailed historical perspective of the CS and how this may have contributed to the confusion surrounding this clinical test. In fact, there is no record in the literature regarding the original description or genesis of the CS, which lends itself to misinterpretations over time. As a result, many problems are inherent to the CS, including discrepancies as to the conditions and syndromes tested and the definition of a positive test, intertester reliability, multiple techniques, and varied terminology for the CS and similar tests.
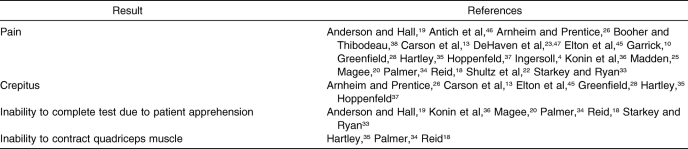
First and foremost, the literature provides conflicting information regarding which syndromes or conditions the CS actually assesses and what constitutes a positive test result. Chondromalacia patella is the most common diagnosis mentioned in the literature that results in a positive CS, although several other conditions are also described as resulting in a positive CS ( Table 3). Thus, the confusion is compounded, because a single clinical diagnostic technique is reported to assess 6 different conditions, including CP. However, it could be argued that these conditions and syndromes are not all unique entities and that patients with PF pain may be simultaneously classified as having more than 1 condition. Therefore, the conditions resulting in a positive test vary, thus affecting the diagnostic utility of the test. Additionally, many authors disagree as to what constitutes a positive test ( Table 4). For example, Percy and Strother 8 and Abernethy et al 16 believed that crepitus alone was not a clear diagnostic sign of CP, whereas Fulkerson 14 stated that pain with compression of the patella in full knee extension was not clear evidence of articular pain. The literature is riddled with these kinds of issues regarding what is considered a positive test and what a positive test means clinically.
Table 3. Clinical Patellofemoral Joint Syndromes Diagnosed With a Positive Clarke Sign.
Table 4. Four Possible Positive Results for the Clarke Sign.
Another reason that CS is highly suspect is the inconsistent technique practiced by examiners. We deliberately used a single examiner with 24 years of experience to eliminate the possibility of intertester differences. Many authors agree that if CS is performed with too much manual pressure, it can be painful and result in a false positive in almost everyone, even those without existing anterior knee injury. 1, 4, 10, 19, 20, 22, 32, 34–36, 38 Many of these same authors also mentioned that if CS must be included in the knee examination, it should be the last test performed in order to avoid unnecessary pain and apprehension in the patient. Although Garrick 10 did not use a name for the CS, he claimed that performing this maneuver is unnecessarily painful and has little diagnostic value during the physical examination for anterior knee pain. Accordingly, 2 theories have been described to explain why CS can be so painful in healthy knees, especially in the absence of CP. Several authors 6, 9, 13, 35, 48 believed the synovium was pinched between the patella and trochlea, whereas Levine 1 described the pinching of the supratrochlear fat pad; both types of pinching cause pain and are interpreted as a positive test for CP. Anecdotally, a number of authors 1, 10, 20, 28, 33, 35, 45, 49 referred to a high rate of false positives with the CS and warned against its indiscriminate use. Our results substantiate these anecdotal reports.
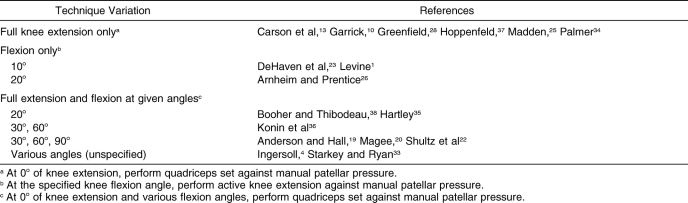
Technique variations constitute yet another problem with the CS, which can be performed both during full knee extension and at various angles of flexion ( Table 5). For our study, we chose to perform only the most common technique described in the literature as full knee extension and did not attempt any of the flexion techniques. In exploring the flexion variations, several authors 1, 23, 26 performed the CS at 10° to 20° of flexion and had the patient actively extend the knee while the examiner attempted to resist superior movement of the patella. With this variation, DeHaven et al 47 found pain in 70% of patients thought to have CP when the dynamic patellar compression test (same as the CS) was performed at 10° of flexion. However, the authors' diagnosis of CP in their participants was made clinically without the aid of arthroscopic evidence. At the time of their study, it was quite common to use the term chondromalacia patellae as a catch-all diagnosis for anterior knee pain. This raises some serious concerns regarding the interpretation of the data they reported.
