Abstract
This retrospective study was conducted to analyse the reliability of clinical diagnosis in meniscal tear injuries. All patients attending our clinic with knee pain from January 2003 to December 2004 underwent systematic and thorough clinical assessment. One hundred and fifty patients were clinically diagnosed to have meniscal tears. All these patients underwent therapeutic arthroscopic knee surgery. The clinical diagnosis was confirmed during this procedure. The accuracy, sensitivity and specificity were calculated based on these arthroscopic findings. The accuracy of clinical diagnosis in our study was 88% for medial meniscal tears and 92% for lateral meniscal tears. The results of this study demonstrate that clinical diagnosis of meniscal tears is as reliable as the results published by other authors for magnetic resonance imaging (MRI) scan. We recommend the use of MRI for more doubtful, difficult and complex knee injuries.
Résumé
Cette étude rétrospective analyse la fiabilité du diagnostic clinique dans les lésions méniscales. De janvier 2003 à décembre 2004 tous les patients présentant des gonalgies ont eu un examen clinique minutieux. 150 avaient des signes de déchirure méniscale et ils ont eu une arthroscopie thérapeutique qui a permis de calculer l’exactitude, la sensibilité et la spécificité du diagnostic. L’exactitude était de 88% pour les lésions méniscales médiales et de 92% pour les lésions latérales. Les résultats montrent que le diagnostic clinique était aussi fiable que le diagnostic par IRM d’après des résultats publiés par d’autres auteurs.
Introduction
The menisci are essential and play an important role in the function of the knee joint. They increase the stability, facilitate lubrication and load bearing of the knee. It is a well recognised fact that large numbers of patients attend orthopaedic clinics with knee injuries. The clinical diagnosis as first step of assessment should be as reliable as possible. Nevertheless no clinical assessment or advanced investigations such as MRI diagnose meniscal tears in all patients. Although magnetic resonance imaging (MRI) is considered by some as the gold standard for accurate, non-invasive evaluation of meniscal tears, it is expensive, not widely available and has inter-observor errors. In this study meniscal tears were clinically diagnosed by positive McMurray test. Arthroscopy was used to assess the reliability of clinical diagnosis.
Materials and methods
All patients attending our clinic with knee pain from January 2003 to December 2004 underwent systematic and thorough clinical assessment. One hundred and fifty patients were clinically diagnosed to have meniscal tears. Ninety-four of these patients presented to us with history of trauma of which 53 were sports related. All these patients were examined by the senior author. Proper clinical history was obtained prior to clinical examination. Physical examination involved assessing joint line tenderness and McMurray test [6]. It also included other special tests to rule out any other associated structural damage to the knee. All patients were examined supine. Knee joint line tenderness was assessed with the patient’s knee flexed to 90° on lateral and medial sides. McMurray test was evaluated with hip in 90° and knee flexed to more than 90°. The examiner should stand to the patient’s right side for right knee with left hand on the knee and right hand holding the foot. The foot is taken from a position of abduction and external rotation to one of adduction and internal rotation. This is repeated for various angles between full flexion and 90°. Painful trapping of damaged meniscus is felt as a clunk on the joint line. Radiographs of the knee were obtained. All these patients underwent therapeutic knee arthroscopy to assess the accuracy of clinical diagnosis. All arthroscopies were performed by the senior author or by a junior under the senior author’s supervision and carried out under regional or general anaesthesia with tourniquet. Most were treated as day cases. Standard anteromedial and anterolateral portals were used. Additional portals were used when required.
Patients with cruciate ligament injuries, tricompartmental arthritis, previous knee operations and patients with both medial and lateral joint line tenderness were excluded. One hundred and thirty patients met our study criteria for clinical diagnosis of meniscal tears.
Results
The study group of 130 patients consisted of 90 men (69%) and 40 women (31%). All underwent arthroscopic knee surgery. The average age was 49 years (range: 19–79 years). Sixty-six were right knees (51%) and 64 were left knees (49%). Of the 130 patients in the study group, 102 patients had medial meniscal tears (78%) and 28 patients had lateral meniscal tears (22%) on clinical examination. Tables 1 and 2 show the methods and formulas used to calculate the reliability of clinical diagnosis.
Table 1.
Methods of calculation
| Test positive | Test negative | |
|---|---|---|
| Patient with disease | True positive (TP) | False negative (FN) |
| Normal patient | False positive (FP) | True negative (TN) |
Table 2.
