Abstract
Arthropathy of the hip is moderate in frequency in haemophiliac patients, but is less common than ankle, knee or elbow arthropathy. We report about our experience with total hip replacement in patients with severe bleeding disorders over a period of 30 years. Between July 1972 and 2002, 15 hips in 13 patients were replaced. The main bleeding disorders were Haemophilia A in ten patients and severe v. Willebrand disease in three patients. The mean follow-up was 132 months (range 12–363). We can demonstrate good long-term results, with only one aseptic loosening after 14 years and one septic loosening after 14 months in an HIV-positive patient. The Harris Hip Score increased from 48 points (32–66) preoperatively to 89 (76–100) postoperatively. In conclusion, total hip replacement performed in a specialised haemophiliac centre is a safe procedure, and results in pain relief and improvement of the quality of life in patients with severe bleeding disorders.
Résumé
Les lésions de hanche sont peu fréquentes chez les patients hémophiliques et de toute façon moins fréquente que les lésions de la cheville, du genou ou de l’épaule. Nous rapportons notre expérience du remplacement par une prothèse totale chez des patients représentant des troubles sévères de la coagulation sur une période de 30 ans. De juillet 1972 à ce jour, 15 hanches chez 13 patients ont été remplacées. Le trouble de la coagulation le plus fréquent a été l’hémophilie A, chez 10 patients et une maladie de Willebrand sévère chez 3 patients. Le suivi moyen a été de 132 mois (12 à 363). Résultats : cette étude montre un bon résultat à long terme de ces remplacements avec simplement un descellement aseptique après14 ans et un descellement septique après 14 mois chez un patient HIV+. Le score de Harris s’est amélioré de 48 en préopératoire (32 à 66) à 89 points en postopératoire (76 à 100). En conclusion, la prothèse totale de hanche réalisée dans un centre spécialisé de traitement des hémophiles est un procédé sûr, les résultats sur la douleur et l’amélioration de la qualité de vie sont importants chez ces patients présentant de graves troubles de la coagulation.
Introduction
End-stage haemophiliac arthropathy is associated with loss of function and impaired quality of life. In childhood, rapidly progressive severe arthropathy of the hip may result from a single haemarthrosis causing increased intracapsular pressure, which may lead to an osteonecrosis of the capital femoral epiphysis. More often, hip arthrosis is the result of chronic synovitis similar to that which occurs in other joints. Between the second and fourth decade, many haemophiliac patients develop severe articular destruction. In all stages, conservative treatment of the affected joints and prophylactic treatment comes to the fore. Only in cases of ineffective conservative treatment over 3–6 months can synovectomy of the affected joint be considered. At later stages with pronounced joint contractures, possible treatments include arthrodesis and arthroplasty. For the hip, arthroplasty is the option of choice and remains the best solution [8, 11, 19].
Arthropathy of the hip is moderate in frequency but is less common than arthropathy of the knee or ankle joint. In addition to thorough preoperative medical preparation of the patient, considerable surgical preparation is required. Depending on the age of the onset of significant bleeding, the proximal anatomy of the femur can be distorted and, in the most severe cases, there can be an extremely small femoral medullary canal, valgus and excessive anteversion of the head and neck, together with protrusion of the acetabulum. Due to the sometimes severe contracture and extensive fibrosis, a muscular release may be required to achieve an adequate range of motion postoperatively. The bone stock is almost always of poor quality.
In this retrospective analysis, we report on our experience with total joint replacement of the hip in patients with severe bleeding disorders. Of interest were survival of the implants, complications, and the functional outcome.
Materials and methods
Between July 1972 and 2002, 15 total hip replacements in 13 patients were performed at our institute. The main bleeding disorders were major Haemophilia A in 10 patients and severe v. Willebrand disease in 3 patients. None of the patients had haemophilia with inhibitors. The mean age of the patients was 42 years of age (32–67), and the mean follow-up time was 132 months (12–363). Indication for total hip replacement was satisfied when two of the following five criteria were fulfilled: (1) Arthropathy stages IV or V [1], (2) rapid progress of the radiographic signs of joint destruction (Petterson-score >6) [18], (3) increasing contractures of the joint >15° (WFH-joint-score), (4) severe disabling pain, and (5) recurrent irritation of the joint with or without intraarticular bleeding. Although the knees of these patients showed radiological findings of haemarthrosis, the leading symptom was the pain in the hip. If knee function is unsatisfactory the knee joint should be replaced before the hip, although this was not necessary in our series. Whereas at the start only cemented implants were used, we changed our procedure to hybrid total hip replacement, with a non-cemented cup and a cemented stem, and later, cementless total hip replacement. In the retrospective analysis the charts of the patients were evaluated for complications during surgery, blood loss, early complications after surgery, survival of the implants, cases of revision surgery, and infection. To determine the functional outcome the Harris Hip Score was applied for the time before surgery. At follow-up examination the Harris Hip Score and the Charnley Score were applied [4, 9]. The patients were seen at least once a year and in addition to X-rays a complete functional check was carried out.