Table 5. Clarke Sign Technique Variations.
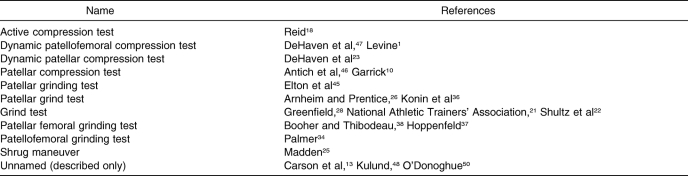
The last significant issue compounding the use and interpretation of CS is the number of similar tests in the literature described under different names ( Table 6). Many of these other tests have only subtle differences, if any, from the CS. For example, the National Athletic Trainers' Association's Athletic Training Educational Competencies 21 listed the “grind test.” This test name is problematic because it describes 2 different PF tests in educational textbooks: the CS test, 22, 28 and a different test 51 that we will refer to, for the sake of discussion, as the “passive” patellofemoral compression test. This test is similar to the CS but is often mistaken for the CS. This passive patellofemoral compression technique involves posteriorly directed pressure on the patella and passive manipulation of the patella in all directions; provoked pain is the only positive result. Common names for this test very similar to if not the same as some of the synonyms for the CS include patellofemoral compression, 35 patellofemoral grind, 51 patellar compression, 26 passive patellar compression, 18 articular compression, 14 and unnamed descriptions only. 4, 6–9, 24 This passive PF compression test differs from the CS in that there is no superior buttress to the patella and no active quadriceps contraction. Basically, the patella is passively manipulated after posteriorly directed pressure in an attempt to stress the articular surfaces of both the patella and the femoral trochlear groove. Perhaps Reid 18 recognized and captured the essence of some of the confusion by calling the CS “active patellar compression” due to the contraction of the quadriceps, as compared with a passive patellar compression test. However, it must be noted that no reports in the literature show the diagnostic values for the passive patellar compression test.
Table 6. Other Names for the Clarke Sign.
CONCLUSIONS AND RECOMMENDATIONS
Patellofemoral pain is a clinical entity that is very difficult to understand and treat. Reliable and valid evaluation techniques are lacking. Perhaps DeHaven et al 23 stated it best when they referred to the patella and PF joint as the “great masquerader.” The CS has frequently been used by clinicians to assess CP and other PF syndromes, but its clinical diagnostic value is highly suspect. We do not recommend using the CS as a diagnostic test for any PF syndrome due to the lack of clarity in the literature regarding its actual mechanics of application, confusion regarding what constitutes a positive test, and its poor diagnostic accuracy. Continued evidence-based research is needed to identify and confirm those clinical signs and tests that objectively predict extensor mechanism abnormalities.
Footnotes
Scott T. Doberstein, MS, LAT, ATC, CSCS, contributed to conception and design; analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Richard L. Romeyn, MD, and David M. Reineke, PhD, contributed to acquisition and analysis and interpretation of the data and critical revision and final approval of the article.
REFERENCES
- Levine J. Chondromalacia patellae. Physician Sportsmed. 1979;7(8):40–43. doi: 10.1080/00913847.1979.11948468. [DOI] [PubMed] [Google Scholar]
- Host JV, Craig R, Lehman RC. Patellofemoral dysfunction in tennis players: a dynamic problem. Clin Sports Med. 1995;14(1):177–203. [PubMed] [Google Scholar]
- Fulkerson JP. The etiology of patellofemoral pain in young, active patients: a prospective study. Clin Orthop Relat Res. 1983;179:129–133. [PubMed] [Google Scholar]
- Ingersoll CD. Assessment of patellar pain. Athl Ther Today. 1998;3(2):45–50. [Google Scholar]
