Abstract
The NOD (nonobese diabetic) mouse has been studied as an animal model for autoimmune insulin-dependent diabetes and Sjögren’s syndrome. NOD.Igμnull mice, which lack functional B lymphocytes, develop progressive histopathologic lesions of the submandibular and lachrymal glands similar to NOD mice, but in the absence of autoimmune insulitis and diabetes. Despite the focal appearance of T cells in salivary and lachrymal tissues, NOD.Igμnull mice fail to lose secretory function as determined by stimulation of the muscarinic/cholinergic receptor by the agonist pilocarpine, suggesting a role for B cell autoantibodies in mediating exocrine dryness. Infusion of purified serum IgG or F(ab′)2 fragments from parental NOD mice or human primary Sjögren’s syndrome patients, but not serum IgG from healthy controls, alters stimulated saliva production, an observation consistent with antibody binding to neural receptors. Furthermore, human patient IgG fractions competitively inhibited the binding of the muscarinic receptor agonist, [3H]quinuclidinyl benzilate, to salivary gland membranes. This autoantibody activity is lost after preadsorption with intact salivary cells. These findings indicate that autoantibodies play an important part in the functional impairment of secretory processes seen in connection with the autoimmune exocrinopathy of Sjögren’s syndrome.
Sjögren’s syndrome is an autoimmune rheumatic disease primarily targeting the salivary and lachrymal glands (1, 2). It is often a complication of connective tissue diseases such as rheumatoid arthritis or systemic lupus erythematosus. Although the histopathology of the tissue is characterized by the presence of lymphocytic infiltrates consisting of CD4+ T cells, a minor component of CD8+ T cells, B cells, and macrophages, the pathophysiological outcome is the loss of exocrine gland secretory function (1, 2). Patients with Sjögren’s syndrome additionally demonstrate hypergammaglobulinemia on serological analyses, with a range of autoantibodies reactive against cell surface, cytoplasmic and nuclear proteins of exocrine tissue (1, 3, 4). Although the pathogenesis of autoimmune sialoadenitis and dacryoadenitis remain unclear, animal models for the histopathology have demonstrated the dependence of this aspect of disease on transfer of activated T cells (5–7).
Despite the identification of numerous mouse models mimicking the histopathology of Sjögren’s syndrome, only the nonobese diabetic (NOD) mouse has been found to develop the corresponding clinical outcome of loss of secretory function (8–10). The NOD mouse, first identified as a model for type I, insulin-dependent diabetes, develops a Sjögren’s syndrome-like immunopathology of the exocrine glands (11). Genetic analyses and immune cell transfer studies have shown that these two autoimmune diseases arise independently in the same animal (5–7, 12, 13). Cell transfer studies (5–7) have demonstrated a major role for CD4+ T cells in the pathogenesis of both these autoimmune diseases, but more recent results have implicated the need for immunologically active B cells in the initiation of the autoimmune process. Noorchashm et al. (14) have shown that continuous injection of anti-Igμ antibodies into NOD mice results in the absence of insulitis, diabetes, and sialoadenitis. Additionally, congenic NOD B cell knockout mice, NOD.Igμnull, do not develop insulitis or diabetes, demonstrating a requirement for B lymphocytes in the initiation of the autoimmune tissue targeting of the pancreas (15, 16).
An analysis of the underlying signal transduction response in the exocrine tissues from NOD mice has revealed the specific down-regulation of intracellular second-messenger signaling components adenylate cyclase and phospholipase C (17, 18). This was accompanied by a corresponding reduction in the density of cell surface muscarinic and β-adrenergic receptors. Further evaluation of sera collected from older NOD mice detected the presence of a population of autoantibodies capable of reacting with the receptors responsible for neural stimulatory initiation of exocrine secretion. A similar set of neurostimulatory autoantibodies has been reported to be present in the IgG pool isolated from primary Sjögren’s syndrome patients (19). Using the congenic NOD.Igμnull mouse, we have investigated the role of B lymphocytes in the pathogenesis of autoimmune exocrinopathy in the NOD mouse model for Sjögren’s syndrome. The observations presented here suggest that development of exocrine gland secretory dysfunction depends on the presence of B lymphocytes and that autoantibodies generated from these cells are important in the clinical manifestation of xerostomia and keratoconjunctivitis sicca. Furthermore, the appearance of T cells in exocrine tissue, despite the lack of a corresponding insulitis, supports the concept that NOD mice develop two, independent autoimmune diseases.
METHODS
Materials.
C57BL/6-scid and NOD/Lt mice (n = four to six animals/group) were bred and maintained under specific pathogen-free conditions in the mouse facility at the University of Florida, Gainesville, FL, and the Forsyth Dental Center, Boston, MA. NOD.Igμnull mice were obtained from David Serreze, The Jackson Laboratory, and bred in the above animal facility. Both male and female mice at 8–12 weeks and >20 weeks of age were used.
Histological Evaluation.
