Abstract
Context:
The valgus stress test is used clinically to assess injury to the medial knee structures in 2 positions: full extension and some degree of flexion. The amount of flexion used to “isolate” the medial collateral ligament is not consistent in the literature, but most studies have shown that stiffness of the ligaments was consistent between the limbs.
Objective:
To determine (1) if the stiffness of the medial knee structures was the same bilaterally, and (2) if the stiffness was different in full extension compared with 20° of knee flexion.
Design:
Criterion standard, before-after design.
Setting:
University research laboratory.
Patients or Other Participants:
Both knees of 45 healthy and active volunteers (26 females, 19 males; age = 23.2 ± 3.96 years, height = 170.6 ± 7.75 cm, mass = 74.2 ± 15.14 kg) were studied.
Intervention(s):
A valgus force of 60 N was applied to the lateral aspect of both knees in full extension and in 20° of flexion.
Main Outcome Measure(s):
The slope of the force-strain line of the medial knee during a valgus force was calculated using the LigMaster arthrometer.
Results:
Slope means in full extension were 16.1 ± 3.3 (right knee) and 15.8 ± 3.1(left knee). Means for 20° of flexion were 12.2 ± 3.1 (right) and 11.7 ± 2.8 (left). Stiffness was greater when the knee was in full extension versus 20° of flexion (t44 = 12.04, P < .001). No difference was noted between the slopes of the 2 knees in extension (t44 = 0.74, P = .46) or in flexion (t44 = 1.2, P = .27).
Conclusions:
These findings support the use of the contralateral knee as a control. Further, the valgus stress test should be performed in full extension and in some degree of flexion to assess the different restraining structures of the medial tibiofemoral joint.
Keywords: arthrometry, leg dominance, valgus stress
Key Points.
In healthy participants, the static stabilizers of the knee (particularly the medial collateral ligament) had the same stiffness bilaterally, thus supporting the use of the uninjured knee as a control in injury assessment.
Resistance to valgus force was greater when the knee was in extension than in 20° of flexion. Thus, testing the medial knee in both extension and some degree of flexion is useful to differentiate medial tibiofemoral joint structures.
Future researchers should determine the ideal amount of knee flexion needed to isolate the medial collateral ligament.
Athletic trainers, physical therapists, and physicians diagnose a medial collateral ligament (MCL) injury by identifying a history of medial knee pain and a mechanism of injury in which a valgus force was applied to the lateral aspect of the tibiofemoral joint. Clinically, injury severity is based on point tenderness, swelling over the ligament, and the amount of opening of the medial knee joint line during manual abduction, a valgus stress test (VST).1,2 Movement of the joint (instability of the tibiofemoral joint) during a valgus stress is compared with that of the unaffected knee, and pain and motion are compared bilaterally. The interpretation of the amount of displacement between the tibia and femur is a subjective evaluation of the integrity of the MCL by the clinician. Ligament stiffness and, thus, displacement with force of healthy right and left legs are assumed to have been the same before injury, and leg dominance is of little consequence when comparing the extremities bilaterally. However, evidence that the ligaments in both knees have equal stiffness is inconclusive.3–5
When performing the VST on the tibiofemoral joint, structures tested in full extension are different from those tested in flexion.6–9 Yet investigators6,8,9 of the structural properties of the medial knee joint disagree on the positioning of the knee to best assess the contribution of the MCL when valgus stress is applied. Most agree that testing should be performed in both full extension and in flexion, although the amount of flexion is not consistent. In a cadaver study, Grood et al6 determined that the knee only needs to be flexed 5° to distinguish between the MCL and posterior structures and that the optimal amount of flexion to isolate the MCL is 25°. Robinson et al8 also reported the latter finding, whereas Hughston et al9 considered 30° of flexion the standard amount of knee flexion necessary to assess the MCL during the VST. Textbooks7,10,11 used in teaching the VST suggest a range of 20° to 30° of knee flexion. Although textbook recommendations may lead to common practice clinically, no definitive evidence suggests that one position is most appropriate to characterize MCL integrity during the VST. Our purposes, therefore, were to determine (1) if the slope of the force-strain line, or the calculated stiffness of the medial tibiofemoral joint, was the same in the dominant and nondominant legs, and (2) if the difference in stiffness of the medial knee in 2 clinically common positions used for the VST (full extension and 20° of flexion) was significant, as cadaver studies6,8,9 have shown, and to quantify this difference with an in vivo measurement.