Formulas for calculation
| Value | Calculation |
|---|---|
| Sensitivity | TP/(TP+FN)×100 |
| Specificity | TN/(TN+FP)×100 |
| Positive predictive value (PPV) | TP/(TP+FP)×100 |
| Negative predictive value (NPV) | TN/(TN+FN)×100 |
| Accuracy | TP+TN/TK×100 |
Clinical diagnostic test characteristics
Sensitivity: how good the test is at detecting meniscal tear
Specificity: how good the test is at identifying normal knee
Positive predictive value: how often a patient with a positive test has the meniscal tear
Negative predictive value: how often a patient with a negative test does not have meniscal tear
Accuracy: proportion of test which correctly identifies meniscal injuries
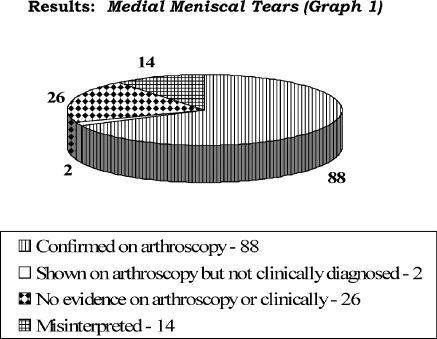
Of the 102 patients (Fig. 1) with a clinical diagnosis of medial meniscal tears, 88 (86%) were confirmed on arthroscopy (true positive). Twenty-six patients had no evidence of medial meniscal tears either clinically or on arthroscopic procedure (true negative). Fourteen patients were misinterpreted to have medial meniscal tears (false positive) and two patients with medial meniscal tears were not diagnosed clinically (false negative). The clinical diagnosis had an accuracy of 88% for medial meniscal tears (sensitivity 98%, specificity 65%, positive predictive value 87% and negative predictive value 93%). Fourteen false positive clinical diagnoses comprised one normal knee, two lateral meniscal tears, three medial compartment arthritis, two medial femoral condyle osteochondral flaps and six patella degenerative changes presenting with medial meniscal symptoms.
Fig. 1.
Results: medial meniscal tears
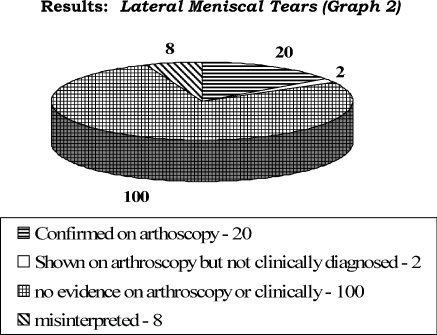
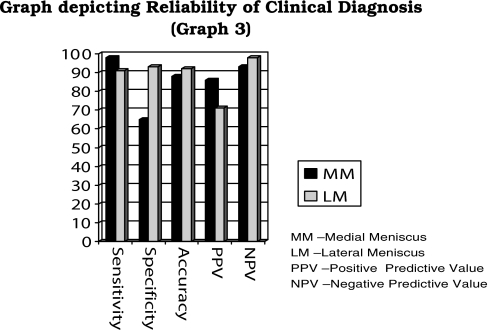
Of the 28 patients (Fig. 2) with clinical diagnosis of lateral meniscal tears, 20 (71%) were confirmed on arthroscopy (true positive). One hundred patients had no evidence of lateral meniscal tears either clinically or on arthroscopic procedure (true negative). Eight patients were misinterpreted to have lateral meniscal tear (false positive) and two patients with lateral meniscal tears were not diagnosed clinically (false negative). The clinical diagnosis for lateral meniscal tears had an accuracy of 92% (sensitivity 91%, specificity 93%, positive predictive value 71% and negative predictive value 98%). Eight false positive clinical diagnoses comprised one normal knee, two medial meniscal tears, three tibial articular surface degeneration and two patients with patellar maltracking causing symptoms of lateral meniscal tears. Table 3 and Fig. 3 show the reliability of clinical diagnosis for medial and lateral meniscal injuries.
Fig. 2.
Results: lateral meniscal tears
Table 3.
Reliability of clinical diagnosis for medial and lateral meniscal injuries
| Medial meniscal tear | Lateral meniscal tear | |
|---|---|---|
| Sensitivity | 98 | 91 |
| Specificity | 65 | 93 |
| Accuracy | 88 | 92 |
| PPV | 86 | 71 |
| NPV | 93 | 98 |
Fig. 3.
Graph depicting reliability of clinical diagnosis
Discussion
Although major advances have taken place in the field of non-invasive diagnostic tools such as MRI, clinical diagnosis remains important and reliable. Expensive investigation could be avoided if clinical diagnosis is as reliable as MRI. This study was conducted to determine the reliability of clinical diagnosis of meniscal tears as compared to MRI scan results. There are various tests described to diagnose meniscal tears such as joint line tenderness, McMurray test and Apley compression test. We have used joint line tenderness and McMurray test in our study. The advent of arthroscopy of the knee has revolutionalised the diagnosis and treatment of meniscal tears. It is routinely carried out as a day case procedure. It facilitates rapid rehabilitation. The clinical diagnosis was confirmed or refuted during this procedure. The accuracy, sensitivity and specificity were calculated based on the arthroscopic findings.