Parotid, submandibular, and lachrymal glands as well as pancreas were identified by gross morphology and freed of connective tissue and lymph nodes before a 4-hr fixation in 10% formalin and embedding in paraffin blocks. Five-micron thin sections were cut, stained with hematoxylin/eosin, and examined for focal lymphocytic infiltrates by light microscopy (8, 9).
Saliva Collection and Preparation of Gland Lysates.
Whole saliva was collected after stimulation of secretion by using isoproterenol (0.20 mg/100 g body weight) and pilocarpine (0.05 mg/100 g body weight) dissolved in saline as described previously (8, 9). Saliva samples were collected for 10 min from groups of n = four to six mice on two separate occasions and then frozen at −80°C. Excised parotid and submandibular glands were homogenized in 10 mM Tris buffer (pH 7.4) and immediately frozen at −80°C. Protein assays of both saliva and gland lysates were performed using the Bio-Rad protein assay reagent with BSA as the standard (20). Amylase assays were performed as described previously by using starch as the substrate (8, 20).
Cysteine Protease Activity.
Protease activity in saliva and gland lysates were determined by using a standard protease assay as described elsewhere (21). The reaction mixture consisted of 25 μl 100 mM sodium benzoyl-dl-arginine-p-nitroanilide (BAPNA) in DMSO, 10 μl unknown sample, 190 μl phenylmethylsulfonyl fluoride (PMSF) buffer consisting of 0.2 mg/ml DTT, 0.5 mg/ml Na2EDTA, and 1.0 mM PMSF in 100 mM phosphate buffer (pH 6.0). Experimental samples, as well as a dilution profile of papain, were incubated at 37°C for 1 hr. The reactions were terminated by the addition of 25 μl of glacial acetic acid and adjusted to 1.0 ml with ddH2O, and the optical density was determined at OD405 to determine the amount of p-nitroaniline released. Each assay was performed in duplicate on three separate occasions.
PAGE and Western Blot Analysis.
Total salivary proteins (15 μg/well) or gland lysates (50 μg/well) were separated on 10% or 12% SDS-polyacrylamide gels (17, 21). Individual submandibular gland lysates from groups of 4- to 8-week-old and 20-week-old mice were prepared by Dounce homogenization in 10 mM Tris buffer (pH 7.5) after removal of lymph nodes and connective tissue. The proteins were transferred to Immobilon-P membranes (Millipore), blocked in TBS containing 3% nonfat milk and 3% BSA, and incubated in a 1:10,000 dilution of rabbit polyclonal antibody to parotid secretory protein, washed three times, incubated with a goat anti-rabbit alkaline phosphatase-conjugated secondary antibody, and reacted with chromogenic substrate as described previously (20). All gels were run on two separate occasions for reproducibility of results from individual mice.
IgG Preparation and Injection into Mice.
Sera were isolated from whole blood collected from patients diagnosed with primary Sjögren’s syndrome (SS) by the loss of saliva and tear production, positive Rose Bengal staining, lymphocytic foci in minor labial gland biopsies, and the presence of antinuclear SS-A/Ro and SS-B/La autoantibodies in serological evaluations (1, 2). At the time of serum collection, the patients were determined to be free of other complicating autoimmune diseases. Age- and sex-matched healthy individuals were used for control sera. The ages ranged from 30 to 68 years of age. Sera were also collected from >20-week-old NOD/Lt mice.
Murine and human IgG fractions were isolated by standard protein A-agarose and DEAE-chromatography, respectively, dialyzed to remove excess salts, and lyophilized to concentrate. The purity of the IgG fractions was assessed at >90% by SDS/PAGE. Normal control mouse IgG was purchased from Sigma and was of >90% purity (ultrapure grade). The final IgG fraction was filter-sterilized and injected into the intraperitoneal cavity of 10- to 12-week-old NOD.Igμnull mice at 100 μg/100 μl PBS.
Preparation of F(ab′)2 from Human IgG.
Antibody fractions isolated by DEAE chromatography were digested overnight with pepsin (1:100 of IgG) in a water bath at 37°C. The preparations were passed over protein-G Sepharose columns to remove undigested antibodies and Fc fragments. The unbound fraction was tested with anti-F(ab′)2-specific and anti-Fc-specific peroxidase-conjugated antibodies (Jackson ImmunoResearch) to confirm the purity of the preparation. F(ab′)2 fragments were injected into the intraperitoneal cavity of mice at 10 μg/100 μl.
Muscarinic Receptor Binding Assay.
Mouse parotid gland membranes were isolated as described previously (8). Total membrane protein (250 μg) was incubated in a 1.0-ml volume of 50 mM Tris buffer (pH 7.4) containing 10 mM MgCl2 and protease inhibitors (8) at 4°C for 15 hr with no or varying concentrations of human IgG. After the incubation with gentle mixing, the samples were incubated at 25°C for 1 hr with the addition of 5.0 nM [3H]QNB (quinuclidinyl benzilate; Amersham; 5 × 105 cpm/reaction). The radiolabel bound to membranes was collected by centrifugation at 15,000 × g and washed in the above buffer three times before the addition of scintillation mixture and analysis of the radiolabel bound to the membranes by liquid scintillation counting in a Beckman LSC 3801 Counter. Alternatively, membrane receptors were first radiolabeled by incubation with [3H]QNB in the above buffer containing 1.0% Triton X-100 for 1 hr at 37°C, followed by immunoprecipitation with human control or Sjögren’s syndrome patient IgG. Receptor–IgG complexes were collected by the addition of Protein A-agarose (Sigma) beads followed by centrifugation as above.