Results
No perioperative complications such as extensive bleeding were documented. The main blood loss did not exceed the normal distribution curve compared to patients without bleeding disorders. The replacement rate of the factors was 100%. Factor substitution in patients with haemophilia was adjusted according to the concentration of factor VIII in the blood and to the postoperative findings after an initial loading dose. Substitution lasted until wound healing. We only saw one patient with loosening of the cemented cup after 14 years. In one HIV-positive patient, septic loosening was seen 14 years after the implantation of a total hip prosthesis. A second HIV-positive patient developed a Candida-infection of the skin and soft tissue, without involvement of the prosthesis 5 months postoperatively. These patients died 7 and 5 years respectively after their HIV-related infections, without any further complications related to the implanted total hip prosthesis. Another patient died 31 years after primary and 17 years after revision surgery, but not due to any complication of the hip. The remaining patients are still alive. There were no further signs of infections in the remaining patients. The survival rate after a median time of 11 years was 86.7%. The postoperative movement as the sum of the three standard directions showed an improvement from 90° (mean) preoperatively to 189.6° (mean) postoperatively. This result expresses an improvement from 2.9 to 4.6 points in the Charnley Score. The subjective assessment of pain in particular showed an improvement, from 2.0 to 5.4 points. The subjective assessment of mobility showed an improvement from 2.0 to 4.6 points. The Harris Hip Score increased remarkably from 48 points (32–66) preoperatively to 89 (76–100) postoperatively. Based on the classification, excellent results were found in 72% of cases, fair results in 19% and bad results in 9%.
Case report
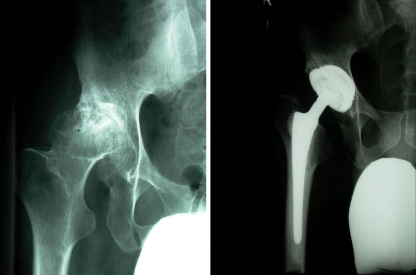
In July 1972 the first total hip arthroplasty in a patient with advanced haemophiliac arthropathy was performed at our institution. The patient presented with severe pain and reported overuse of analgesics which led, due to its toxicity, to cirrhosis of the liver and compensated renal insufficiency. Though the risks of an elective major surgical procedure could not be overlooked at this time, the relatives and the patient pushed for a surgical treatment. The patient even threatened to commit suicide. Under appropriate haemostasis a cemented total hip prosthesis was implanted. Fourteen years later, in 1986, the cemented cup had to be revised due to an aseptic loosening. (see Fig. 1) In 2004, the patient died without any recurrent signs of loosening.
Fig. 1.

Revised acetabular component in a cemented hip arthroplasty
Discussion
Haemophiliac arthropathy develops after recurrent intra-articular bleeding. Prophylactic replacement factor treatment, which has to start in early childhood, reduces the severity of spontaneous bleeding significantly [1, 7, 20] and can prevent or at least delay joint destruction [5]. The development of purified clotting factor concentrates, and the increased use of radiosynovectomy are two factors in current improvements in treatment leading to a significant reduction of the frequency of haemarthrosis [15]. Teitelbaum reviewed pelvic radiographs of 34 patients complaining of pain in the hip (64 hips) from a population of 175 patients seen at one haemophilia centre. Sixteen of 20 hips that had an open proximal femoral epiphysis had a valgus deformity, but none had osteoarthritic changes. Fifteen of 48 skeletally mature hips had degenerative changes, including protrusion of the acetabulum in eight hips [23].