Methods
We used a criterion standard, before-after design for this study. The variables were side (right or left) and knee position (0° or 20° of flexion). The main outcome measure was the slope of the force-strain line measured from 0 to 60 N.
Participants
Forty-five healthy and physically active volunteers (26 females, 19 males; age = 23.2 ± 3.96 years, height = 170.6 ± 7.75 cm, mass = 74.2 ± 15.14 kg) with no history of knee surgery or of knee injury in the past 6 months were studied. The Institutional Review Board for the Social and Behavioral Sciences at the University of Virginia approved this study protocol, and written informed consent was obtained from each volunteer before testing.
Instrumentation
Medial knee stiffness was calculated using the LigMaster instrumented arthrometer (Sport Tech Inc, Charlottesville, VA). The LigMaster is a modified Telos stress device that has been fitted with a custom electronic sensor package. A pressure actuator is set at the joint line and a linear decoder detects displacement (in millimeters) of the bones of the joint when force is added. In our study, a 100-N to 120-N force was added to the tibiofemoral joint on the lateral femoral epicondyle to produce a valgus stress and, thus, displace the tibia and femur at the medial joint line. Medial knee stiffness was calculated and represented by the slope of the force-strain line generated by the software (version 1.36a) embedded in the arthrometer. Data analysis was performed on the resulting slope value at 60 N of force after pilot work determined that this value was where linearity of the force-strain line was best maintained.
Repeatability for this device has been estimated to be within 10% accuracy for inexperienced users and within 2% to 5% accuracy with practice.12 Aronson13 found the intratester reliability of the experienced examiner (P.A.A.) when measuring the medial knee with the arthrometer to be strong (for 11 subjects, intraclass correlation coefficients of .79 and .80 in extension and 20° flexion and standard errors of measurement of 1.5 and 0.69 for slope values, respectively).
A standard goniometer (model G 800; Whitehall Manufacturer, City of Industry, CA) was used to accurately measure 20° of knee flexion and 0° (full extension) in subjects who displayed recurvatum of the tibiofemoral joint.
Procedures
For consistency of procedures and measurements, one author (P.A.A.) performed all measurements on each volunteer in a single session. The leg to be tested first was chosen by the flip of a coin. The dominant knee was determined by asking the participant which leg was preferred to kick a ball a long distance and then having him or her draw a diamond on the floor with 1 leg to confirm the dominant side.
The side arms of the arthrometer were placed in the extreme positions, 440 mm apart. The pressure plate was positioned equidistant between the side arms and the joint line on the lateral aspect of the tibiofemoral joint and secured in place.
The participant lay supine with the test leg fully extended into the arthrometer and placed squarely onto a stationary foot plate (Figure 1A). Each subject's shoeless foot was secured at the bottom of the foot plate with 2 hook-and-loop straps that held the foot stationary during testing and eliminated rotation of the leg during a valgus force; thus, joint motion was limited to 1 df. The goniometer was used to measure the knees of those volunteers who displayed tibiofemoral joint hyperextension to make certain that all knees were tested in 0° of flexion.
Figure 1. Participant and leg positioning in the arthrometer for testing. A, The medial left knee in full extension. B, The medial left knee in 20° of flexion.
The contralateral leg was comfortably placed to the side of the device. The pressure plate was positioned with the face of the rubber padding at the level of the lateral joint space of the tibiofemoral joint and was moved to the point of just touching the skin. The magnitude of the force applied was increased from 0 N to 120 N at a rate of 0.1 N per 1 to 2 seconds for each measurement.
