Abstract
The methods and clinical outcomes of intra-sheath triamcinolone injection in the treatment of de Quervain’s disease are described. We used 38 hands of 36 patients. A mixture of 1 ml of triamcinolone and 1 ml of 1% lidocaine hydrochloride was injected, with an interval of 2 weeks. The fluid was injected into one point above the induration for the first 18 hands and into two points over the extensor pollicis brevis and abductor pollicis longus tendon in the induration for hands 19–38. The efficacy rate was 89%, with the treatment results of the two-point injection better than those of the one-point injection. Recurrence was observed in ten hands, and complications in 13 hands; however, over 90% of patients were satisfied with the injection. The accurate injection of triamcinolone into the sheath of both the extensor pollicis brevis and abductor pollicis longus tendon was considered very effective for de Quervain’s disease.
Résumé
L’injection de triamcinolone dans la maladie de de Quervain a déjà été décrite. 38 mains sur 36 patients ont été traitées par un mélange d’1 ml de triamcinolone et 1 ml d’1% de lidocaine hydrochlorique injectées à l’intervalle de deux semaines. Le liquide a été injecté au dessus de l’induration : à deux niveaux différents en dessous pour les 18 premières mains et en deux points différents au dessus du court extenseur et de l’abducteur du pouce pour les 20 suivants. Le taux de succès a été de 89 avec deux points d’injection, taux supérieur à un point, une récidive a été observée dans 10 mains et des complications dans 13 mains. Cependant, plus de 90% des patients sont satisfaits de cette injection. En conclusion : l’injection triamcinolone dans la gaine de l’extenseur du pouce et de l’abducteur peuvent être considérés comme efficaces dans la maladie de de Quervain.
Introduction
De Quervain’s disease [3] is quite often encountered in the clinical practice of orthopaedics, and the general treatment procedure is as follows: nonsurgical procedures such as limiting the use of the thumb, braces and intra-sheath steroid injections, and, if these processes are ineffective, the tendon sheath of the first dorsal compartment is surgically released [4, 13]. However, in practice, surgery is often performed without exhausting all these nonsurgical treatments. Although there are some recent reports on the efficacy of the intra-sheath injection of triamcinolone acetonide (TC), which is a long-acting and lyophobic steroid, for patients with snapping fingers [2, 8, 10], there are no comprehensive reports describing the clinical outcomes of intra-sheath injection in the treatment of de Quervain’s disease. We describe the intra-sheath injection of TC in the treatment of de Quervain’s disease and report on its clinical outcomes and complications.
Materials and methods
Among 43 hands of 40 de Quervain’s disease patients treated with an intra-sheath injection of TC from July 1994 to June 2003, 38 hands of 36 patients who could answer the survey questions in a face-to-face interview or on the telephone were selected for this study. There were 14 men and 22 women in this series, with a mean age of 46 years (range 22 years to 77 years). The right hand was involved in 23 patients, and the left in 15 patients; two were bilateral. In 24 patients the dominant hand was affected. The mean duration from the onset of pain to the first examination was 17 weeks (range 2 weeks to 45 weeks), and the mean duration of follow-up examination was 36 months (range 29 months to 42 months). All patients showed positive results on the Finkelstein test, had sharply localized tenderness and pain on exertion in the first dorsal compartment of the wrist, and complained of difficulty in using their hands in daily life. Patients who had previously suffered underlying diseases, such as rheumatoid arthritis, gout, chronic renal failure or diabetes mellitus, and those who were pregnant or who had undergone intra-sheath steroid injection for the treatment of de Quervain’s disease were excluded from this subject group. Informed consent was obtained from all the patients selected as subjects in this study.
All injections were performed by one of the authors (T.S.) using the same technique. A mixture of 1 ml (10 mg) of TC and 1 ml of 1% lidocaine hydrochloride was used for injection. In principle, injections were performed a maximum of three times, with an interval of 2 weeks between injections, and treatment was terminated when effects were observed.
Prior to intra-sheath injection, regions with tenderness and induration were confirmed by palpation, and a 26- or 27-gauge needle was inserted vertically through the skin from the site immediately above the region up to the bone. Since resistance is so high, in this position, that the syringe cannot be pushed, the needle was pulled back to reach the point where the syringe could be pushed under resistance, we injected the mixture, stretching the synovial sheath by a volume effect. Sufficient filling in the tendon sheath distally and proximally was confirmed by palpation, and the needle was pulled out when injection was no longer possible. In principle, intra-sheath injection was used, but it should be noted that slight leakage into subcutaneous tissues could have occurred.
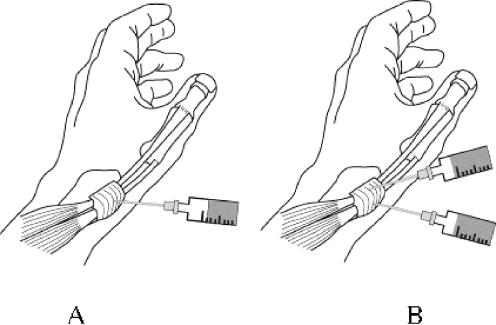
For the first 18 hands of 17 patients, the fluid was injected into one point immediately above the indurated tendon sheath in the first dorsal compartment of the wrist. However, in hands 19–38, with sufficient verification of the contours of the extensor pollicis brevis (EPB) tendon and abductor pollicis longus (APL) tendon, the amount of fluid was halved and injected into two points in the indurated part that coincided with the paths of these two tendons (Fig. 1).
