Abstract
Bone loss in the forearm results from high-energy trauma or follows non-union with infection. Ilizarov methodology provides stable fixation without implantation of permanent foreign bodies while permitting wrist and elbow movement. We are reporting our experience using distraction osteogenesis in the treatment of traumatic bone loss in the forearm. From 1991 to 2000, 11 consecutive patients with traumatic forearm bone loss were treated with Ilizarov ring fixation. Records were reviewed retrospectively. All patients were contacted 2-10 years after surgery at the Ilizarov Clinic in Lecco, Italy. Eleven atrophic non-unions with bone loss were treated. The time from injury to Ilizarov treatment averaged 2.1 years. Follow-up averaged 6.2 years. The union rate with Ilizarov treatment alone was 64%. Thirty-six percent of the patients were converted to a hypertrophic non-union and underwent compression plating. The overall rate of union was 100%. There were four unplanned reoperations and no refractures, neurovascular injuries or deep infections. Three patients had significant limitations of wrist function. Nine patients described their function as excellent. Ilizarov fixation with bone transport is a viable treatment option for atrophic forearm non-unions with bone loss. Treatment resulted in ablation of infection, healing of atrophic non-unions with minimal complications and early extremity use.
Résumé
Les pertes de substance osseuses à l’avant-bras résultent d’un traumatisme à haute énergie ou d’une pseudarthrose septique. La méthode d’Ilizarov avec transport osseux donne une fixation stable permettant une mobilisation du poignet et du coude sans implantation permanente de matériel. De 1991 à 2000 11 patients consécutifs présentant une pseudarthrose atrophique avec perte de substance osseuse de l’avant-bras ont été traité ainsi et revus rétrospectivement 2 à 10 ans après. Le délai entre le traumatisme et le traitement étudié était en moyenne de 2,1 ans et le suivi moyen de 6,2 ans. Il y avait 64% de consolidation après traitement simple par la méthode d’Ilizarov et chez les autres patients elle avait conduit à une pseudarthrose hypertrophique nécessitant ensuite une ostéosynthèse en compression par plaque vissée. Quatre réinterventions non prévues ont été nécessaires. Le taux total de consolidation était de 100%. Il n’y avait pas de fracture itérative ni de complication vasculo-nerveuse ni d’infection profonde. Trois patients avaient une limitation nette de la fonction du poignet. Neuf patients décrivaient leur fonction comme excellente. La méthode d’Ilizarov est une bonne option thérapeutique pour les pseudarthrose atrophiques de l’avant-bras avec perte de substance osseuse. Elle permet le traitement de l’infection, la consolidation osseuse avec un minimum de complications et un recouvrement rapide de la fonction.
Introduction
Bone loss in the forearm may occur as a result of high-energy blunt trauma, gunshot injury or following non-union with infection. A resulting defect in either the radius or ulna is difficult to treat because of the close proximity of vital neurovascular structures and the need to maintain supination, pronation and range of motion of the wrist and elbow. In cases with significant soft tissue damage or coexisting infection, the placement of the bone graft and metal implants through extensive incisions may be undesirable. Ilizarov methodology provides stable fixation without implantation of permanent foreign bodies while permitting movement of the wrist and elbow. The technique of distraction osteogenesis also allows bone loss to be treated without the morbidities associated with autogenous iliac crest or vascularised free fibula transfer. This report describes our experience using Ilizarov ring fixation for the treatment of traumatic bone loss in the forearm.
Materials and methods
From 1991 to 2000, 44 cases of non-unions were treated using various surgical modalities. Of these, 11 consecutive patients with forearm bone loss and atrophic non-union resulting from injuries were treated with Ilizarov ring fixation. Our study comprised the 11 cases of atrophic non-unions with bone loss. Patients were followed prospectively and their records reviewed retrospectively through a database at the Ospedale Generale de Lecco, where all the patients had undergone surgery by a single surgeon (M.A.C). All patients were contacted 2 to 10 years after treatment for re-examination and interview. Demographic data were collected through a medical record review. Follow-up examinations were performed at the Ilizarov Clinic in Lecco, Italy, by surgeons other than the primary operating surgeons.