Statistical Analysis.
All measures of variance are given as SEM. By the Shapiro and Wilks test (13) the distributions for saliva and tear volumes as well as protein concentration were found to be normal (P > 0.05) and were analyzed by a parametric ANOVA (20, 21). Tests of ANOVA between independent means were not normal (P < 0.05) for cysteine protease activity and were performed subsequently with a nonparametric single-factor test by using a sas computer software program, results in which P < 0.05 was considered significant.
RESULTS
Histological Evaluation of NOD.Igμnull Exocrine Glands.
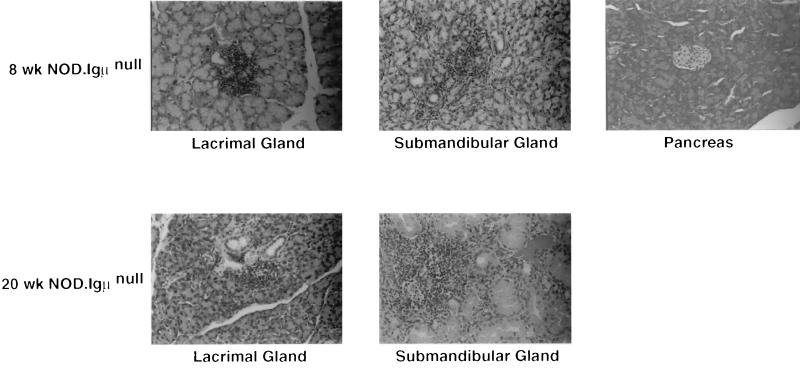
Flow cytometric analyses of splenic lymphocytes prepared from NOD.Igμnull mice failed to detect the presence of B cells. At the same time, sera isolated from these mice lacked detectable IgG. These findings indicate that NOD.Igμnull mice used in these studies preserve the knockout genotype/phenotype. Despite the absence of pancreatic autoimmunity in 8-week-old NOD.Igμnull mice, histological evaluation revealed the presence of small lymphocytic infiltrates of both the lachrymal and submandibular salivary glands (Fig. 1). Older NOD.Igμnull mice (>20 weeks) revealed the continued presence of focal infiltrates of the exocrine tissues with only an occasional peri-islet or islet infiltration observed. However, none of these mice developed elevated blood glucose levels or diabetes.
Figure 1.
Histological analysis of the exocrine tissues and pancreas from NOD.Igμnull mice. Glands from n = 4 animals per age group were evaluated by two individuals for independent analysis. (×200.)
Detection of Biochemical Alterations in the Saliva and Exocrine Tissue Lysates of NOD.Igμnull Mice.
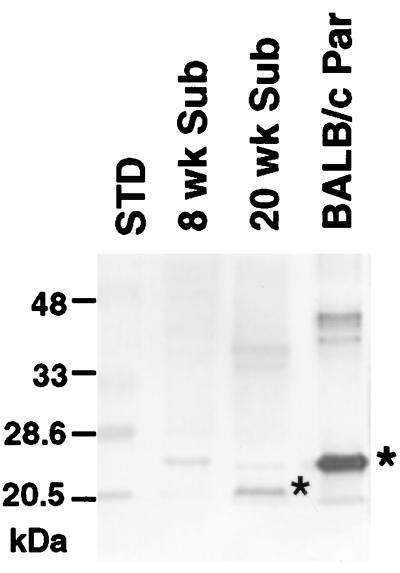
Hallmark biochemical changes in saliva volume and composition, as well as glandular protein synthesis that occur independently of autoimmunity (20, 21), were observed with increased age of the mice. Secretory function of NOD.Igμnull mice >20 weeks of age showed that stimulated flow rates were not different from those of 8-week-old mice (P > 0.05; Table 1), with values similar to those reported previously for healthy control BALB/c and C57BL/6 mice (8, 9). Cysteine protease activity, a marker for acinar and ductal epithelial cell apoptosis, was increased 1.4-fold in the saliva of NOD.Igμnull at 20 weeks of age as compared with mice 8 weeks of age (Table 1; P < 0.01). Both young and older mice had overall elevated cysteine protease activity in submandibular gland lysates, activities similar to the parental NOD strain. However, further analysis of 8-week-old male mice consistently produced higher levels of enzyme activity than 20-week-old male or female NOD.Igμnull mice, while 8-week-old female mice had levels of activity similar to that reported previously for BALB/c and young NOD-scid mice (20, 21). Amylase activity, an enzyme produced by the parotid gland acinar cells, was reduced by 32% in older mice (P < 0.05), again consistent with the previous observations in NOD and NOD-scid mice (8, 9, 17, 18). Total protein content of saliva remained constant between the two age groups. Parotid secretory protein, a normal constituent of differentiated parotid gland synthesis, was observed to be aberrantly synthesized and processed in the submandibular gland of NOD.Igμnull mice by 20 weeks of age (4/4), while gland lysates of younger 8-week-old mice either did not produce the protein (2/4) or produced a small amount (2/4) of the normal 25-kDa isoform (Fig. 2). Thus, except for the loss of secretory function, development of biochemical and physiological changes consistent with previously described nonimmune components of the exocrine tissue epithelial cell pathology occurs independently of the absence of B lymphocytes in NOD.Igμnull mice.
