Abstract
Pain control following painful orthopaedic procedures such as total knee arthroplasty (TKA) is an ongoing challenge, as current pain management techniques often result in under-medication and/or complications. In a study designed to test the effect of the micro-current skin patch (MCT) on pain relief in patients following TKA, we followed 24 patients, randomly divided into two groups, one group receiving MCT plus tramadol hydrochloride (tramadol) for pain relief and a control group receiving only tramadol, for 10 days postoperatively. Tramadol was given intramuscularly in increment doses of 100 mg, as needed, for the duration of the study period. Pain was assessed daily using a visual analogue score (VAS). Other parameters, including the effect of MCT on the dose of tramadol needed for pain relief, the degree of wound healing measured at the end of the follow-up period, category of the wound 10 days postoperatively (1, 2 or 3) and total drain fluid volume, were also assessed. During the 10-day postoperative period there was a progressive decrease in pain in patients of both groups, however the patients of the MCT group showed a consistently lower VAS throughout the observation period, most markedly on those follow-up days with the highest pain scores in patients of the control group. This effect was monitored on the basis of the average dose of tramadol administered per day: 200.0±7.0 mg/day in the control group and 63.3±15.8 mg/day in the MCT group. Wound healing was better with the application of the MCT patch: grade 1 wounds were observed in 50% of the patients of the MCT group as compared to 8.3% in control group. The total drain volume was lower in patients of the MCT group compared to the controls (1020.8±211.6 and 1170.8±243.5 ml, respectively). None of the patients indicated that they wished to discontinue MCT therapy. This pilot study shows that MCT therapy led to better pain control with a markedly lower need for tramadol as compared to the control group. This better pain control was accompanied by a better healing of the wound and a lower drain volume.
Résumé
Le contrôle de la douleur après une intervention de chirurgie orthopédique (prothèse totale de genou) doit être prise en charge. Cette étude pilote inclut 24 patients qui ont bénéficié d’une prothèse totale. Les patients ont été divisés en deux groupes : un groupe de 12 patients chacun. Le groupe 1 était traité par un patch MCT de tramadol hydrochloride SOS (groupe MCT). Le groupe 2 a reçu du tramadol hydrochloride SOS sans utilisation du patch et a servi de groupe contrôle. Les deux groupes ont reçu du tramadol intraveineux la dose de 100 mg pendant les 10 jours postopératoires. La douleur a été analysée par une échelle analogique (VAS). D’autres facteurs ont été étudiés dont la dose de tramadol, le degré de cicatrisation et le volume des pertes sanguines. Ces résultats montrent une diminution progressive de la douleur. Le groupe MCT a nécessité une utilisation moindre de tramadol que le groupe control (200±7 mg/jour, versus 63.3±15.8 mg/jour). La cicatrisation a été meilleure dans le groupe MCT de même que le volume des pertes sanguines (1020±211.6 et 1170±243.5 dans les deux groupes respectivement). Cette étude montre que l’utilisation d’un patch MCT dans la PTG permet de mieux contrôler la douleur, une meilleure cicatrisation et moins de pertes sanguines.
Introduction
Postoperative pain management is critical for the optimal care of orthopaedic surgery patients, especially following operations that cause considerable pain, such as total knee arthroplasty (TKA). Opioids, administered intramuscularly (i.m.), as epidurals or intravenously (i.v.) as patient-controlled analgesia, are effective for the relief of severe pain [10].
Adjunctive therapy and pre-emptive analgesia such as nerve blocks and methods of delivery such as infusion pumps are recognised but are not used as standard practice. Oral opioids are effective for relieving moderate to severe pain, and tramadol hydrochloride (tramadol), which has an efficacy comparable to that of morphine but with fewer severe side effects, is often selected for the relief of moderate to moderately severe pain [1]. Opioid-sparing NSAIDs, such as ketorolac, and COX-2-specific NSAIDS are also widely used. However, these current pain management techniques often result in under-medication and/or complications [4, 9].
Non-pharmacologic treatments and alternative approaches are less widely applied. Such approaches are generally more individually oriented, often involving one or a combination of such therapies as physical therapy, cryotherapy, continuous passive motion (CPM), transcutaneous electrical nerve stimulation (TENS) and patient education [1, 8].