- Nissen CW, Cullen MC, Hewett TE, Noyes FR. Physical and arthroscopic examination techniques of the patellofemoral joint. J Orthop Sports Phys Ther. 1998;28(5):277–285. doi: 10.2519/jospt.1998.28.5.277. [DOI] [PubMed] [Google Scholar]
- Insall J, Falvo KA, Wise DW. Chondromalacia patellae: a prospective study. J Bone Joint Surg Am. 1976;58(1):1–8. [PubMed] [Google Scholar]
- Reider B, Marshall JL, Warren RF. Clinical characteristics of patellar disorders in young adults. Am J Sports Med. 1981;9(4):270–274. doi: 10.1177/036354658100900419. [DOI] [PubMed] [Google Scholar]
- Percy EC, Strother RT. Patellalgia. Physician Sportsmed. 1985;13(7) doi: 10.1080/00913847.1985.11708831. 43– 46,49–51,55,56,58,59. [DOI] [PubMed] [Google Scholar]
- Malek MM, Mangine RE. Patellofemoral pain syndromes: a comprehensive and conservative approach. J Orthop Sports Phys Ther. 1981;2(3):108–116. doi: 10.2519/jospt.1981.2.3.108. [DOI] [PubMed] [Google Scholar]
- Garrick JB. Anterior knee pain (chondromalacia patellae) Physician Sportsmed. 1989;17(1):75–76. doi: 10.1080/00913847.1989.11709683. 81–84. [DOI] [PubMed] [Google Scholar]
- Holmes SW, Jr, Clancy WG., Jr. Clinical classification of patellofemoral pain and dysfunction. J Orthop Sports Phys Ther. 1998;28(5):299–306. doi: 10.2519/jospt.1998.28.5.299. [DOI] [PubMed] [Google Scholar]
- Kelly MA, Insall JN. Historical perspectives of chondromalacia patellae. Orthop Clin North Am. 1992;23(4):517–521. [PubMed] [Google Scholar]
- Carson WG, Jr, Stanley JL, Larson RL, Singer KM, Winternitz WW. Patellofemoral disorders: physical and radiographic evaluation. Part I: physical examination. Clin Orthop Relat Res. 1984;185:165–177. [PubMed] [Google Scholar]
- Fulkerson JP. Disorders of the Patellofemoral Joint. 3rd ed. Baltimore, MD: Williams & Wilkins; 1997.
- Casscells W. Chondromalacia of the patella. J Pediatr Orthop. 1982;2(5):560–564. doi: 10.1097/01241398-198212000-00017. [DOI] [PubMed] [Google Scholar]
- Abernethy PJ, Townsend PR, Rose RM, Radin EL. Is chondromalcia patellae a separate clinical entity? J Bone Joint Surg Br. 1978;60(2):205–210. doi: 10.1302/0301-620X.60B2.659466. [DOI] [PubMed] [Google Scholar]
- Outerbridge RE, Dunlop JA. The problem of chondromalacia patellae. Clin Orthop Relat Res. 1975;110:177–196. doi: 10.1097/00003086-197507000-00024. [DOI] [PubMed] [Google Scholar]
- Reid DC. Sports Injury Assessment and Rehabilitation. London, United Kingdom: Churchill Livingston; 1992:369–370.
- Anderson MK, Hall SJ. Sports Injury Management. 2nd ed. Media, PA: Williams & Wilkins; 2000:476–477.
- Magee DJ. Orthopedic Physical Assessment. 3rd ed. Philadelphia, PA: WB Saunders; 1997:566.
- National Athletic Trainers' Association. Athletic Training Educational Competencies. 3rd ed. Dallas, TX:1999:22.
- Shultz SJ, Houglum PA, Perrin DH. Assessment of Athletic Injuries. Champaign, IL: Human Kinetics; 2000:302.
- DeHaven KE, Dolan WA, Mayer PJ. Chondromalacia patellae and the painful knee. Am Fam Physician. 1980;21(1):117–124. [PubMed] [Google Scholar]
- Goodfellow J, Hungerford DS, Woods C. Patello-femoral joint mechanics and pathology, I: functional anatomy of the patello-femoral joint. J Bone Joint Surg Br. 1976;58(3):287–290. doi: 10.1302/0301-620X.58B3.956243. [DOI] [PubMed] [Google Scholar]
- Madden C. Pearls: screening strategies for patellofemoral pain. Physician Sportsmed. 2000;28(11):16. [Google Scholar]
- Arnheim DD, Prentice WE. Principles of Athletic Training. 10th ed. Boston, MA: McGraw-Hill Higher Education; 2000:535–536.
- Galea AM, Albers JM. Patellofemoral pain: beyond empirical diagnosis. Physician Sportsmed. 1994;22(4):48,49,53,54,56,58. doi: 10.1080/00913847.1994.11947624. [DOI] [PubMed] [Google Scholar]
- Greenfield BH. Rehabilitation of the Knee: A Problem-Solving Approach. Philadelphia, PA: FA Davis; 1993:184.