Table 1.
Analysis of age-related physiological and biochemical changes in NOD.Igμnull mice
| Animal | Saliva volume | Total protein | Amylase activity | Crysteine protease activity |
|---|---|---|---|---|
| 8-week NOD.Iμnull (n = 4) | 297.6 ± 28.1 | 13.77 ± 1.98 | 2,961 ± 256 | 31.5 ± 4.8/39.7 ± 5.1 |
| 20-week NOD.Igμnull (n = 6) | 324.8 ± 17.3 | 13.04 ± 2.57 | 2,331 ± 241 | 44.7 ± 3.6/38.8 ± 2.9 |
| 20-week NOD* | 106.2 ± 10.5 | 21.6 ± 3.3 | 1,732 ± 356 | 45.8 ± 5.3/40.6 ± 4.7 |
All values expressed as mean ± SE based on two experimental determinations. Volume and protein concentration, collected over a 10-min period, after stimulation of secretion with a cocktail of autonomic agonists isoproterenol and pilocarpine, is expressed as μl/10 min or mg/ml per 100 g body weight, respectively (8, 9). Amylase activity is expressed as mg starch hydrolyzed/mg protein per 100 g body weight. Cysteine protease activity is expressed as μg protease/min per mg saliva protein and μg protease activity/min per mg submandibular gland lysate. The significance of differences between mean values was tested by use of a paired ANOVA and Student’s t test.
Figure 2.
Western blot detection of parotid secretory protein in gland lysates prepared from 8- and 20-week-old NOD.Igμnull mice. Fifty micrograms of tissue lysates was separated by SDS-polyacrylamide gels. The normal 25-kDa BALB/c isoform and the NOD-specific ≈20.5-kDa isoform are indicated by asterisks. Sub, submandibular gland; Par, parotid gland.
Transfer of Secretory Gland Dysfunction with Serum IgG Fractions.
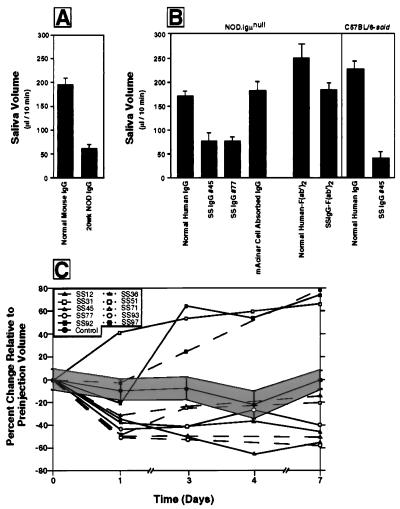
Both primary Sjögren’s syndrome patients and NOD mice produce autoantibodies that interact with the autonomic nervous system receptors responsible for initiating the secretory response (17–19). To determine the potential for IgG antibodies to transfer exocrine tissue dysfunction to young NOD.Igμnull mice, a series of transfer experiments was performed in which IgG from healthy control mice and healthy humans, prediabetic NOD mice, as well as human Sjögren’s syndrome patients were infused into NOD.Igμnull mice. As indicated in Fig. 3A and B, mice given a single infusion of IgG from nondisease mice or healthy human sera retained near-normal secretory function at 24 hr (P > 0.05; n = 4) after secretory stimulation with a secretagogue mixture of β-adrenergic and muscarinic/cholinergic receptor agonists (8). Mice treated with IgG isolated from older, parental NOD/Lt mice secreted only 30% of the saliva volume normally generated. Treatment with IgG from four different Sjögren’s syndrome sera (#77, #36, #93, and #45) resulted in an average 54% decrease in saliva volumes generated, relative to the control, after 24 hr (Fig. 3B; P < 0.001). A 37% decline was noted when purified F(ab′)2 fragments from autoimmune patients were given to mice at a concentration of 10 μg/animal. Injection of the Sjögren’s syndrome sera IgG into an unrelated mouse strain, C57BL/6-scid, again resulted in a decrease in secretory response after challenge with secretory agonists (Fig. 3B). Repeated infusion of normal human IgG caused a decrease in volume collected with time in the control animals (Fig. 3C, 20%; P < 0.05), which was most likely a result of the stress of constant handling of the animals for injection and the saliva collection regimen. More interesting was the observation that 1 week of continuous treatment of mice with individual Sjögren’s syndrome serum IgG showed a loss of secretory function between 40 and 60% (P < 0.001). Whereas 7/10 patients’ sera caused a significant loss of function 24 hr after the first injection of IgG, 1/10 patient’s IgG fraction was capable of stimulating an increase (60–100%; P < 0.001) above initial saliva volumes after 24 hr, and another two patients’ IgG fraction stimulated saliva secretion in all subsequent injections (Fig. 3C). The recovery of saliva production in some of the mice with continuous infusion of IgG is not understood at this time. An additional 1-week washout period with injection of normal human IgG every 48 hr demonstrated that the volumes of stimulated saliva secretion returned to normal levels in mice treated with Sjögren’s syndrome sera and, in some cases, resulted in an overcompensation of volume generated after agonist injection. As an additional control, Sjögren’s syndrome patient IgG fractions were preabsorbed with intact murine salivary gland cells before injection into mice. This resulted in the loss of the ability to induce secretory dysfunction (Fig. 3B).
