Abstract
There is a high variance in sagittal morphology and complaints between different subjects suffering from spinal disorders. Sagittal spinal alignment and clinical presentation are not closely related. Different parameters have been used to describe the pelvispinal morphology based on standing lateral radiographs. We conducted a study using radiography of the lumbar spine combined with force platform data to examine the correlation between pelvispinal parameters and the gravity line position. Fifty consecutive patients with a mean age of 55 years (18–84 years) were compared to normal controls. Among patients we found a statistically significant correlation between the following spinal parameters: lumbar lordosis and sacral slope (r=0.77; P<0.001), sacral slope and pelvic incidence (r=0.72; P<0.001) and pelvic tilt and overhang (r=−0.93; P<0.001). In patients and controls, the gravity line position was found to be located at 60 and 61%, respectively, of the foot length measured from the great toe, ranging from 53 to 69%, when corrected for the individual foot length. The results indicate that subjects with and without spinal disorders have their gravity line position localised within a very small range despite the high variability for lumbar lordosis and pelvic tilt.
Résumé
L’aspect sagittal de profil de sujets présentant des problèmes rachidiens est très fréquent. Différents paramètres ont été utilisés pour décrire la morphologie du canal rachidien, avec radiographie de profil debout. Nous avons pratiqué une étude utilisant la radiographie de la colonne lombaire sur plateforme de force pour déterminer la corrélation existante entre les paramètres du canal rachidien et le centre de gravité. Cinquante patients d’âge moyen 55 ans (de 18 à 84 ans) ont été comparés à un groupe de patients contrôle. Parmi ces patients, nous avons trouvé une différence significative concernant les paramètres suivants, lordose lombaire, pente sacrée (r=0.77; P<0.001) pour la pente sacrée l’incidence pelvienne est: r=0.72; P<0.001, pour la bascule du pelvis r=0.93; P<0.001. La position du centre de gravité dans les deux groupes de patients a été localisée à 60 et 61% respectivement de la longueur du pied mesuré à partir du gros orteil et à partir de 53 à 69% lorsqu’une correction de la longueur du pied a été effectuée. Ces résultats montrent que chez les sujets avec ou sans troubles spinaux, la position du centre de gravité varie peu en dépit de grosses variations de la lordose lombaire et de la bascule pelvienne.
Introduction
Sagittal spine alignment and clinical presentation are not closely related. Sagittal morphology is specific to each individual and varies from one person to another, as do the complaints. Different parameters have been used to describe the pelvispinal morphology based on standing lateral radiographs [1]. It is well known that there is a correlation between the inclination of the sacrum and the lumbar lordosis [13]. Sagittal pelvic position influences the spinal balance [9, 11]. Recently, sagittal alignment of the lumbar spine during growth was studied [10]. Pelvic incidence was found to increase during growth as do pelvic tilt and lumbar lordosis. The authors suggested these changes probably occurred to avoid significant anterior displacement of the body’s centre of gravity. For acceptable long-term results in spinal arthrodesis, it is necessary to achieve adequate lumbar lordosis [8].
However, the gravity line is the vertical line passing through the center of gravity of the entire body. For a standing subject, the reference posture is described by the relation between the gravity line and all body segments [3].
Analysing standing posture in upright standing subjects needs an exact measurement of the orientation of various body segments with respect to the gravity line. The global gravity line was found to be on average 9 mm anterior of the bicoxofemoral line in healthy young adults [15]. A displacement of the gravity line position that was on average 10.9 mm posterior to the bicoxofemoral line was described in patients after thoracic Harrington spondylodesis and flat backs [7]. Several methods are described to obtain data on the gravity line [2, 3, 16]. Using a force platform to record gravitational data is an established technique. It provides information on the position of the gravity line [4].
Thus, the aim of this study was to examine the correlation between gravity line position and pelvispinal parameters using radiography of the lumbar spine combined with force platform data. Furthermore, we wished to gain improved understanding of the correlation of the sagittal spinal balance and the centre of gravity.