Data collected included the nature of the original injury, initial treatment and surgery, type of non-union, presence of infection, amount of resection and time period for transport and docking. Outcome measurements included time to healing, presence or absence of complications and final range of motion of the wrist and elbow. Healing was defined as the presence of clinical and radiographic union. Radiographic union was defined as a minimum of three of four bridging cortices at the non-union site. Clinical union was defined as the resumption of activities of daily living without pain at the treatment site and the absence of pain with a stress examination. Complications were defined as any condition requiring unplanned operation during the treatment period, non-union, infection, unplanned synostosis or premature discontinuation of treatment.
Surgical technique
The operating surgeon used the “hybrid system” of Ilizarov fixation as described by Catagni and Cattaneo in all cases [2–4, 18]. Standard Ilizarov rings were used in conjuction with 4- or 5-mm pins and 1.8-mm stainless steel wires. Limbs were prepared and draped and the elbow positioned at 90º. External olecranon or metacarpal traction was applied if required to maintain alignment. The frame was assembled with appropriately sized rings and kept ready on the side table, at the time of surgery. The olecranon proximally , the subcutaneous border of the mid ulna and styloid process of the radius served as landmarks. Kirschner wires (1.8 mm) were carefully passed through the safe corridors of the forearm and bone and affixed to the frame. Generally, two rings were used for each segment of intact bone. Additional half-pins were used in metaphyseal sites or where wire placement would compromise the soft tissues. The Kirschner wires were tensioned with a tensioning device.
The non-union site was exposed either before or after frame assembly, depending on the location and stability of the bone. Infected or atrophic bone was exposed until bleeding bone was present at both ends. The soft tissue bed was debrided of all non-viable tissue. Thorough irrigation of the wound with saline solution was performed following debridement. If possible, the wound was closed by direct suture, in some cases over a drain. Once the wound was stable and the Ilizarov frame had been applied, a metaphyseal corticotomy in the distal radius or proximal ulna was performed using the technique described by Ilizarov [7]. Care was given to preserving as much periosteum as possible . Diastasis of the corticotomy site was avoided and postoperative reduction confirmed by radiography.
Distraction was started after a latent period of 7–10 days, depending upon the age of the patient and the quality of the bone at the rate of 1 mm per day (one-quarter turn every 6–8 h). Postoperatively, the patient attended physical therapy and was encouraged in active use of the hand and elbow for activities of daily living. Radiographic union was defined as the presence of bridging callus on at least three of the four cortices on the antero-posterior and lateral radiographic views. Healing at the docking site was determined by the presence of complete cortication of the regenerate on at least three sides, using orthogonal radiographs. Clinical union was defined as no pain with activities of daily living and the absence of tenderness at the docking and regenerate sites. We defined healing for the purposes of this study as the presence of radiographic and clinical union.
Results
Forty-four consecutive forearm non-unions were treated during the study period. Of the 44, 33 showed varying degrees of bone formation and were classified as normotrophic and hypertrophic non-unions. The remaining 11 patients who had atrophic non-union with bone loss comprise the cohort of this study. There were seven males and four females with an age range of 3 to 50 years (mean =32 years) at the time of treatment. The average time from injury to Ilizarov treatment was 2.1 years (range 6 months to 9 years). Patients averaged 1.4 operations before presentation. Seven patients had osteomyelitis verified by bone culture. The average follow-up after Ilizarov treatment was 6.2 years (range 2.3 to 16 years). Transport times prior to docking ranged from 6 to 30 weeks (mean =15.6 weeks). The mean regenerate length was 4.2 cm (range 1.7 to 7.3 cm). Docking time averaged 21 weeks. The mean time to frame removal was 30 weeks (range 16 to 62 weeks) (Table 1). Three patients underwent planned bone grafting at the docking site. The union rate with Ilizarov treatment alone was 64%. Four (36%) patients were converted from an atrophic non-union with bone loss to a stable hypertrophic non-union. All of these patients subsequently underwent frame removal and compression plating with eventual successful union. All non-unions eventually united. Four unplanned reoperations were performed: two for loss of reduction and two for pin tract infection. No unplanned reoperations were required for docking site refracture or failure. There were no regenerate refractures, nerve or vascular injuries, or deep infections. The overall rate of union, including subsequent plate treatment, was 100% (Table 2).