The sample-size in our study represents the few patients in which a total hip replacement was necessary. Even the larger studies in literature only report on 13 patients in 20 years [15] and 39 patients in 16 years [17]. Kelley et al. reported in a multicentre trial on 34 hip arthroplasties in 28 years [12]. Total hip arthroplasty is less common than total knee arthroplasty [2, 16]. The first reported arthroplasty of the hip in a haemophiliac patient was in 1967. Bellingham et al. reported on a 21-year-old man who underwent arthroplastic surgery after a non-union of a femoral neck fracture [3]. The first important series was published by Luck and Kasper in 1989 announcing that the first prosthetic arthrosplasty of the hip in a haemophiliac in the United States was performed in 1968 [15]. Further studies by Nelson in 1992, Löfquist in 1996 and Kelley in 1995 report on 39 in 38, 13 in 11, and 34 in 27 patients respectively [12, 14, 17]. According to the literature the first total hip replacement in haemophiliac arthropathy in Europe was performed at our centre in 1972.
The septic loosening as well as the Candida-infection of the skin and soft tissue in HIV-positive patients in our study, are reflected in the literature. Haematological and technical problems were held responsible for this high rate of complications. Earlier studies from several haemophilia centres suggest that between 33% and 92% of patients with haemophilia B carry the HIV antibody [22]. In 2004, Luck et al. assumed that the high incidence of late infection may be related to frequent intravenous self-infusion of clotting factor combined with immune suppression [16]. Whereas we could only report one septic and two aseptic loosenings (20%), Luck et al. revised 60% of their hip replacements of whom were 33% septic loosenings. Eight of their patients required revision, and one required an excision arthroplasty [15, 16]. Löfquist et al. saw a loosening rate of 38%. They reported in 1996 on six aseptic revisions and two septic revisions out of 13 total hip arthroplasties in patients who were also seropositive for HIV [14]. In a multi-centre trial, Kelley et al. saw aseptic revisions of the cup in 23% of cases, and of the femoral stem in 21%. Nelson et al. noticed a revision rate of 36.4% after 7.6 years (mean), which mainly affected the femoral stem, and a loosening rate of 65%. After studying the influence of HIV, they concluded that although they advise caution when total hip arthroplasty is considered in patients with HIV, total hip arthroplasty has a continuing role in the treatment of haemophiliac arthropathy in patients with severe pain and disability. From their point of view, seropositive patients without AIDS have a postoperative complication risk similar to that for the general population [12, 17].
Since 1972 we have seen some excellent results after total hip replacement with good long-term results, as demonstrated by the Charnley Score and the Harris Hip Score. This confirms statements in literature concerning a significant increase in the quality of life after total hip arthroplasty—with or without haemophilia—though the functional results in haemophiliac patients did not reach the same level as that in the corresponding population without haemophilia [6, 10, 16, 21].
Whilst we used a cemented prosthesis in our early patients, we went on to implant hybrid total endoprostheses with a cemented stem and cementless cup. This reflects the development in total hip arthroplasty and its possibilities, which we were able to transfer to our haemophiliac patients without an increase of complications [13].
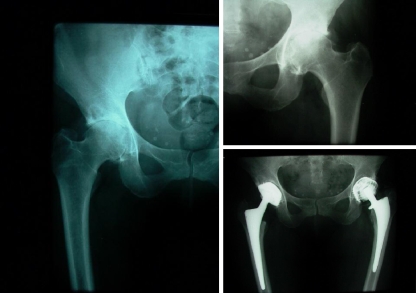
We conclude, that after more than 30 years of experience with total hip arthroplasty in haemophiliac patients, and based on our positive results for advanced severe haemophiliac hip arthropathy, replacement of the joint leads to a relief of pain, improved function and an increase in the quality of life. Despite F VIII prophylaxis leading to better joint surfaces in haemophiliac patients, this group of patients will get older; and since arthritis of the hip is an increasing problem in the older generation, they will be in need of total joint replacement. Regardless of haemophiliac arthropathy, the patients will develop hip and knee arthritis, and the need for surgery will increase. Thus, total hip replacement should be considered regardless of the age of the patient, and the surgical intervention should be performed in specialised centres with experience in the treatment of bleeding disorders. Hip replacement in haemophiliac patients should be performed using implants which have been proved to have a long survival rate in the specific centre. Though some authors have seen a higher complication rate in cementless implants due to the haematological disease, we did not see any septic or aseptic loosening in those patients. Close interdisciplinary co-operation with a team of heamatologists is essential for successful treatment of these patients. In our opinion the control of the bleeding disorder combined with the surgical technique is the reason for a high success rate (Figs. 2 and 3).
Fig. 2.
Hybrid total hip arthroplasty in a patient with Haemophilia A
Fig. 3.
