Abstract
Total hip arthroplasty through minimally invasive procedures potentially reduces operative trauma, which is expected to result in improved recovery and rehabilitation. We presently perform total hip arthroplasty using minimally invasive techniques via an anterolateral modification of the Watson-Jones approach. This approach is performed in the supine position and requires sterile draping of both legs. It also involves a modified operative technique which preserves the pelvitrochanteric muscles and extends the release of the hip capsule. In order to employ a proven implant system (BICON-PLUS® threaded cup, SL-PLUS® stem), it was necessary to modify the stem rasps and use manipulation rasps as trial stems. In this report, we compare 50 conventional total hip replacements with 50 procedures performed using the minimally invasive procedure in terms of blood loss and the duration of the operation. The length of the skin incision varied between 7 and 12 cm with the minimally invasive technique, compared to 15 to 22 cm with the conventional procedure. Both groups were virtually identical with respect to average blood loss (haemoglobin on 10th post-operative day: minimally invasive group, 108.0 g/L; conventional group, 112.0 g/L) and the duration of the procedure (minimally invasive group, 60 minutes; conventional group, 58 minutes). The position of the implanted components correlated with the pre-operative planning with regard to medial head offset, centre of rotation of the hip, and leg length, and was as satisfactory as that observed with the conventional procedure. The complication rate was low (2.9%). Shaft fissures occurred in the first months of use of the minimally invasive procedure before adaptation of the shaft rasps. Dislocations were attributable to improper patient behaviour. Minimally invasive surgery via the anterolateral approach in the supine position was equivalent to the conventional procedure, had a low rate of complications, and did not adversely impact the technical success of the procedure.
Introduction
Minimally invasive surgery (MIS) performed through the anterolateral approach potentially leads to a reduction in operative trauma through lower blood loss with a smaller soft tissue wound, a reduction in post-operative pain, and earlier mobilisation accomplished by preserving muscle insertions. Theoretically, these improvements should result in a shorter hospitalisation, convalescence, and rehabilitation period, as well as an enhanced cosmetic result through smaller skin incision and atraumatic wound closure. However, given the outstanding long-term results of total hip replacement performed via conventional surgical approaches, it is essential that any minimally invasive approach not lead to a reduction in the technical or long-term success of the procedure, including the post-operative position of the implanted components and restoration of the patient’s leg length, head offset, and centre of rotation.
With all of these requirements in mind, we have developed a minimally invasive approach to cementless hip replacement, based on the anterolateral Watson-Jones approach [1] with the patient in the supine position. To make this procedure minimally invasive, we have developed techniques to preserve the insertions of the gluteal muscles on the greater trochanter while allowing bony preparation and component placement via a smaller skin incision. In choosing this approach, our aim was to allow the surgeon to perform the procedure under direct vision using the usual anatomic landmarks for orientation, while maintaining the ability to revert to a conventional procedure by extending the skin incision. In order to optimize the outcome of procedures performed via this approach, we have also selected prosthetic components with proven clinical performance (Zweymüller SL-PLUS® stem and BICON-PLUS® threaded cup) in conventional hip replacement procedures [6].
Since September 2004, we have performed 350 primary total hip arthroplasties using our modified anterolateral Watson-Jones approach with the patient in the supine position, combined with instruments adapted to the requirements of minimally invasive arthroplasty. In this report, we describe the modifications to the operative technique that are necessary to enable this procedure to be performed with preservation of the pelvitrochanteric muscles and extension of the release of the hip capsule. We also present data collected from several cohorts of cases performed using this new approach in comparison with a conventional incision.
Material and methods
Based on a sample of 150 cases, our minimally invasive THR patients are predominantly female (64%), with an average age of 68 years (47–93 years). Diagnoses included idiopathic osteoarthritis (76%), osteoarthritis secondary to dysplasia (8%), femoral head necrosis (12%), osteoarthritis with protrusio (2%), and osteoarthritis after a previous hip fracture (2%).