Reports on the effectiveness of microcurrent therapy (MCT) in the management of pain are promising and, as such, MCT may offer a new non-pharmacologic approach which, to our knowledge, has not been applied to postoperative pain for TKA.
The main objective of this study was an assessment of postoperative pain following TKA, with and without the application of an MCT patch. Our secondary objectives included an assessment of the tramadol dose needed for pain relief and the effect of tramadol on the degree of wound healing and total drain fluid volume.
Patients and method
This pilot case-control study included 24 patients who underwent TKA. Patients were randomly allocated into two groups of 12 patients each. Group 1 patients were administered MCT applied by means of Painmaster electrodes (Painmaster MCT Patch, Newmark, Conn.) which did not interfere with the wound or its dressing (Fig. 1), with tramadol for pain relief (MCT Group). Group 2 patients received only tramadol for pain relief, without the application of MCT and served as a control group. Tramadol was given i.m. in increment doses of 100 mg to a maximum of 400 mg/day, and both groups were observed for 10 days postoperatively.
Fig. 1.

Microcurrent adhesive skin patch in situ (arrows) during postoperative dressing; the second patch is positioned on the opposite side of the knee at the level of the patella
The board of the Orthopaedic Department at Ain Shams University approved this study from the scientific and ethical point of view. This study meets the ethical standards and comply with the national as well as the local standards set within the department. All patients signed an informed consent form before being included in the study.
The primary endpoint was pain assessment, which was measured daily using a visual analogue score (VAS). Other endpoints included dose of tramadol needed for pain relief, degree of wound healing measured at the end of the follow-up period, a categorisation of the wound into grade 1, 2 and 3, respectively (grade 1: dry suture line, no redness around suture line, normal skin texture around suture line’; grade 2: wet suture line, no or minimal redness, normal skin; grade 3: wet or draining suture line, redness and surrounding skin changes of oedema or bullae) and total drain fluid volume (in millilitres).
Data are summarised using means ± standard deviations for quantitative variables and percentages for categorical variables. Nonparametric tests were used for analysis due to the limited number of patients in this pilot study. The threshold of significance was fixed at the 5% level.
Results
Effect of MCT on pain control
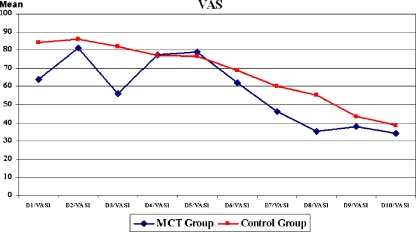
The VAS was lower in patients administered MCT from day 1 postoperatively onwards for all 10 days of the study (Table 1, Fig. 2).
Table 1.
Pain visual analogue score (mean ± standard deviation) during the 10-day observation period in the two groups
| Days | Control group | MCT group |
|---|---|---|
| 1 | 84.2±4.2 | 63.7±19.4 |
| 2 | 86.3±4.8 | 81.3±14.6 |
| 3 | 82.1±7.2 | 55.8±18.3 |
| 4 | 77.1±9.6 | 77.5±17.4 |
| 5 | 76.7±8.1 | 78.8±26.8 |
| 6 | 68.8±7.4 | 62.1±15.9 |
| 7 | 60.0±12.1 | 46.1±19.8 |
| 8 | 55.4±10.9 | 35.4±11.9 |
| 9 | 43.8±7.4 | 37.9±17.8 |
| 10 | 38.8±10.9 | 34.2±13.8 |
Fig. 2.
Change in visual analogue score in the two groups during the 10-day observation period
Effect of MCT on dose of tramadol
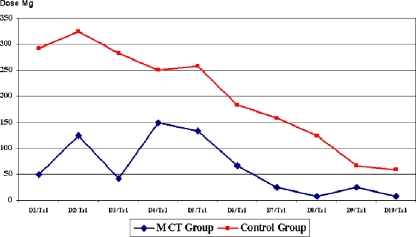
The lower VAS for pain in the MCT group was achieved using a significantly (p<0.001) lower dose of tramadol than in the controls. The average daily dose in the control group was 200.0±7.0 mg and in the MCT group, 63.3±15.8 mg. Throughout the entire postoperative observation period, patients of the MCT group needed lower doses of tramadol for pain relief (Table 2, Fig. 3).