Patients
The study was approved by the local ethics committee (205/2004V). Fifty consecutive patients were prospectively recruited from the outpatient clinics of the spine unit. Twenty-nine female and 21 male patients were included, with a mean age of 55 years (18–84 years). For the men, the mean age was 51.6 years (34–72 years) and for the women 57.8 years (18–84 years). The patients were referred to the spine service for the following diseases: low-grade degenerative spondylolisthesis (16), lumbar spinal canal stenosis (11), sciatica (9), vertebral fractures (5), disc pathology (4), degenerative lumbar scoliosis (3) and spondylodiscitis (2). A modified questionnaire of the American Orthopedic Foot and Ankle Society (AOFAS) was used to rule out any foot and ankle disorders [6]. None of the patients were taking medication which could cause peripheral neuropathy or orthostatic problems. The mean (AOFAS) score was 95.3 points (85–100 points).
A second group comprised 25 healthy volunteers without spinal or foot and ankle disorders. There were 15 male and 10 female health care professional and student volunteers with a mean age of 32.9 years (21–56 years). For the men, the mean age was 30.7 years (21–45 years) and for the women 36.4 years (21–56 years). The populations were not age matched. The mean AOFAS score for the controls was 99.6 points (90–100 points).
After informed consent had been given, radiographs were obtained for the patient group, and plantar pressure measurement was done for the patients and normal controls.
Methods
Anatomic parameters
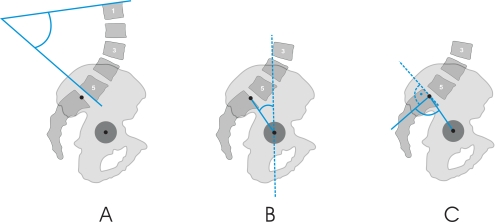
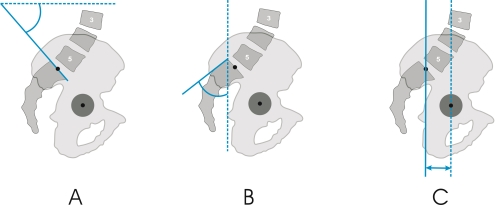
The analysis of lumbopelvic parameters was based on the criteria of Duval- Beaupère [1]. If the femoral heads were not exactly superimposed, the middle of the line connecting the centers of the two femoral heads was used as the landmark [8]. The spinal parameter is the lumbar lordosis (LL), measured between the cranial endplate of L1 and the caudal endplate of L5 (Fig. 1a). Pelvic tilt (PT) is the angle between the vertical plane and the line connecting the centre of the sacral plateau and the centre of the bicoxofemoral axis (Fig. 1b). Pelvic incidence (PI) was measured as the angle formed by the perpendicular line to the tangent line to the centre of the sacral plateau and the line connecting this centre to the centre of the axis of the femoral heads (Fig. 1c). The sacral slope (SS) is defined as the angle between the tangent line to the superior endplate of S1 and the horizontal plane (Fig. 2a). Sacral inclination (SI) is defined as the angle between the vertical plane and the tangential line to the sacral dorsum (Fig. 2b). The overhang of S1 (O) is the horizontal distance between the centre of the sacral plateau and the bicoxofemoral axis, measured in millimeters. It is negative when the hips are anterior to the sacral plateau and positive when the hips are posterior to it (Fig. 2c).
Fig. 1.
The lumbar lordosis (LL) is measured between the cranial endplate of L1 and caudal endplate of L5 (a). Pelvic tilt is the angle between the vertical plane and the line connecting the centre of the sacral plateau and the centre of the bicoxofemoral axis (b). Pelvic incidence is the angle formed by the perpendicular line to the tangent line to the centre of the sacral plateau and the line connecting this centre of the bicoxofemoral axis (c)
Fig. 2.
The sacral slope (SS) is measured between the tangent line to the superior endplate of S1 and the horizontal plane (a). Sacral inclination (SI) is defined as the angle between the vertical plane and the tangential line to the sacral dorsum (b). The overhang of S1 is the horizontal distance between the center of the sacral plateau and the bicoxofemoral axis (c)
Imaging and measurements
Standard anteroposterior and lateral radiographs of the lumbar spine including the centre of the femoral heads were taken in a standardised standing position with arms folded across the chest. The patients were asked to stand up straight but relaxed, with their knees extended. The 35×43-cm radiographs were taken using the standard protocol for the standing view. The distance from the radiographic source to the film was maintained at 115 cm for all exposures. The images were digitised (ADC Compact Plus, AGFA, Mortsel, Belgium) and transferred to a picture archiving and communication system (SIENET Magic Web, Version VA44A, Siemens AG, Erlangen, Germany). Means were derived by repeated (twice) manual angle measurements. The two legs of each angle were drawn with a mouse-driven pointer and calculated by the software.