The participant was encouraged to relax in the supine position, and a trial was performed to promote relaxation of the tested leg musculature. Two measurements were then taken and recorded for data analysis. Next, the participant was asked to recline and relax in a long sitting position with both forearms behind the hips to support body weight. A 4-in (10.16-cm) foam roller was placed under the upper leg, and a goniometer was used to position the knee being tested in 20° of flexion (Figure 1B). The angle was remeasured after each test. In pretrials at 20° of flexion, while the femur and tibia displaced at the medial knee (ie, opened with valgus stress), the thigh tended to rotate with valgus forces greater than 120 N. To control for this tendency, we limited the maximum force applied to 120 N. The same procedure was then used to measure the contralateral leg.
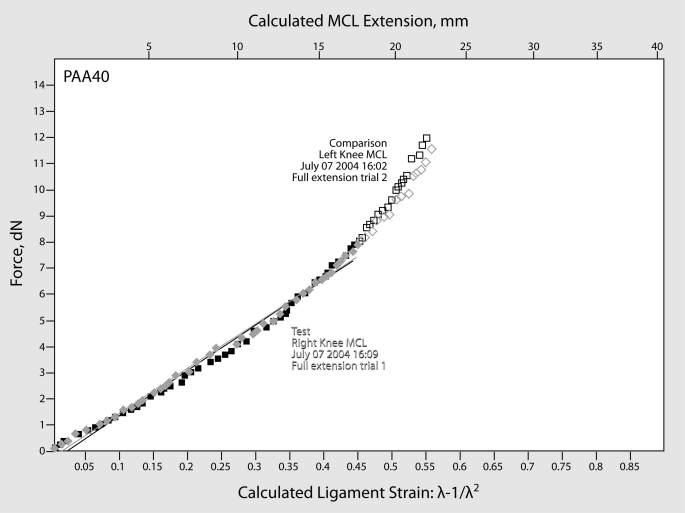
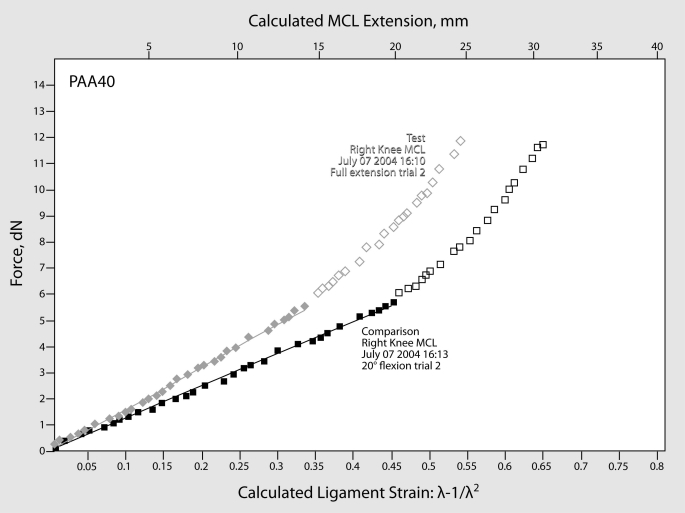
The slope of the force-strain line was produced by the arthrometer software (Figures 2 and 3). Data analysis was performed on the resulting slope at 60 N; beyond this force, the slope line becomes more curvi linear than linear, indicating a change in how consistently the strain is increasing as additional force is applied. No conclusion can be drawn from in vivo studies as to the cause of this curvature beyond 60 N of force, but other restraining structures of the medial knee may be able to contribute to resistance when additional force is added.
Figure 2. A typical plot of the resultant slopes of a participant's medial knee in full extension. The difference between the left and right leg was approximately 1.2%. Data were collected to 120 N (12 dN), but data points above 60 N (6 dN) of force were disabled (empty boxes). MCL indicates medial collateral ligament.
Figure 3. A typical plot of the resultant slopes, comparing the slope of the knee in full extension and in 20° of flexion. The difference was approximately 33% in this volunteer. MCL indicates medial collateral ligament.