Figure 3.
Alteration in the levels of saliva volume generated in NOD.Igμnull mice after a single or repeated injection of normal serum IgG, parental NOD, or Sjögren’s syndrome serum IgG fractions. (A) Histogram of saliva volume collected 24 hr after injection of NOD.Igμnull mice with normal or NOD/Lt sera IgG fractions. (B) Histogram of saliva volume after injection with four normal human or four patient IgG fractions. Salivary flow was collected from the oral cavity beginning 1 min after stimulation (n = 4 mice/injection regimen). Mice were injected with 100 μg IgG or 10 μg F(ab′)2. All values are expressed as the mean saliva flow/10 min ± SE. (C) Individual mice injected for 1 week with normal human IgG (n = 5) or individual Sjögren’s syndrome patient (n = 10) IgG fractions.
Histological Changes in Acinar Cells After Repeated Antibody Treatment.
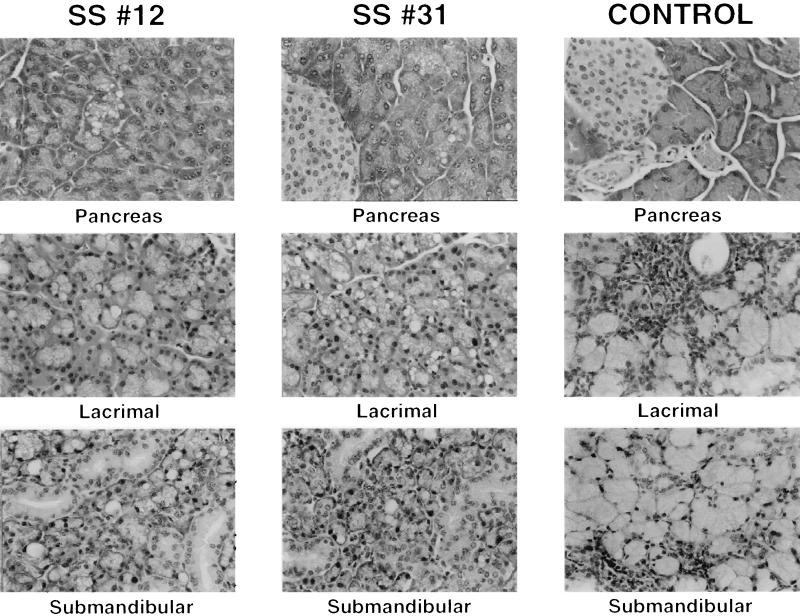
Examination of exocrine tissues from mice after chronic treatment with IgG fractions of Sjögren’s syndrome patient sera revealed the presence of vacuolar structures predominantly in the acinar cell portions of lachrymal, submandibular, and, to a lesser extent, pancreatic tissue (Fig. 4). Observation at higher magnification (×400) clearly showed that vacuolated cells contained condensed nuclei and vacuolar cell structures with indistinguishable cytoplasmic contents surrounded by membranes. Furthermore, there were greater numbers of nuclei whose appearance suggested apoptosis, consistent with previous biochemical studies (20, 21). These vacuolated cells were not detected in significant numbers in mice repeatedly infused with normal human IgG, nor in the ductal cells or pancreatic islets of the Sjögren’s syndrome IgG-treated mice (Fig. 4). Similar structural changes in exocrine tissue histology was observed after the injection of F(ab′)2.
Figure 4.
Histologic profiles of the exocrine tissues of NOD.Igμnull mice after chronic treatment with control or Sjögren’s syndrome IgG fractions. The sections of submandibular, lachrymal, and pancreas were stained by hematoxylin/eosin and observed by light microscopy (×400). Sjögren’s syndrome patients #12 and 31, one stimulating secretion and the other inhibiting secretion, were used in this evaluation.
Muscarinic Receptor Interaction with Sjögren’s Syndrome Patient IgG Fractions.
