Abstract
Implantation of the total hip prosthesis should always be as atraumatic as possible. The principle underlying this technique is to visualise the working area while keeping the aperture to a minimum, with a resulting reduction in trauma to the soft tissue. We present a new, improved single-incision approach in total hip arthroplasty: the mini-posterior approach. Preliminary results from 60 patients operated using this approach indicate rapid functional recovery, minimal postoperative pain, a reduced duration of hospitalisation, few complications, and optimal component positioning. Further follow-up is warranted.
Introduction
The most widely used approaches for total hip arthroplasty (THA) are the posterior, anterior, direct lateral, and anterolateral approaches. The anterolateral approach is said to be more resistant to dislocation, but partial detachment of the gluteus medius and minimus at their insertions at the greater trochanter is associated with postoperative limp and abductor dysfunction [1, 3, 5].
Biomechanical notions are in a constant process of evolution. One such recent evolution is the adjustment from an optimised, classical posterolateral surgical approach to a genuine mini-posterior approach. Although the difference between these approaches may appear relatively minor, the impact on clinical outcome may well be much more significant. The use of a standard posterior approach is associated with a low rate of dislocation, a low incidence of limp, and an excellent overall functional outcome when performed with a capsular repair. The primary difference between the mini-incision and the standard posterior approach is the elimination of numerous instruments that obscure the operative field and inevitably place tension on the delicate structures, which in turn increases the risk of neurological and soft-tissue complications.
This paper provides an overview of the mini-posterior technique as applied in our clinic and provides preliminary early results demonstrating its safety and efficacy.
Materials and methods
Between January 2002 and January 2004, 60 primary total hip replacements were performed using the mini-posterior approach. During this period, we implemented conservative criteria for patient selection. Patients who were over 70 years of age, had a body mass index (BMI) >30, were inactive, or had severe comorbidities (cardiovascular, diabetes, neurological) were excluded from this procedure. All patients received a tapered, titanium cementless femoral component, the SL-Plus (Plus Orthopedics AG, Rotkreuz, Switzerland). This implant design was selected because of its versatility and its ability to provide secure axial positioning through its tapered rectilinear design. In addition, this implant system gives the surgeon a wide variety of technical and reconstructive options, which the author has found to be clinically valuable. All procedures were performed with the implantation of a cementless, press-fit acetabular shell (EP-FIT, Plus Orthopedics AG).
Proper positioning of the patient on the operating table is fundamentally important when employing the mini-incision posterior approach. Study participants were all placed in a lateral decubitus position with the pelvis fully supported and perpendicular to the operating table. The route of the mini-posterior approach is essentially located under the gluteus medius muscle. The incision was made 2 cm posterior to the greater trochanter and at approximately 20° to the shaft of the femur using the reference markers formalised by Swanson [4]. The incision length varied between 5–6 cm (Fig. 1).
Fig. 1.
Correct placement of the pelvis: KEY for positioning acetabulum component placement of the incision
The tissues were incised subcutaneously. The fibres of the gluteus maximus muscle were split in line, thus sparing them from trauma. A Hohmann retractor was then placed under the gluteal musculature, followed by dissection of the fatty layer over the short rotators. The short external rotators were exposed by internally rotating the hip to achieve maximum resistance. The piriformis tendon was preserved intact, except in cases of coxa vara where it was detached at its femoral insertion to provide adequate mobilisation of the femur. Because the lateral circumflex artery is protected by the quadratus femoris muscle, it can remain intact if the approach is kept very proximal. We preferred to ligate the artery to prevent secondary bleeding when it was visualised or slightly traumatised.
The short external rotators and the posterior capsule were taken down as a flap to protect the sciatic nerve in the manner described by Dixon et al. [2] (Fig. 2). After femoral dislocation, a threaded pin from an external fixator was inserted into the femoral head and an osteotomy of the femoral neck was performed. This allowed the head to be extracted from the hip en bloc. Satisfactory visualisation was achieved through the use of fewer retractors than would have been necessary with a conventional technique (Fig. 3). Two Steinmann pins were placed on the posterior column; one distally in the postero-inferior iliac spine and the other in the middle of the column through the posterior capsular flap so as to keep it out of the way during reaming. A third pin was placed above the acetabulum in order to separate the capsula and suprajacent muscles. A Hohmann retractor was placed adjacent to the anterior column to maintain anterior femoral dislocation while the leg remained flat on the operating table.
Fig. 2.
The sciatic nerve is protected by a capsulo-tendinous flap
Fig. 3.