Statistical Analysis
We calculated dependent t tests to analyze the data and determine if differences existed in medial tibiofemoral joint and MCL stiffness bilaterally and in 2 positions of knee flexion. The SPSS statistical software (version 11.0; SPSS Inc, Chicago, IL) was used in all statistical analysis and α was set a priori at .05.
Results
The means and SDs of the slope values measured at 60 N were 16.1 ± 3.3 (right) and 15.8 ± 3.1 (left) with the knee in full extension and 12.2 ± 3.1 (right) and 11.7 ± 2.8 (left) at 20° of flexion. No difference was noted in the slope of the dominant knee versus the nondominant knee in full extension (t44 = 0.743, P = .461, η2 = .012, 1 − β = .112) or in 20° of flexion (t44 = 1.2, P = .236, η2 = .032, 1 − β = .217).
The slope values for the right and left legs were averaged and used to determine if differences existed in the 2 knee positions (extension: 16.0 ± 2.9, 20° of flexion: 12.0 ± 2.7). Stiffness was greater when the knee was in full extension versus 20° of flexion (t44 = 12.0, P < .001).
Discussion
The Slope of the Force-Strain Line
It is important to first make clear what is meant by ligament stiffness and what the slope of the force-strain relationship, generated by the arthrometer, represents. In this paper, we have used the term stiffness to represent the slope of the force-strain relationship with the understanding that both the Young elastic modulus (E) and cross-sectional area of the unstretched ligament (Ao) contribute to this stiffness. The arthrometer encoders record force-displacement data that the software processes to produce plots of force against strain. Thus, force equals cross-sectional area of the unstretched tissue times its elastic modulus times strain (F = Ao·E [α − 1/α2], where F stands for the force, Ao for the cross-sectional area of the unstretched tissue, E for the Young elastic modulus of the tissue, and [α − 1/α2] for the strain in the tissue). α is the ratio of the lengths of the stretched and the unstretched tissue.14
It is also important to be clear about what is meant by strain in the context of this paper. Physically, 1-dimensional strain is defined as Δl/lo, where Δl is the increase in length as the result of the applied force, and lo is the unstretched length of the test sample.15 Differentiation of the force with respect to length, dF/dl, then yields the value for Ao·E for samples of nonpolymeric materials such as metals. On the other hand, for polymeric materials, such as ligaments, the relationship F = Ao·E(α − 1/α2) applies, at least for small extensions of the ligament. Differentiation with respect to length (l) then yields dF/dl = Ao·E(1 + 2/α3). For the purpose of this study and built into the design of the LigMaster system, only changes in the values of Ao and E are of importance. These can be most easily assessed by differentiating force with respect to (α − 1/α2) instead of length (l).
As a result, the slope of the linear relationship produced by the LigMaster system is proportional to both the cross-sectional area of the unstretched ligament and the elastic modulus of the ligament. Therefore, an observed decrease in the slope could represent a decrease in either Ao or E, or both, depending on the circumstances. When comparing the slope values on healthy knees in full extension and in 20° of flexion, a difference in the size of the compared medial knee structures results in a difference in slope values. We compared calculated ligament stiffness in uninjured adults and found no differences in the slope of the force-strain line between the dominant and nondominant knees, as would be expected in healthy participants. We did find a significant difference in the slope values between full extension and 20° of flexion, as expected, because the flexed knee has fewer tissues (ie, smaller Ao) aligned to resist the force than the fully extended knee.
All subjects showed an essentially linear force-strain relationship up to 60 N of force applied when the knee was extended and slightly less when the joint was in 20° of flexion. Above 60 N of force, the relationship showed an upward curvilinearity for all participants. For the purpose of this study, we determined the slope of the force-strain relationship from the linear portion up to 60 N by using the built-in, linear best-fit-line technique and disabling all points above 60 N (Figures 2 and 3).