Fig. 1.
Injection methods. a For the first 18 hands the fluid was injected into one point immediately above the indurated tendon sheath in the first dorsal compartment of the wrist. b In hands 19–38 the amount of fluid was halved and injected into two points that coincided with the paths of the extensor pollicis brevis tendon and abductor pollicis brevis tendon
The treatment results were categorised into four groups: no pain or disruption of daily life was classified as excellent; occasional pain but no disruption of daily life as good; reduced pain but disruption of daily life as fair; and continued or worsening pain and disruption of daily life as poor. Differences between the two groups in terms of the number of injections, the recurrence of tenovaginitis, the occurrence of complications, and differences in the outcome of the treatment depending on differences in the injecting method were surveyed. Additionally, in the questionnaire, the three items listed in Table 1 were surveyed. All follow-up examinations were performed by one of the authors (T.S.).
Table 1.
Three items in the questionnaire
Statistical comparison of the treatment results between the one-injection group and two-injection group was by the Mann–Whitney U test for non-parametric data. A P value <0.05 was taken as statistically significant.
Results
Thirty-three patients were examined in person and three patients were telephoned.
The treatment results of the TC injection at the final investigation were excellent in 24 hands (63%), good in ten (26%), and fair in four (11%); no hands showed a poor result. The efficacy rate, determined as an outcome of good or better than good with no difficulties in daily life, was 89%. Two of four hands with a “fair” outcome eventually required surgical release of the tendon sheath. For differences in the injection method, the one-point injection was excellent in nine hands (50%), good in five hands (28%), and fair in four hands (22%), and the two-point injection was excellent in 15 hands (75%), and good in five hands (25%). The two-point injection was better than the one-point injection, with an efficacy rate of 100%. There was significant difference between the one-injection and two-injection groups (P<0.001).
The number of injections was 1 for 26 hands, 2 for nine hands, and 3 for three hands, with a mean of 1.4. For 68% of subjects, treatment was completed after one injection. For differences in the injection method, the number of one-point injections was 1 for 12 hands (67%), 2 for four hands (22%), and 3 for two hands (11%), and that of two-point injections was 1 for 14 hands (70%), 2 for five hands (25%), and 3 for one hand (5%). There were fewer two-point injections than one-point injections, but there was no significant difference between the two groups.
Tenovaginitis recurrence was observed in ten hands, of which five hands were in the two-point injection group and five were in the one-point injection group; however, this was relieved by repeating the intra-sheath injection of TC.
Regarding the treatment choice, 32 patients (89%) in both the one-injection and two-injection groups answered that they were satisfied with the intra-sheath injection, with 14 patients in the one-injection group and 18 patients in the two-injection group. Regarding the treatment choice in the case of recurrence, 31 patients (86%) in both the one-injection and two-injection groups answered that they would choose the intra-sheath injection, with 12 patients in the one-injection group and 19 patients in the two-injection group. Five patients (14%), all from the one-injection group, answered that they would choose surgery; however, they all had jobs or hobbies that required intensive use of their hands.
Complications
In five hands of four patients, pain was temporarily aggravated around the injection site from 3 days to 10 days after the injection; however, it had disappeared in all these hands by the time of subsequent examination 2 weeks later. De-pigmentation around the needle-insertion site was observed in four hands, and atrophy of subcutaneous fat tissue at the same site was observed in three; however, these symptoms had disappeared spontaneously in all these hands within 6 months. No injury to the superficial radial nerve, tendon rupture or evidence of infection after injection was observed.
Discussion
Since de Quervain [3] reported pain along the radial styloid process caused by impaired tendon gliding in the first dorsal compartment of the wrist in 1895, there have been many reports on its clinical features and treatments. Recently, nonsurgical treatment using intra-sheath steroid injections has been reviewed [1, 6, 12, 14–16]. We performed intra-sheath injections of TC for patients with de Quervain’s disease, and the efficacy rate was 94% in this study. Richie and Eriner [12], who reviewed seven current reputable papers and surveyed the treatment outcomes, concluded that the efficacy rate of injecting the steroid alone was 83%. Although the evaluation method in this study was different from that in their reports, our outcomes were much better than those previously reported.
The action of TC in the body remains to be clarified. Since TC is a lyophobic steroid and has two insoluble methyl groups in the constitutional formula, the absorption of TC by tissues is slower than that of other steroids and it remains in the tendon sheath for a long time, so the anti-inflammatory effects of TC are considered to persist from 2 weeks to about 1 month after injection [11]. TC is therefore considered more effective in treating chronic inflammation, such as de Quervain’s disease, than other steroids. However, before starting the treatment, patients should be fully informed of a transient increase in pain and side effects of TC on the skin and subcutaneous tissue, which may persist for a time after injection.