Surgical procedure
The patient is placed supine on the normal table with the option of tilting the legs down. Both legs are prepped surgically and draped sterile. The contralateral leg is placed in an extended position, flexed about 20 degrees on a support (Fig. 1). The skin and subcutaneous tissue are opened through an oblique incision between the anterior superior iliac spine and the greater trochanter or, alternatively, through a straight incision made at the anterior border of the trochanter, 1/3 caudal and 2/3 cranial to the trochanter tip (Fig. 2). Though not the principal criterion of the minimal invasiveness of the procedure, the length of the skin incision is varied between 7 and 12 cm, depending on the build of the patient and the anticipated size of the implanted components. After splitting the iliotibial tract, the femoral neck is reached by blunt dissection between tensor fasciae latae and the anterior border of gluteus medius. The neck is grasped with two Hohmann hooks. After dissecting the fat pad off the anterior portion of the joint capsule, the curved rectus tendon is exposed and incised and an anterior hook is placed under the rectus and psoas tendon. After making a double door-shaped opening in the capsule (i.e., proximally along the rim of the acetabulum and distally), one removes the head-neck fragment in situ or after dislocation. With the leg in slight hyperextension, adduction, and external rotation, further capsule release is performed with preservation of the dorsal capsular structures and absolute sparing of the attachments of gluteus medius and minimus.
Fig. 1.
Extended contralateral leg flexed approximately 20 degrees on a support
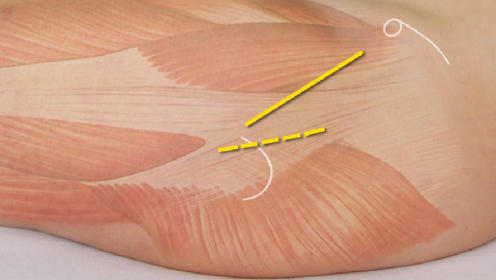
Fig. 2.
Incision area at the anterior border of the trochanter, 1/3 caudal and 2/3 cranial to the trochanter tip
After horizontally positioning the operating table, the surgeon exposes the acetabulum with three standard retractors. The acetabulum is reamed and the acetabular component is inserted using the conventional surgical technique. The surgeon must exercise caution at this step, as the pelvis position is altered after a difficult dislocation manoeuvre. After tilting the operating table again, the surgeon places the femur in adduction, external rotation, and hyperextension, and prepares the femoral shaft for implantation of the prosthesis using a box chisel, curette, reamer, luer forceps, and the offset manipulation rasps. After attaching the selected neck module and head, one performs a trial reduction, test of stability, and check of length. This is followed by implantation of the prosthetic component, grafting of the proximal stem-bone interface with cancellous bone, reduction of the prosthetic joint, insertion of drains, and closure of the wound with intracutaneous sutures.
Data collection and analysis
The impact of the surgical approach on blood loss, the duration of the operative procedure, and the length of skin incision were examined by collecting data from 100 hip replacement cases all performed by the senior surgeon (G.P.) using the minimally invasive and the conventional techniques. Data from the first 50 consecutive MIS cases operated in 2004 were compared with 50 consecutive THR procedures performed in 2003 using a conventional Watson-Jones approach [5]. During the recruitment period in 2003, the Watson-Jones approach was exclusively used for all patients undergoing primary THR while later in 2004, all patients were operated with the MIS technique.
We also performed a radiographic analysis of the first 150 consecutive MIS cases to assess the effect of the procedure on leg length, medial head offset, and the centre of rotation of the hip. The position of the femoral and acetabular components was measured on the first post-operative radiograph and compared to the pre-operative plan for each arthroplasty. All complications were collated through examination of operative and medical records. In 28 minimally invasive THR patients, a hip replacement had been previously performed on the contralateral side using the conventional method. A structured questionnaire, which examined the outcome of both the minimally invasive and conventional procedures, was administered to each of these patients via telephone by an independent expert.