Bilateral cementless hip arthropathy in a patient with Haemophilia A
References
- 1.Arnold WD, Hilgartner MW (1977) Hemophilic arthropathy. J Bone Joint Surg Am 59:287–305 [PubMed]
- 2.Beeton K, Rodriguez-Merchan EC, Alltree J (2000) Total joint arthroplasty in haemophilia. Haemophilia 6:474–481 [DOI] [PubMed]
- 3.Bellingham A, fletcher D, Kirwan E, Prankerd T, Cleghorn T (1967) Hip arthroplasty in a haemophiliac and subsequent prophylactic therapy with cryoprecipitate. BMJ 4:531–532 [DOI] [PMC free article] [PubMed]
- 4.Charnley J (1972) The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br 54:61–76 [PubMed]
- 5.Dzinaj T, Funk M, Schmidt H, Böttger S, Güngör T, Klarmann D, Kreuz W (1996) Radiological score in paediatic haemophilic patients with early and late onset of factor VIII-prophylaxis. Thromb Haemost 76:630–631 [PubMed]
- 6.Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY (2004) Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 86(5):963–974, May [DOI] [PubMed]
- 7.Fernández-Palazzi F, Rivas S, Cibeira JL, Dib O, Viso R (1996) Radioactive synoviorthesis in hemophilic hemarthrosis. Clin Orthop 328:14–18 [DOI] [PubMed]
- 8.Gilbert MS (1993) Prophylaxis: musculoskeletal evaluation. Sem Hematology 30(Suppl 2):3–6 [PubMed]
- 9.Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by Mold Arthroplasty. An end result study using a new method of result evatluation. J Bone Joint Surg Am 51:737–755 [PubMed]
- 10.Heeg M, Meyer K, Smid WM, Van Hor JR, Van der Meer J (1998) Total knee and hip arthroplasty in haemophilic patients. Haemophilia 4(5):747–751, Sep [DOI] [PubMed]
- 11.Hilgartner MW (2002) Current treatment of hemophilic arthropathy. Curr Opinion Ped 14:46–49 [DOI] [PubMed]
- 12.Kelley SS, Lachiewicz PF, Gilbert MS, Bolander ME, Jankiewicz JJ (1995) Hip arthroplasty in haemophilic arthropathy. J Bone Joint Surg Am 77:828–834 [DOI] [PubMed]
- 13.Kirschner P (2005) Hip endoprothesis. Chirurg 76:95–104 [DOI] [PubMed]
- 14.Löfquist T, Sanzén L, Petersson C, Nilsson IM (1996) Total hip replacement in patients with hemophilia. Acta Orthop Scand 4:747–751 [DOI] [PubMed]
- 15.Luck JV Jr, Kasper CK (1989) Surgical management of advanced haemophilic arthropathy. An overview of 20 years experience. Clin Orthop 242:60–82 [PubMed]
- 16.Luck JV Jr, Silva M, Rodriguez-Merchan EC, Ghalambor N, Zahiri CA, Finn RS (2004) Hemophilic arthropathy. J Am Acad Orthop Surg 12(4):234–245, Jul–Aug [DOI] [PubMed]
- 17.Nelson IW, Sivamurugan S, Latham PD, Matthews J, Bulstrode CJ (1992) Total hip arthroplasty for haemophilic arthroplasty. Clin Orthop 276:210–213 [PubMed]
- 18.Petterson H, Ahlber A, Nilsson IM (1980) A radiologic classification of hemophilic arthropathy. Clin Orthop 149:153–159 [PubMed]
- 19.Rodriguez-Merchan EC (1998) Editorial. Management of the orthopaedic comlications of haemophlia. J Bone Joint Surg Br 80:191–196 [DOI] [PubMed]
- 20.Rodriguez-Merchan EC (1997) Pathogenesis, early diagnosis, and prophylaxis for chronic hemophilic synovitis. Clin Orthop 343:12–18 [PubMed]
- 21.Schick M, Stucki G, Rodriguez M, Meili EO, Huber E, Michel BA, Brühlmann P (1999) Haemophilic; athropathy: assessment of quality of life after total knee arthroplasty. Clin Rheumatol 18:468–472 [DOI] [PubMed]
- 22.Sethr-Green JK, Evatt BL, Lawrence DN (1989) Acquired immuno deficiency syndrome associated with hemophilia in the United States. Instr Course Lect 38:357–365 [PubMed]
- 23.Teitelbaum S (1977) Radiologic evaluation of the hemophlic hip. Mt Sinai J Med 44:400–401 [PubMed]