- Larson RL, Cabaud HE, Slocum DB, James SL, Keenan T, Hutchinson T. The patellar compression syndrome: surgical treatment by lateral retinacular release. Clin Orthop Relat Res. 1978;134:158–167. [PubMed] [Google Scholar]
- Kolowich PA, Paulos LE, Rosenberg TD, Farnsworth S. Lateral release of the patella: indications and contraindications. Am J Sports Med. 1990;18(4):359–365. doi: 10.1177/036354659001800405. [DOI] [PubMed] [Google Scholar]
- Ficat RP, Hungerford DS. Disorders of the Patellofemoral Joint. Baltimore, MD: Williams & Wilkins; 1977:85–148.
- Merchant AC. Classification of patellofemoral disorders. Arthroscopy. 1988;4(4):235–240. doi: 10.1016/s0749-8063(88)80037-9. [DOI] [PubMed] [Google Scholar]
- Starkey C, Ryan JL. Evaluation of Orthopedic and Athletic Injuries. Philadelphia, PA: FA Davis; 1996:179–181.
- Palmer ML. Fundamentals of Muscoloskeletal Assessment Techniques. 2nd ed. Philadelphia, PA: Lippincott-Raven; 1998:318–319.
- Hartley A. Practical Joint Assessment Lower Quadrant. 2nd ed. St. Louis, MO: Mosby-Year Book; 1995:218–219.
- Konin JG, Wiksten DL, Isear JA. Special Tests for Orthopedic Examination. Thorofare, NJ: Slack; 1997:208–210.
- Hoppenfeld S. Physical Examination of the Spine and Extremities. New York, NY: Appleton-Century-Crofts; 1976:194.
- Booher JM, Thibodeau GA. Athletic Injury Assessment. 2nd ed. St. Louis, MO: McGraw-Hill Higher Education; 1989:457,459.
- Denegar CR, Fraser M. How useful are physical examination procedures? Understanding and applying likelihood ratios. J Athl Train. 2006;41(2):201–206. [PMC free article] [PubMed] [Google Scholar]
- Dawson-Sanders B, Trapp RG. Basic & Clinical Biostatistics. 2nd ed. Norwalk, CT: Appleton & Lange; 1994:234–244.
- Jaeschke R, Guyatt GH, Sackett DL. User's guides to the medical literature, III: How to use an article about a diagnostic test. B, What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA. 1994;271(9):703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- Scholten RJMP, Opstelten W, van der Plas CG, Bijl D, Deville WLJM, Bouter LM. Accuracy of physical diagnostic tests for assessing ruptures of the anterior cruciate ligament: a meta-analysis. J Fam Pract. 2003;52(9):689–694. [PubMed] [Google Scholar]
- Guanche CA, Jones DC. Clinical testing for tears of the glenoid labrum. Arthroscopy. 2003;19(5):517–523. doi: 10.1053/jars.2003.50104. [DOI] [PubMed] [Google Scholar]
- Fritz JM, Wainner RS. Examining diagnostic tests: an evidence-based perspective. Phys Ther. 2001;81(9):1546–1564. doi: 10.1093/ptj/81.9.1546. [DOI] [PubMed] [Google Scholar]
- Elton K, McDonough K, Savinar E, Jensen G. A preliminary investigation: history, physical, and isokinetic exam results versus arthroscopic diagnosis of chondromalacia patella. J Orthop Sports Phys Ther. 1985;7(11):115–123. doi: 10.2519/jospt.1985.7.3.115. [DOI] [PubMed] [Google Scholar]
- Antich TJ, Randall CC, Westbrook FA, Morissey MC, Brewster CE. Evaluation of knee extensor mechanism disorders: clinical presentation of 112 patients. J Orthop Sports Phys Ther. 1986;8:248–254. doi: 10.2519/jospt.1986.8.5.248. [DOI] [PubMed] [Google Scholar]
- DeHaven KE, Dolan WA, Mayer PJ. Chondromalacia patellae in athletes. Clinical presentation and conservative management. Am J Sports Med. 1979;7(1):5–11. doi: 10.1177/036354657900700102. [DOI] [PubMed] [Google Scholar]
- Kulund DN. The Injured Athlete. 2nd ed. Philadelphia, PA: JB Lippincott; 1988:456.
- Kulund DN. The Injured Athlete. Philadelphia, PA: JB Lippincott; 1982: 379.
- O'Donoghue DH. Treatment of Injuries in Athletes. 3rd ed. Philadelphia, PA: WB Saunders; 1976:672.
- Booher JM, Thibodeau GA. Athletic Injury Assessment. 4th ed. Boston, MA: McGraw-Hill Higher Education; 2000:343–344.