Anatomy of the Medial Collateral Ligament
The medial knee ligaments are divided into the capsular and noncapsular layers.9 More specifically, the MCL is often divided into the superficial layer and deep layer, whereas the posterior oblique ligament (POL) is considered a thickening in the capsular ligament that is closely related to the 2 layers of the MCL.16,17 The superficial layer, which is also called the tibial collateral ligament, is not a part of the medial capsule but a separate anatomical entity that supports the medial capsule and has its proximal attachment about 1 cm anterior and distal to the adductor tubercle.9 The positioning of these fibers increases the ligament's ability to resist valgus and external rotation stresses, but this resistance depends upon the amount of flexion in which the knee is positioned.6,16,18 During flexion, the anterior fibers tighten and resist valgus motion, while the posterior fibers slacken.6,16,18–20 How much flexion is needed to decrease the contribution of the anterior fibers to resisting a valgus force is unknown, but our findings suggest that between 0° and 20° of flexion, the tibiofemoral joint has fewer structures (contributing to Ao) positioned to resist force. In other words, the slope of the force-strain line is less; thus, the calculated stiffness of the medial knee changes at some point between 0° and 20° of knee flexion.
Functional Units of the Medial Collateral Ligament
In acting as a tibiofemoral joint stabilizer, the MCL can be divided into 3 functional units: (1) the superficial medial portion, with the anterior border containing the long fibers, (2) the deep medial portion, which includes the meniscofemoral and meniscotibial ligaments, or middle capsular ligament, and (3) the posterior oblique fibers, which blend into the knee's posterior capsule.8,16,21 Scientists6,16 have found that the mid medial capsule provides important attachment sites for the medial meniscus but that it does not have a role in limiting medial laxity. Grood et al6 noted little resistive support from the capsule in most specimens and considered it only to function as insertion sites for the meniscus. Pressman and Johnson19 reported that when the knee was extended, the anterior cruciate ligament (ACL) and posteromedial corner (the POL, medial meniscus, and semimembranosus) assisted in resisting valgus force. In general, medial soft tissue structures provide joint stability as well as tissue stiffness to the medial knee joint. Researchers have studied the medial knee structures at various angles: some22,23 tested the MCL in full extension and in 30° of flexion; one group24 tested the knee in 0°, 10°, 20°, and 45° of flexion; and another group3 tested the functional properties of the MCL in 0°, 20°, and 90° of knee flexion. We chose to test the MCL in 20° of knee flexion because it is the minimum of the standard 20° to 30° range and because it was difficult to measure the medial knee in more than 20° of flexion with the LigMaster. We found greater calculated stiffness in the medial knee when the limb was in full extension than when it was flexed to 20°.
Strain Measurements of the Tibiofemoral Joint
Strain across the MCL is highly nonhomogeneous, meaning that different regions of the ligament withstand different amounts of load.25 Fibers of different portions of the MCL are positioned at different angles, so they become slack or taut during motion and, therefore, stabilize the tibiofemoral joint at different angles and joint positions.8,18,23 When the knee flexes, the MCL slides backward, the anterior portion becomes taut in nearly all degrees of flexion,18,20,26 and the posterior portion of the ligament becomes slack.6,24 When the knee extends, the MCL moves forward, and both the anterior and posterior portions are taut.20 In full extension, positioning of all portions of the MCL prevents tibiofemoral joint valgus movement.6,18,19,22,27
Warren et al16 sectioned portions of the MCL and tested medial joint opening as each structure was cut. When the superficial fibers alone were cut, a significant increase in medial joint opening resulted, even with the deep ligaments, posterior capsule, ACL, and posterior cruciate ligament (PCL) intact. However, the tibiofemoral joint was not forced into full extension but was grossly set at 0° of flexion and, therefore, could have been lacking the last “bit of jog of extension.”16
One group6 found that at full extension, the MCL decreased valgus stress by about 50% while the capsule (both anterior and posterior portions) added nearly 25%, and the ACL and PCL together (but mostly the PCL) assisted by approximately 25%. Haimes et al27 found that the superficial MCL alone had a significant restraint to knee abduction at all flexion angles except 0°. As long as the superficial MCL was intact, cutting the posteromedial capsule and POL had no effect, but when the superficial MCL was sectioned, the posterior elements became more important in resisting valgus stress in the MCL-deficient knee.27 When the tibiofemoral joint is released from full extension, rotation of the tibia permits more degrees of freedom. We added a foot plate in this study, as described earlier, to decrease rotational motion of the leg when adding a valgus force to limit the abduction motion to 1 degree of freedom (Figure 1).