To assess the prevalence of complications associated with the minimally invasive anterolateral approach, we also examined data collected from all 350 cases performed since we commenced using this approach in September 2004.
All statistical analyses were undertaken with the open source software for statistical computing and graphics R [4]. Shapiro-Wilk’s test of normality was performed for distribution of continuous variables. Normally distributed data were then compared with unpaired t-tests and Mann-Whitney’s tests were used for other distributions. A chi-square test or a test of proportions was used to compare categorical data, such as blood transfusion status or implant positioning.
Results
Comparison of 50 MIS and 50 conventional patients
Blood loss
The pre-operative haemoglobin and hematocrit values did not differ significantly between the groups nor did the values measured on the 10th post-operative day (Table 1). Fifty-eight percent of patients in the MIS group did not require a blood transfusion, compared to 62% in the conventional group (p = 0.34). The prevalence of autologous blood transfusion was virtually the same in both groups (p > 0.99) (Table 2).
Table 1.
Comparison of blood loss
| MIS ( = 50) | Conventional ( = 50) | -value | ||
|---|---|---|---|---|
| Pre-op | Hct | ∅ 41.4% | ∅ 41.6% | 0.35 |
| Hb | ∅ 135.0 g/L | ∅ 137.0 g/L | 0.39 | |
| Day 10 post-op | Hct | ∅ 33.5% | ∅ 34.5% | 0.06 |
| Hb | ∅ 108.0 g/L | ∅ 112.0 g/L | 0.09 | |
Hct=Hematocrit
Hb=Hemoglobin
Table 2.
Comparison of autologous and donor blood transfusion
| MIS ( = 50) | Conventional ( = 50) | |||
|---|---|---|---|---|
| None | 29 | 58% | 31 | 62% |
| 1 unit | 3 | 6% | 6 | 12% |
| 2 units | 6 | 12% | 4 | 8% |
| 3 units | 0 | 0% | 1 | 2% |
| 1 autologous unit | 3 | 6% | 3 | 6% |
| 2 autologous units | 9 | 18% | 5 | 10% |
Surgery duration and length of skin incision
The duration of the operative procedure, measured from incision to suture was similar in both groups (median values: MIS group: 58 minutes; conventional group: 56 minutes; p = 0.12). The skin incision was approximately twice as long in the conventionally operated group (median: 17.5 cm; range:15 to 22 cm), compared to the MIS group (median: 8.0 cm; range: 7 to 12 cm). This difference was statistically significant (p < 0.01).
Analysis of the post-operative radiographs (n = 150)
No differences were identified between the position or alignment of components implanted using the MIS and conventional techniques. In 90% of the MIS cases analysed, the difference in radiographic leg length of the operated and contralateral extremities was less than 4 mm, in keeping with pre-operative planning. In the remaining 10%, the difference in leg length was between 4 and 7 mm. The planned offset was achieved in 93% of cases (reconstruction within ± 3 mm), and the difference in the remaining 7% was between minus and plus 1 cm.
In terms of stem alignment, stem sizing, and axial position, there were no statistically significant differences between the MIS group and previous published series in which the same prosthesis was implanted via conventional incisions (p = 0.74) [2, 3, 6, 7]. In the MIS group, the stem was placed in the correct axial position in 83% of cases vs. 82% of the conventional group. Nine percent of stems in the MIS group were undersized by one size, vs. 12% of the published group. Eight percent of the MIS stems were slightly misaligned (valgus: 3, varus:5%), compared to 6% of the conventional group (valgus:1%, varus:5%).
Complications
Ten complications (2.9%) were observed in the entire clinical series of 350 cases performed via the minimal incision approach. Four shaft fissures occurred early in the development of the technique and led us to recommend routine capsular release, and when necessary, additional incision of the piriformis tendon. We also modified the femoral rasps through the incorporation of an offset drive shaft. Four dislocations occurred after these procedures and were all associated with failure of the patient to follow post-operative precautions (sitting on a low seat, alcohol use, walking, and a fall). None required reoperation. There was also one early infection and one trochanteric fracture after a fall.