Table 2.
Daily dose (mg) of tramadol (mean ± standard deviation) in the two groups during the 10-day postoperative observation period
| Days | Control group | MCT group |
|---|---|---|
| 1 | 291.7±66.9 | 50.0±67.4 |
| 2 | 325.0±45.2 | 125.0±75.4 |
| 3 | 283.3±71.8 | 41.7±66.9 |
| 4 | 250.0±67.4 | 15.0±90.5 |
| 5 | 258.3±108.4 | 133.3±49.2 |
| 6 | 183.3±71.8 | 66.7±65.1 |
| 7 | 158.3±90.0 | 25.0±45.2 |
| 8 | 125.0±86.6 | 8.3±28.9 |
| 9 | 66.7±65.1 | 25.0±45.2 |
| 10 | 58.3±51.5 | 8.3±28.9 |
Fig. 3.
Average daily dose (mg) of tramadol needed by patients in the two groups during the 10-day postoperative observation period
These figures clearly illustrate that lower doses of tramadol for pain relief were needed by patients of the MCT group in comparison to those of the control group. On day 1 postoperatively almost 60% of the patients in the MCT group did not require tramadol. In contrast, 80% of the patients in the control group required more than 300 mg of tramadol. On the tenth day postoperatively, more than 90% of the patients in the MCT group no longer required the drug in comparison to 40% in the control group (Table 3).
Table 3.
Distribution of dose of tramadol in the two groups during the 10-day postoperative observation period
| Day | Groupa | Dose (mg) | ||||
|---|---|---|---|---|---|---|
| 0 | 100 | 200 | 300 | 400 | ||
| 1 | Control | 0 | 0 | 1 | 7 | 4 |
| MCT | 7 | 4 | 1 | 0 | 0 | |
| 2 | Control | 0 | 0 | 0 | 9 | 3 |
| MCT | 1 | 8 | 2 | 1 | 0 | |
| 3 | Control | 0 | 0 | 4 | 6 | 2 |
| MCT | 8 | 3 | 1 | 0 | 0 | |
| 4 | Control | 0 | 0 | 7 | 4 | 1 |
| MCT | 2 | 3 | 6 | 1 | 0 | |
| 5 | Control | 0 | 1 | 7 | 0 | 4 |
| MCT | 0 | 8 | 4 | 0 | 0 | |
| 6 | Control | 0 | 4 | 6 | 2 | 0 |
| MCT | 5 | 6 | 1 | 0 | 0 | |
| 7 | Control | 1 | 5 | 4 | 2 | 0 |
| MCT | 9 | 3 | 0 | 0 | 0 | |
| 8 | Control | 2 | 6 | 3 | 1 | 0 |
| MCT | 11 | 1 | 0 | 0 | 0 | |
| 9 | Control | 5 | 6 | 1 | 0 | 0 |
| MCT | 9 | 3 | 0 | 0 | 0 | |
| 10 | Control | 5 | 7 | 0 | 0 | 0 |
| MCT | 11 | 1 | 0 | 0 | 0 | |
aNumbers given in the table are the number of patients administered that dose of tramadol
Effect of MCT on wound healing
As shown in Table 4, wound healing was better in the MCT group. The patients of this group had a higher frequency of grade 1 wounds [50.0 vs. 8.3% (control)], while the patients of the control group had a higher frequencey of grade 2 and 3 wounds. Ridit analysis revealed that the higher frequency of lower grade wounds in the MCT group was significant (p<0.001). This was accompanied by a lower drain volume in the MCT group.
Table 4.
Grade of wound healing
| Grade | Control (%) | MCT (%) |
|---|---|---|
| 1 | 8.3 | 50.0 |
| 2 | 66.7 | 41.7 |
| 3 | 25.0 | 8.3 |
Effect of MCT on drain volume
The lower pain VAS and better wound healing in patients of the MCT group were accompanied by a lower drain volume compared to the control patients. The mean drain volume was 1020.8+211.6 ml in the MCT group and 1170.8±243.5 ml in control group. The difference was proved to be statistically significant (p<0.05).
Side effects and discontinuation of treatment
During the entire observation period, none of the patients had any side effects from the patch application, and none requested discontinuation of MCT treatment.