Pedography measurement
The centre of pressure (COP) was derived by an EMED-SF pressure measurement platform with a sensor density of 1/cm2 and maximum force of 125 N/cm2 (Novel, Munich, Germany). The patients had to stand barefoot on the platform in the same standardised standing position as the radiographs were taken. The patients were asked to stand up straight but relaxed with their knees extended and their arms folded across the chest. Plantar pressure measurements were performed three times in the dynamic mode with a frame rate of 10 Hz for a time interval of 5 seconds. Pressure values for each frame were exported as an ASCII file and analysed using MatLab (The Mathworks Inc., Natick, Mass.). For each frame the COP was determined within the force plate coordinate system. The mean value for all frames was established with respect to foot length (FL) and stance width (SW). FL was measured on the y-axis from the great toe to the heel, and SW was measured on the x-axis from the most lateral prominence of the left foot to the most lateral prominence of the right foot. Both were characterised by x- and y-coordinates, respectively (COPx; COPy). We thus corrected the COP for foot size by division by the individual FL and SW, respectively, and consequently derived the relative position of the COP in each subject using the formula: COPcx=COPx/SW and COPcy= COPy/FL.
From the standard deviation of the COP, we were able to quantify the amount of postural sway in each direction (Sx=SD COPx; Sy=SD COPy).
Data analysis
All data were analysed using SPSS for Windows (Release 9.0.1). As suggested by previous publications, an intraclass correlation coefficient was calculated for assessment of the intrarater reliability [14].
Intrarater reliability figures were calculated from repeated measurements of a subset of 20 randomly selected lateral radiographs of the lumbar spine. Likewise, the coordinates of the centre of pressure were correlated with the different lumbopelvic parameters to assess a possible interaction using two-sided Pearson’s correlation [5]. In order to test for possible influences of factors such as sex and age on the lumbopelvic parameters, we performed a subsequent factorial ANOVA where these factors were separately chosen as co-factors. The level of significance was set at 0.01.
Results
Out of 50 patients, two were excluded due to missing data. The results of repeated angle measurements demonstrated satisfactory reproducibility. The mean variability was 4° for measurements obtained on digitised radiographs using the mouse-driven cursor. The intraclass correlation coefficient (ICC) calculated as described above varied between 0.98 and 0.99. Reliability figures for the LL measurement had a mean of 0.99, 0.99 for SS, 0.98 for SI, 0.98 for PT, 0.99 for PI and 0.99 for the O of S1, respectively.
The mean values of the minimum, maximum and standard deviations of each variable measured are presented (Table 1).
Table 1.
Results of pelvic and spinal parameters in patients
| Study group | Lazennec et al. [8] | |||||
|---|---|---|---|---|---|---|
| Minimum | Maximum | Mean | SD | Mean | SD | |
| Lumbar lordosis (degrees) | 18.5 | 74 | 42.1 | 14.7 | - | - |
| Sacral slope (degrees) | 22.5 | 64 | 39.7 | 10.8 | 38.9 | 2.7 |
| Sacral inclination (degrees) | 27 | 95 | 52.5 | 13.7 | - | - |
| Pelvic incidence (degrees) | 38 | 92 | 62.9 | 14.9 | 56.9 | 7.7 |
| Pelvic tilt (degrees) | 2.5 | 40 | 21.7 | 9.4 | 17.9 | 7.4 |
| Overhang of S1 (mm) | −80 | −4.5 | −41.7 | −9.4 | - | - |
Mean value of overhang of S1 was −41.6 mm (±17.8 mm) ranging from −4.5 to −84 mm.
Plantar pressure findings are summarised (Table 2). The mean foot length of men was significantly longer compared to the women (P<0.001). There were no significant statistical differences between men and women with respect to pelvic or spinal parameters.
Table 2.