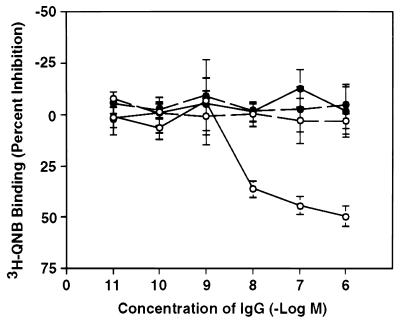
Direct interaction of the antibody fraction with salivary gland muscarinic receptors was demonstrated by dose-dependent competition for receptor binding by using radiolabeled agonist. As indicated in Fig. 5, incubation of IgG fractions from Sjögren’s syndrome patients, but not from healthy controls, inhibited the subsequent binding of the muscarinic receptor agonist, [3H]QNB, to mouse parotid gland membrane preparations in a dose-dependent fashion. When muscarinic/cholinergic receptors first were incubated with radiolabeled agonist, solubilized with nonionic detergent, and immunoprecipitated with antibody fractions, prior binding of agonist prevented subsequent immunoprecipitation with Sjögren’s syndrome patient-derived reagents (Fig. 5). This is consistent with the interpretation that both the muscarinic receptor ligand and a population of patients’ sera IgG compete for interaction with the receptor agonist-binding site.
Figure 5.
Inhibition of‘[3H]QNB binding to NOD parotid gland membranes by primary Sjögren’s syndrome IgG (n = 5; open circles) or normal patient IgG (n = 3; solid circles). Increasing concentrations of human IgG were incubated with parotid gland membranes followed by the addition of 0.5 nM radiolabeled ligand agonist (21) (solid lines). Immunoprecipitation of [3H]QNB-labeled muscarinic receptors by normal and patient IgG is represented by the dashed lines. The results are the mean ± SE for Sjögren’s syndrome patients (#36, 71, 77, 93, 97) and normal healthy controls (#4, 5, 6) performed on two separate occasions in duplicate. Control binding of 100% refers to the value of [3H]QNB bound to the membrane without the addition of antibody reagents (20).
DISCUSSION
A requirement for B lymphocytes in the pathogenesis of Sjögren’s syndrome-like disease is suggested by the fact that NOD.Igμnull mice retain full secretory capacity on stimulation with autonomic receptor agonists, similar to previous observations with the congenic, immunodeficient NOD-scid mouse. The role of secreted autoantibodies rather than B cells as antigen-presenting cell phenotype appears to be potentially more important in the ability of NOD and Sjögren’s syndrome patients to develop the loss of secretory function. The use of isolated IgG fractions to produce salivary gland dysfunction in immunodeficient mice suggests that this component of the immune system is a critical mediator for clinical presentation of sicca complex. Autoimmune exocrinopathy often is thought to result from cytotoxic effects of activated T lymphocytes or cytokines in response to programmed cell death occurring in the glandular epithelial cells (2, 22–24). However, the present results indicate that although T cells may be involved in the pathology of the exocrine tissue in NOD mice, the B cell effector arm appears to induce the full loss of exocrine tissue secretory function. In this regard, the B cell-deficient NOD mouse represents an advance in our ability to evaluate the role of specific immune cells in exocrine tissue secretory function.
Salivary flow is a result of neural stimulation of the acinar and ductal cells of the glands, specifically in response to muscarinic/cholinergic receptor agonists. In contrast, the protein phase is generated in response to agonists stimulating the β-adrenergic receptors (25–27). Autoantibodies directed against autonomic nervous system receptors and possessing agonistic properties have been described in a number of human pathologies (28, 29). Our previous studies in NOD mice have shown decreased receptor density and intracellular signal transduction components, along with autoantibody populations directed against the β-adrenergic and muscarinic/cholinergic receptors (17, 18). Alterations also have been detected in the glandular innervation of the exocrine tissues from Sjögren’s syndrome patients (30, 31). Recent analyses of autoantibodies from primary Sjögren’s syndrome patients have detected antimuscarinic receptor activity capable of acting as a neural receptor agonist (19, 32, 33).
Although the present study does not exclude a role for other circulating autoantibodies, such as SS-A or SS-B (1, 2), in mediating hypofunction, antineural receptor antibodies represent an intriguing potential mechanism for the down-regulation of exocrine secretion. Desensitization of the signal-transduction response can occur through chronic activation of agonist-binding sites or through the generation of autoantibodies capable of directly blocking or sterically hindering the ability of agonists to bind to cell surface receptors, thereby depriving cells of the necessary signals to generate a secretory response. Alternatively, chronic stimulation of receptors can lead to desensitization of the secretory response through down-regulation of surface receptor density (34).
The ability of IgG and F(ab′)2 fragments of sera from Sjögren’s syndrome patients to either stimulate or inhibit secretory function could be related to the stage of the disease at the time the serum was collected or the titer of specific autoantibody fractions. In our study, we found evidence of both exocrine stimulation and inhibition in different Sjögren’s patient IgG. One possible explanation for our results would be that the antiglandular reactive antibody titer is important in determining whether the IgG is stimulatory or inhibitory in NOD.Igμnull mice. We have not observed a similar response when IgG from systemic lupus erythematosus or rheumatoid arthritis patients, free of secondary Sjögren’s syndrome complications, are injected into NOD-scid mice (unpublished observations). The ability of a subset of Sjögren’s syndrome patients to stimulate secretory response is intriguing in light of the potential therapeutic value to patients suffering from secretory dysfunction.