Subjective patient assessment
Twenty-eight bilateral patients were asked to give their subjective impressions of their post-operative experiences after THR (Table 3). Each of these patients had undergone conventional hip arthroplasty prior to a minimally invasive procedure. Patients reported a clear preference for the procedure performed via the minimally invasive approach compared to conventional surgery and reported a significant improvement in post-operative pain, post-operative mobility, and scarring (p < 0.01).
Table 3.
Results of patient survey ( = 28)
| Applies to minimally invasive operation/conventional operation: | MIS | CONV. | The same | Don‘t know |
|---|---|---|---|---|
| Less post-op pain | 57.1% | 7.1% | 32.1% | 3.6% |
| Easier to stand up on first post-op day | 78.6% | 3.6% | 14.3% | 3.6% |
| Less help needed during the first days | 57.1% | 0.0% | 35.7% | 7.1% |
| Walking sooner without crutches | 75.0% | 7.1% | 3.6% | 14.3% |
| Easier stair climbing | 67.9% | 10.7% | 10.7% | 10.7% |
| Shorter scar | 96.4% | 0.0% | 3.6% | 0.0% |
| Preferred operation method | 78.6% | 3.6% | 3.6% | 14.3% |
Discussion
For a hip replacement procedure to be truly “minimally invasive”, it is not necessary to perform the operation via the smallest possible skin incision, but it is essential that the procedure be performed with minimal soft-tissue trauma, sparing all muscle attachments. In the case of the anterolateral approach, this means preservation of the anterior parts of the attachment of the gluteus medius and the minimus tendon. The trend to operate as atraumatically as possible in hip surgery also continues the experience gained in arthroscopic and laparoscopic techniques. Tissue structures that are not divided cannot cause the patient pain. On the other hand, over-stretched soft tissues can very well cause pain and delay healing. Consequently, the optimal soft tissue sparing incision for total hip replacement balances the desire to minimize the size of the entry portal with the need to provide the required intraoperative view and atraumatic access to the femur and acetabulum.
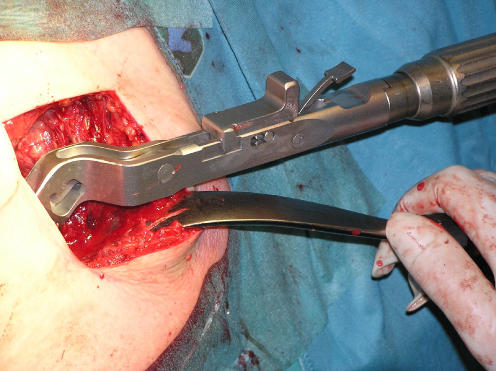
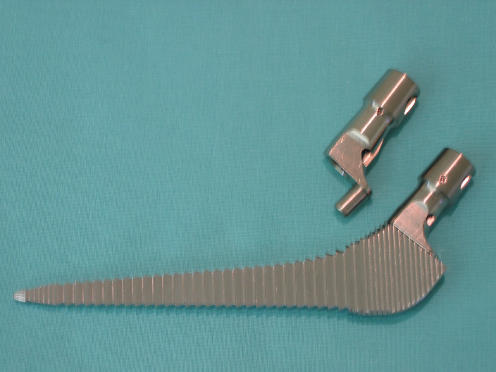
Our experience with the development of minimally invasive approaches to hip replacement has taught us that several key considerations facilitate these procedures and minimize complications. Correct instrumentation is critical. Whereas the acetabular cup can be implanted with standard instruments, specialized rasps with double offset shafts have proved particularly helpful in preparing the femur. These instruments enable the surgeon to gain access to the canal without impinging upon the skin outside the wound (Fig. 3). Manipulation rasps with modular necks have also been developed to replace the trial components and substantially facilitate the procedure (Fig. 4).
Fig. 3.
Novel rasp with double offset
Fig. 4.