Table 1.
Patient treatment data
| Range | Mean | |
|---|---|---|
| Age | 3 to 50 years | 32 years |
| Number of prior operations | 1–4 | 1.4 |
| Transport time | 6 to 30 weeks | 15.6 weeks |
| Docking time | 10 to 44 weeks | 21 weeks |
| Regenerate length | 1.7 to 7.3 cm | 4.2 cm |
| Time to healing | 26 weeks to 154 weeks | 57.1 weeks |
Table 2.
Treatment outcome
| Total number | Percentage | |
|---|---|---|
| Ostemyelitis eliminated | 8 | 100% |
| Union rate with Ilizarov alone | 7 | 64% |
| Union rate with additional procedures | 4 | 36% |
| Total union rate | 11 | 100% |
Range of motion was evaluated at the final follow-up. Three patients had significant limitations of wrist function. Nine of 11 patients described their function subjectively as excellent (Table 3). Ten of 11 patients were gainfully employed and 2 of the 11 patients stated that their work status was impaired because of their injury. No clinical evidence of infection was found in any of the patients.
Table 3.
Wrist function outcome
| Function | Total number | Percentage |
|---|---|---|
| Flexion >70° | 8 | 73% |
| Extension >60° | 8 | 73% |
| Pronation >80° | 8 | 73% |
| Supination >80° | 8 | 73% |
Discussion
Diaphyseal forearm fractures are common injuries that can be treated with a high rate of success [15]. Depending on the age of the patient and pattern of the injury, both open and closed techniques have been shown to be effective treatment methods. Reduction of the forearm bone is difficult to maintain in acceptable alignment using closed treatment techniques, particularly in adults [1]. Intramedullary nailing and plating of these fractures have been shown to produce excellent results with union rates approaching 98%; however, there can be a significant incidence of non-union [1, 16, 17, 20].
Non-union in the upper limb leads to loss of movement and, consequently, reduced function. Functional impairment is frequently exacerbated by restriction of supination and pronation of the forearm caused by the angulation of the radius and ulna. A proportion of the patients with non-union develop an atrophic pattern with which there is often associated bone loss. The causes of bone loss are multiple, including open fractures, infection following surgery or gunshot wounds. Treatment of bone loss in the forearm following trauma is a reconstructive challenge. Deep infections, a damaged soft tissue envelope and long periods of upper extremity disuse complicate these difficult injuries.
Intramedullary nailing has been recommended as a treatment method for non-union despite 7% non-union rates reported for primary nailing [5, 16]. Weiland has recommended the use of vascularized autografts for the management of bone defects [19]. Autologous fibular grafting is technically demanding and has potential donor site morbidity, but has a high rate of success [11]. Jupiter (1997) reported 11% development of non-union of the graft to the host site following compression plating and grafting [9] with iliac crest autograft.
Bone defects and non-union have been dealt with by bone grafting and plating [8, 14]. A variety of new composite biosynthetic bone graft substitutes are available and have been advocated [10]. Often temporary stabilisation is required prior to open reduction and internal fixation for these fractures as the bone loss is associated with open fractures. Bone grafting and plating would b precluded if infection were suspected in an atrophic non-union. Ilizarov treatment with bone transport is a viable option for treatment of both atrophic non-unions and bone loss in the forearm [6, 12, 13, 18].