Histological analysis of exocrine tissues treated with patient IgG or F(ab)2 fractions revealed marked morphological changes. Subsequently, both terminal deoxynucleotidyltransferase-mediated UTP end labeling and a specific caspase-3 assay have been conducted to determine whether increased programmed cell death (PCD) is related to this observation. Preliminary results have provided no evidence for increased PCD after antibody transfer (J.B., A.B.P., and M.G.H.-B., unpublished observations). An alternative explanation to PCD is that the autoantibody reaction with receptors on the exocrine cell surface provokes a functional quiescence in the cells manifested in loss of stimulated secretory response. The appearance of histologically identifiable vacuolar structures may be the result of fusion of intracellular secretory granules and digestion of their contents because of a lack of response. Thus, by entering a period of functional rest, the cells may avoid further attack by the activated immune system. The induction of functional quiescence is consistent with the observation that the salivary glands are able to fully recover secretory response after a 1-week washout period in which antibody treatment is terminated.
In summary, the results presented here indicate a primary role for autoantibodies, presumably directed against the autonomic nervous system receptors (17–19), as playing a primary role in the clinical manifestation of Sjögren’s syndrome, namely, the loss of secretory function. The identification of these antibodies as agents in the disease process suggests new modalities for treatment potentially based on specific immunomodulatory therapy.
Acknowledgments
We thank Mr. M. Kerr, Ms. J. Nanni, and Ms. K. Nguyen for technical assistance. This work was supported by National Institute on Dental Research Grant DE 10515 and administrative supplement from the National Institutes of Health Office for Research in Women’s Health Policy (M.G.H.-B.), Juvenile Diabetes Foundation International Grant I96091 (A.B.P.), European Community Biomed Grant BMH4-CT96–0595 (R.J.), the Research Council of Norway Project Nr. 111159/320 (E.P.) and 115563/320 (R.J.), and the Arthritis Foundation (T.R.E.).
ABBREVIATIONS
- NOD
nonobese diabetic
- SS
Sjögren’s syndrome
- QNB
quinuclidinyl benzilate
- BAPNA
sodium benzoyl-dl-arginine-p-nitroanilide
References
- 1.Fox R I, Kang H-I. Rheum Dis Clin N Am. 1992;18:517–538. [PubMed] [Google Scholar]
- 2.Fox P C, Speight P. Crit Rev Oral Biol Med. 1996;7:144–158. doi: 10.1177/10454411960070020301. [DOI] [PubMed] [Google Scholar]
- 3.Haneji N, Nakamura T, Takio K, Yanagi K, Higashiyama H, Saito I, Noji N, Sugino H, Hayashi Y. Science. 1997;276:604–607. doi: 10.1126/science.276.5312.604. [DOI] [PubMed] [Google Scholar]
- 4.Chan E K L, Hamel J C, Buyon J P, Tan E M. J Clin Invest. 1991;87:68–75. doi: 10.1172/JCI115003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Christianson S W, Schultz L D, Leiter E H. Diabetes. 1993;42:44–55. doi: 10.2337/diab.42.1.44. [DOI] [PubMed] [Google Scholar]
- 6.Garchon H J, Juan J J, Eloy L, Bedossa P, Bach J F. Eur J Immunol. 1994;24:380–384. doi: 10.1002/eji.1830240217. [DOI] [PubMed] [Google Scholar]
- 7.Skarstein K, Johannessen A C, Holmdahl R, Jonsson R. Clin Immunol Immunopathol. 1997;84:177–184. doi: 10.1006/clin.1997.4387. [DOI] [PubMed] [Google Scholar]
- 8.Hu Y, Nakagawa Y, Purushotham K R, Humphreys-Beher M G. Am J Physiol. 1992;263:E607–E614. doi: 10.1152/ajpendo.1992.263.4.E607. [DOI] [PubMed] [Google Scholar]
- 9.Humphreys-Beher M G, Hu Y, Nakagawa Y, Wang P-L, Purushotham K R. Adv Exp Med Biol. 1994;350:631–356. doi: 10.1007/978-1-4615-2417-5_105. [DOI] [PubMed] [Google Scholar]
- 10.Moore P A, Bounous D I, Kaswan R L, Humphreys-Beher M G. Lab Animal Sci. 1996;46:125–138. [PubMed] [Google Scholar]
- 11.Asamoto H, Oishi M, Akazawa Y, Tochino Y. In: Insulitis and Type I Diabetes. Seiichiro T, Tochino Y, Noraka K, editors. Tokyo: Academic; 1986. pp. 61–71. [Google Scholar]