Kennedy et al28 determined that the most lax position of the MCL is full flexion and the most taut position is in hyperextension, but the most strain on the MCL occurs when the tibiofemoral joint is between 0° and 30° of flexion. This posterior and middle fibers are affected more than the anterior fibers, which stay taut throughout the range of motion.20,28 We took care to be sure that participants able to hyperextend at the knee joint were tested in 0° of flexion, that is, full extension.
Arms et al18 differentiated among the anterior, mid, and posterior divisions of the superficial MCL and found that the posterior long fibers demonstrated the greatest increases in strain of all fibers between 15° and 35° of knee flexion. Our results support these findings; calculated stiffness changed (decreased) at 20° of knee flexion when fewer structures were involved in resisting the induced strain, and the superficial MCL was, in theory, most likely isolated from these other supportive structures.
All of these groups6,18,22,27,28 were testing stiffness of human cadaver ligaments, and we were calculating in vivo stiffness in human knees. However, from these studies, although the findings are inconsistent and difficult to compare because of the different protocols used, it seems acceptable to conclude that in full extension, the MCL provides the primary resistance to valgus stress, and the posterior capsule and cruciate ligaments add stiffness to the knee, acting as important secondary restraints. Other soft tissue structures add support to the medial knee joint, and the “screw-home” mechanism adds to strain values when the joint is in full extension. This explains our result of increased stiffness of the knee in full extension versus in 20° of flexion. These strain values change when the knee is flexed, but they remain equal bilaterally and, therefore, do not affect the difference between the slopes for the left and right knee.
Dominant Versus Nondominant Leg: Side Differences
Ford et al29 defined leg dominance as an imbalance between muscular strength and recruitment patterns of the lower extremities, such that one side demonstrates greater dynamic control. Leg dominance, as it relates to dynamic stabilizers (ie, the neuromuscular system) is obvious in athletes who predominantly use one leg over the other in a functional manner. Whether one leg is dominant with regard to the static stabilizers (ie, the ligaments, menisci, and bony geography) is less obvious. Our findings support the lack of a dominant leg with regard to static stabilizers of the tibiofemoral joint.
Markolf et al3 found significant differences (ranging from 35% to 50%) in laxity and stiffness (19% to 24%) between normal right and left legs of participants but did not distinguish between dominant and nondominant legs; they also concluded that no consistent pattern of difference existed between the legs of the same person. Rosene and Fogarty4 found that in males tested with the KT-1000 arthrometer (MEDmetric Corp, San Diego, CA), anterior tibial translation was statistically different in the right and left knees (the right side had lower anterior translation means) and suggested that differences between the sides should be expected when making comparisons of ligament laxity with arthrometers. However, when measuring laxity of the ACL, Anderson et al5 noted no difference in side-to-side measurements using 5 different arthrometers. We found no differences between the dominant and nondominant legs in medial knee stiffness in full extension or the calculated stiffness of the MCL in 20° of knee flexion using the LigMaster arthrometer.
Conclusions
Static stabilizers of the medial knee, in particular the MCL, had the same stiffness bilaterally and, thus, we support the use of the uninjured knee as a control when performing bilateral comparisons after injury. Resistance to valgus force was greater when the knee was in full extension than in 20° of flexion. This finding supports testing of the medial knee in both extension and flexion when trying to isolate different medial tibiofemoral joint structures, in particular the MCL. Future researchers should determine if the ideal amount of knee flexion to isolate the MCL is 5°, 10°, 15°, 25°, or 30°, rather than 20° of tibiofemoral joint flexion.
Acknowledgments
We thank Kevin Lynch at Sport Tech, Inc (Charlottesville, VA), for technical assistance with this study.