Good visualisation using fewer retractors
When preparing the socket, it is important to excise the osteophytes and inflammatory, hypertrophic, and retractile capsular zones, to facilitate correct visualisation of the true acetabular margin and correct implantation of the acetabular cup. Acetabular exposure was achieved with the proper placement of retractors and did not require tensioning the skin or other soft tissue.
Certain tools prove indispensable when using the mini-posterior approach, most notably the offset acetabular reamer, which minimises the forces applied to the access channel in order to obtain correct alignment of the reamer during acetabular preparation.
When the acetabular reaming has exposed bleeding subchondral bone, the acetabular component is implanted using a curve impactor. This instrument allows the cup to be positioned in the correct orientation, without pressing on the wound edges or on the femur.
In order to provide adequate exposure to the proximal femur, the limb is repositioned with the knee flexed to 90° with the tibia vertical. This position serves as the reference for the stem orientation. A lip retractor is placed under the neck to elevate the femur, and a small Hohmann retractor is inserted under the gluteus medius muscle to provide unobstructed access to the femur at the trochanteric level. The femur is prepared in the conventional manner: the canal is opened with a trochanteric punch, and rasps of incremental size are passed down the canal. Particular attention is paid to placement and alignment of the smallest rasp, which is inserted as laterally as possible against the medial border of the greater trochanter. When the largest rasp is correctly positioned, tests are performed using components with different neck lengths and offsets; the stability and the length of the limb are estimated by another knee palpation (starting reference). All retractors are removed in order to facilitate testing and liberate soft tissues. Once the trial components have been removed, the definitive components are implanted using the basic principle of retraction and tissue preservation.
After achieving femoral reduction, the tendinous-capsular flap is often spontaneously re-positioned. In those cases where the piriformis tendon was preserved, the soft-tissue restraints of the hip are reconstructed using the capsular noose technique described by Swanson [4]. This technique allows for closure of soft tissues around the implant, resulting in a stable capsular sleeve. If a capsulotendinous flap was created, it was repositioned under the major trochanter and sutured beneath the tendon of the gluteus medius to provide a posterior barrier against dislocation. This was followed by successive layered closure with resorbable sutures. A drain was inserted for a time period usually lasting 24 h. Postoperative pain was controlled with intravenous analgesics for 24 to 48 h with perfusions that combined Prodafalgan and Ketoprofene and second-line oral analgesics (e.g., paracetamol and codeine) in the following days. Deep venous thrombosis prophylaxis was given via low-molecular-weight heparin administrated pre- and post-operatively for 5 weeks.
Physical therapy, with the use of continuous passive motion, was initiated on the 1st postoperative day. Patients were allowed to attempt full weight bearing from day 1 if tolerated and depending on pain status and muscular recovery. Patients were instructed to prevent motions that could provoke dislocation for the first 4 weeks.
Results
Sixty patients (21 male, 39 female) of average age 63.5 years (range: 41–70 years) took part in the study. The average BMI was 26.5 kg/m2. Indications for THA were primary osteoarthritis in 39 patients, dysplasia of the hip in 15 patients, and avascular necrosis in 6 patients. The average duration of the operative procedure (skin-to-skin) was 53 min (range: 40–70 min). The total hospitalisation period was 5–7 days, which varied with the patients’ age and physical condition.
Intra- and postoperative complications were rare. No major adverse events occurred. Intraoperatively, there were no incidents of cracking of the femur or neuro-vascular injuries. No postoperative dislocations occurred. There were no haematomas, and transfusions were not required. Sepsis was not observed in any patient, although one patient had a wound complication consisting of a single localised area of superficial necrosis that did not require surgical treatment. No discrepancies in leg length were noted.
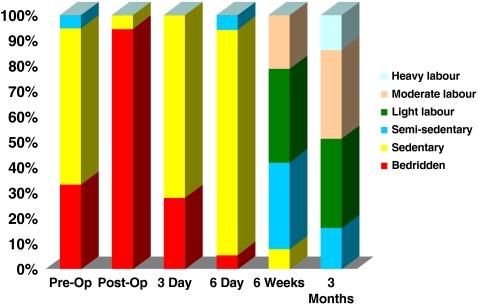
Postoperative care appeared to be enhanced through early mobilisation from day 0 on full weight-bearing. In most cases, full ambulation was achieved after the 3rd day postoperatively. On average, patients were able to rise from a chair without using the hands after 3 days and climb stairs at 5 days. Patients were released from the hospital after an average of 4 days. Basic home mobility was regained in 80% of the patients on day 6. Basic home activities could be performed on day 15 and light work on day 30 (Fig. 4). The patients were able to discard their walking aids after an average of 12 days.