We reviewed 44 patients who developed forearm non-unions. Eleven developed an atrophic pattern with an associated bone defect. The Ilizarov technique of distraction osteogenesis was used to eliminate infection, restore the defect with autologous bone and gain union. Union was ultimately achieved in all cases. In four (36%) patients, union was not achieved in the apparatus, and subsequent plating was required. Nonetheless, in these four cases atrophic non-unions with infection and bone loss were converted to uninfected, hypertrophic non-unions that could be safely and reliably treated with a standardised technique.
A limitation of our study is the small sample size from a single surgeon. The retrospective, case series method as opposed to a prospective study introduces potential inconsistencies of treatment, particularly given the small sample size. Nonetheless, the study highlights the benefits and difficulties of using this innovative technology in the treatment of a relatively rare, yet complex problem.
This technique is useful in dealing with traumatic bone loss in the forearm resulting from high-energy trauma or non-union with infection [12]. Ilizarov methodology provides stable fixation without implantation of permanent foreign bodies. The Ilizarov apparatus allows for immediate therapy of the hand, wrist and elbow as well as early use of the extremity in the activities of daily living. The majority of patients were able to resume normal working activity. Additionally, Ilizarov treatment resulted in the ablation of infection and ultimately healing of atrophic non-unions with minimal complications.
The technique of bone transport in the forearm is technically demanding, as are all other forms of treatment for these challenging injuries. The treatment approach with Ilizarov should be viewed as a staged paradigm including the eradication of infection, restoration of bone loss, healing of osseous non-union and ongoing rehabilitation of the upper extremity (Fig. 1).
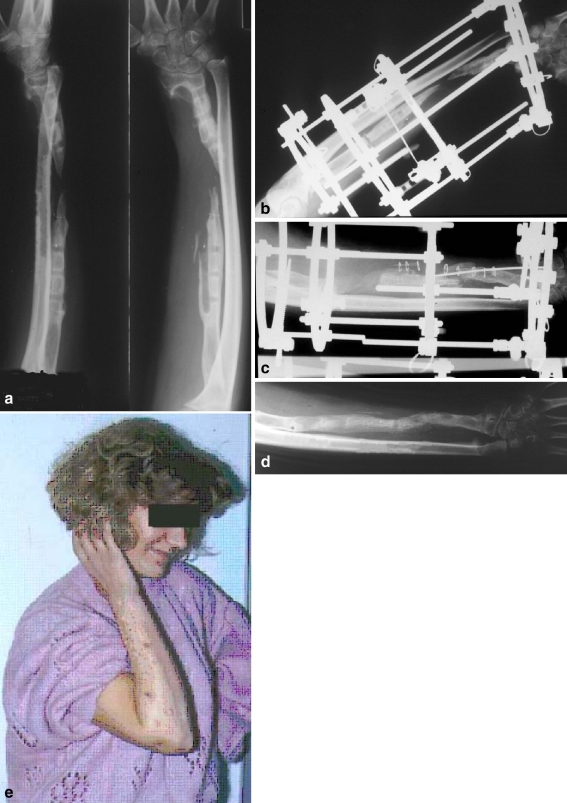
Fig 1.
Case of a 34-year-old female with infected, atrophic non-union of the radius following plating. a Preoperative anteroposterior and lateral radiographs following plate removal. b Joint-sparing Ilizarov fixator in situ following resection of infected bone and corticotomy. c Anteroposterior radiograph showing docking of the transported segment aided by an intramedullary guide wire, with a maturing regenerate. d Final radiograph, after fixator removal, showing a bridging regenerate across the radial defect. e Outcome after 26 weeks with an excellent range of motion
Footnotes
The authors did not receive grants or outside funding in support of their research preparation of this manuscript.