Eren [8] reported on accuracy of joint line tenderness in meniscal tears in 104 knees, which was 74% for medial meniscal tears and 96% for lateral meniscal tears. The study group had a mean age of 19.2 years (range: 18–20 years) with definite history of injury. Our study group with an average age of 49 years (range: 19–79 years) had definite history of injury in 40% of patients. Although we have a wide range of age in our group, we had a better accuracy for medial meniscal injuries. Use of two diagnostic tests has certainly improved the reliability for medial meniscal tear evaluation but has not improved lateral meniscal tear accuracy rates.
Miller [5] found overall clinical diagnosis accuracy of meniscal tears of 80.7% and the corresponding accuracy for MRI was 73.7%. We had an accuracy of 90% for the clinical diagnosis test. Rose and Gold [7] found the clinical examination to be correct more often than MRI diagnosis. They stated that most often MRI just confirms the clinical diagnosis and adds a little more information about the injury pattern. They suggested that negative clinical examination eliminates the need for MRI as a screening tool. They found no significant difference in accuracy between clinical examination and MRI in both medial and lateral meniscal tears or anterior cruciate ligament (ACL) tears. The accuracy of MRI in their study for medial meniscal tears was 75% and 76% for lateral meniscal tears which is lower than our accuracy rates. Munk et al. [3] recommended MRI as a clarifying tool to reduce the number of normal arthroscopies. They had MRI sensitivity of 84%, specificity of 75% and clinical accuracy of 79% for meniscal tears. We have a clinical accuracy of 88% for medial meniscal tears and 92% for lateral meniscal tears.
Boden et al. [2] showed that it would be cost effective to bypass MRI and proceed directly to arthroscopy based on their mathematical formula. They showed that up to 78% of knees scanned require arthroscopy for treatment. Kocabey et al. [9] stated that clinical examination is as accurate as MRI in the skilled orthopaedic surgeon’s hands and MRI should be reserved for more complicated and confusing cases. Bohnsack et al. [4] also concluded that an experienced examiner can diagnose adequately by clinical examination alone. Akseki et al. [1] suggested that the accuracy of clinical diagnosis of a meniscal tear is decreased by the presence of an ACL tear and the presence of both these injuries requires more frequent magnetic resonance imaging.
Conclusions
Most studies do not show any significant differences in clinical and MRI diagnosis of meniscal tears. Our study has an accuracy similar to most of the MRI studies on meniscal tears. Hence we conclude that physical examination is a useful and important diagnostic technique and is as reliable as MRI to diagnose meniscal tears. We recommend the use of MRI for more doubtful, difficult and complex knee injuries.
Contributor Information
B. R. Mohan, Phone: +44-07940579332, Email: drmohanbr@rediffmail.com
Harminder S. Gosal, Phone: +44-08454-222925, FAX: +44-08454223404
References
- 1.Akseki D, Pinar H, Karaoglan O (2003) The accuracy of the clinical diagnosis of meniscal tears with or without associated anterior cruciate ligament tears. Acta Orthop Traumatol Turc 37(3):193–198 [PubMed]
- 2.Boden SD, Davis DO, Dina TS, Stoller DW, Brown SD, Vailas JC, Labropoulos PA (1992) A prospective and blinded investigation of magnetic resonance imaging of the knee. Abnormal findings in asymptomatic subjects. Clin Orthop 282:177–185 [PubMed]
- 3.Munk B, Madsen F, Lundorf E, Staunstrup H, Schmidt SA, Bolvig L, Hellfritzch MB, Jensen J (1998) Clinical magnetic resonance imaging and arthroscopic findings in knees: a comparative prospective study of meniscus anterior cruciate ligament and cartilage lesions. Arthroscopy 14(2):171–175 [DOI] [PubMed]
- 4.Bohnsack M, Ruhmann O, Sander-Beuermann A, Wirth CJ (1999) Comparison of clinical examination with NMR spectroscopy in the diagnosis of meniscal lesions in daily practice. Z Orthop Ihre Grenzgeb 137(1):38–42 [DOI] [PubMed]
- 5.Miller GK (1996) A prospective study comparing the accuracy of the clinical diagnosis of meniscus tear with magnetic resonance imaging and its effect on clinical outcome. Arthroscopy 12(4):406–413 [DOI] [PubMed]
- 6.McMurray TP (1941) The semilunar cartilages. Br J Surg 29:407 [DOI]
- 7.Rose NE, Gold SM (1996) A comparison of accuracy between clinical examination and magnetic resonance imaging in the diagnosis of meniscal and anterior cruciate ligament tears. Arthroscopy 12(4):398–405 [DOI] [PubMed]
- 8.Eren OT (2003) The accuracy of joint line tenderness by physical examination in the diagnosis of meniscal tears. Arthroscopy 19(8):850–854 [DOI] [PubMed]
- 9.Kocabey Y, Tetik O, Isbell WM, Atay OA, Johnson DL (2004) The value of clinical examination versus magnetic resonance imaging in the diagnosis of meniscal tears and anterior cruciate ligament rupture. Arthroscopy 20(7):696–700, (September) [DOI] [PubMed]