- 12.Wicker L S, Appel M C, Dotta F, Pressey A, Miller B J, DeLatato N H, Fischer P A, Boltz R C, Peterson L B. J Exp Med. 1992;176:67–77. doi: 10.1084/jem.176.1.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Robinson C P, Yamachika S, Brayer J, Peck A B, Humphreys-Beher M G. Arthritis Rheum. 1998;41:150–156. doi: 10.1002/1529-0131(199801)41:1<150::AID-ART18>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- 14.Noorchashm H, Noorchashm N, Kern J, Rostami S Y, Barker C F, Naji A. Diabetes. 1997;46:941–946. doi: 10.2337/diab.46.6.941. [DOI] [PubMed] [Google Scholar]
- 15.Serreze D V, Chapman H D, Varnum D S, Hanson M S, Reifsnyder P C, Richard S D, Fleming S A, Leiter E H, Schultz L D. J Exp Med. 1996;184:2049–2053. doi: 10.1084/jem.184.5.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang M, Charlton B, Gautam A M. J Autoimmun. 1997;10:257–260. doi: 10.1006/jaut.1997.0128. [DOI] [PubMed] [Google Scholar]
- 17.Hu Y, Purushotham K R, Wang P-L, Dawson R J, Jr, Humphreys-Beher M G. Am J Physiol. 1994;266:G433–G443. doi: 10.1152/ajpgi.1994.266.3.G433. [DOI] [PubMed] [Google Scholar]
- 18.Yamamoto H, Sims N E, Macauley S P, Nguyen K-H T, Nakagawa Y, Humphreys-Beher M G. Clin Immunol Immunopathol. 1996;78:245–255. doi: 10.1006/clin.1996.0036. [DOI] [PubMed] [Google Scholar]
- 19.Bacman S, L, Sterin-Borda L, Jose Camusso J, Arana R, Hubscher O, Borda E. Clin Exp Immunol. 1996;104:454–459. doi: 10.1046/j.1365-2249.1996.42748.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Robinson C, Yamamoto H, Peck A B, Humphreys-Beher M G. Clin Immunol Immunopathol. 1996;79:50–59. doi: 10.1006/clin.1996.0050. [DOI] [PubMed] [Google Scholar]
- 21.Robinson C P, Yamachika S, Alford C E, Cooper C, Pichardo E L, Shah N, Peck A B, Humphreys-Beher Proc Natl Acad Sci USA. 1997;94:5767–5771. doi: 10.1073/pnas.94.11.5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wu A J, Chen Z J, Tsokos M, O’Connell B, Ambudkar I, Baum B J. J Cell Physiol. 1996;167:297–304. doi: 10.1002/(SICI)1097-4652(199605)167:2<297::AID-JCP14>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 23.Kong L, Ogawa N, Nakabayashi T, Lui G, D’Souza E, McGuff H S, Guerrero G, Talal N, Dang H. Arthritis Rheum. 1997;40:87–97. doi: 10.1002/art.1780400113. [DOI] [PubMed] [Google Scholar]
- 24.Skarstein K, Nerland A H, Eidsheim M, Mountz J D, Jonsson R. Scand J Immunol. 1997;46:373–378. doi: 10.1046/j.1365-3083.1997.d01-142.x. [DOI] [PubMed] [Google Scholar]
- 25.Baum B J, Ito H, Roth G S. In: Adrenoreceptors and Catecholamine Action Part B. Kunos G, editor. New York: Wiley; 1983. pp. 265–294. [Google Scholar]
- 26.Garrett J R. In: The Salivary System. Screebny L M, editor. Boca Raton, FL: CRC Press; 1988. pp. 69–93. [Google Scholar]
- 27.Williams J A. Annu Rev Physiol. 1984;46:361–375. doi: 10.1146/annurev.ph.46.030184.002045. [DOI] [PubMed] [Google Scholar]
- 28.Fu M L X, Herlitz H, Wallukat G, Hilme E, Hedner T, Hoebeke J, Hjalmarson A. Lancet. 1994;344:1660–1663. doi: 10.1016/s0140-6736(94)90456-1. [DOI] [PubMed] [Google Scholar]
- 29.Fu M L X, Magnusson Y, Bergh C-H, Liljequest J A, Waagstein F, Hjalmarson A, Hoebeke J. Clin Immunol Immunopathol. 1994;72:15–20. doi: 10.1006/clin.1994.1101. [DOI] [PubMed] [Google Scholar]
- 30.Konttinen Y T, Sorsa T, Hukkanen M, Segerberg M, Kuhlefelt-Sundström M, Malmström M, Polak J M. J Rheumatol. 1992;19:30–37. [PubMed] [Google Scholar]
- 31.Konttinen Y T, Hukkanen M, Kemppinen P, Segerberg M, Sorsa T, Malmström M, Rose M, Itescu S, Polak J M. Arthritis Rheum. 1992;35:815–820. doi: 10.1002/art.1780350717. [DOI] [PubMed] [Google Scholar]
- 32.Bacman S, Perez Leiros C, Sterin-Borda L, Hubscher O, Arana R, Borda E. Invest Ophthalmol Vis Sci. 1998;39:151–156. [PubMed] [Google Scholar]
- 33.Borda E, Camusso J J, Perez Leiros C, Bacman S, Hubscher O, Arana R, Sterin-Borda L. Mol Cell Biochem. 1996;163:335–341. doi: 10.1007/BF00408674. [DOI] [PubMed] [Google Scholar]
- 34.Hausdorff W P, Caron M G, Lefkowitz R J. FASEB J. 1990;4:2881–2889. [PubMed] [Google Scholar]