Fig. 4.
Level of activity
Radiographic analysis revealed no problems associated with the stem and no cases of varisation exceeding 3°. The medium acetabular inclination angle was 40°, ranging from 35° to 50°. No components were observed to be in retroversion.
After 1 year, standard AP and lateral radiographs revealed evidence of osseointegration of the stem without abnormal radiolucent lines. Leg length discrepancy, as measured by radiographs, did not exceed 7 mm in any patient.
Discussion
In this author’s experience, the mini-posterior approach used resulted in no significant complications, and, in comparison with the previously used standard posterolateral approach, provided encouraging postoperative pain relief and faster recovery. We attribute this to the reduced trauma necessitated by the surgical technique. The procedure minimises soft tissue trauma by using the smallest incision required to ensure satisfactory visualisation. The hospitalisation period was short and the postoperative care was reduced to a strict minimum. The patients experienced a quick recovery, with a swift return to normal daily function. Additionally, the enhanced aesthetic value of a smaller incision and reduced rehabilitation time required with this approach appeared to work in tandem to rapidly restore patient well-being.
The mini-posterior approach is a simple, planned technique that imposes less stress on the surgical team and delivers quantifiable and predictable results. The results of this series support the conclusions of Swanson [4], who demonstrated satisfactory results in a cohort of 1,000 consecutive patients using a posterior, single-incision, minimally invasive approach. Surgical time, blood loss, length of hospitalisation, and recovery time in our series were all favourable. We have found similarly favourable results with our approach.
It is important to note that the mini-incision approach is not suitable for procedures such revision hip surgery, as these usually require a much wider exposure. Patient size may also be a limiting factor, as reaching the deep structures through a mini incision can be very difficult in an obese or muscular patient. For this reason, it is recommend that the length of the incision be adjusted to compensate for the increased tissue bulk of larger patients, and in this regard, a good rule of thumb appears to be Swanson’s recommendation that the incision length in centimetres equal the patient’s BMI divided by 3 [4]. The author’s experience with minimally invasive approaches to total hip replacement have shown that training and experience are both crucial to success, and the surgical team must go through an initial learning phase. Conservative patient selection is recommended when starting with this procedure.
Conclusion
THA has remained an effective treatment for all patients with classic cases of osteoarthritis or other destructive conditions of the hip. A basic principle of surgery is that interventions should be as atraumatic as possible. With the mini-posterior approach, the prosthesis is placed through an incision that measures just a few centimetres in length, but which still provides perfect visualisation of the surgical site while reducing trauma to the soft tissue.
The visualisation of the acetabulum poses no particular problem and its positioning is reliable and validated on postoperative control radiographs. All radiographs in our study showed a well-positioned acetabulum with a good anteversion. Working in the femoral axis when implanting the stem is easily achievable under visual control and eliminates the risk of taking a false route or of significant malalignment of the implant. In the event of an intraoperative incident, the approach can always be enlarged without traumatising sensitive structures or causing excessive sacrifice of muscle.
The mini-posterior, single-incision approach represents an easy, planned, less hazardous, and predictive pathway in THA. Future comparisons of this approach with conventional methods of THA are warranted.
Acknowledgements
The author did not receive grants or outside funding in support of preparation of this manuscript. He did not receive payments or other benefits or a commitment or agreement to provide such benefits from a commercial entity. No commercial entity paid or directed, or agreed to pay or direct, any benefits to any research fund, foundation, education institution, or other charitable or non-profit organisation with which the author is affiliated or associated.
References
- 1.Baker AS, Bitounis VC (1985) Abductor function after total hip replacement: an electromyographic and clinical review. J Bone Joint Surg 71B:47–50 [DOI] [PubMed]
- 2.Dixon MC, Scott RD, Shai PA, Stamos V (2004) A simple capsulorrhapy in a posterior approach for total hip arthroplasty. J Arthroplasty 19:373–376 [DOI] [PubMed]
- 3.Horwitz BR, Rockowitz NL, Goll SR et al (1993) A prospective randomized comparison of two surgical approaches to total hip arthroplasty. Clin Orthop 291:154–163 [PubMed]
- 4.Swanson TV (2005) Early results of 1000 consecutive, posterior, single-incision minimally invasive surgery total hip arthroplasties. J Arthroplasty 20(7 Suppl 3):26–32 [DOI] [PubMed]
- 5.Vicar AJ, Coleman CR (1984) A comparison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop 188:152–159 [PubMed]