Discussion
Pain control following painful orthopaedic procedures such as TKA is an ongoing challenge, as current pain management techniques often result in under-medication and/or complications [1, 10]. The standard approach depends on systemic opioids given in bolus i.v. or i.m., or by patient-controlled analgesia (PCA) self-administration pumps. Pre-emptive analgesia in the form of epidural pumps and several techniques of regional nerve blocks also depend on opioids and local anaesthetic agents. Oral pharmacological postoperative pain therapy similarly depends on opioids, however non-opioid agents such as tramadol hydrochloride are widely used due to their relative safety and known potency. NSAIDs and the new COX-2-specific NSAIDs are widely administered despite the range of side effects associated with their administration in the relatively higher doses required in such operations as TKA [1, 4, 10].
Non-pharmacological methods for pain relief, such as physical therapy, cryotherapy, CPM, TENS and patient education [4], are less widely accepted. Reports on the efficacy of cryotherapy [5, 6, 8] and TENS [2] are generally disappointing, while the use of CPM to control pain is controversial [11]. While several investigators have reported a favourable effect of MCT on pain control and tissue healing through the modification and recruitment of cell membrane ATP (adenosine triphosphate), this occurred mostly under conditions of chronic pain [3, 7]. If MCT proves to be a reliable and effective method to control pain postoperatively while avoiding the side effects associated with pharmacologically based methods, a new approach for postoperative pain management would be available to the orthopaedic surgeon.
This pilot study was designed to investigate such an approach. Based on our results on this small number of patients, it is evident that those patients using the MCT had a lower requirement for tramadol to control the pain, indicating better pain control. We also provide evidence that the use of MCT may improve localised healing of the wound, which may be of major importance in TKA and other operations with major surgical approaches.
Conclusion
This pilot study showed that MCT led to better pain control, with a markedly lower requirement for tramadol as compared to the control group.
This improved pain control was accompanied by a better healing of the wound and a lower drain volume.
-
There were neither adverse effects nor a need to discontinue MCT therapy.
Further formal clinical trials with larger numbers are required to establish the validity of this pilot study.
Footnotes
Financial support:
None of the authors received financial support for this study.
References
- 1.Bourne MH (2004) Analgesics for orthopedic postoperative pain. Am J Orthop 33:128–135 [PubMed]
- 2.Breit R, Van der Wall H (2004) Transcutaneous electrical nerve stimulation for postoperative pain relief after total knee arthroplasty. J Arthroplasty 19:45–48 [DOI] [PubMed]
- 3.Cheng N, Van Hoof H, Bockx E, Hoogmartens MJ, Mulier JC, De Dijcker FJ, Sansen WM, De Loecker W (1982) The effects of electric currents on ATP generation, protein synthesis, and membrane transport of rat skin. Clin Orthop Relat Res 171:264–272 [PubMed]
- 4.Colwell CW Jr (2004) The use of the pain pump and patient-controlled analgesia in joint reconstruction. Am J Orthop 33:10–12 [PubMed]
- 5.Healy WL, Seidman J, Pfeifer BA, Brown DG (1994) Cold compressive dressing after total knee arthroplasty. Clin Orthop Relat Res 299:143–146 [PubMed]
- 6.Ivey M, Johnston RV, Uchida T (1994) Cryotherapy for postoperative pain relief following knee arthroplasty. J Arthroplasty 9:285–290 [DOI] [PubMed]
- 7.Jaffe LF, Vanable JW Jr (1984) Electric fields and wound healing. Clin Dermatol 2:34–44 [DOI] [PubMed]
- 8.Scarcella JB, Cohn BT (1995) The effect of cold therapy on the postoperative course of total hip and knee arthroplasty patients. Am J Orthop 24:847–852 [PubMed]
- 9.Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM (1998) Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg 87:88–92 [DOI] [PubMed]
- 10.Skinner HB, Shintani EY (2004) Results of a multimodal analgesic trial involving patients with total hip or total knee arthroplasty. Am J Orthop 33:85–92 [PubMed]
- 11.Walker RH, Morris BA, Angulo DL, Schneider J, Colwell CW Jr (1991) Postoperative use of continuous passive motion, transcutaneous electrical nerve stimulation, and continuous cooling pad following total knee arthroplasty. J Arthroplasty 6:151–156 [DOI] [PubMed]