Abstract
The mini-incision anterior approach in total hip replacement is not new, but uses a shorter incision than the traditional Hueter approach, typically only 6–8 cm in length. Despite its size, the single anterior incision allows good exposure. It is very atraumatic, preserves muscles and tendons, and allows the patient early mobilisation and fast postoperative recovery. Although, a special table (e.g., a Judet table) and specific tools (e.g., a curved reamer) are needed to perform hip replacement via the mini-anterior approach, any kind of hip prosthesis (cemented or uncemented) can be implanted. As there is a significant learning curve in mastering the mini-incision anterior approach, surgeons are advised to start with a longer incision and then to decrease its length with increasing experience.
Introduction
The mini-anterior approach for total hip arthroplasty (THA) is an old approach first described as the Smith-Petersen [1], then as the Hueter approach more than 50 years ago. The anterior Hueter approach has been used by Judet and Judet for hip joint exposure for arthroplasty techniques since 1947 [2]. The initial technique involved detaching the tensor fascia lata from the antero-lateral crest, whereas the Hueter approach respected the tensor. In France, thousands of hip arthroplasties have been performed via this approach over several decades.
In the 1990s surgeons who were comfortable with the anterior approach reduced the length of the incision from around 12 cm to 6–8 cm. However, nothing but the length of the incision was changed in developing what is now regarded as the “new” minimal anterior approach. In this paper, the author describes, in detail, the mini-anterior approach to total hip replacement and his clinical experience in terms of post-operative recovery and long-term restoration of hip function.
Surgical technique
The procedure described is reproducible and can be used for patients with osteoarthritis (OA) and in patients with previous hip surgery. The SL-Plus stem (Plus Orthopedics AG, Rotkreuz, Switzerland) and the EP-Fit cup were used in all of our cases.
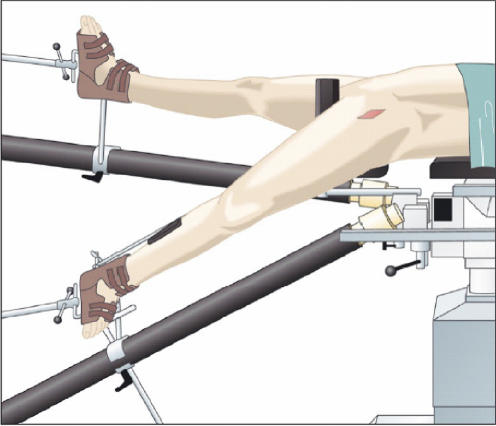
The patient is placed in a dorsal decubitus position on a Judet-type orthopaedic table (Hana table, OSI, USA) (Fig. 1). This table allows traction of the operative extremity, combined with hyperextension, external and internal rotation of the hip, and lowering of foot to the ground during the surgery. All cases were performed with only one surgical assistant. The skin incision is started at a point 2 cm below and 1 cm distal to the antero-superior iliac spine and is extended 6 to 8 cm parallel to an imaginary line joining the anterosuperior iliac spine to the head of the fibula (Fig. 2). Particular care is taken in identifying the bony landmarks due to the proximity of the lateral femoral cutaneous nerve. After incising the skin and subcutaneous fat, the aponeurosis of the tensor fascia lata is reached. The superficial aponeurosis of the tensor fascia lata is incised, and two retractors are placed to displace the tensor fascia lata laterally, and the sartorius medially. The innominate aponeurosis is located immediately on the deeper surface of the tensor fascia lata and may be thick. Beneath this aponeurosis the anterior circumflex vessels are located. They must be identified and tied off or coagulated. The reflected tendon of the rectus femoris is either incised or preserved [3], though we choose to incise it to achieve a better release of the rectus femoris muscle.
Fig. 1.
Judet-type orthopaedic table: Hana table, OSI, USA
Fig. 2.
The skin incision landmarks
The anterior capsule of the hip is exposed by retracting the psoas, iliacus and rectus femoris muscles. Another retractor is slid under the surface of the neck of the femur. The femoral head and neck are exposed via a partial anterior capsulectomy. The cut of the neck is performed with an oscillating saw to avoid damage to the skin or muscles. Following exposure and reaming of the acetabulum, the acetabular component is seated with a curved impactor and oriented in 40°–45° of abduction. Good positioning may be facilitated by palpating the anterior iliac crest. After releasing the traction, the lower limb is carefully lowered and externally rotated to 90°, and locked with the foot on the ground (Fig. 3). Sectioning of the external rotators is avoided and is not required for good femoral exposure. After rasping the femur, the stem is implanted. The hip is reduced by raising the leg from 90° external rotation to the neutral position and releasing traction. After testing stability and motion, closure is done in two planes: the superficial aponeurosis of the tensor and the skin. An aspiration drain is put in and kept in place for 2 days.