Manipulation rasp with modular neck
Additional measures are necessary to allow mobilization of the femur to provide access to the acetabulum. Extended release of the hip capsule and partial dissection of the rectus tendon are essential for tension-free adjustment of the acetabular cup, particularly when using a threaded device. Additional incision of the piriformis tendon may also be necessary to allow sufficient mobilization of the femur for canal preparation and stem insertion. Moreover, during shaft preparation, manipulations must be checked carefully to avoid malpositioning of the cup. The soft tissues must not deflect the rasps upon entry into the femur, to prevent perforation of the dorsal cortex. Right-left lateral offset rasps can be helpful in avoiding this problem.
The results of our study show that the use of the minimally invasive anterolateral approach has no effect on the position or the alignment of the prosthetic components. Similarly, in comparison with conventional cementless hip replacement procedures, there is no change in haemoglobin and hematocrit levels, or the need for blood transfusion. In this series, one third of patients in each treatment group required transfusion. It should be noted that, in Austria, the gold standard of thromboembolic prophylaxis consists of low-molecular-weight heparin, and treatment with fondaparinux sodium (Arixtra) is given to high-risk patients. Aspirin or warfarin therapy in combination with pneumatic vein pumps is not customary.
In principle, every case of primary osteoarthritis is amenable to the minimally invasive approach that we have presented. However, the minimally invasive operative technique makes higher demands on the experience and skill of the surgeon. The presence of severe hip dislocation, a failed acetabular component from previous hip replacement, destructive rheumatoid arthritis, multiple previous operations on the joint, and major leg length differences all represent relative contraindications of the minimally invasive approach. Nonetheless, when correctly performed, the minimally invasive approach provides the patient with a functional result on discharge similar to that obtained 6 weeks after convention surgery. Gluteal insufficiency or dehiscence, which can be observed with the transgluteal or conventional Watson-Jones approach, is eliminated by preserving the muscle attachments. The design of conventional prostheses necessitates invasion of the bone within the greater trochanter to allow neutral stem placement. Moreover, the entry curve of conventional rasps may endanger the gluteal muscle fibres, especially in cases of coxa vara. It is anticipated that, in the future, changes in implants may solve these problems while still maintaining the proven diaphyseal anchorage of established implant designs.
Acknowledgements
The authors have not received any funding related to this study. No potential conflicts of interest are declared.
References
- 1.Bertin KC, Röttinger H (2004) Anterolateral mini-incision hip replacement surgery. A modified Watson-Jones approach. Clin Orthop Relat Res 429:248–255 [DOI] [PubMed]
- 2.Grübl A, Chiari C, Gruber M, Kaider A, Gottsauner-Wolf F (2002) Cementless total hip arthroplasty with a tapered, rectangular titanium stem and a threaded cup. A minimum ten-year follow-up. J Bone Joint Surg 84:425–431 [DOI] [PubMed]
- 3.Pflüger G, Junk-Jantsch S, Schöll V, Mösslacher I (2005) Results of a 10-Year Follow-Up Study of Hip Replacements with SL-Plus Stem, Radiological Findings. Abstract Book, 35th Annual Meeting, Japanese Society for Replacement Arthroplasty, Okinawa, Feb. 3–4
- 4.R Development Core Team (2006) R: A Language and Environment for Statistical Computing, Vienna, Austria: R Foundation for Statistical Computing
- 5.Watson-Jones R (1936) Fractures of the neck of the femur. Br J Surg 23:787–808 [DOI]
- 6.Zenz P, Pospisil C, Fertschak W, Schwägerl W (1995) 10 years of cementless implantation of total hip endoprosthesis using Zweymuller’s stem. Z Orthop Ihre Grenzgeb 133:558–561 [DOI] [PubMed]
- 7.Zweymüller K (1990) Radiologische Grundphänomene des Titan-Geradschaftes. In: Zweymüller K (ed) 10 Jahre Zweymüllerhüftendoprothese. Hans Huber, Bern, Stuttgart, Toronto, pp 23–34