Values of plantar pressure measurement in patients and healthy controls
| Patients | Controls | |||
|---|---|---|---|---|
| Mean (range) | SD | Mean (range) | SD | |
| FL (cm) | 23.5 (20–27.5) | 1.85 | 24.5 (20.7–28.7) | 2.11 |
| SW (cm) | 23 (17–27.7) | 2.56 | 23.8 (20–27.3) | 2.2 |
| COPy (cm) | 14.2 (11.3–17) | 1.39 | 14.8 (11.9–17.4) | 1.5 |
| COPx (cm) | 11.2 (8–13.54) | 1.35 | 11.9 (9.7–14.2) | 1.2 |
| COPcy | 0.60 (0.53–0.69) | 0.04 | 0.61 (0.53–0.69) | 0.03 |
| COPcx | 0.49 (0.43–0.55) | 0.02 | 0.50 (0.45–0.54) | 0.02 |
| Sy (cm) | 0.28 (0.15–0.47) | 0.07 | 0.30 (0.14–0.77) | 0.14 |
| Sx (cm) | 0.28 (0.14–0.57) | 0.08 | 0.28 (0.15–0.58) | 0.12 |
FL= foot length; SW= stance width; COPy= y-coordinate of COP; COPx= x-coordinate of COP; COPcy=COPy/FL; COPcx=COPx/SW; Sy=SD(COPy); Sx=SD(COPx)
The position of the corrected centre of pressure (COPcx; COPcy) for patients and controls was equal within a very small range.
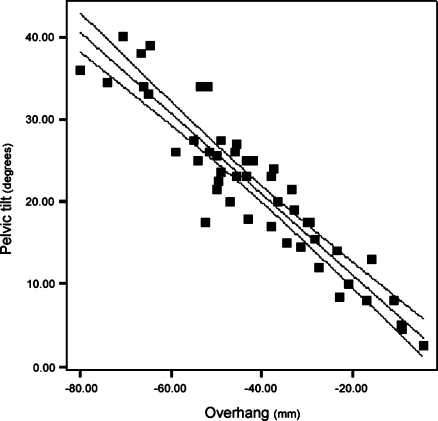
We found a statistically significant correlation (Pearson’s bilateral test) between the following values: lumbar lordosis and sacral slope (r=0.77; P<0.001); lumbar lordosis and sacral inclination (r=0.51; P<0.001); lumbar lordosis and pelvic incidence (r=0.53; P<0.001); sacral slope and sacral inclination (r=0.66; P<0.001); sacral slope and pelvic incidence (r=0.72; P<0.001); pelvic incidence and pelvic tilt (r=0.68; P<0.001); pelvic incidence and overhang (r=−0.52; P<0.001); pelvic tilt and overhang (r=−0.93; P<0.001) (Fig. 3); sacral inclination and pelvic incidence (r=0.3; P=0.038); sacral inclination and overhang (r=0.41; P=0.003).
Fig. 3.
Main statistical linear correlations (Pearson’s bilateral test): correlation between pelvic tilt angle and overhang of S1 (r=−0.93; P<0.001)
There was no significant statistical correlation between the pelvic parameters and the values of plantar pressure measurement. Age and sex did not influence any of the studied parameters.
Discussion
The purpose of the study was to document the sagittal alignment of the lumbar spine and pelvis in 50 patients with spinal disorders and to correlate the parameters with the gravity line position.
The results demonstrate the high variability of sagittal alignment of the lumbar spine and pelvis in the standing position. In contrast, the determined position of the gravity line is almost constant in controls and patients despite different underlying diseases.
We found the gravity line position in patients and healthy controls to be located at 0.60 and 0.61, respectively (i.e., at 60 and 61%, respectively, of the foot length measured from the great toe), ranging from 0.53 to 0.69 when corrected for the individual foot length.
There are two major limitations to this work. First, the recruited group of patients is small and heterogeneous because they were selected consecutively from our outpatient clinic. Secondly, we had no radiographs of the normal controls due to ethical concerns. Therefore, no lumbopelvic parameters of the controls were obtained. Since the normal controls studied were mainly recruited from medical and paramedical students at our institution, the control group was significantly younger than the patient group.
Plantar pressure measurement and imaging of the lumbar spine by radiography was done in the same standardised posture. In both settings, the patients were asked to stand barefoot in an upright but relaxed position with their knees extended and their arms folded across the chest.
In any case, small numbers are a problem of power, i.e., the validity of negative findings remains questionable, while the probability of eliciting true-positive findings is reduced. Thus, our positive findings are not touched by the small sample size. The method we used is sound and valid and has been described in a number of other publications [3, 7, 15, 16]. The reliability of the measurements was very good and compared well to other figures [12]. Earlier studies have pointed out the usual degree of variability in lumbopelvic parameters in children [10], in normal volunteers [12] and in patients after lumbosacral fusion [8].