Fig. 3.
After releasing the traction, the inferior limb is lowered and rotated 90° externally
Discussion
In total hip replacement, the posterior approach has been popularized because of good exposure of the femur and preservation of the gluteus medius and minimus. However there is an increased incidence of dislocation because of the division of the posterior hip capsule and the external rotators [5, 6]. The lateral approaches involve the detachment of the gluteus medius and minimus from the greater trochaner with a high incidence of postoperative limp [7]. In contrast, the anterior mini-incision offers many theoretical and practical advantages because sectioning of muscle and tendon or the greater trochanter are not required to implant the prosthetic components.
The theoretical advantages of the anterior mini-incision include good visualisation of the acetabulum, although preserving all muscles, no fluoroscopy is required and one does not have to use a specific implant using this approach. Practical advantages include the fast postoperative recovery, no hip limp (because the buttock muscles and the greater trochanter are not affected) and almost no risk of dislocation [3].
In the author’s experience, most patients achieve full weight-bearing on the 1st day postoperatively. Most patients are able to walk without their crutches a few days after the surgery, depending on their age and physical condition of the superior gluteal nerves. The postoperative recovery was fast and there were no cases of hip limp or dislocation. There is almost no risk of dislocation. This observation is consistent with previous follow-up studies of the anterior min-procedure. Siguier et al. [3] reported a dislocation rate of 0.96% in over 1,000 patients, while Mattta et al. [4] reported a dislocation rate of 0.61% in their study with over 400 patients.
A disadvantage of the approach is the fact that a special operating table and specific tools are required. Potential complications include intraoperative femoral and ankle fractures, and damage to the lateral femoro-cutaneous nerve. These can be avoided through use of caution during external rotation of the hip and lowering the foot of the lower limb, which must be performed without traction. If a femoral fracture occurs, the incision can be extended distally and laterally to expose the femoral shaft for application of cerclage wires. Relative contraindications of this procedure include patients who are obese, muscular or have a wide pelvis, but can be easily addressed by simply increasing the length of the incision. To minimise the risk of complications in mastering the mini-incision anterior approach, surgeons are advised to start with a longer incision and then to decrease its length with increasing experience.
Conclusion
The mini-incision anterior approach in total hip arthroplasty is an old approach (Hueter approach) with a shorter skin incision. It is a safe and reproducible technique providing low morbidity and fast postoperative recovery for the patient. Not only the aesthetic aspects of the approach, but also the psychological aspects are predominant because the patients’ well-being is rapidly restored. Early mobilisation and short hospitalisation time have significant social and financial benefits.
Training and experience are crucial to successfully performing this minimally invasive surgical technique, so there is a learning curve for the surgeon and the team. But one can always start with a regular incision length and decrease it when getting familiar with the approach.
Acknowledgements
No sources of funding were used to assist in the preparation of the manuscript, and no conflicts of interest are declared.
References
- 1.DeWal H, Su E, DiCesare PE (2003) Instability following total hip arthroplasty. Am J Orthop 32:377–382 [PubMed]
- 2.Matta JM, Shahrdar C, Ferguson T (2005) Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop 441:115–124 [DOI] [PubMed]
- 3.McCollum DE, Gray WJ (1990) Dislocation after total hip arthroplasty: causes and prevention. Clin Orthop 261:159–170 [PubMed]
- 4.Judet J, Judet R (1950) The use of an artificial femoral head for arthroplasty of the hip joint. J Bone Joint Surg 32B:166–173 [DOI] [PubMed]
- 5.Siguier T, Siguier M, Brumpt B (2004) Mini-incision anterior approach does not increase dislocation rate: a study of 1037 total hip replacements. Clin Orthop 426:164–173 [DOI] [PubMed]
- 6.Smith-Petersen MN (1949) Approach to and exposure of the hip joint for mold arthroplasty. J Bone Joint Surg AM 31-A:40 [PubMed]
- 7.Vicar AJ, Coleman CR (1984) A comaprison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop Relat Res 188:152–159 [PubMed]