Footnotes
Patricia A. Aronson, PhD, LPTA, ATC, contributed to conception and design; acquisition and analysis and interpretation of the data; and drafting, critical revision, and final approval of the article. Arie M. Rijke, PhD, MD, and Christopher D. Ingersoll, PhD, ATC, FACSM, contributed to conception and design, analysis and interpretation of the data, and critical revision and final approval of the article.
References
- 1.Hillard-Sembell D, Daniel D.M, Stone M.L, Dobson B.E, Fithian D.C. Combined injuries of the anterior cruciate and medial collateral ligaments of the knee: effect of treatment on stability and function of the joint. J Bone Joint Surg Am. 1996;78(2):169–176. doi: 10.2106/00004623-199602000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Petersen W, Laprell H. Combined injuries of the medial collateral ligament and the anterior cruciate ligament: early ACL reconstruction versus late ACL reconstruction. Arch Orthop Trauma Surg. 1999;119(5,6):258–262. doi: 10.1007/s004020050405. [DOI] [PubMed] [Google Scholar]
- 3.Markolf K.L, Graff-Radford A, Amstutz H.C. In vivo knee stability: a quantitative assessment using an instrumented clinical testing apparatus. J Bone Joint Surg Am. 1978;60(5):664–674. [PubMed] [Google Scholar]
- 4.Rosene J.M, Fogarty T.D. Anterior tibial translation in collegiate athletes with normal anterior cruciate ligament integrity. J Athl Train. 1999;34(2):93–98. [PMC free article] [PubMed] [Google Scholar]
- 5.Anderson A.F, Snyder R.B, Federspiel C.F, Lipscomb A.B. Instrumented evaluation of knee laxity: a comparison of five arthrometers. Am J Sports Med. 1992;20(2):135–140. doi: 10.1177/036354659202000207. [DOI] [PubMed] [Google Scholar]
- 6.Grood E.S, Noyes F.R, Butler D.L, Suntay W.J. Ligamentous and capsular restraints preventing straight medial and lateral laxity in intact human cadaver knees. J Bone Joint Surg Am. 1981;63(8):1257–1269. [PubMed] [Google Scholar]
- 7.Starkey C, Ryan J. Evaluation of Orthopedic and Athletic Injuries. 2nd ed. Philadelphia, PA: FA Davis; 2002. pp. 211–219. [Google Scholar]
- 8.Robinson J.R, Bull A.M.J, Amis A.A. Structural properties of the medial collateral ligament complex of the human knee. J Biomech. 2005;38(5):1067–1074. doi: 10.1016/j.jbiomech.2004.05.034. [DOI] [PubMed] [Google Scholar]
- 9.Hughston J.C, Andrews J.R, Cross M.J, Moschi A. Classification of knee ligament instabilities, part I: the medial compartment and cruciate ligaments. J Bone Joint Surg Am. 1976;58(2):159–172. [PubMed] [Google Scholar]
- 10.Shultz S.J, Houglum P.A, Perrin D.H. Assessment of Athletic Injuries. Champaign, IL: Human Kinetics; 2000. pp. 290–291. [Google Scholar]
- 11.Arnheim D.D, Prentice W.E. Principles of Athletic Training. 10th ed. Boston, MA: McGraw Hill; 2000. The knee and related structures. pp. 515–565. [Google Scholar]
- 12.Rijke A.M. LigMaster user's manual. Sport Tech Inc. US patent 6,419,645. 2002 [Google Scholar]
- 13.Aronson P.A. Intertester and intratester reliability of measurement of the medial collateral ligament stiffness using the LigMaster [dissertation] Charlottesville, VA: University of Virginia; p. 2005. [Google Scholar]
- 14.Rijke A.M, Perrin D.H, Goitz H.T, McCue F.C., III Instrumented arthrometry for diagnosing partial versus complete anterior cruciate ligament tears. Am J Sports Med. 1994;22(2):294–298. doi: 10.1177/036354659402200223. [DOI] [PubMed] [Google Scholar]