As shown in Table 1, the values for PI, PT and SS were comparable to those obtained by Lazennec et al. [8]. Marty and co-workers studied 39 patients with spondylolisthesis and reported a strong correlation between sacral parameters and the pelvic incidence. They found the pelvic incidence to be greater than among normal adults [11]. The correlation between the different parameters of the lumbar spine and pelvic alignment indicates that the morphology of lumbar lordosis is dependent on the orientation of the sacral slope, sacral inclination and pelvic incidence. These relations have been described by Duval-Beaupere and colleagues [2].
We confirm the relation between lumbar lordosis and sacral slope (r=0.77; P<0.001), which is not as strong as that found in 100 healthy volunteers described by Vaz et al. [15]. The relation between lumbar lordosis and pelvic incidence was less pronounced than that found in healthy controls [15].
The results of this study, therefore, indicate that subjects with or without different spinal disorders have their gravity line position localised within a very small range despite the variability for lumbar lordosis and pelvic tilt. Since muscle tone, strength and neurological mechanisms affect the standing posture in an individual, we think it is necessary to consider these factors of foremost importance to understand the control of posture and the gravity line position. The individual active muscular activity necessary to keep the centre of gravity controlled might be the key to understand the different clinical presentation of patients with the same sagittal misalignment. Therefore, we will correlate the results of electromyography with pelvispinal parameters and the gravity line position in our future investigations to address the question of how patients compensate to achieve a similar positioning of the centre of gravity.
References
- 1.Duval-Beaupere G, Robain G (1987) Visualization on full spine radiographs of the anatomical connections of the centres of the segmental body mass supported by each vertebra and measured in vivo. Int Orthop 11:261–269 [DOI] [PubMed]
- 2.Duval-Beaupere G, Schmidt C, Cosson P (1992) A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 20:451–462 [DOI] [PubMed]
- 3.Gangnet N, Pomero V, Dumas R, Skalli W, Vital J-M (2003) Variability of the spine and pelvis location with respect to the gravity line: a three-dimensional stereoradiographic study using a force platform. Surg Radiol Anat 25:424–433 [DOI] [PubMed]
- 4.Graf P (1993) The EMED System of foot pressure analysis. Clin Podiatr Med Surg 10:445–454 [PubMed]
- 5.Harms V (1992) Biomathematik, Statistik und Dokumentation. Harms Verlag, Kiel
- 6.Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M (1994) Clinical rating system for the ankle-hindfoot, midfoot, hallux and lesser toes. Foot Ankle 15:349–353 [DOI] [PubMed]
- 7.Kluba T, Muller O, Grieb S, Zeger G, Schafer J, Niemeyer T (2004) Measurement of gravity line position 15–25 years after Harrington-spondylodesis in adolescent idiopathic scoliosis. Z Orthop 142:188–193 [DOI] [PubMed]
- 8.Lazennec J, Ramare S, Arafati N, Laudet C, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R (2000) Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J 9:47–55 [DOI] [PMC free article] [PubMed]
- 9.Legaye J, Duval-Beaupere G, Hecquet J, Marty C (1998) Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal curves. Eur Spine J 7:99–103 [DOI] [PMC free article] [PubMed]
- 10.Mac-Thiong J, Berthonnaud E, Dimar J, Betz R, Labelle H (2004) Sagittal alignment of the spine and pelvis during growth. Spine 29:1642–1647 [DOI] [PubMed]
- 11.Marty C, Boisaubert B, Descamps H, Montigny JP, Hecquet J, Legaye J, Duval-Beaupere G (2002) The sagittal anatomy of the sacrum among young adults, infants, and spondylolisthesis patients. Eur Spine J 11:119–125 [DOI] [PMC free article] [PubMed]
- 12.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J (2005) Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine 30:346–353 [DOI] [PubMed]
- 13.Stagnara P, De Mauroy JC, Dran G, Gonon GP, Costanzo G, Dimnet J (1982) Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine 7:335–342 [DOI] [PubMed]
- 14.Streiner DL, Norman GR (1995) From health measurements scales. A practical guide to their development and use. Oxford Medical Publications, London
- 15.Vaz G, Roussouly P, Berthonnaud E, Dimnet J (2002) Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J 11:80–87 [DOI] [PMC free article] [PubMed]
- 16.Zatsiorsky VM, King DL (1998) An algorithm for determining gravity line location from posturographic recordings. J Biom 31:161–164 [DOI] [PubMed]