As Froimson [4] observed, surgery is readily chosen to treat de Quervain’s disease with the view of reducing the treatment period and preventing recurrence despite good outcomes with intra-sheath injection. Surgical treatment has been chosen for tenovaginitis without careful consideration, and nonsurgical treatment has not been emphasised [1]. In our series the average number of injections was 1.4, requiring 10 days, i.e., less than 2 weeks for one treatment period. This treatment period is not long and is almost the same as that from the day of surgery to the removal of stitches. In our survey more than 90% of patients were satisfied with their choice of intra-sheath injection. Recurrence was observed in 26% of patients, which was not insignificant; however, with regard to treatment choice in the event of recurrence, 87% of patients answered that they would again choose intra-sheath injection. Although complications were observed in 12 hands (32%), they did not have serious effects and all resolved spontaneously, suggesting that surgery should not be chosen so readily.
Although a septum is highly probable within the first dorsal compartment of the wrist [5, 7, 9], we first performed a one-point injection into a tender induration. In the middle of our study we started to perform two-point injections into the indurated part along the paths of the EPB tendon and the APL tendon after identifying their contours. With this injection method the outcomes improved and the efficacy rate increased to 100%. It is vital to inject the therapeutic agent accurately into the tendon sheath to improve the treatment outcome. We initially inserted the tip of the needle immediately above the radial styloid process, pulled the needle backward while pressing the syringe, found the injection point by feeling resistance, and then injected the fluid at that point. Accurate injection of the fluid into the tendon sheath can be confirmed by thickening of the synovial tendon sheath along the tendon. From these results we conclude that an accurate injection of TC into both the EPB and APL tendon sheaths by the two-point injection method is a very effective treatment for de Quervain’s disease.
References
- 1.Ahuja NK, Chung KC (2004) Fritz de Quervain, MD (1868–1940) Stenosing tendovaginitis at the radial styloid process. J Hand Surg [Am] 29:1164–1170 [DOI] [PubMed]
- 2.Bonnici AV, Spenser JD (1988) Survey of “Trigger finger” in adults. J Hand Surg [Br] 13:202–203 [DOI] [PubMed]
- 3.De Quervain F (1895) Uber eine Form von chronischer Tendovaginitis. Corresp Blatt Schweizer Arzte 25:389–394
- 4.Froimson A (1993) Tenosynovitis and tennis elbow. In: Green DP (ed) Operative hand surgery, vol. 2, 3rd edn. Churchill Livingstone, New York, pp 1989–2006
- 5.Giles KW (1960) Anatomical variations affecting the surgery of de Quervain’s disease. J Bone Joint Surg Br 42:352–355 [DOI] [PubMed]
- 6.Harvey FJ, Harvey PM, Horsley MW (1990) de Quervain’s disease: surgical or nonsurgical treatment. J Hand Surg [Am] 15:83–87 [DOI] [PubMed]
- 7.Jackson WT, Viegas SF, Coon TM et al (1986) Anatomical variation in the first extensor compartment of the wrist: a clinical and anatomical study. J Bone Joint Surg Am 68:923–926 [PubMed]
- 8.Lapidus PW (1953) Stenosing tenosynovitis. Surg Clin North Am 33:1317–1347 [DOI] [PubMed]
- 9.Leslie BM, Ericson WB Jr, Morehead JR (1990) Incidence of a septum within the first dorsal compartment of the wrist. J Hand Surg [Am] 15:88–91 [DOI] [PubMed]
- 10.Newport L, Lane LB, Stuchin SA (1990) Treatment of trigger finger by steroid injection. J Hand Surg [Am] 15:748–750 [DOI] [PubMed]
- 11.Quinnel RC (1980) Conservative management of trigger finger. Practitioner 224:187–190 [PubMed]
- 12.Richie CA 3rd, Eriner WW Jr (2003) Corticosteroid injection for treatment of de Quervain’s tenosynovitis: a pooled quantitative literature evaluation. J Am Board Fam Pract 16:102–106 [DOI] [PubMed]
- 13.Ta KT, Eidelman D, Thomson JG (1999) Patient satisfaction and outcomes of surgery for de Quervain’s tenosynovitis. J Hand Surg [Am] 24:1071–1077 [DOI] [PubMed]
- 14.Weiss AC, Akeiman E, Tabatabai M (1994) Treatment of de Quervain’s disease. J Hand Surg [Am] 19:595–598 [DOI] [PubMed]
- 15.Witt J, Pess G, Gelberman RH (1991) Treatment of de Quervain tenosynovitis: a prospective study of the results of injection of steroids and immobilization in splint. J Bone Joint Surg Am 73:219–222 [PubMed]
- 16.Zingas C, Failla JM, Holsbeek MV (1998) Injection accuracy of clinical relief of de Quervain’s tendinitis. J Hand Surg [Am] 23:89–96 [DOI] [PubMed]