References
- 1.Burwell HN, Charnley AD (1964) Treatment of forearm fractures in adults with particular reference to plate fixation. J Bone Joint Surg Br 46:404–425 [PubMed]
- 2.Catagni MA, Guerreschi F, Holman JA, Cattaneo R (1994) Distraction osteogenesis in the treatment of stiff hypertrophic non-unions using the Ilizarov apparatus. Clin Orthop Relat Res 301:159–163 [PubMed]
- 3.Catagni MA, Malzev V, Kirienko A (2004) Advances in Ilizarov apparatus assembly. Il quadratino, Italy
- 4.Cattaneo R, Villa A, Catagni MA, Bell D (1990) Lengthening of the humerus using the Ilizarov technique. Description of the method and report of 43 cases. Clin Orthop Relat Res 250:117–124 [PubMed]
- 5.Christensen NE (1976) Technique, errors and safeguards in modern Kuntscher nailing. Clin Orthop Relat Res 115:182–188 [PubMed]
- 6.Esser RD (1996) Treatment of a bone defect of the forearm by bone transport. A case report. Clin Orthop Relat Res 326:221–224 [DOI] [PubMed]
- 7.Ilizarov GA (1992) Transosseous osteosynthesis. Theoretical and clinical aspects of the regeneration and growth of tissue. Springer-Verlag-Heidelberg
- 8.Jupiter JB, Ruedi T (1992) Intraoperative distraction in the treatment of complex non-unions of the radius. J Hand Surg [Am] 17(3):416–422 [DOI] [PubMed]
- 9.Jupiter JB, Gerhard HJ, Guerrero J, Nunley JA, Levin LS (1997) Treatment of segmental defects of the radius with use of the vascularized osteoseptocutaneous fibular autogenous graft. J Bone Joint Surg Am 79(4):542–550 [DOI] [PubMed]
- 10.Lane JM, Bostrom MP (1998) Bone grafting and new composite biosynthetic graft materials. Instr Course Lect 47:525–534 [PubMed]
- 11.Mack GR, Lichtman DM, MacDonald RI (1979) Fibular autografts for distal defects of the radius. J Hand Surg [Am] 4(6):576–583 [DOI] [PubMed]
- 12.Pavolini B, Maritato M, Turelli L, D’Arienzo M (2000) The Ilizarov fixator in trauma: a 10-year experience. J Orthop Sci 5(2):108–113 [DOI] [PubMed]
- 13.Saleh M, Yang L, Sims M (1999) Limb reconstruction after high energy trauma. Br Med Bull 55(4):870–884 [DOI] [PubMed]
- 14.Scaglietti O, Stringa G, Mizzau M (1965) Bone grafting in non-union of the forearm. Clin Orthop Relat Res 43:65–76 [DOI] [PubMed]
- 15.Singer BR, McLauchlan GJ, Robinson CM, Christie J (1998) Epidemiology of fractures in 15,000 adults: the influence of age and gender. J Bone Joint Surg Br 80(2):243–248 [DOI] [PubMed]
- 16.Street DM (1986) Intramedullary forearm nailing. Clin Orthop Relat Res 212:219–230 [PubMed]
- 17.Stern PJ, Drury WJ (1983) Complications of plate fixation of forearm fractures. Clin Orthop Relat Res 175:25–29 [PubMed]
- 18.Villa A, Paley D, Catagni MA, Bell D, Cattaneo R (1990) Lengthening of the forearm by the Ilizarov technique. Clin Orthop Relat Res 250:125–137 [PubMed]
- 19.Weiland AJ, Phillips TW, Randolph MA (1984) Bone grafts: a radiologic, histologic, and biomechanical model comparing autografts, allografts, and free vascularized bone grafts. Plast Reconstr Surg 74(3):368–379 [DOI] [PubMed]
- 20.Wei SY, Born CT, Abene A, Ong A, Hayda R, DeLong WG Jr (1999) Diaphyseal forearm fractures treated with and without bone graft. J Trauma 46(6):1045–1048 [DOI] [PubMed]