- 15.Billmeyer F.W. Textbook of Polymer Science. New York, NY: Wiley International Edition; 1963. p. 184. [Google Scholar]
- 16.Warren L.F, Marshall J.L, Girgis F. The prime static stabilizer of the medial side of the knee. J Bone Joint Surg Am. 1974;56(4):665–674. [PubMed] [Google Scholar]
- 17.Sullivan D, Levy I.M, Sheskier S, Torzilli P.A, Warren R.F. Medial restraints to anterior-posterior motion of the knee. J Bone Joint Surg Am. 1984;66(6):930–936. doi: 10.2106/00004623-198466060-00015. [DOI] [PubMed] [Google Scholar]
- 18.Arms S, Boyle J, Johnson R, Pope M. Strain measurement in the medial collateral ligament of the human knee: an autopsy study. J Biomech. 1983;16(7):491–496. doi: 10.1016/0021-9290(83)90063-5. [DOI] [PubMed] [Google Scholar]
- 19.Pressman A, Johnson D.H. A review of ski injuries resulting in combined injury to the anterior cruciate ligament and medial collateral ligament. Arthroscopy. 2003;19(2):194–202. doi: 10.1053/jars.2003.50054. [DOI] [PubMed] [Google Scholar]
- 20.Brantigan O.C, Voshel A.F. The mechanics of the ligaments and menisci of the knee joint. J Bone Joint Surg. 1941;23(1):44–46. [Google Scholar]
- 21.Slocum D.B, Larson R.L, James S.L. Late reconstruction of ligamentous injuries of the medial compartment of the knee. Clin Orthop Relat Res. 1974;100:23–55. [PubMed] [Google Scholar]
- 22.Seering W.P, Piziali R.L, Nagel D.A, Schurman D.J. The function of the primary ligaments of the knee in varus-valgus and axial rotation. J Biomech. 1980;13(9):785–794. doi: 10.1016/0021-9290(80)90240-7. [DOI] [PubMed] [Google Scholar]
- 23.Hull M.L, Berns G.S, Varma H, Patterson H.A. Strain in the medial collateral ligament of the human knee under single and combined loads. J Biomech. 1996;29(2):199–206. doi: 10.1016/0021-9290(95)00046-1. [DOI] [PubMed] [Google Scholar]
- 24.Shapiro M.M, Markolf K.L, Finerman G.A, Mitchell P.W. The effect of section of the medial collateral ligament on force generated in the anterior cruciate ligament. J Bone Joint Surg Am. 1991;73(2):248–256. [PubMed] [Google Scholar]
- 25.Gardiner J.C, Weiss J.A, Rosenberg T.D. Strain in the human medial collateral ligament during valgus loading of the knee. Clin Orthop Relat Res. 2001;391:266–274. doi: 10.1097/00003086-200110000-00031. [DOI] [PubMed] [Google Scholar]
- 26.Meister B.R, Michael S.P, Moyer R.A, Kelly J.D, Schneck C.D. Anatomy of kinematics of the lateral collateral ligament of the knee. Am J Sports Med. 2000;28(6):869–878. doi: 10.1177/03635465000280061601. [DOI] [PubMed] [Google Scholar]
- 27.Haimes J.L, Wroble R.R, Grood E.S, Noyes F.R. Role of the medial structures in the intact and anterior cruciate ligament-deficient knee: limits of motion in the human knee. Am J Sports Med. 1994;22(3):402–409. doi: 10.1177/036354659402200317. [DOI] [PubMed] [Google Scholar]
- 28.Kennedy J.C, Hawkins R.J, Willis R.B. Strain gauge analysis of knee ligaments. Clin Orthop Relat Res. 1977;129:225–229. doi: 10.1097/00003086-197711000-00031. [DOI] [PubMed] [Google Scholar]
- 29.Ford K.R, Myer G.D, Hewett T.E. Valgus knee motion during landing in high school female and male basketball players. Med Sci Sports Exerc. 2003;35(10):1745–1750. doi: 10.1249/01.MSS.0000089346.85744.D9. [DOI] [PubMed] [Google Scholar]